Introduction
Modified Blalock-Taussig shunt (BT shunt) is a palliative operation used for cyanotic heart diseases in with decreases pulmonary blood supply. The first BT shunt was performed at Johns Hopkins Hospital in 1944 by collaborative work of three individuals: the paediatric cardiologist Dr Helen Taussig, the cardiac surgeon Dr Alfred Blalock, and Mr. Vivien Thomas, a laboratory assistant. Reference Mainwaring and Mainwaring1 The original technique has been modified, which utilises an interposition polytetrafluoroethylene (PTFE) graft to make a systemic to pulmonary shunt without transecting the subclavian artery. Reference Yuan, Shinfeld and Raanani2 The definitive management of tetralogy of Fallot (TOF) is total corrective surgery, but these patients can be managed with BT shunt. The aim is to enhance the growth of pulmonary arteries by increasing pulmonary perfusion. Reference Starr3
With the advancement in interventional cardiology, palliative interventions like right ventricular outflow tract stent, Reference Li, Zhao, Hu, Zhang, Wu and Liu4 balloon pulmonary valvotomy, Reference Remadevi, Vaidyanathan, Francis, Kannan and Kumar5 and PDA (patent ductus arteriosus) stenting, Reference Ilyas, Rehman, Hussain, Khan, Ahmed and Akbar6 the role of BT shunt in TOF is decreasing. In Figure 1, we have shown the latest algorithm for the management of TOF, which does not have BT shunt in it. Reference Moorjani and Moorjani7

Figure 1. Current management algorithm for TOF.
In this article, we will share our 5-year experience at our institute.
Patients and methods
Settings
Children Hospital Lahore/University of Child Health Sciences.
Duration
Five years (January 2019–December 2023). It is a retrospective observational study. Files of all the patients admitted in our department from January 2019 to December 2023 were reviewed. Age, weight, hospital stay, inotropic support duration, mechanical ventilation duration, and outcome were studied. In each year, a number of patients were noted, the indications for BT shunt were noted, the site of incision (sternotomy/thoracotomy) was noted, and major outcomes were described in percentages. The age, weight, and other characteristics were described in mean with range.
Results
As shown in Figure 2, from January 2019 to December 2023, 595 patients underwent total correction, while 173 patients underwent BT shunt.
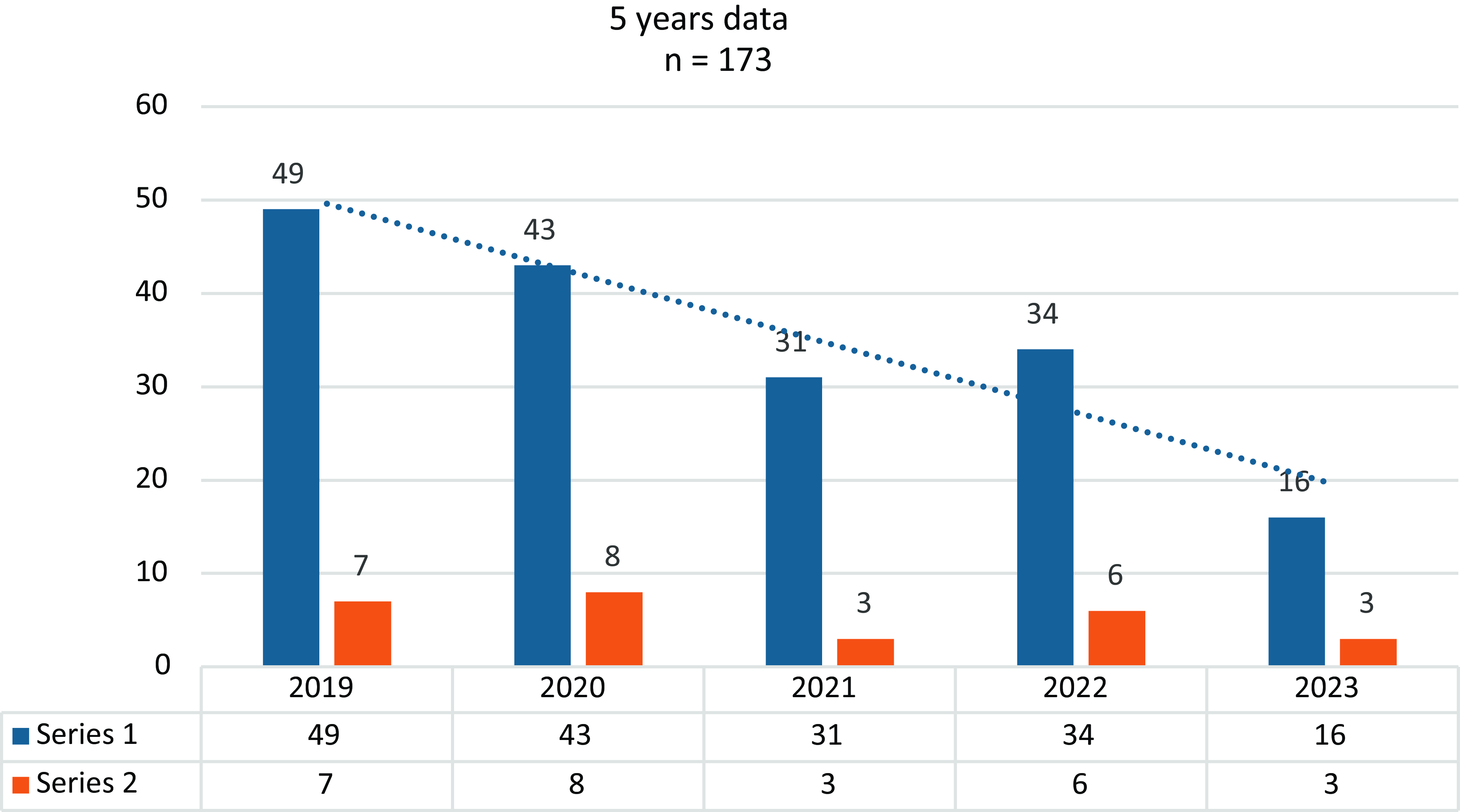
Figure 2. Five years data of BT shunt in TOF.
The mean age was 31 months, and the mean weight was 9.3 kg. The overall mortality for BT shunt was 15% after BT shunt. Table 1 shows the patient characteristics. Table 2 shows indications for BT shunt.
Table 1. Characteristics of the patients
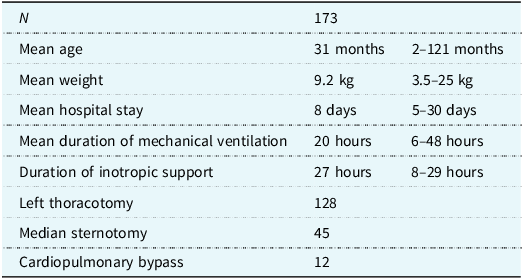
Table 2. Indications of BT shunt

CPB = cardiopulmonary bypass.
Hypercyanotic spell not controlled by medical management was the most common indication for BT shunt in our setup. About 12 patients required cardiopulmonary bypass for BT shunt. Most of them were those with disconnected pulmonary arteries.
About 27 (15%) patients died during hospital stay. The most common cause of death was shunt blockage. A few patients died of pulmonary overflooding and left ventricular dysfunction. A 5 mm PTFE graft was used in 138 patients, while 4 mm in 6 mm grafts were used in others. Only two patients received a 3.5 mm shunt.
Most of the surgeons in our institute prefer left thoracotomy for BT shunt, but some routinely do median sternotomy for BT shunt.
Discussion
While the modern world is moving towards interventions like PDA stenting or right ventricle outflow tract stenting, the role of BT shunt in developing countries like ours is also on the decline as shown in Figure 2. While PDA stenting is becoming more common in developed countries, we are moving towards total correction of TOF in earlier age groups. Now, we are doing total correction at a lower age. Figure 3 shows the decline in the mean age at the time of total correction over the last 7 years. While in the modern world, it is rare to see unrepaired patient with TOF beyond the age of 6 months, in our setup, where there are large numbers of patients waiting for surgery, elective repair of TOF before the age of 6 months is probably not possible in the near future.

Figure 3. Decreasing mean age for total correction for tetralogy of Fallot.
In our institute, till 2015, the trend was to go for BT shunt in any patient with TOF who has weight less than 10 kg. With the improvement in intraoperative and post-operative care, we are now doing total correction in TOF patients with weight as low as 5 kg.
The mortality rate of BT shunt in TOF is 4–8%, Reference Singh, Chauhan and Choudhury8 while those who need cardiopulmonary bypass for shunt placement have a higher mortality rate especially in neonates. Reference Petrucci, Brien and Jacobs9 Reference Ashraf, Tian, Zacharrias, Cowan, Martin and Watterson,10 In our study, the mortality rate for BT shunt placement was 15%, which is higher than the international standards. This can be attributed to poor post-operative care in ICU. Most of the deaths occurred in our ICU within 48 hours post-operatively. Shunt blockage was the most common reason for the death. In a few patients, ventricular dysfunction was aggravated by the BT shunt resulting in death. Our results are comparable to a study by Ryandi, Reference Riyandi, Lilyasari, Juzar and Rahmat11 which had a mortality rate of 12–14.5%.
The thoracotomy approach was used more often than sternotomy for the BT shunt procedure at our centre. This approach is thought to be accessible, faster, and safer, but a study in Boston revealed that thoracotomy had higher chances of failure as compared to sternotomy. Reference Talwar, Kumar, Muthukkumaran and Airan13 One of the life-threatening risk is phrenic nerve paralysis, with chances as high as 23.8% in patients who undergo this procedure through thoracotomy. Reference Akay, Ozkan and Gultekin14 In our study, there was not a single incidence of phrenic nerve injury during BT shunt placement.
PDA stenting is replacing BT shunt in developed countries, which has shown promising results. Reference Glatz, Petit and Goldstein15 Tseng et al. in their meta-analysis showed the superiority of PDA stent over BT shunt in terms of better haemodynamics and hospital stay. Reference Tseng, Truong and Peck16 Sheeth et al. Reference Shaath, Jijeh and Fararjeh17 in their study demonstrated better and smoother ICU stay with ductal stenting. Nesser Reference Nasser, Abdulrahman, Qwaee, Alakfash, Mohamad and Kabbani18 and Al Kindi Reference Al Kindi, Al Harthi and Al Balushi19 in their studies highlighted the importance of PDA stenting as the first option in patients with PDA-dependent pulmonary circulation.
In our institute, PDA stenting is rapidly being developed. With primary repair being done at earlier age and development of PDA stenting programme, the role of BT shunt in TOF will soon be a history.
Conclusion
While the role of BT shunt in patients with TOF is decreasing due to PDA/RVOT stenting, it is likely that the BT shunt in TOF will become a thing of the past in the future even in developing countries like ours.








