CLINICAL SCENARIO
A 43-year-old female presents to the emergency department (ED) after she woke up with the sensation that the room was spinning and vomited three times at home. She continues to have significant vertigo when she presents to the ED 4 hours later. Her symptoms are worsened by head movement. She has noticed some unsteadiness but is able to walk unaided. When you examine her, she has left-beating horizontal nystagmus with a slight rotatory component to the left.
KEY CLINICAL QUESTIONS
- 1.
What are the most common causes of this presentation?
Vestibular neuritis is the most common cause, whereas a cerebellar stroke presenting with vertigo is a less common but more dangerous cause. Due to the presence of spontaneous nystagmus and her persistent significant vertigo, this is not benign paroxysmal peripheral vertigo (BPPV). Other rare but worrisome causes of vertigo include cerebellar hemorrhage and multiple sclerosis.Reference Tarnutzer, Berkowitz, Robinson, Hsieh and Newman-Toker1
- 2.
What are the stroke/central symptoms or signs you should screen this patient for?
New significant headache or neck pain would be concerning for cerebellar hemorrhage or vertebral artery dissection, respectively. Physicians should assess for the usual stroke symptoms such as facial/limb weakness or numbness, as well as posterior circulation stroke symptoms, such as dysarthria, diplopia, dysmetria, dysphonia, and dysphagia. Spontaneous vertical nystagmus, if seen, would indicate a central cause. Finally, inability to walk unaided would also be concerning for stroke.Reference Goldman and Johns2 (See Figure 1 – Approach Algorithm.)
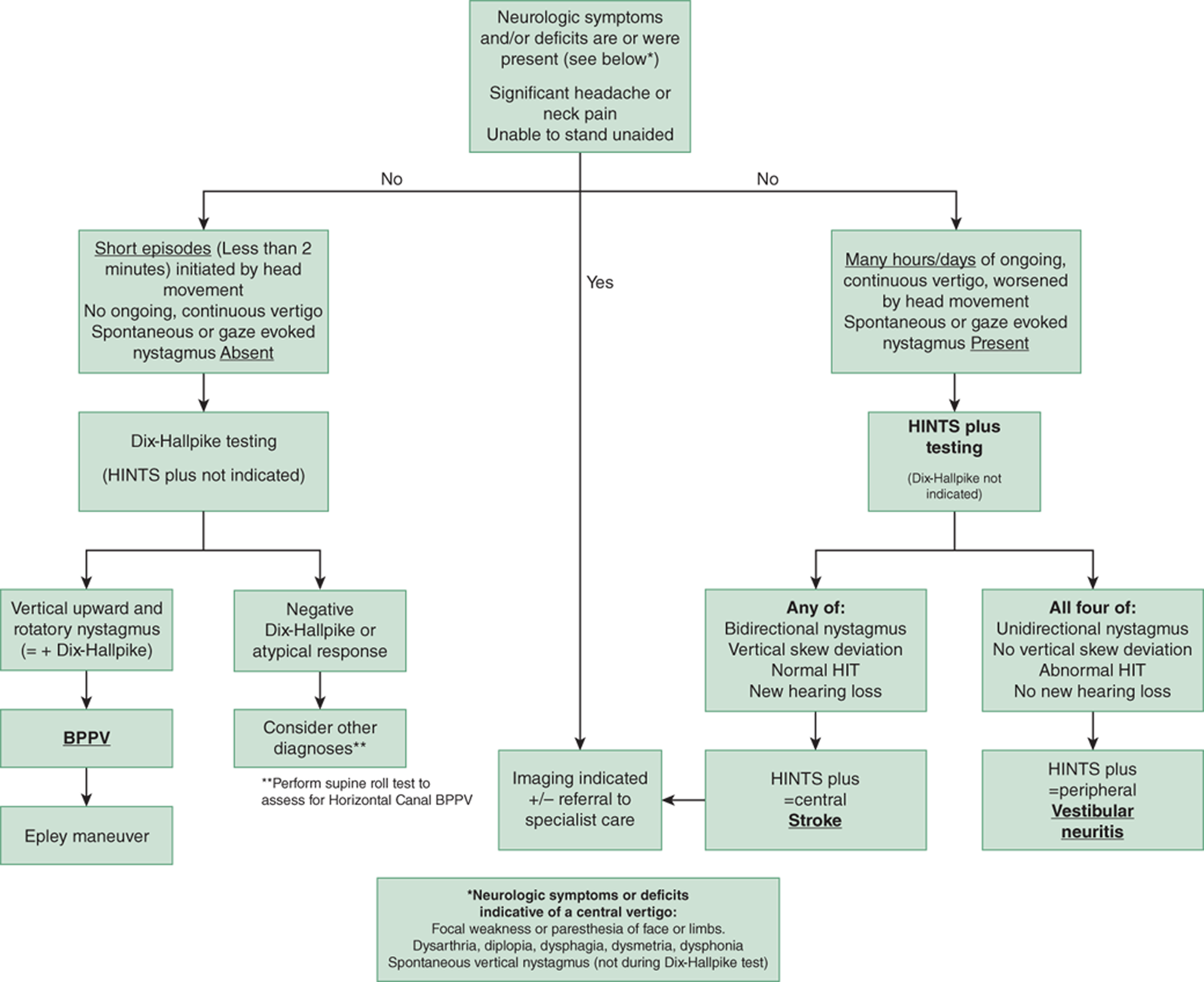
Figure 1. Algorithm approach to patients presenting with vertigo and nystagmus.
- 3.
After she has screened negative for stroke features, how can we be more certain she isn't having a cerebellar stroke that is causing her symptoms?
The HINTS plus exam is 99% sensitive and 97% specific for identifying a central cause of vertigo in patients with constant vertigo and nystagmus. Unlike commonly used stroke screening tools, such as the ABCD2 risk score, the HINTS plus exam maintains a very high sensitivity regardless of application to younger (< 60 years old) or elderly patients (up to 92 years old).Reference Newman-Toker, Kerber and Hsieh3 It should not be applied in patients unless they have both significant constant vertigo and spontaneous nystagmus.
- 4.
What is the HINTS plus exam?
The HINTS plus exam is a series of four bedside tests: nystagmus, Test of Skew, Head Impulse Test (HIT), and a bedside test of hearing. Unidirectional nystagmus, no vertical skew, an abnormal HIT, and no new hearing loss would be deemed an overall HINTS plus “peripheral” result and confirm the diagnosis of vestibular neuritis.Reference Newman-Toker, Kerber and Hsieh3 The HIT is performed by asking the patient to fixate on your nose and then rapidly moving the patient's head from 20 degrees off midline back to midline. In vestibular neuritis, one side will demonstrate an abnormal “catch-up saccade,” where the eyes will overshoot your nose and then re-fixate on your nose. This is an abnormal HIT and not seen in cerebellar strokes. Thus, the counter-intuitive finding with a normal HIT is concerning for a stroke in a patient with constant vertigo and nystagmus. (See Figure 2 – HIT Infographic.)
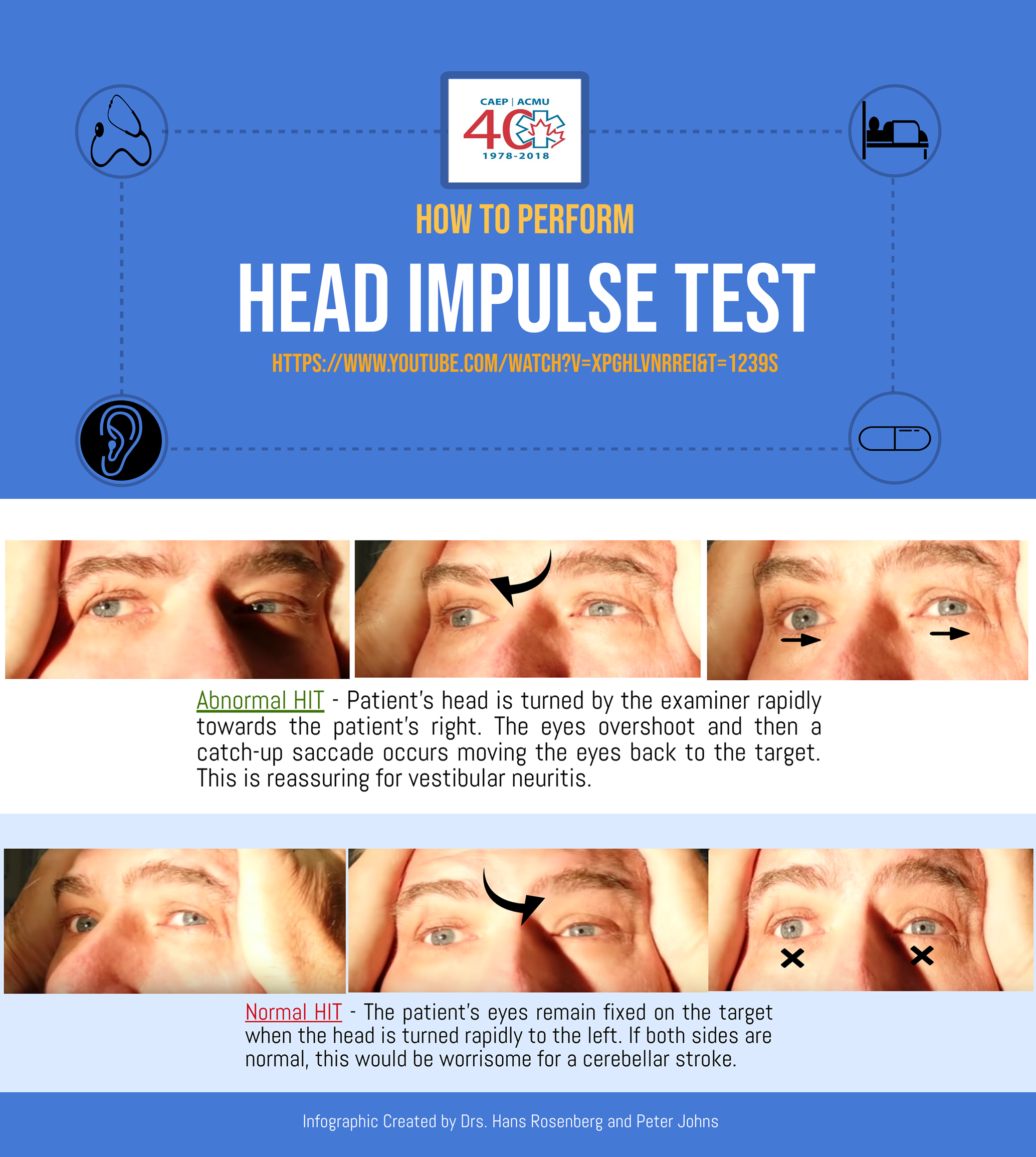
Figure 2. How to perform the head impulse test.
(Video of HINTS plus exam being performed https://youtu.be/84waYROlI4U)
(Video of HIT being performed https://www.youtube.com/watch?v=XpghlvnrREI&feature=youtu.be&t=666)
- 5.
If vestibular neuritis is confirmed, what then?
No diagnostic imaging is necessary in typical cases of vestibular neuritis with a HINTS plus “peripheral” result. Anti-emetic medications, such as metoclopramide, dimenhydrinate, or meclizine, can be used for 2 or 3 days to control nausea and vomiting. Referral to vestibular rehabilitation may hasten the recovery from vestibular neuritis. The benefit from corticosteroids in vestibular neuritis is questionable, and shared decision-making with patients regarding their use may be the best approach.Reference Fishman, Burgess and Waddell4
- 6.
If the patient had screened positive for central features or had a HINTS plus “central” result, what would be the workup?
Magnetic resonance imaging (MRI) after 48 hours is the optimal way to rule out a stroke.Reference Saber-Tehrani, Kattah and Mantokoudis5 However, if cerebellar hemorrhage is a concern due to new sustained significant headache, a plain computed tomography (CT) should be performed. If new sustained neck pain is present, a computed tomography angiogram (CTA) could be performed to rule out vertebral artery dissection. If other neurologic features are present, as outlined in question 2 above, a CTA is also warranted in these circumstances. A specialist consultation with neurology would also be necessary to determine next steps and disposition.
CASE RESOLUTION
You perform the HINTS exam and only unidirectional left-beating nystagmus is seen. The HIT is abnormal, with a prominent “catch-up” saccade when her head is turned rapidly to the right. There is no vertical skew seen. Bedside test of hearing is normal bilaterally. You do not perform a Dix-Hallpike test as the presence of spontaneous nystagmus rules out BPPV. You are confident that this patient does not have a central cause of her vertigo and this is most likely vestibular neuritis. You treat her nausea with intravenous (IV) metoclopramide and afterwards she is feeling significantly better and is discharged with a 3-day supply of metoclopramide and instructions to follow up with a local expert interested in dizzy patients.
KEY POINTS
• In patients with constant significant vertigo with nystagmus, first screen for high-risk stroke/central features that would mandate imaging and referral to specialist care.
• If the patient screens negative for stroke/central features, perform the HINTS plus exam.
• Patients who screen negative for stroke/central features and have an overall HINTS plus exam with a peripheral result can be considered for discharge with appropriate follow-up.
• Patients who screen positive for stroke/central symptoms or have an overall HINTS plus exam with a central result will need diagnostic imaging and referral to specialist care.
• An MRI obtained 48 hours after onset of symptoms is the optimal method of ruling out a suspected posterior circulation stroke. If cerebellar hemorrhage or vertebral artery dissection is a concern due to new significant headache or neck pain, a plain CT or CTA could be performed respectively.
Competing interests
None declared.




