Background
Bipolar disorder is a severe mental disorder that affects more than 1% of the population and constitutes one of the main causes of disability worldwide.Reference McIntyre, Berk, Brietzke, Goldstein, Lopez-Jaramillo and Kessing1,Reference Ferrari, Stockings, Khoo, Erskine, Degenhardt and Vos2 People with bipolar disorder exhibit markedly increased risk of premature death, with an approximately two to three times higher mortality rate relative to the general population.Reference Crump, Sundquist, Winkleby and Sundquist3–Reference Chan, Wong, Yung, Chen and Chang5 Natural causes, particularly cardiovascular diseases, respiratory diseases and cancers, are a major contributor to excess mortality associated with bipolar disorder.Reference Crump, Sundquist, Winkleby and Sundquist3–Reference Medici, Videbech, Gustafsson and Munk-Jørgensen6 Literature also consistently has found that patients with bipolar disorder have a greatly elevated rate of unnatural deaths, especially suicide, compared with the general population.Reference Crump, Sundquist, Winkleby and Sundquist3–Reference Chan, Wong, Yung, Chen and Chang5 Such mortality gap has persistedReference Crump, Sundquist, Winkleby and Sundquist3,Reference Chan, Wong, Yung, Chen and Chang5,Reference Ajetunmobi, Taylor, Stockton and Wood7 or even widenedReference Hayes, Marston, Walters, King and Osborn8–Reference Lomholt, Andersen and Sejrsgaard-Jacobsen10 in recent decades despite an overall increase in life expectancy in the general population as a result of healthcare improvements. This indicates an urgent unmet need to address physical health inequalities experienced by patients with bipolar disorder.
Most earlier studies assessed differential mortality between patients with bipolar disorder and the general population with relative measures such as standardised mortality ratio (SMR) and mortality rate ratios.Reference Hayes, Miles, Walters, King and Osborn4 An alternative approach to measure excess mortality is by estimating life expectancy and years of potential life lost (YPLL). Life expectancy is a widely used health metric referring to the number of years a person is expected to live based on the estimate of the average age at death of the standard population, although YPLL is the best-known life expectancy-related metric that denotes the difference between the observed age at death and the optimal remaining life expectancy at that age. It is acknowledged that life expectancy is an intuitive and readily understandable measure of premature mortality by quantifying the impact of diseases on survival, with more emphasis on the effect of deaths occurring at younger ages. Recently, an increasing number of studies have been conducted to examine life expectancy and YPLL for people with bipolar disorder, and mostly suggested 10–15 years shorter lifespan in patients relative to the general population.Reference Crump, Sundquist, Winkleby and Sundquist3,Reference Ajetunmobi, Taylor, Stockton and Wood7,Reference Chang, Hayes, Perera, Broadbent, Fernandes and Lee11–Reference Iturralde, Slama, Kline-Simon, Young-Wolff, Mordecai and Sterling21 Notably, thus far, there has been no study to systematically review the literature specifically for life expectancy or YPLL in people with bipolar disorder. However, a comprehensive evaluation of premature mortality quantified in terms of the magnitude of reduced lifespan associated with bipolar disorder is crucial for developing effective strategies as well as optimising resource allocation and healthcare service delivery to reduce avoidable deaths in this vulnerable population.
Aims
To this end, we conducted a systematic review and meta-analysis with an aim to provide summary estimates of life expectancy and YPLL in patients with bipolar disorder. When applicable, meta-regression models and subgroup analyses stratified by study characteristics encompassing gender, geographical region, study period and given set-age for life-expectancy estimation was performed to explore potential sources of heterogeneity. Additionally, we investigated YPLL estimates attributable to natural and unnatural deaths so as to quantify their impact on excess mortality in bipolar disorder.
Method
This study was conducted in accordance with guidelines of Meta-analysis of Observational Studies in Epidemiology (MOOSE)Reference Stroup, Berlin, Morton, Olkin, Williamson and Rennie22 and the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA;Reference Page, McKenzie, Bossuyt, Boutron, Hoffmann and Mulrow23 Supplementary Table 1 available at https://doi.org/10.1192/bjp.2022.19). The study protocol was registered with PROSPERO (CRD42021241705). As this meta-analysis was based on published data, the requirement for ethical approval was waived.
Search strategy
We systematically searched four electronic databases (Embase, Medline, PsycINFO and Web of Science) for articles published from inception to 31 March 2021. Relevant articles were searched using the following keywords: (bipolar disorder OR bipolar affective disorder OR severe mental illness OR mental disorder OR mania OR affective disorder OR mood disorder) AND (life expectancy OR lifespan OR years of potential life lost OR years of life lost OR life years OR life years lost OR survival rate OR premature mortality). The full search strategy for each database is available in Supplementary Table 2. We also checked the references of all eligible articles and relevant review articles to identify additional studies for inclusion in the meta-analysis. Two reviewers (J.K.N.C. and C.W.H.Y.T.) performed the searches independently and then compared the results. We did not apply any restrictions on language to the studies.
Inclusion criteria and study selection
Studies were included if they fulfilled the following criteria:
(a) patients aged 15 years or above with bipolar disorder diagnosed according to ICD or DSM classification (any versions) or by validated diagnostic instruments that could be mapped to ICD/DSM criteria; and
(b) reported data on life expectancy and/or YPLL for a bipolar disorder cohort relative to the general population or a comparison group without bipolar disorder.
We excluded studies that had a sample size for the bipolar disorder cohort below 50, restricted to subgroups of the population (for example homeless people, individuals who were incarcerated or elderly patients) or reported duplicate data.
Following the removal of duplicates, titles and abstracts of the identified articles were screened independently by two reviewers (J.K.N.C. and C.W.H.Y.T.) for potentially relevant studies. The full text of the publications identified at the screening stage was then evaluated independently by two reviewers (J.K.N.C. and C.W.H.Y.T.) using our selection criteria to determine the eligibility for inclusion in data synthesis, with disagreements being resolved by discussion with other members (W.C.C. and C.S.M.W.) of the research team.
Data extraction and quality assessment
Data were extracted independently by two reviewers (J.K.N.C. and C.W.H.Y.T.) from the included studies, and discrepancies were resolved by consensus. Information extracted included: first author's name, year of publication, study country and region, study design and data sources, study period, diagnostic classification system, sample size of the bipolar disorder cohort, set-age for life expectancy estimation, causes of death and estimates of life expectancy and YPLL.
In case of overlapping samples, we selected studies with reported measures of uncertainty (i.e. s.e., CIs) for life expectancy/YPLL estimates) and/or with the longest follow-up period. For natural-cause and unnatural-cause YPLLs, we calculated the mean YPLL by averaging across all YPLLs for the respective individual causes of death (for example cardiovascular diseases and respiratory diseases for natural cause deaths; suicide and accidents for unnatural cause deaths) if studies reported YPLL for specific causes of death or the weighted average if number of deaths for each specific cause of death was reported. We contacted authors to request data if estimates of life expectancy or YPLL stratified by gender and the corresponding s.e.s were not reported in the publication.
Risk of bias was assessed independently by two reviewers (J.K.N.C. and C.W.H.Y.T.) using the Newcastle–Ottawa ScaleReference Wells, Shea, O'Connell, Peterson, Welch and Losos24 to address the following three criteria: (a) selection (representativeness, selection of non-exposed cohort, ascertainment of mortality, mortality was not present at baseline), (b) comparability (study controlled for covariates), and (c) outcome (assessment of mortality, follow-up duration ≥3 years). Disagreements were resolved through consultation with other members (W.C.C. and C.S.M.W.) of the research team.
Statistical analysis
A random-effects meta-analytic model was adopted to generate a pooled estimate of life expectancy from included studies. Heterogeneity was assessed using the chi-squared Cochran's Q-test and the I2 statistic. We applied random-effects meta-regression models to explore heterogeneity for four pre-specified study characteristics including gender, geographical regions (grouped based on continents), study periods of ‘2000–2005’, ‘2006–2010’ and ‘2011–2015’ (categorised according to the middle year of cohort data collection) and the given set-age for life expectancy estimation (at birth or 15/20 years). Subgroup analyses were also conducted to examine potential sources of heterogeneity separately in each of the four pre-specified study characteristics. For studies that did not report s.e.s of life expectancy estimates, we extrapolated the pooled s.e. from those studies with reported s.e.s using a fixed-effects model.Reference Furukawa, Barbui, Cipriani, Brambilla and Watanabe25 For studies that reported CIs, we converted these to s.e.s before inclusion into the fixed-effects model. In studies that reported remaining life expectancy at a given set-age (for example 15 years), we added this age to the estimate of remaining life expectancy to obtain an expected age at death. In studies that reported multiple estimates of life expectancy using different set-ages (for example 15 years, 25 years, 35 years), life expectancy estimate derived from the youngest set-age was selected for analysis. Publication bias was examined using the funnel plot and Egger's regression asymmetry test. We performed two sets of sensitivity analyses by employing Duval and Tweedie's trim-and-fill procedureReference Duval and Tweedie26 as well as sequentially removing one study at a time (i.e. leave-one-out analysis) to evaluate the stability of results on pooled estimates of life expectancy.
For YPLL, as most included studies did not report s.e.s or CIs, we could not perform meta-analysis using the usual variance-based approaches. This also precluded us from formally quantifying heterogeneity, publication bias and statistical significance in subgroup comparison analyses. We followed the approach adopted by Hjorthøj et al (2017)Reference Hjorthøj, Stürup, McGrath and Nordentoft27 to calculate the average YPLL weighted by the size of individual study populations. The 95% CI around the weighted-average YPLL was generated using the pooled s.e. extrapolated from the studies with reported s.e.s by a fixed-effects model. Subgroup analyses stratified by gender, geographical region, study period, set-age for life expectancy estimation (at birth or 15/20 years), and cause of death (natural and unnatural cause) were performed. We conducted a sensitivity analysis by excluding a studyReference Fekadu, Medhin, Kebede, Alem, Cleare and Prince15 that was removed by the trim-and-fill procedure in the sensitivity analysis for life expectancy estimates, based on the assumption that publication bias of the included studies for investigating life expectancy and YPLL would be similar as the latter is derived from the former. Meta-analysis models were performed in R (version 4.0.2) with the metafor package. P < 0.05 was considered statistically significant.
Results
Study selection
The PRISMA flow diagram describing the process of study identification and selection is shown in Fig. 1. Literature search identified 18 412 articles, from which 16 391 remained after removal of duplicates. Upon exclusion of irrelevant studies, we retrieved 121 full-text articles to be assessed for eligibility. Of these, 108 were excluded mainly because of a lack of relevant outcomes, absence of original data or inclusion of patients without diagnosis of bipolar disorder. A total of 13 publications met inclusion criteria, with 11 articles reporting both estimates of life expectancy and YPLL, and 2 reporting YPLL only. There were five studies reporting data of overlapping samples for Denmark. Kessing et al (2015)Reference Kessing, Vradi, McIntyre and Andersen17 was selected for meta-analysis of life expectancy as it had the largest sample size and longest follow-up duration relative to other studies. Data from both Kessing et alReference Kessing, Vradi, McIntyre and Andersen17 and Weye et al (2020)Reference Weye, Momen, Christensen, Iburg, Dalsgaard and Laursen20 were included in meta-analysis of YPLL estimates because these two studies employed different methodological approaches for YPLL estimation. Kessing et alReference Kessing, Vradi, McIntyre and Andersen17 derived YPLL from life expectancy estimation based on a single fixed set-ageReference Kessing, Vradi, McIntyre and Andersen17 whereas Weye et alReference Weye, Momen, Christensen, Iburg, Dalsgaard and Laursen20 incorporated variations in age at onset of bipolar disorder (i.e. age of first-recorded diagnosis) in the life expectancy calculation.Reference Weye, Momen, Christensen, Iburg, Dalsgaard and Laursen20 Data from Laursen (2011),Reference Laursen12 Laursen et al (2013)Reference Laursen, Wahlbeck, Hallgren, Westman, Osby and Alinaghizadeh14 and Kessing et alReference Kessing, Vradi and Andersen16 for Denmark were not included in the syntheses of pooled life expectancy estimates and weighted average YPLL owing to overlapping samples, which would otherwise introduce potential bias of increased risk for type I error, but its data from Sweden and Finland were included in meta-analysis. Hence, we pooled data from 9 articles with 11 studies for life expectancy and 11 articles with 13 studies for YPLL in our meta-analyses (Table 1).
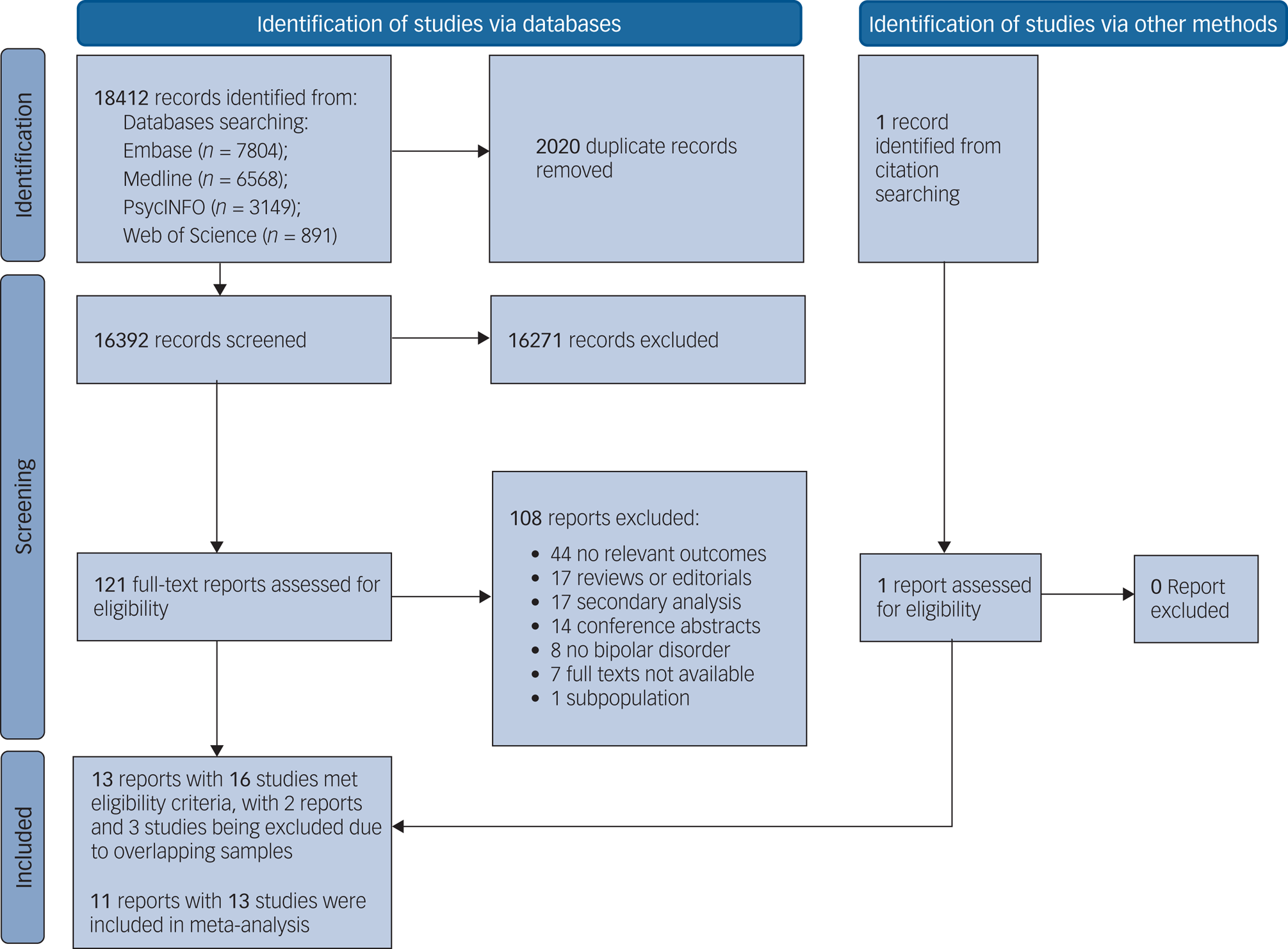
Fig. 1 PRISMA flow chart for study selection.
Table 1 Characteristics of included studies.

YPLL, years of potential life lost.
a. There were five studies reporting life expectancy and/or YPLL estimates in Denmark. Data from Kessing et al (2015)Reference Kessing, Vradi, McIntyre and Andersen17 were included in the meta-analysis of life expectancy estimates because it had the largest sample size and longest follow-up duration relative to other Danish studies. Data from both Kessing et al (2015)Reference Kessing, Vradi, McIntyre and Andersen17 and Weye et al (2020) were included in meta-analysis of YPLL estimates because these two studies adopted different methodological approaches for YPLL estimation. Data from Laursen (2011),Reference Laursen12 Laursen et al (2013)Reference Laursen, Wahlbeck, Hallgren, Westman, Osby and Alinaghizadeh14 and Kessing et al (2015)Reference Kessing, Vradi and Andersen16 for Denmark were not included in the syntheses of pooled life expectancy estimates and weighted average YPLL owing to overlapping samples.
b. Values represented life expectancy and YPLL owing to all causes of death, unless otherwise specified.
c. Calculation of the reduced remaining life expectancy in Weyes et al (2020)Reference Weye, Momen, Christensen, Iburg, Dalsgaard and Laursen20 took into consideration varying ages at onset of bipolar disorder.
Study characteristics
Overall, the current meta-analysis included 96 601 and 128 989 patients with bipolar disorder for life expectancy and YPLL estimation, respectively. Sample sizes of the included studies varied from 345 to 28 512 patients, with a median of 5096 patients. The included studies were conducted in Africa (n = 1, Ethiopia), Asia (n = 2, Taiwan and Israel), Europe (n = 4, Denmark, Finland, UK and Sweden) and North America (n = 1, USA). For most studies, patient samples were identified via case registers from the healthcare system. One study used a health insurance case register to identify patients with bipolar disorder,Reference Pan, Yeh, Chan and Chang18 and another study adopted community survey screening followed by diagnostic confirmation using semi-structured interview.Reference Fekadu, Medhin, Kebede, Alem, Cleare and Prince15
Diagnosis of bipolar disorder in all of the included studies was based on ICD criteria. All but one studies examined the life expectancy and YPLL of patients with bipolar disorder relative to that of the general population. Crump et al (2013)Reference Crump, Sundquist, Winkleby and Sundquist3 estimated life expectancy and YPLL for people with bipolar disorder by comparing them with the general population without bipolar disorder. Follow-up duration ranged from 3 to 16 years, with a median of 8 years. There were nine studies reporting gender-specific estimates for life expectancy and ten for YPLL. Characteristics of the included studies are presented in Table 1.
Meta-analysis of life expectancy
Figure 2 summarises life expectancy estimates for patients with bipolar disorder in individual studies. The pooled life expectancy was 66.88 years (95% CI 64.47–69.28). Significant heterogeneity was observed across studies (Q = 27 423, P < 0.001, I2 = 99.9%). There was publication bias as indicted by visual inspection of the funnel plot (i.e. asymmetry) and result of Egger's test (z = −2.3, P = 0.024; Supplementary Fig. 1). Sensitivity analysis using the trim-and-fill procedure, with an outlier studyReference Fekadu, Medhin, Kebede, Alem, Cleare and Prince15 being removed from the meta-analysis, yielded a pooled life expectancy of 67.44 years (65.20–69.67) and Egger's test became statistically non-significant (z = –0.9, P = 0.380; Supplementary Fig. 2). The pooled life expectancy estimates did not differ significantly from each other when one study was omitted at a time (data not shown).
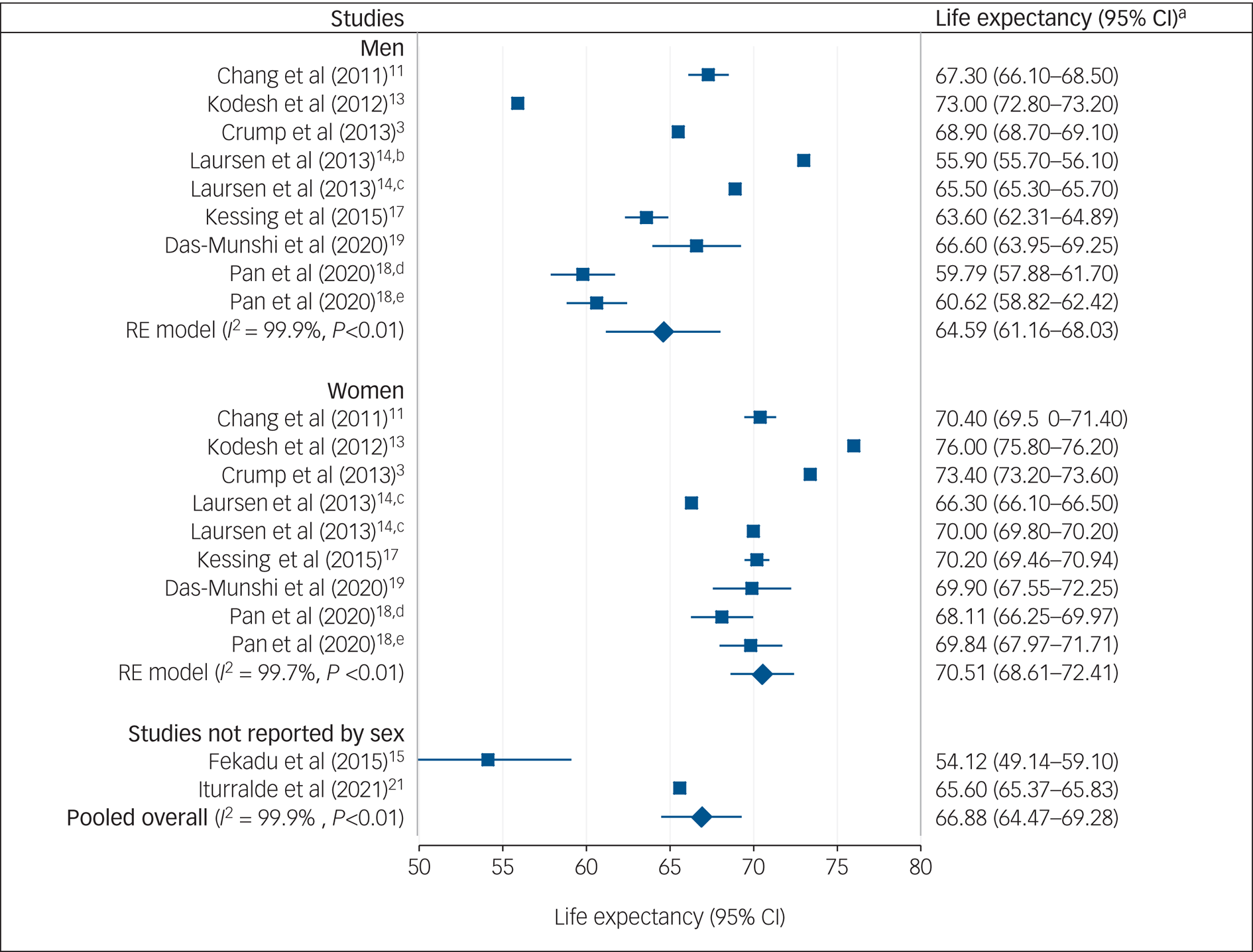
Fig. 2 Meta-analysis on life expectancy in bipolar disorder.
a. Unreported variance was extrapolated from studies with reported s.e.s including Chang et al (2011),Reference Chang, Hayes, Perera, Broadbent, Fernandes and Lee11 Fekadu et al (2015),Reference Fekadu, Medhin, Kebede, Alem, Cleare and Prince15 Kessing et al (2015),Reference Kessing, Vradi, McIntyre and Andersen17 Pan et al (2020),Reference Pan, Yeh, Chan and Chang18 Das-munshi et al (2020)Reference Das-munshi, Chang, Dragon, Hatch, Morgan and Thornicroft19 and Iturralde et al (2021).Reference Iturralde, Slama, Kline-Simon, Young-Wolff, Mordecai and Sterling21 b. Data from cohort in Finland in Laursen et al (2013)Reference Laursen, Wahlbeck, Hallgren, Westman, Osby and Alinaghizadeh14 is presented. c. Data from cohort in Sweden in Laursen et al (2013)Reference Laursen, Wahlbeck, Hallgren, Westman, Osby and Alinaghizadeh14 is presented. d. Data from the 2005 cohort in Pan et al (2020)Reference Pan, Yeh, Chan and Chang18 is presented. e. Data from 2010 cohort in Pan et al (2020)Reference Pan, Yeh, Chan and Chang18 is presented. RE, random effect.
Subgroup and meta-regression analyses of life expectancy
Subgroup analyses stratified by gender demonstrated that life expectancy was significantly lower in men (64.59 years (95% CI 61.16–68.03)) than women with bipolar disorder (70.51 years (95% CI 68.61–72.41); z = 2.00, P = 0.003).
Comparison among geographical regions showed that life expectancy was lowest in Africa (54.12 years (95% CI 42.79–65.45)), which was significantly lower than that in Asia (67.97 years (95% CI 63.76–72.17); z = 2.24, P = 0.025) and in Europe (67.33 years (95% CI 64.37–70.29); z = 2.21, P = 0.027) but did not significantly differ from that in North America (65.60 years (95% CI 55.42–75.78); z = 1.48, P = 0.140; Fig. 3).

Fig. 3 Subgroup analysis of pooled life expectancy stratified by geographical regions.
When findings were stratified by study period, life expectancy was lowest in 2000–2005 (62.71 years (95% CI 58.21–67.21)), which was significantly lower than that in 2006–2010 (69.12 years (95% CI 65.98–72.25); z = 2.29, P = 0.022) but not 2011–2015 (66.49 years (95% CI 62.00–70.98); z = 1.2, P = 0.245; Supplementary Fig. 3). No significant difference was observed for subgroup analyses according to set-age for life expectancy estimation (at birth: 66.43 years (95% CI 63.53–69.32); at 15/20 years: 67.57 years (95% CI 63.71–71.42); z = 0.46, P = 0.645).
Univariate meta-regression analyses revealed that the life-expectancy estimate was significantly associated with gender (Qm = 8.6, P = 0.003), but not geographical regions (Qm = 5.27, P = 0.153), study periods (Qm = 5.3, P = 0.071) or set-ages for the life-expectancy calculation (Qm = 0.21, P = 0.645).
A multivariate meta-regression model accounting for all of these four pre-specified study variables explained 45.9% of the variance (Qm = 22.7, P = 0.002), indicating that there was residual variance because of heterogeneity in life-expectancy estimates.
Meta-analysis and subgroup analyses of YPLL
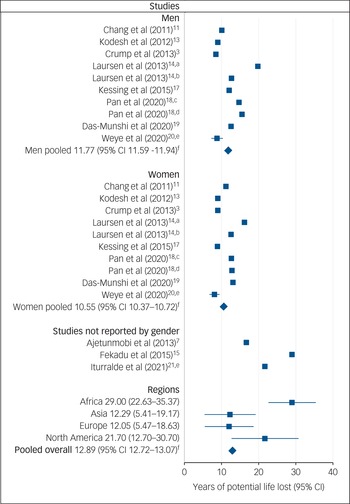
As shown in Fig. 4, the weighted average YPLL of patients with bipolar disorder was 12.89 years (95% CI 12.72–13.07). Sensitivity analysis with removal of a studyReference Fekadu, Medhin, Kebede, Alem, Cleare and Prince15 that contributed to publication bias in the life-expectancy estimate yielded a similar result of YPLL (12.85 years (95% CI 12.68–13.03)).

Fig. 4 Meta-analysis of years of potential life lost (YPLL) in bipolar disorder.
a. Data from cohort in Finland in Lauren et al. (2013)Reference Laursen, Wahlbeck, Hallgren, Westman, Osby and Alinaghizadeh14 is presented. b. Data from cohort in Sweden in Lauren et al (2013)Reference Laursen, Wahlbeck, Hallgren, Westman, Osby and Alinaghizadeh14 is presented. c. Data from 2005 cohort in Pan et al (2020)Reference Pan, Yeh, Chan and Chang18 is presented. d. Data from 2010 cohort in Pan et al (2020)Reference Pan, Yeh, Chan and Chang18 is presented. e. All of the included studies, except Weye et al (2020)Reference Weye, Momen, Christensen, Iburg, Dalsgaard and Laursen20 and Iturralde et al (2021),Reference Iturralde, Slama, Kline-Simon, Young-Wolff, Mordecai and Sterling21 did not report variance of YPLL estimates. The 95% CIs for YPLL estimates in Weye et al (2020)Reference Weye, Momen, Christensen, Iburg, Dalsgaard and Laursen20 were 7.26–10.34 (men) and 6.76–9.44 (women), and in Iturralde et al (2021)Reference Iturralde, Slama, Kline-Simon, Young-Wolff, Mordecai and Sterling21 was 21.52–21.88 for both men and women combined. f. Variance around the pooled estimates was extrapolated from studies with reported s.e.s including Weye et al (2020)Reference Weye, Momen, Christensen, Iburg, Dalsgaard and Laursen20 and Iturralde et al (2021).Reference Iturralde, Slama, Kline-Simon, Young-Wolff, Mordecai and Sterling21
Subgroup analyses stratified by gender showed a slightly greater YPLL in men (11.77 years (95% CI 11.59–11.94)) than women with bipolar disorder (10.55 years (95% CI 10.37–10.72)).
Concerning geographical regions, YPLL was greatest in Africa (29.00 years (95% CI 22.63–35.37)), followed by North America (21.70 years (95% CI 12.70–30.70)). Studies from Asia (12.29 years (95% CI 5.41–19.17)) and Europe (12.05 years (95% CI 5.47–18.63)) reported comparatively less YPLL.
Subgroup analyses stratified by study period found that the YPLL estimate in 2000–2005, 2006–2010 and 2011–2015 was 17.71 years (95% CI 17.53–17.88), 12.76 years (95% CI 12.59–12.94) and 12.71 years (95% CI 12.54–12.89), respectively (Supplementary Fig. 4).
For studies with YPLL estimated at birth, the weighted average YPLL was 16.88 years (95% CI 16.70–17.05). For studies with YPLL estimated at other given set-age (15/20 years), the weighted average YPLL was 12.25 years (95% CI 12.07–12.43).
Natural and unnatural causes of death contributed to 5.94 years (95% CI 5.81–6.07) and 5.69 years (95% CI 5.59–5.79) of weighted average YPLL, respectively (Fig. 5).

Fig. 5 Meta-analysis on years of potential life lost (YPLL) in bipolar disorder owing to natural and unnatural causes.
a. All of the included studies, except Weye et al (2020),Reference Weye, Momen, Christensen, Iburg, Dalsgaard and Laursen20 did not report variance of natural-cause and unnatural-cause YPLL estimates. In Weye et al (2020)Reference Weye, Momen, Christensen, Iburg, Dalsgaard and Laursen20, the 95% CI of natural-cause YPLL estimate was 3.43–3.95 (men) and 4.64–5.04 (women), and of unnatural-cause YPLL estimate was 4.93–5.31 (men) and 2.30–2.56 (women). b. Variance around the pooled estimates was extrapolated from studies with reported s.e.s including Weye et al (2020)Reference Weye, Momen, Christensen, Iburg, Dalsgaard and Laursen20 and Iturralde et al (2021).Reference Iturralde, Slama, Kline-Simon, Young-Wolff, Mordecai and Sterling21
Assessment of study quality
Of the 11 studies included in the meta-analysis, eight studies were rated as of good qualityReference Crump, Sundquist, Winkleby and Sundquist3,Reference Chang, Hayes, Perera, Broadbent, Fernandes and Lee11,Reference Kodesh, Goldshtein, Gelkopf, Goren, Chodick and Shalev13,Reference Laursen, Wahlbeck, Hallgren, Westman, Osby and Alinaghizadeh14,Reference Kessing, Vradi, McIntyre and Andersen17–Reference Weye, Momen, Christensen, Iburg, Dalsgaard and Laursen20 and three studies were judged to be of fair quality.Reference Ajetunmobi, Taylor, Stockton and Wood7,Reference Fekadu, Medhin, Kebede, Alem, Cleare and Prince15,Reference Iturralde, Slama, Kline-Simon, Young-Wolff, Mordecai and Sterling21 Failure to adjust for gender as a covariate was the most common methodological omission. Details of the quality assessment for individual studies are presented in Supplementary Table 3.
Discussion
Main findings and interpretation
To our knowledge, this is the first meta-analysis examining life expectancy and YPLL in people with bipolar disorder. Our main analyses showed that patients with bipolar disorder experienced reduced life expectancy relative to the general population, with approximately 13 years of potential life lost. Consistent pooled estimates of life expectancy were observed in sensitivity analyses correcting for publication bias and using the leave-one-out method, indicating that our synthesised results were stable and robust. Significant heterogeneity was detected across studies for life-expectancy estimates, and was partly explained by gender and study period. However, as most included studies examining YPLL did not report measures of uncertainty (i.e. s.e.s or CIs), level of heterogeneity (and statistical difference in subgroup comparison analyses) for YPLL could not be quantified in our meta-analysis.
Compared with an earlier meta-analysis for schizophrenia, our results suggest that patients with bipolar disorder have fewer years of life lost that those with schizophrenia (weighted average YPLL of 14.5 years).Reference Hjorthøj, Stürup, McGrath and Nordentoft27 More recent data from Danish case-register researchReference Plana-Ripoll, Pedersen, Agerbo, Holtz, Erlangsen and Canudas-Romo28,Reference Plana-Ripoll, Musliner, Dalsgaard, Momen, Weye and Christensen29 also revealed that bipolar disorder was associated with a smaller life-expectancy gap than substance/alcohol use disorders and schizophrenia. Nonetheless, patients with bipolar disorder were in general found to display a greater reduction in lifespan (relative to the general population) than those with common mental disorders including depressive and anxiety disorders.Reference Weye, Momen, Christensen, Iburg, Dalsgaard and Laursen20,Reference Plana-Ripoll, Pedersen, Agerbo, Holtz, Erlangsen and Canudas-Romo28
Our gender-stratified analyses demonstrated that life expectancy was significantly lower in men with bipolar disorder than in women with bipolar disorder, whereas slightly more years of potential life were lost for men (11.77 years) than for women (10.55 years) with the disorder. We also observed regional differences in life expectancy for bipolar disorder. Patients in the African study exhibited the shortest lifespan (54.12 years), whereas life expectancy was highest in Asia and Europe. Similarly, the greatest YPLL was noted in Africa (29.00 years), and YPLL was least (around 12 years) in Asia and Europe. Our results might in fact partly reflect cross-regional differences in the distribution for life expectancy in the general population,30 particularly in Africa.
Differences in access to and quality of healthcare services and lifestyle factors might also contribute to the variations in life expectancy across regions. In this context, regional variations in YPLL, which indicates difference in lifespan between patients and the general population, would provide more informative cross-regional comparisons. Of note, our findings of regional differences should be treated with caution as all of the continents reported in this meta-analysis except Europe were represented by one or two studies only. Moreover, data from the African study was based on a small sample size (n = 345).Reference Fekadu, Medhin, Kebede, Alem, Cleare and Prince15
Alternatively, patients with bipolar disorder had significantly increased lifespan from the period of ‘2000–2005’ to ‘2006–2010’ (from 62.71 years to 69.12 years). We also found a reduced YPLL of around 5 years across the study periods in patients with bipolar disorder. This seems to be contrary to the findings of most previous individual studies that assessed SMR (primarily on an annual basis) for bipolar disorder and indicated persistentReference Crump, Sundquist, Winkleby and Sundquist3,Reference Chan, Wong, Yung, Chen and Chang5,Reference Ajetunmobi, Taylor, Stockton and Wood7 or even a widening mortality gapReference Hayes, Marston, Walters, King and Osborn8–Reference Lomholt, Andersen and Sejrsgaard-Jacobsen10 in recent decades. However, our analysis comparing life-expectancy/YPLL estimates of three discrete study periods might be limited by the fact that these periods were categorised according to the middle year of cohort data collection per study irrespective of the length of follow-up and only a small number of studies were included in each of the three study periods. Additionally, studies included in the current meta-analysis had an overall observation period spanning 16 years only (from 2000 to 2015), which might be too short to capture actual temporal trends in life expectancy or YPLL but instead reflected short-term fluctuations. Conversely, life expectancy estimated at birth did not differ significantly from that based on another given set-age (i.e. 15 or 20 years), whereas approximately 5 more years of potential life were lost in patients whose life expectancy was calculated at birth (16.88 years) than at 15/20 years of age (12.25 years).
Causes of death
Subgroup analyses on YPLL stratified by causes of death showed that both natural and unnatural causes contributed to around 6 years of life lost among patients with bipolar disorder. Previous research has in fact consistently found that bipolar disorder is associated with an increased prevalence of physical comorbidity.Reference Crump, Sundquist, Winkleby and Sundquist3,Reference Laursen, Munk-Olsen and Gasse31–Reference Forty, Ulanova, Jones, Jones, Gordon-Smith and Fraser33 Excess mortality by natural causes in bipolar disorder could be attributable to a multitude of factors including unhealthy lifestyle such as sedentary behaviours,Reference Vancampfort, Firth, Schuch, Rosenbaum, Mugisha and Hallgren34 smokingReference Heffner, Strawn, DelBello, Strakowski and Anthenelli35 and alcohol use, antipsychotic-induced metabolic side-effects,Reference Correll, Joffe, Rosen, Sullivan and Joffe36 and inequitable medical care.Reference Smith, Martin, McLean, Langan, Guthrie and Mercer32,Reference Laursen, Mortensen, MacCabe, Cohen and Gasse37,Reference Heiberg, Nesvåg, Balteskard, Bramness, Hultman and Naess38 The link between bipolar disorder and increased physical morbidity and mortality may also be explained by the presence of common aetiological factors including shared genetic susceptibilityReference Amare, Schubert, Klingler-Hoffmann, Cohen-Woods and Baune39 and overlapping pathophysiological mechanisms such as inflammatory dysregulation.Reference SayuriYamagata, Brietzke, Rosenblat, Kakar and McIntyre40
Our results also highlighted the significant impact of unnatural deaths on reduced life expectancy in bipolar disorder. This concurs with a recent meta-analysis revealing that patients with bipolar disorder had a seven-fold elevated risk of unnatural cause mortality, as measured by SMR, relative to the general population.Reference Hayes, Miles, Walters, King and Osborn4 Although the data from the included studies did not permit us to further quantify the contribution of specific unnatural causes to YPLL, substantial evidence has indicated that suicide is the predominant cause of unnatural deaths in patients with bipolar disorder whose suicide risk is 20- to 30-fold greater than that of the general population.Reference Plan, Barrot, Nieto, Rios, Schulze and Papiol41
Implications
Findings from the current meta-analysis have several important clinical and research implications. Our results that bipolar disorder is associated with markedly shortened life expectancy underscores substantial unmet therapeutic needs for people with the disorder. Given that YPLLs for natural and unnatural causes are of similar magnitude, both physical health and suicide risk (as a major contributor to unnatural deaths) should be adequately addressed in order to significantly reduce the longevity gap for bipolar disorder. A multilevel intervention framework managing risk factors at the individual, health system and socio-environmental levelsReference Liu, Daumit, Dua, Aquila, Charlson and Cuijpers42 should be implemented to reduce excess mortality because of physical diseases, such as lifestyle modification, early detection and equitable treatment of physical morbidity, guideline-concordant monitoring of medication-induced metabolic side-effects, and coordinated delivery of mental and physical healthcare.
Concerning suicide prevention, early intervention for bipolar disorder, with regular systematic suicide risk assessment for early identification and prompt management of high-risk patients should be incorporated in clinical practice. This is based on the premise that suicide risk is highest during the early course of bipolar disorder,Reference Crump, Sundquist, Winkleby and Sundquist3,Reference Medici, Videbech, Gustafsson and Munk-Jørgensen6 and accumulating evidence suggests that intervention in the early illness stage is more effective than in later stages for outcome improvement,Reference Joyce, Thompson and Marwaha43 which in turn lowers recurrence and suicide rates. In addition, lithium, which has a well-documented anti-suicidal effectReference Del Matto, Muscas, Murru, Verdolini, Anmella and Fico44 and is recommended as a first-line agent for acute mania and maintenance treatment of bipolar disorder, should be considered as a treatment option for patients at high-risk of suicide.
YPLL assesses the impact of premature mortality on survival based on estimating life expectancy at a single fixed age (mostly at birth or 15 years). This approach, however, does not reflect the underlying age-at-onset distribution of the disorder. Recent research has indicated that life-years lost (LYL),Reference Andersen45 a novel health metric, may represent a more realistic measure of reduced life expectancy by taking into consideration the variations in age at illness onset in lifespan estimation.Reference Plana-Ripoll, Pedersen, Agerbo, Holtz, Erlangsen and Canudas-Romo28,Reference Erlangsen, Andersen, Toender, Laursen, Nordentoft and Canudas-Romo46 In fact, several studies on bipolar disorder or schizophrenia demonstrated that the magnitude of life expectancy gap between patients and the general population was influenced by the set-age for lifespan calculation, with life expectancy gap decreased with increasing set-age.Reference Kessing, Vradi and Andersen16,Reference Leng, Chou, Lin, Yang and Wang47 Our subgroup analyses also revealed similar findings that life expectancy estimated at 15/20 years yielded less YPLL than that calculated at birth. Thus, adoption of the LYL method should be considered in future studies on bipolar disorder so as to provide more accurate quantification of reduced life expectancy.
Limitations
Several limitations warrant consideration in interpreting the study results. First, the current meta-analysis was based on a relatively limited number of studies (n = 13). Notably, life expectancy and YPLL are much less studied compared with relative risk measures for mortality (such as SMR) in bipolar disorder. Hence, findings about life expectancy and YPLL for people with bipolar disorder should be comprehensively re-evaluated when more studies have been conducted in this respect. This will also minimise potential bias in assessing sources of heterogeneity, for instance, by including a broader representation of geographical regions.
Second, as several studies on life expectancy and most studies on YPLL in people with bipolar disorder did not report measures of uncertainty, we extrapolated the pooled s.e. from the fixed-effect models from these studies to derive 95% CIs of our summary estimates of life expectancy and YPLL. This might, however, compromise the accuracy of the true variance.
Third, the unavailability of s.e.s or CIs for YPLL in most of the included studies precluded us from formally quantifying heterogeneity and publication bias in our meta-analysis for YPLL.
Fourth, only a small number of studies have examined YPLL for specific causes of death, thus we were not able to generate pooled estimates of cause-specific YPLLs.
Fifth, there was significant heterogeneity among studies for life-expectancy estimates, and it could not be fully accounted for by the pre-specified study characteristics, thereby indicating the presence of other unidentified factors. Nonetheless, as data for other potentially relevant variables such as socioeconomic status and deprivation, prescription of psychotropic medications and lifestyle risk factors were not reported in most included studies, sources of heterogeneity could not be further explored in the current meta-analysis. This also precludes us from clarifying and quantifying the impact of individual risk factors on excess mortality in people with bipolar disorder.
Sixth, given that all of the included studies did not differentiate patient cohorts into disorder subtypes for analysis, potential difference between people with bipolar I and II disorders in these health metrics could not be examined.
In conclusion, this meta-analysis indicates that bipolar disorder is associated with reduced life expectancy, with around 13 years of life lost relative to the general population. Men with bipolar disorder have a shorter lifespan than women with the disorder. A comparable degree of contribution from natural and unnatural deaths to YPLL for bipolar disorder highlights the importance of developing and implementing a comprehensive and multipronged interventional approach, particularly in the early course of illness, to effectively promote physical health and lower suicide risk, with consequent reduction of premature mortality.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1192/bjp.2022.19.
Data availability
The data that support the findings of this study are available from the corresponding author (W.C.C.) upon reasonable request.
Author contributions
W.C.C. and J.K.N.C. conceived and designed the study. J.K.N.C. and C.H.Y.T. did the literature search, selection of the studies, quality assessment and data extraction. J.K.N.C. performed statistical analysis and drafted the manuscript. C.S.M.W. supervised the processes for study selection and data synthesis. W.C.C. revised and finalised the manuscript. All authors interpreted the data, critically reviewed and approved the final version of the manuscript.
Funding
The study was supported by the Hong Kong Research Grants Council (17125820). The funder of the study had no role in study design, data extraction and analysis, decision to publish or preparation of the manuscript.
Declaration of interest
The authors declared no conflicts of interest in relation to the subject of this study.









eLetters
No eLetters have been published for this article.