Psychological treatments for psychosis, particularly cognitive–behavioural therapy (CBT), have been shown to be effective in patients with chronic treatment-resistant psychosis and recent-onset psychosis (Reference Lewis, Tarrier and HaddockLewis et al, 2002; Reference Cormac, Jones and CampbellCormac et al, 2004). However, evaluations of psychological treatments have not usually examined outcomes in relation to a particular patient age group, even though people of different ages may have different therapeutic needs. For example, young adults may have significant developmental issues which may need to be taken into account when developing and delivering treatments. The aim of this study was to evaluate the interaction between age and symptomatic and functioning outcomes in a randomised controlled trial designed to evaluate the effectiveness of CBT and supportive counselling plus treatment as usual compared with treatment as usual alone in first- and second-episode patients with schizophrenia (the Study of Cognitive Reality Alignment Therapy in Early Schizophrenia (SoCRATES) trial).
METHOD
The study design was a multi-centre, prospective, rater-masked, randomised controlled trial with an 18-month follow-up. Eligible patients were randomly allocated to one of three treatments, namely CBT and treatment as usual, supportive counselling and treatment as usual, or treatment as usual alone. Phase 1 of the study presented the recovery data for the first 70 days (Reference Lewis, Tarrier and HaddockLewis et al, 2002). Patients were then followed up and re-assessed by psychiatric interview and examination of hospital records and case notes 18 months after randomisation (Reference Tarrier, Lewis and HaddockTarrier et al, 2004). A detailed description of the entire SoCRATES sample and methodology has been provided (Reference Lewis, Tarrier and HaddockLewis et al, 2002), so will be only briefly described here.
Participants, recruitment and assignment
Participants were recruited over a period of 26 months. Inclusion criteria for entry to the trial were as follows: either first or second admission (within 2 years of a first admission) to in-patient or day-patient unit for treatment of psychosis; DSM–IV criteria for schizophrenia, schizophreniform disorder, schizoaffective disorder, delusional disorder or psychosis not otherwise specified (American Psychiatric Association, 1994); positive psychotic symptoms for 4 weeks or more; a score of 4 or more on the Positive and Negative Syndrome Scale (PANSS) (Reference Kay, Opler and LindenmayerKay et al, 1989) target item for either delusions (P1) or hallucinations (P3); neither substance misuse nor organic disorder judged to be the main cause of psychotic symptoms.
Assessment measures
A number of assessment measures were employed as part of the SoCRATES study at baseline and during the 18-month follow-up period (Reference Lewis, Tarrier and HaddockLewis et al, 2002; Reference Tarrier, Lewis and HaddockTarrier et al, 2004). However, only the following measures will be reported here. Measures of symptoms and functioning at baseline and follow-up included the PANSS (Reference Kay, Opler and LindenmayerKay et al, 1989) total, positive, negative and general sub-scale scores, the Psychotic Symptom Rating Scales (PSYRATS; Reference Haddock, McCarron and TarrierHaddock et al, 1999a ), the Social Functioning Scale (SFS; Reference Birchwood, Smith and CochraneBirchwood et al, 1990), the Birchwood Insight Scale (BIS; Reference Birchwood, Smith and DruryBirchwood et al, 1994) and two measures of therapeutic alliance, namely the California Therapeutic Alliance Scales (CALPAS; Reference GastonGaston, 1990) and the Psychotherapy Status Report (PSR; Reference Frank and GundersonFrank & Gunderson, 1990). Data on demographics, substance use and duration of untreated psychosis were also collected at baseline.
Intervention groups
The interventions were based on those evaluated in previous treatment studies (Reference Tarrier, Yusopoff and KinneyTarrier et al, 1998; Reference Haddock, Tarrier and MorrisonHaddock et al, 1999b ). The CBT was manual-based and was undertaken by five therapists trained in CBT for psychosis, who were supervised by experienced cognitive–behavioural therapists. At the beginning of the study the therapists were trained in both interventions, and throughout the study they received separate expert and peer supervision on a regular basis to maintain treatment quality. The aim was for a ‘treatment envelope’ of 15–20 hours within a 5-week post-admission period, plus ‘booster’ sessions after a further 2 weeks, and after 1, 2 and 3 months. Details of the CBT have been provided by Haddock et al (Reference Haddock, Tarrier and Morrison1999b ). Supportive counselling was used as a comparison intervention to control for non-specific elements of therapist exposure. The same five research therapists administered both CBT and supportive counselling interventions, according to randomisation. All treatment sessions, both for CBT and for supportive counselling, were audiotaped if participants had given their consent, and the treatment fidelity as judged by independent, expert raters was good (Reference Lewis, Tarrier and HaddockLewis et al, 2002).
Analysis
Baseline data were compared according to age using a cut-off point of age 21 years (i.e. ‘over 21’ and ‘21 years and under’). This cut-off was considered to be a pragmatic developmental point at which to divide the groups. It also allowed sufficient numbers of participants in both groups to ensure that the appropriate comparisons could be made. Comparisons were performed using analyses of variance following assessment of the normality of the data. Data on duration of untreated psychosis were analysed using a Mann–Whitney U-test. Analysis of covariance was performed to assess the effects of therapy on symptom and functioning outcomes of the PANSS, PSYRATS and SFS according to age group. The dependent variables were the 3- and 18-month outcome scores, with baseline scores and logged duration of untreated psychosis as covariates. Therapy group, centre and age group were fixed factors. All of the data were analysed using SPSS version 10 for Windows.
RESULTS
Seventy-one patients from the total sample of 309 participants were aged 21 years or less. Table 1 shows the characteristics of the sample by age, and demonstrates that most of the patients in the sample were male and were experiencing their first episode of psychosis. Approximately one-third of the patients were detained under the Mental Health Act 1983. The diagnostic category is also shown. There were no significant differences between the two age groups on any of these variables. A higher proportion of the patients aged 21 years or under were misusing substances on a daily basis compared with the older group (33% ν. 25%). However, an analysis of variance performed on the total sample revealed that there were no significant differences in baseline, 3- or 18-month PANSS total scores between daily substance misusers and those who were infrequent or non-misusers, although there was a non-significant trend for the substance misusers to have poorer PANSS total scores at baseline (P=0.064). Duration of untreated psychosis also differed between the age groups, with median values of 8 weeks (range 2–100) and 12 weeks (range 0–624) for the younger and older age groups respectively (Mann–Whitney U-test=6260.5, P=0.002). The duration of untreated psychosis was calculated according to an algorithm based on accounts from patients, staff, notes and (where practicable) relatives. The most conservative estimate was used for each source, with the longest estimate and patient account being given most weight provided that they were consistent with external evidence (Reference Drake, Haley and AkhtarDrake et al, 2000).
Table 1 Demographic and diagnostic descriptions of the sample

| Group aged ≤21 years | Group aged >21 years | |
|---|---|---|
| Sample size, n | 71 | 233 |
| Age, years: mean (s.d.) | 19.6 (1.6) | 32.9 (9.9) |
| Males, % | 77 | 68 |
| Detained under mental health act, % | 39 | 37 |
| First-episode psychosis, % | 87 | 83 |
| Mean number of years of education | 11.1 | 11.8 |
| Diagnostic category | ||
| Schizophreniform disorder, n | 41 | 67 |
| Schizophrenia, n | 18 | 102 |
| Schizoaffective disorder, n | 9 | 30 |
| Delusional disorder, n | 1 | 24 |
| Psychosis not otherwise specified, n | 2 | 10 |
| Self-reported daily/weekly substance misuse, % | 33 | 25 |
Birchwood Insight Scale scores did not differ significantly between the two groups.
Symptom outcomes
Baseline
Baseline data for the PANSS, PSYRATS, SFS and BIS for the two age groups are shown in Table 2. It can be seen that the younger age group had significantly higher PANSS total, PANSS negative and PANSS general sub-scale scores at baseline compared with the older group (F(1,301)=6.72, P=0.01; F(1,301)=5.90, P=0.016; F(1,301)=5.51, P=0.02, respectively). Although there were no significant differences in total PSYRATS scores at baseline, analysis of the individual items of the PSYRATS revealed that the younger group reported a higher proportion of distressing content in their delusions than the older group (F(1,300)=4.38, P=0.037).
Table 2 Baseline data for symptom, functioning and insight scales

| Group aged ≤21 years | Group aged >21 years | P | |
|---|---|---|---|
| PANSS total sub-scale | 92.6 | 86.6 | 0.001 |
| PANSS positive sub-scale | 24.1 | 23.1 | NS |
| PANSS general sub-scale | 47.6 | 44.7 | 0.02 |
| PANSS negative sub-scale | 20.9 | 18.8 | 0.016 |
| PSYRATS delusions sub-scale | 18.3 | 17.3 | NS |
| PSYRATS hallucinations sub-scale | 16.6 | 17.6 | NS |
| SFS total scale | 108.1 | 119.4 | 0.04 |
| SFS performance sub-scale | 25.8 | 29.3 | 0.017 |
| SFS competence sub-scale | 22.4 | 27.4 | 0.001 |
| BIS | 9.2 | 9.7 | NS |
Follow-up
The number of sessions of therapy received was similar for the two age groups, with participants aged 21 or under receiving an average of 13.5 sessions and the older age group receiving an average of 13.8 sessions. However, there was a significant difference in the response to treatment between the two age groups as rated on the PANSS positive sub-scale (F(2,210)=3.21, P=0.043), the PANSS general sub-scale (F(2,210)=3.01, P=0.051) and PSYRATS delusions sub-scale at 3 months (F(2,197)=3.00, P=0.052), and as rated on the PANSS general sub-scale at 18 months (F(2,218)=3.12, P=0.046). There was also a trend towards a significantly different response according to age at 18 months on the PANSS total sub-scale (F(2,217)=2.47, P=0.087) and the PANSS positive sub-scale (F(2,218)=2.39, P=0.094).
Both psychological treatments were analysed independently with treatment as usual and with each other according to age. This revealed significant interactions between supportive counselling and treatment as usual by age group for PANSS positive sub-scale scores (F(1,134)=4.24, P=0.042) and PSYRATS delusions sub-scale scores (F(1,129)=4.57, P=0.035) at 3 months, and for PANSS general scores (F(1,145)=3.99, P=0.048) at 18 months. There was also a significant interaction between therapy and age group when CBT and supportive counselling were compared on PANSS general sub-scale scores (F(1,147)=6.44, P=0.012), and a trend towards a significant interaction for PSYRATS delusions sub-scale scores (F(1,138)=3.81, P=0.053) at 3 months and for PANSS positive sub-scale scores at 18 months (F(1,147)=4.422, P=0.037). There were no significant age×therapy interactions for CBT v. treatment as usual. The findings are illustrated in Figs 1 and 2. During the intervention period (3 months), supportive counselling appeared to have a greater effect on positive symptoms (measured by the PANSS positive sub-scale and PSYRATS delusions sub-scale) than CBT or treatment as usual in the younger group compared with the older group. The older group showed the opposite pattern. Over 18 months, CBT appeared to have a greater effect than supportive counselling on positive symptoms in the older group compared with the younger group. With regard to general symptoms (measured by the PANSS general sub-scale) there was a similar pattern, with supportive counselling apparently having a greater effect than treatment as usual in the younger patients compared with the older patients.
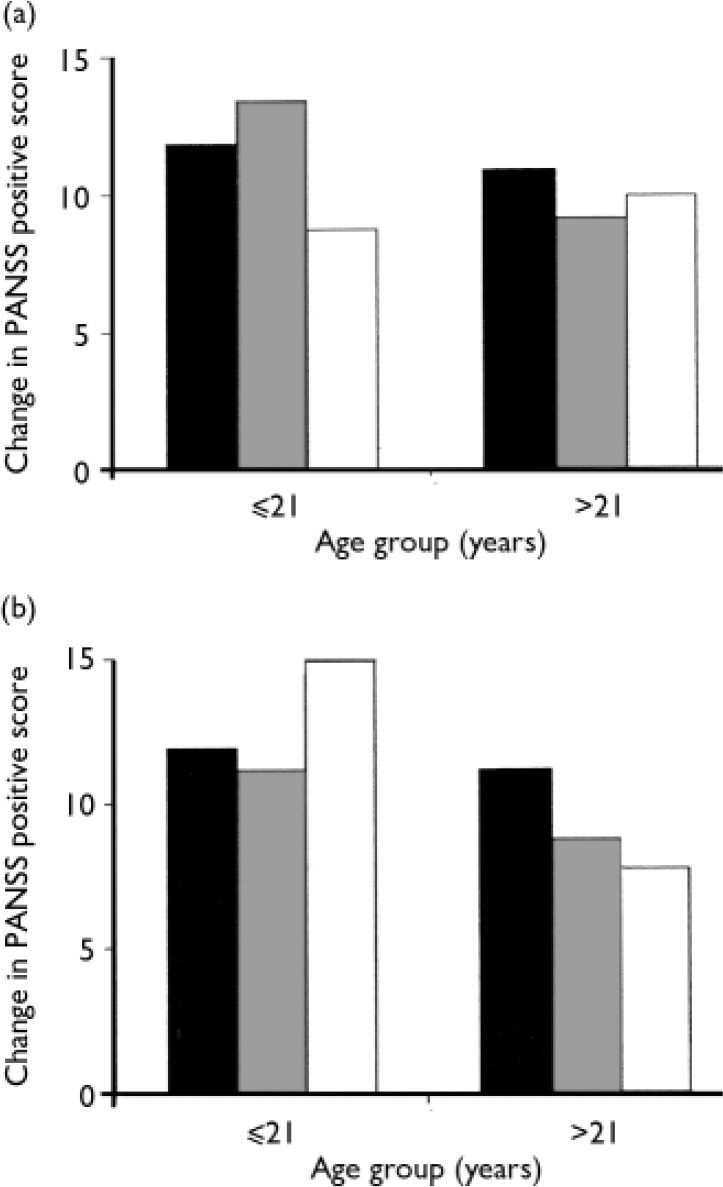
Fig. 1 Changes in PANSS positive sub-scale scores (a) from baseline to 3 months and (b) from baseline to 18 months. ▒, CBT; ░, supportive counselling; □, treatment as usual.
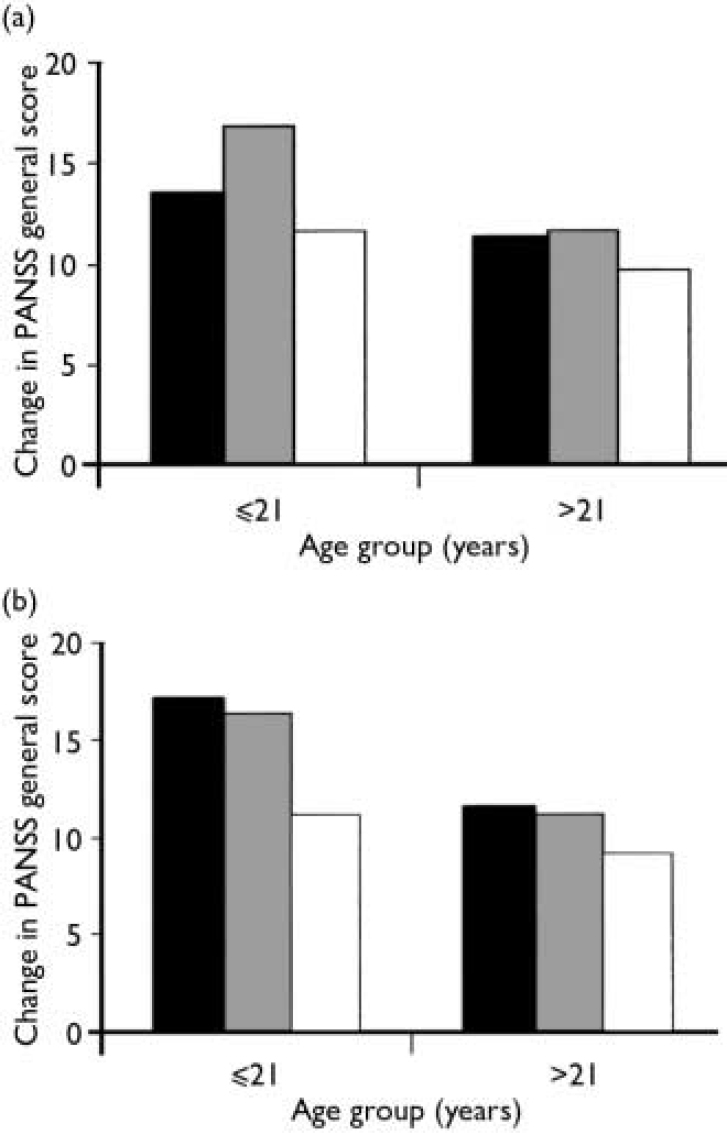
Fig. 2 Changes in PANSS general sub-scale scores (a) from baseline to 3 months and (b) from baseline to 18 months. ▒, CBT; ░, supportive counselling;□, treatment as usual.
Social functioning
Baseline
The younger age group had significantly poorer total social functioning scores (F(1,224)=4.26, P=0.04) at baseline, which were probably accounted for by significantly poorer scores on the competence and performance sub-scales of the SFS (F(1,224)=12.24, P=0.001; F(1,224)=5.77, P=0.017). No other SFS sub-scale scores differed between the two groups. The SFS scores are shown in Table 2.
Follow-up
There were no significant age×therapy interactions with regard to SFS scores at any of the follow-up points.
Insight
Baseline
There were no significant differences between the age groups at baseline.
Follow-up
There was a significant interaction between treatment and age as measured by the Birchwood Insight Scale at 18 months but not at 3 months (F(2,167)=3.88, P=0.023). This was accounted for by a highly significant age×outcome interaction between CBT and treatment as usual (F(1,107)=7.08, P=0.009). There were no significant interactions with age for CBT v. supportive counselling or for supportive counselling v. treatment as usual. These findings are illustrated in Fig. 3. The younger patients who were receiving CBT showed greater increases in insight than those who received treatment as usual. This pattern was not found in the older patients.
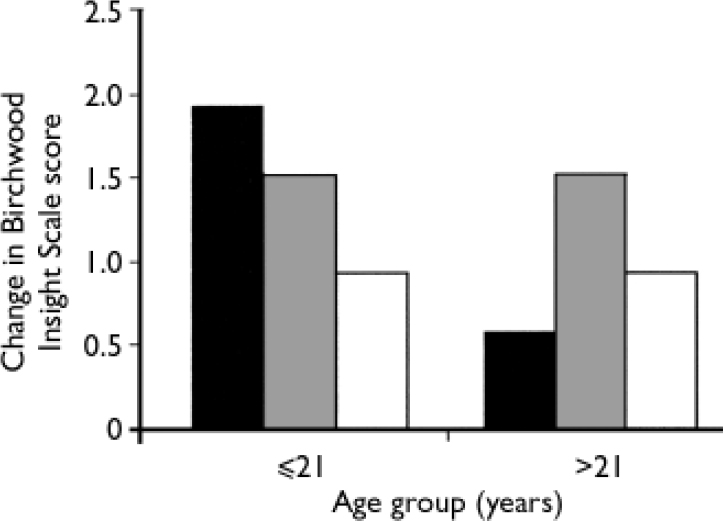
Fig. 3 Changes in Birchwood Insight Scale scores from baseline to 18 months. ▒, CBT; ░, supportive counselling; □, treatment as usual.
Therapeutic alliance
Data on therapeutic alliance were collected during the ‘therapy envelope’ in two ways from patients who received a psychological intervention (i.e. not from those who received treatment as usual alone). Patients’ views of the relationship with the therapist were assessed at two time points (in sessions 4 and 10) using the CALPAS (Reference GastonGaston, 1990). Therapists’ views of the degree to which they were able to engage the patient in therapy were also assessed at three time points (in sessions 4, 10 and 15) using the PSR (Reference Frank and GundersonFrank & Gunderson, 1990). There were no significant differences between the two age groups on the CALPAS at any time point. However, there were significant differences between the age groups on the PSR at all three time points (F(1,134)=9.62, P=0.002); F(1,105)=11.07, P=0.001; F(1,111)=6.525, P=0.012), the younger group having significantly higher scores (indicating that therapists believed there was a poorer relationship) at all measurement points.
To test whether therapeutic alliance might explain the therapy×age group interactions described earlier, cases in which therapeutic alliance scales were available were selected and re-analysed (using the methods outlined in the above section on symptom outcomes). Analyses were performed with and without covarying for initial therapeutic alliance scores. No changes in significance levels for the interactions were found between the two analyses, which suggests that therapeutic alliance cannot explain the age×therapy interactions.
DISCUSSION
Age and outcome
The findings of this exploratory trial suggest that age is a significant factor in relation to treatment in newly diagnosed patients with psychosis. This factor is not usually addressed either in treatment trials or in service provision. Specifically, there appear to be significant differences in the pattern of response to psychological and routine treatments between younger and older people with recent-onset psychosis. Supportive counselling appeared to be of greater benefit than either CBT or treatment as usual in the younger group, and CBT appeared to be of greater benefit to the older group compared with the other two treatment conditions. The differences were consistent over a number of methods of assessment, adding validity to the findings, and were robust even when differences in the sample characteristics (i.e. the shorter duration of untreated psychosis and worse symptoms at baseline in the younger group) were controlled for.
Treatment delivery issues
Although there may be a number of explanations for these differences, some of the findings may relate to the method of delivery of treatment. The younger group was rated by therapists as significantly more difficult to engage in therapy. It may be postulated that a treatment such as CBT requires a higher level of engagement than supportive counselling, as by its very nature CBT is a collaborative, agenda-led intervention which requires the active participation of the recipient. In contrast, in supportive counselling the approach is predominantly supportive and empathic, and is not directed by a collaborative agenda. It is possible that young people with recent-onset psychosis require more strategies to aid their engagement in therapy than older people, although it is not clear why this is the case. One option would be to evaluate the impact of treatment once participants had reached a specified level of engagement in therapy.
Developmental issues
Although further research is needed to help to interpret the relationships described in this study, it is possible that young patients may have different developmental needs to those who develop psychosis later in life. They may be more likely to be in contact with significant others and to be involved in full-time education, and they may not yet have become established in terms of their home circumstances, relationships or career. They are highly likely to be experiencing significant life changes relating to these developmental issues, which may have prevented them from being able to engage fully in more structured treatments. More attention may need to be given to motivating young patients to engage in therapy, and it is possible that supportive approaches such as supportive counselling may be more effective in providing this initially. However, it is also possible that once patients are engaged in therapy, CBT may be the most helpful approach. Further investigation of process variables in relation to therapy outcomes is needed to clarify these points.
Insight
In addition to the differences in symptomatic outcomes in response to treatment, there were also differences in the impact on insight according to age and treatment. Although CBT did not have the greatest impact on symptoms in the younger group, its impact on insight was significantly greater than that of supportive counselling or treatment as usual in this age group. This pattern was only apparent in the younger group. However, it was only found at the 18-month follow-up point, and the actual changes involved were small. Further investigation of this issue is warranted.
Limitations
This study has a number of limitations. First, the small number of participants in the younger age group may limit the generalisability of the findings. In addition, the selection criteria were limited to those individuals who required hospitalisation for recent-onset psychosis. This may mean that the recruited sample was not representative of the recent-onset population as a whole. In addition, there may have been differences between the comparison groups that limit the conclusions that can be drawn. For example, there were significantly higher rates of schizophrenia in the older age group compared with the younger group (43% v. 25%). However, when the differences between individuals with schizophrenia and schizophreniform disorder were examined in the two groups, it was found that participants with the two diagnoses differed in the younger group only in that those with a diagnosis of schizophrenia were experiencing significantly more negative symptoms. In the older group, significant differences between individuals with schizophrenia and schizophreniform disorder were found on all of the PANSS sub-scales. Participants with a diagnosis of schizophreniform disorder scored significantly lower than those with a diagnosis of schizophrenia. This suggests that the differences in diagnosis were not based on the severity of symptomatology alone, and that they may reflect differences in diagnostic procedures for younger compared with older patients. However, the impact of these factors was taken into account in the analysis by controlling for baseline symptoms and other factors that were known to differ between the two age groups.
Finally, although some data that would help to explain our findings were collected during the study, there is a need for a much more detailed exploration of the factors that influence engagement in and outcome of psychotherapy in early psychosis. Our findings suggest that age-related issues may be an important area for further research, and may also be important for service planning.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Treatment as usual may not address the needs of young people with recent-onset psychosis.
-
▪ Psychological therapies for psychosis need to be age-specific.
-
▪ Younger people who are experiencing their first psychotic episode may be more difficult to engage in psychological therapy.
LIMITATIONS
-
▪ The small number of participants in the younger age group may limit the generalisability of our findings.
-
▪ The participants in this study were experiencing an acute first episode of psychosis which required hospitalisation, so may not be representative of first-episode samples generally.
-
▪ Few process measures were used during the trial. Such data might have helped to explain the nature of the differences that were found between the two age groups.
Acknowledgements
The SoCRATES trial was funded by the UK Medical Research Council, the Northwest England National Health Service Executive (NHSE) office, Trent NHSE office and the following health authorities: Manchester; Salford and Trafford; Liverpool; Sefton; St Helens and Knowsley; and Nottinghamshire.








eLetters
No eLetters have been published for this article.