The number of people who are compulsorily admitted to psychiatric hospitals is rising each year in England,1 as well as several other European countries.Reference Zolkowska, Cantor-Graae and McNeil2,Reference Schoevaerts, Bruffaerts, Mulder and Vandenberghe3 Although compulsory admissions may help to reduce short-term risks, there are negative repercussions for both the individual and healthcare services.Reference Katsakou and Priebe4–Reference Cotton, Johnson, Bindman, Sandor, White and Thornicroft8 The reasons for these rising rates are complex and debated, and are likely to include socioeconomic, legal and service-related factors.9 Reducing compulsory admissions has been identified as a priority for mental health services,9 but we lack a strong evidence base on the most effective interventions to achieve this.
Crisis-planning interventions
Crisis-planning interventions are one of the few that have been identified as potentially beneficial in reducing the risk of compulsory admissions.Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10,Reference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11 In this review, we use ‘crisis planning’ as an overall descriptive term for interventions that focus on involving patients in identifying preferences and planning for their care in the event of a future mental health crisis. Multiple types of crisis plan exist that vary in terminology, content and legal enforceability between jurisdictions. In England, advance decisions are legally binding and document a person's instructions for healthcare they want to refuse in the future, if they lose capacity for making treatment decisions at that time.12 However, if patients have been admitted under the Mental Health Act 2007, doctors' statutory authority to provide treatment overrides advance decisions.13 In contrast to advance decisions, advance statements can be used to describe a person's preferences for the care they would like to receive, as well as treatments they want to refuse, but are not legal documents.Reference Dunn14 Joint crisis plans are a type of advance statement developed collaboratively between the patient and mental health professionals, which are also not legally enforceable. In Scotland, advance decisions (which indicate which treatments a person wants to refuse) are known as advance directives, but are not legally binding.15 In the USA, psychiatric advance directives provide documentation of people's preferences for future mental health treatment during a crisis, with legislation varying by state (https://www.nrc-pad.org/).
Crisis-planning interventions may help to prevent relapse, for example by promoting better self-management, or may reduce the need for hospital admissions by encouraging prompt help-seeking or improved community service responses. The presence of crisis plans may also make patients and clinicians more willing to accept voluntary hospital admissions when a crisis occurs, because of greater awareness of indicators of relapse and increased confidence on the part of the patient that their treatment preferences will be respected once admitted, even if capacity is lost.
Aims
A previous review of interventions to reduce compulsory psychiatric admissions found that crisis plans were the only intervention that appeared to be effective,Reference De Jong, Kamperman, Oorschot, Priebe, Bramer and van de Sande16 with pooled estimates for community treatment orders (three randomised controlled trials (RCTs)), adherence enhancement (two RCTs) and integrated treatment (four RCTs) showing no significant effects. However, this review gave little information on the core components of the crisis-planning interventions and did not examine important secondary outcomes, including voluntary admissions, length of stay and therapeutic alliance. We therefore conducted a thorough up-to-date systematic review of RCTs examining crisis-planning interventions for people with psychotic illness or bipolar disorder. The primary review question examines whether crisis-planning interventions are effective for reducing compulsory admissions among people with psychotic illness or bipolar disorder, compared with treatment as usual. Secondary review questions examine the impact of crisis-planning interventions on other outcomes of interest including voluntary admissions, duration of in-patient treatment, psychiatric functioning, quality of life, therapeutic alliance, patient engagement, perceived coercion, adverse effects and cost-effectiveness.
Method
The protocol for this review was prospectively registered on PROSPERO (registration: CRD42018084808) and followed the PRISMA guidelines.
Eligibility criteria and selection of studies
This review sought to identify RCTs examining crisis-planning interventions for people with psychotic illness or bipolar disorder. The inclusion criteria were as follows.
(a) Studies of adults (aged 16 and over) who had a diagnosis of a psychotic illness or bipolar disorder with or without psychotic symptoms. Studies including mixed populations of patients from secondary care mental health services were eligible if the majority of participants had a diagnosis of a psychotic illness or bipolar disorder.
(b) Studies that examined any form of crisis-planning intervention that involved the patient in decisions regarding future treatment preferences (including advance decisions, advance directives, joint crisis plans and other relevant interventions). Interventions that included follow-up meetings were eligible, if the primary aim of these meetings was to review the crisis plan. Interventions where crisis planning was not the primary focus were not eligible.
(c) Studies were eligible if the comparison group was treatment as usual, defined as the standard care in that setting. Studies that compared a crisis-planning intervention with a different active intervention were not eligible.
(d) Only randomised controlled trials (published or unpublished) were eligible, including cluster RCTs.
There were no exclusion criteria based on language or date of publication.
The primary review outcome was compulsory hospital admission for psychiatric care. The secondary outcomes of interest were: (a) voluntary hospital admission for psychiatric care; (b) any hospital admission for psychiatric care; (c) duration of in-patient psychiatric treatment; (d) global and specific psychiatric symptoms; (e) psychiatric functioning; (f) quality of life; (g) therapeutic alliance; (h) service engagement; (i) perceived coercion; (j) adverse effects; and (k) cost-effectiveness. These outcomes could be assessed at any time point.
Data sources and selection of studies
The following databases were searched from inception to 16 October 2018: Cochrane Central Register of Controlled Trials (CENTRAL), CINAHL, Medline, EMBASE, PsycINFO and the International Standard Randomised Controlled Trial Number (ISRCTN) registry. The search strategy was based around terms for crisis plans or advance directives, mental disorders and RCTs. The full search strategy is available in Supplementary Appendix 1 available at https://doi.org/10.1192/bjo.2019.28. Conference proceedings from the European Psychiatric Association, World Psychiatric Association, the European Network for Mental Health Service Evaluation and the American Psychiatric Association from 2011 onwards were hand-searched for relevant RCTs. Forward and backward citation tracking were conducted for all eligible studies and for two relevant systematic reviews,Reference De Jong, Kamperman, Oorschot, Priebe, Bramer and van de Sande16,Reference Campbell and Kisely17 to identify any additional relevant studies.
Title and abstract screening and full-text screening were conducted by two reviewers independently. Following title and abstract screening, the full texts of all articles identified as potentially relevant by either reviewer were obtained. Any discrepancies following full-text screening were resolved through discussion with a third author when necessary. Relevant data for the review (relating to the participants, setting, method, intervention, comparison and outcomes) were extracted into a data extraction table and checked by a second reviewer. Authors of the papers were contacted to request additional information if needed, if this related to the primary outcome of compulsory hospital admission.
Risk of bias assessment
Risk of bias was assessed for each study using the Cochrane Collaboration Risk of Bias ToolReference Higgins, Altman, Gøtzsche, Jüni, Moher and Oxman18,Reference Higgins and Green19 for the following domains: sequence generation, allocation concealment, masking of outcome assessors, incomplete outcome data and selective reporting. Two reviewers conducted risk of bias assessments for all papers independently and any discrepancies were resolved through discussion, including a third author if necessary.
Data synthesis
The number of participants with and without the primary outcome of compulsory psychiatric admission was extracted from all studies for the intervention and control groups separately. A pooled risk ratio (RR) with 95% CI was calculated through random-effects meta-analysis using the Mantel–Haenszel method. Heterogeneity between trials included in the meta-analyses was investigated by visual inspection of the forest plots and calculation of the I 2 statistic. Where there was indication of heterogeneity (for example I 2 statistic higher than 50%), the study quality, clinical population and intervention content were considered as possible explanatory factors. If any studies eligible for the meta-analysis included more than one crisis-planning intervention condition, we combined the active treatment groups into a single arm for comparison against the control group, in line with the recommendations in the Cochrane Handbook for Systematic Reviews of Interventions.Reference Higgins and Green19 A subgroup analysis was planned to pool studies or treatment conditions in which the crisis-planning intervention was facilitated by a healthcare professional, and those where it was not facilitated by a healthcare professional (for example by a patient advocate).
The main meta-analyses were conducted including only participants for whom outcome data was available (i.e. complete case analysis). Such analysis assumes that data are missing at random. Sensitivity analyses were performed to investigate the robustness of findings to changing assumptions regarding the mechanism of missing data, as recommended in the Cochrane Handbook for Systematic Reviews of Interventions.Reference Higgins and Green19 Four different assumptions were made to complete the missing data: first, that participants lost to follow-up had no compulsory admissions; second, that they had the same rate of compulsory readmissions as other participants in the same arm of the same trial; third, that the proportion of readmissions was 10 percentage points lower among those lost to follow-up; and finally, that the proportion of readmissions was 10 percentage points higher among those lost to follow-up. An additional sensitivity analysis excluded studies with high risk of bias in any domain from the meta-analysis. Finally, an influence analysis was conducted in which each study was removed in turn from the meta-analysis. If sufficient (ten or more) studies were included in any meta-analysis, a funnel plot would be used to investigate potential publication bias.Reference Egger, Smith, Schneider and Minder20
Random-effects meta-analysis was also used to pool data for each of the secondary outcomes, if three or more comparable studies were identified. Risk ratios were pooled for dichotomous outcomes and standardised mean differences were calculated and combined for continuous outcomes. If insufficient comparable studies were identified for any planned analyses, narrative synthesis was used. Key components of crisis-planning interventions from the included studies were also described and compared.
Results
The search strategy identified 1428 studies, of which 1023 remained after duplicates were removed. Through title and abstract screening, 964 records were excluded. Full texts for the remaining 59 studies were obtained and assessed for eligibility. Five studies met the inclusion criteria and were included in the review. The study selection process is shown in Fig. 1.
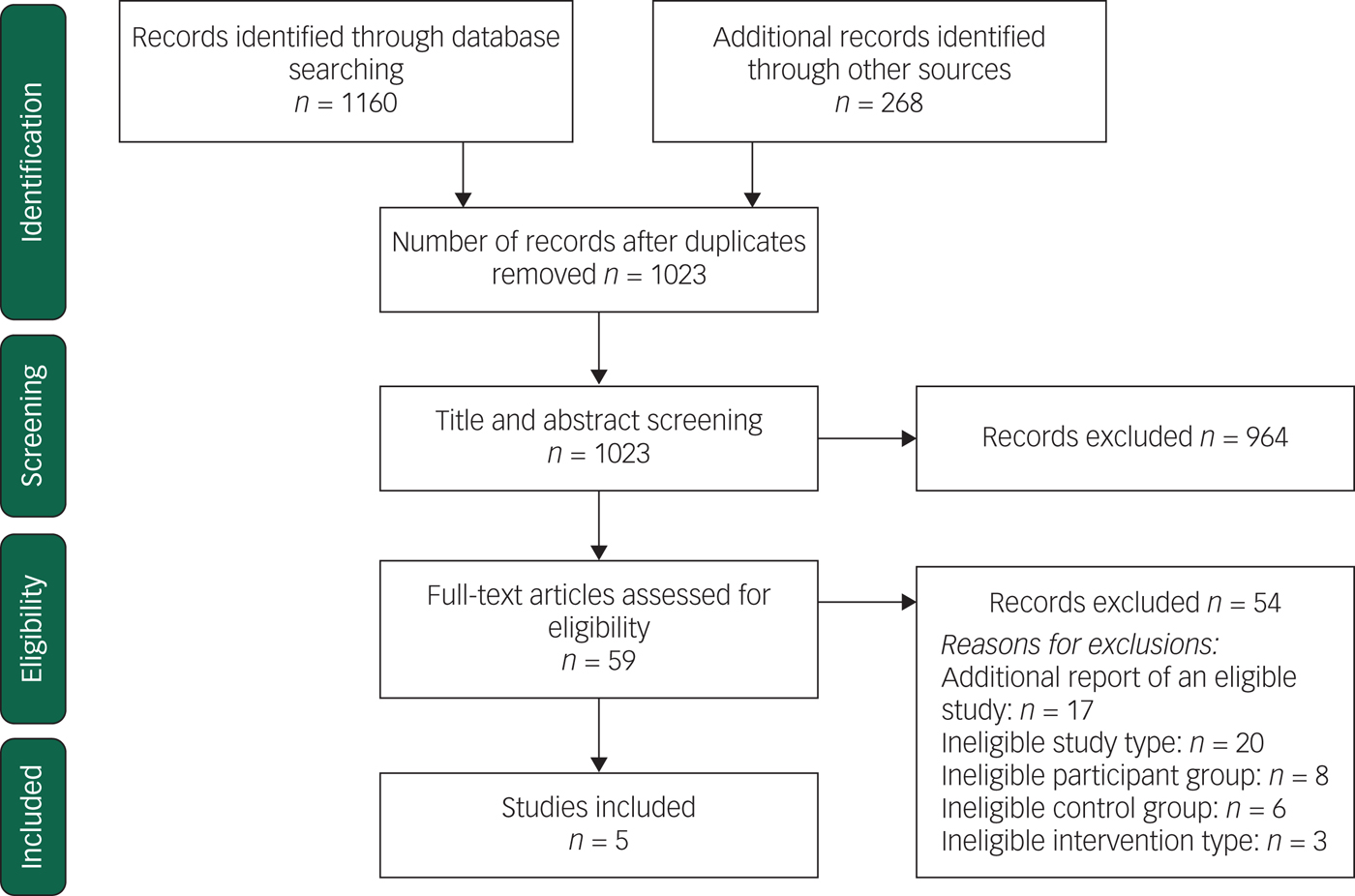
Fig. 1 PRISMA flow diagram.
Study characteristics
Key characteristics of the five included studies are given in Table 1. Three trials only included participants with psychotic disorders or bipolar disorder,Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10,Reference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11,Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21 whereas the other two trials included mixed populations from secondary care mental health services.Reference Lay, Kawohl and Rossler22,Reference Papageorgiou, King, Janmohamed, Davidson and Dawson23 All of the trials reported a majority diagnosis of schizophrenia or schizophrenia-like disorders. Follow-up periods for the trials ranged from 12 to 24 months. In all five trials, the crisis-planning intervention was compared with treatment as usual, however, in one trial the control group also received an information leaflet about local mental health services and the Mental Health Act.Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10
Table 1 Key characteristics of included studies
There was some variation in the components of the crisis-planning interventions across the included trials. In two trials, the intervention commenced while participants were psychiatric in-patients;Reference Lay, Kawohl and Rossler22,Reference Papageorgiou, King, Janmohamed, Davidson and Dawson23 the other three trials recruited out-patients with previous psychiatric admissions.Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10,Reference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11,Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21 One trialReference Papageorgiou, King, Janmohamed, Davidson and Dawson23 examined the effectiveness of a type of advance statement, in which participants completed a booklet consisting of seven statements on future treatment preferences, with support from researchers. Three trials examined joint crisis-planning interventions.Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10,Reference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11,Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21 One of these included two intervention groups; participants could be randomised to a clinician-facilitated crisis plan (i.e. joint crisis plan) or a patient-advocate facilitated crisis plan.Reference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11 In the other two trials of joint crisis plans,Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10,Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21 the crisis plan was facilitated by a healthcare professional who was part of the research team, and discussed at one or more meetings with members of the patient's clinical team, and a family member or friend if they wished.
Finally, one trial examined a crisis-planning intervention that was facilitated by a healthcare professional (psychologist) without involvement from the patient's clinical team.Reference Lay, Kawohl and Rossler22 This trial implemented a higher intensity crisis-planning intervention, in which participants in the intervention group attended a varying number of individualised psychoeducation sessions focused on identifying behaviours prior to crisis and developed crisis cards consisting of future treatment preferences. In addition, they received 4-weekly telephone monitoring, to review the crisis cards and facilitate the detection of early signs of crisis identified in the previous psychoeducation sessions.
A summary of the intended components of the interventions are given in Table 2, and a detailed description of the content of each intervention and control condition is reported in Supplementary Appendix 2. None of the crisis plans examined in the included RCTs were legally enforceable.
Table 2 Components of the (intended) intervention across trials
a. Ruchlewska et al. Reference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11 included two intervention arms, one facilitated by a healthcare professional and one facilitated by a patient-advocate.
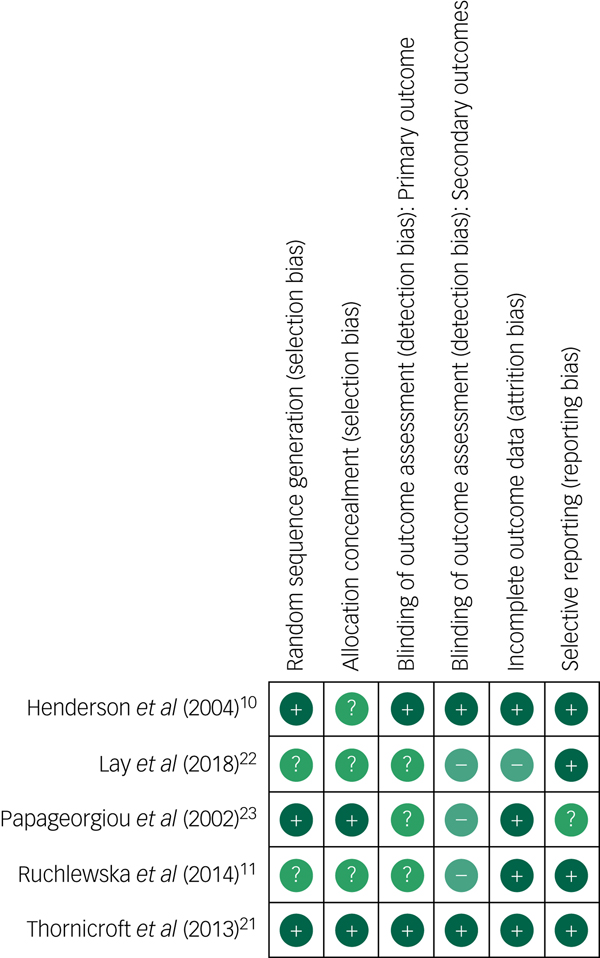
Risk of bias in included studies
Figure 2 summarises the risk of bias in the included trials, assessed using the Cochrane collaboration tool.Reference Higgins, Altman, Gøtzsche, Jüni, Moher and Oxman18 Three trials had low risk of bias for sequence generationReference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10,Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21,Reference Papageorgiou, King, Janmohamed, Davidson and Dawson23 and two had low risk of bias for allocation concealment.Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10,Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21 The remaining studies had unclear risk of bias in these domains, with insufficient detail provided in trial reports. None of the trials were able to mask the participants or staff, because of the nature of the intervention, so this was not included in the risk of bias assessment. However, masking of outcome assessors was examined. Three of the five trials did not mask outcome assessors to group allocation,Reference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11,Reference Lay, Kawohl and Rossler22,Reference Papageorgiou, King, Janmohamed, Davidson and Dawson23 which could lead to risk of detection bias. However, the impact of detection bias on the primary outcome of this review (compulsory hospital admissions) should be limited, as this was assessed or cross-checked with hospital records in all included studies. Risk of bias was therefore assessed separately for the primary and secondary outcomes, and studies in which no masking was performed were rated as having unclear risk of bias for the primary outcome, and high risk of bias for the secondary outcomes.
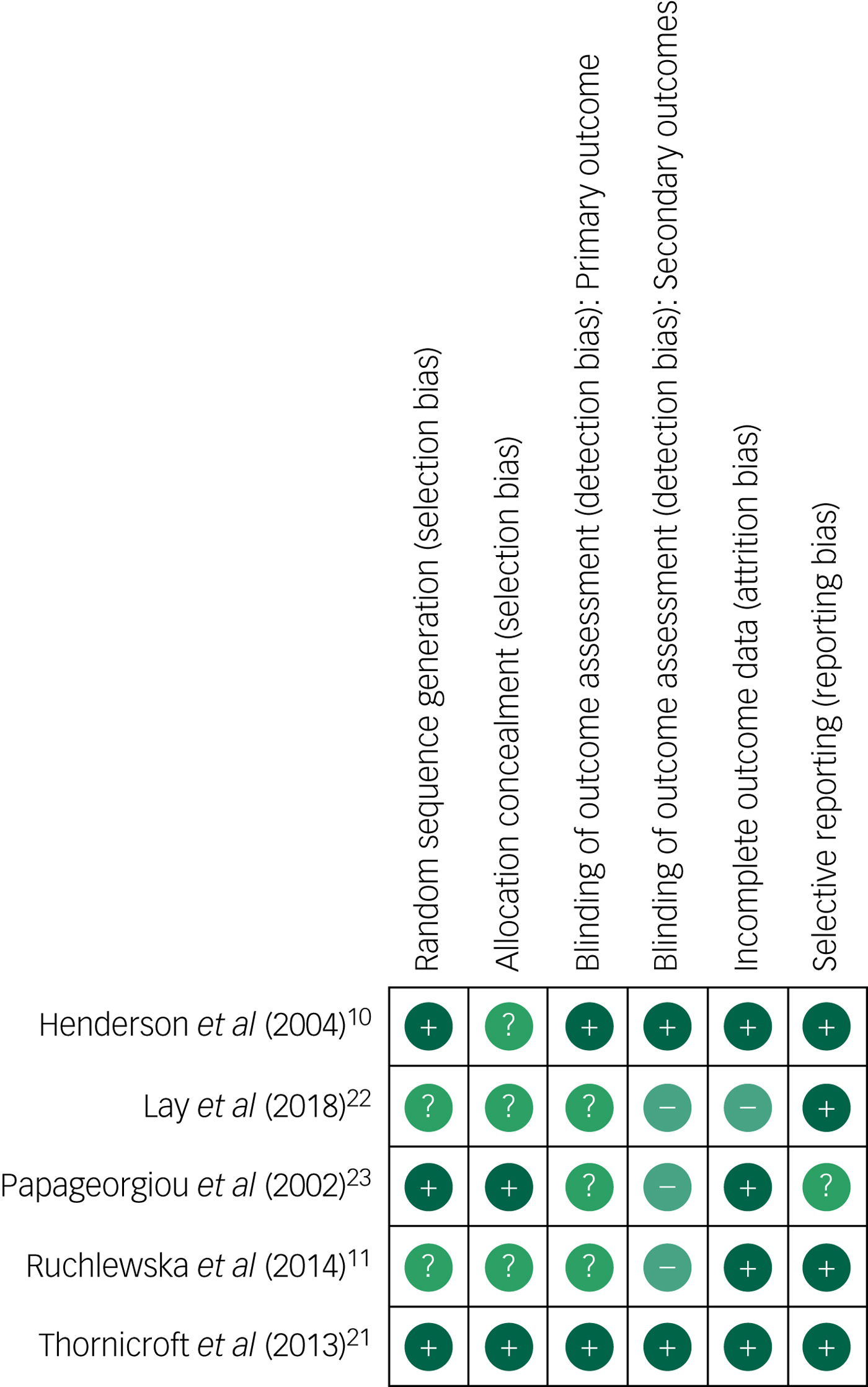
Fig. 2 Risk of bias assessment
In four studies, the risk of attrition bias was low. The primary outcome of compulsory admissions was largely collected from hospital records meaning that missing data for the primary outcome was less than 4% in four studies.Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10,Reference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11,Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21,Reference Papageorgiou, King, Janmohamed, Davidson and Dawson23 However, in one study,Reference Lay, Kawohl and Rossler22 readmission data was only reported for participants who completed the outcome assessments. This study was rated as having high risk of attrition bias as loss to follow-up was unbalanced between groups (32.8% from the intervention group and 14.3% from the control group).
Compulsory hospital admissions
All five trials reported the number of participants who had a compulsory admission or readmission to hospital during the follow-up period, which ranged from 12 to 24 months. Based on complete case analysis, the proportion of participants experiencing compulsory admissions in each study ranged from 13% to 28% in the intervention groups and 20% to 43% in the control groups.
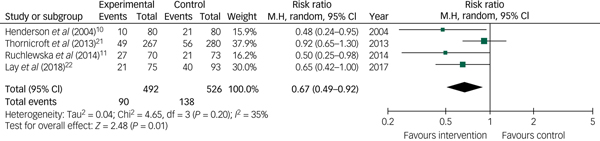
The results of all five studies were pooled using random-effects meta-analysis, as shown in Fig. 3. The pooled estimate showed a 25% reduction in compulsory admissions among those receiving crisis-planning interventions compared with those who did not receive the intervention (RR = 0.75, 95% CI 0.61–0.93, P = 0.008). There was no evidence of moderate or substantial heterogeneityReference Deeks, Higgins, Altman, Higgins, Churchill, Chandler and Cumpston24 (I 2 = 0%, χ2 = 3.94, d.f. = 4, P = 0.41). A subgroup analysis was conducted to pool studiesReference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10,Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21,Reference Lay, Kawohl and Rossler22 or treatment conditionsReference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11 in which the crisis-planning intervention was facilitated by a healthcare professional, which gave a similar estimate (RR = 0.67, 95% CI 0.49–0.92; based on four studies; see Fig. 4).
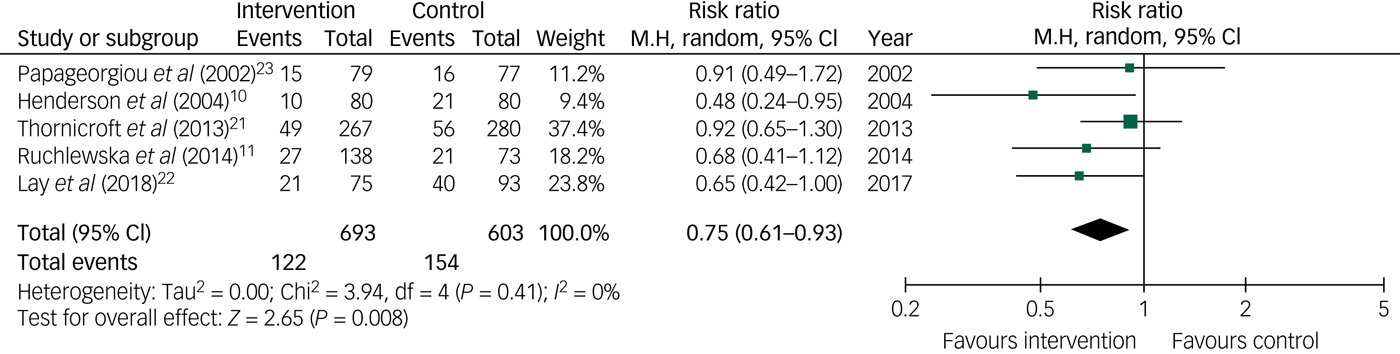
Fig. 3 Forest plot showing the risk of compulsory hospital admissions among those receiving a crisis-planning intervention compared with controls.
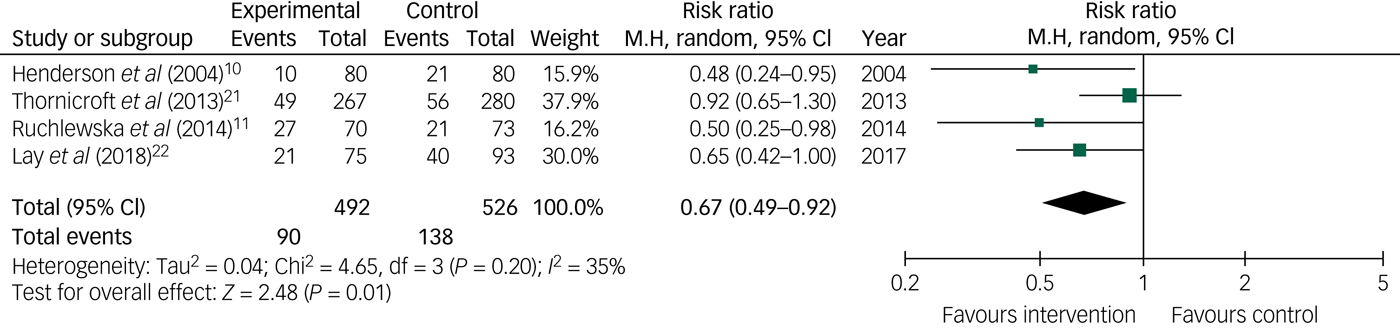
Fig. 4 Forest plot showing the risk of compulsory hospital admissions among those receiving a clinician-facilitated crisis-planning intervention compared with controls.
There were only two studies that examined crisis-planning interventions that were not facilitated by a healthcare professional, so these results were not pooled using meta-analysis. There was no evidence that the crisis-planning intervention facilitated by researchers in Papageorgiou et al'sReference Papageorgiou, King, Janmohamed, Davidson and Dawson23 trial was effective in reducing compulsory hospital admissions. In Ruchlewska et al'sReference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11 trial, 16% of participants receiving patient-advocate-facilitated crisis plans were admitted under court order in the follow-up period, compared with 10% in the clinician-facilitated crisis plan group and 26% in the control group.
Sensitivity analyses were conducted to investigate the robustness of the findings (see Supplementary Appendix 3). First, the proportion of compulsory admissions was calculated under four different assumptions for missing outcome data. All four analyses gave comparable findings to the main results. The pooled estimate was RR = 0.70 (95% CI 0.54–0.90) under the assumption that there were no compulsory admissions among participants with missing follow-up data and RR = 0.74 (95% CI 0.61–0.91) under the assumption that participants with missing follow-up data had the same rate of compulsory admissions as participants with follow-up data in the same arm of that trial. Assuming that the rate of compulsory readmissions was either 10 percentage points lower or higher among participants with missing data, the pooled estimates were RR = 0.72 (95% CI 0.57–0.92) and RR = 0.77 (95% CI 0.63–0.94), respectively.
An additional sensitivity analysis was conducted to exclude studies with high risk of bias from the meta-analysis. Only one study (Lay et al Reference Lay, Kawohl and Rossler22) had high risk of bias in any domain relating to the primary outcome. After excluding this study, the pooled effect was slightly attenuated (RR = 0.78, 95% CI 0.60–1.01). Finally, influence analyses were conducted to remove each study in turn from the pooled estimate. As described previously, excluding Lay et al Reference Lay, Kawohl and Rossler22 slightly attenuated the relationship, but other influence analyses did not alter conclusions (see Supplementary Appendix 3 for full details).
Secondary outcomes
Other hospital admissions and length of admissions
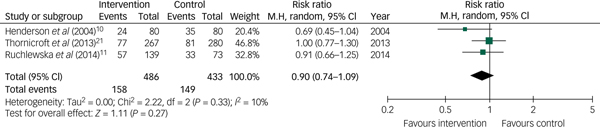
Three studies reported the prevalence of voluntary hospital admissionsReference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11,Reference Lay, Kawohl and Rossler22,Reference Papageorgiou, King, Janmohamed, Davidson and Dawson23 and three reported the overall prevalence of admissions to psychiatric care (i.e. including both compulsory and voluntary admissions).Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10,Reference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11,Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21 Pooled estimates for these secondary outcomes showed no evidence that crisis-planning interventions reduced the risk of voluntary admissions (RR = 1.17; 95% CI 0.91–1.50; see Fig. 5) or any psychiatric admissions (RR = 0.90, 95% CI 0.74–1.09; see Fig. 6).
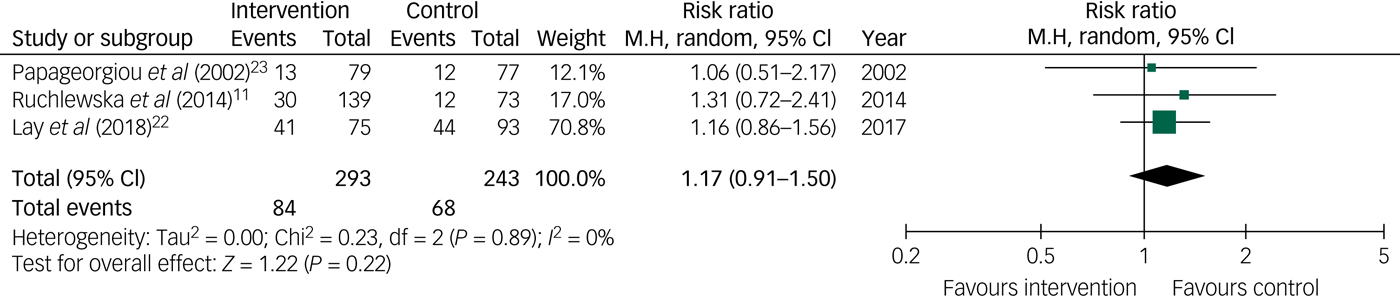
Fig. 5 Forest plot showing the risk of voluntary hospital admissions among those receiving a crisis-planning intervention compared with controls.
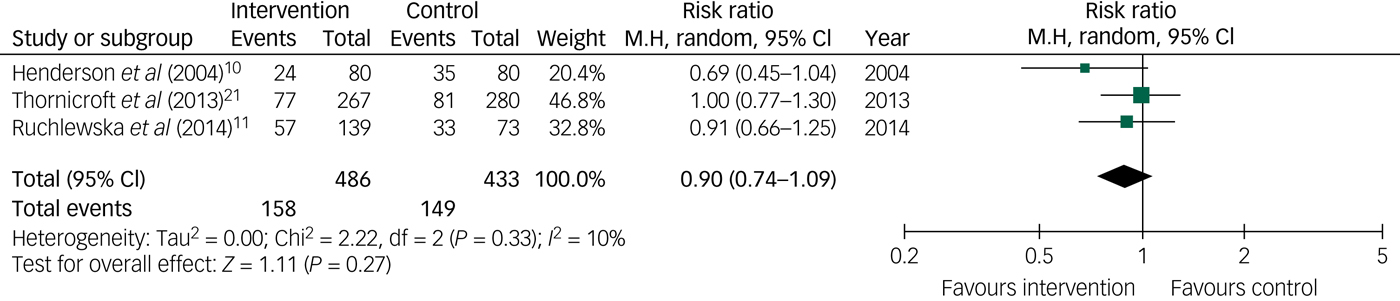
Fig. 6 Forest plot showing the risk of any psychiatric admissions among those receiving a crisis-planning intervention compared with controls.
Only two studies reported data on duration of admissions among those who had received an admission during the study period. One of these studies (Henderson et al Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10) reported that there was no difference in length of compulsory admissions between the intervention and control groups, and the other (Ruchlewska et al Reference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11) reported no difference in overall length of admissions (compulsory and voluntary combined). Four of the studies compared duration of admissions in the intervention and control groups for their entire samples (i.e. also including those who had not received an admission during the study period as having zero days of admission), using means, medians or counts. Of these four studies, two found no difference between the intervention and control groups for the duration of compulsory or voluntary admissions.Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21,Reference Papageorgiou, King, Janmohamed, Davidson and Dawson23 In contrast, two studies reported that the mean length of compulsory admissions was lower for the intervention than the control group, but there was no difference in the length of any admissionsReference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10 or voluntary admissions.Reference Lay, Kawohl and Rossler22
Psychiatric functioning and quality of life
One study reported on psychiatric symptoms and functioning at 12 months’ follow-up,Reference Papageorgiou, King, Janmohamed, Davidson and Dawson23 and found no difference between the intervention and control groups. Lay et al Reference Lay, Kawohl and Rossler22 did not report psychiatric functioning at 24 months, but found no difference in functioning in an interim analysis at 12 months post-randomisation.Reference Lay, Kawohl and Rossler22,Reference Lay, Drack, Bleiker, Lengler, Blank and Rössler25 Finally, one study examined patients' insight into their psychiatric symptoms,Reference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11 again reporting no difference between the intervention and control groups. None of the trials included in this review reported quality of life.
Therapeutic alliance, service engagement and perceived coercion
Thornicroft et al Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21 reported no evidence of a difference in perceived coercion, service engagement or clinician-rated therapeutic alliance between groups. However, there was evidence for a slight improvement in patient-rated therapeutic relationship, assessed by the Working Alliance Inventory Client (WAIC), in the intervention group compared with controls after adjusting for variables associated with trial design and loss to follow-up (mean difference −1.28, P = 0.049, adjusted for baseline WAIC score, site, number of previous admissions and diagnosis).Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21 Ruchlewska et al Reference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11 reported no difference in service engagement or working alliance (either patient or clinician rated) between the intervention arms and the control group. Lay et al Reference Lay, Kawohl and Rossler22 did not report these outcomes at 24 months, but found no group differences in perceived coercion at 12 months post-randomisation.Reference Lay, Drack, Bleiker, Lengler, Blank and Rössler25 Two trials did not report any outcomes related to therapeutic alliance, service engagement or perceived coercion.Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10,Reference Papageorgiou, King, Janmohamed, Davidson and Dawson23
Adverse effects
No studies reported any specific assessment of adverse events.
Cost-effectiveness
Cost-effectiveness was not reported in any of the main trial papers. However, economic evaluations were published separately for two of the included trials.Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10,Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21 For the Henderson et al Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10 trial, cost-effectiveness acceptability curves suggested that there was over 78% probability that joint crisis plans were more cost-effectiveness than usual care.Reference Flood, Byford, Henderson, Leese, Thornicroft and Sutherby26 The economic evaluation of the Thornicroft et al Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21 trial found a similar overall probability (80%) that joint crisis plans were more cost-effective than usual care.Reference Barrett, Waheed, Farrelly, Birchwood, Dunn and Flach27
Discussion
This systematic review identified five RCTs that examined the effectiveness of crisis-planning interventions for adults with psychotic illness or bipolar disorder. A meta-analysis of these studies showed a 25% reduction in risk of compulsory hospital admissions among those receiving crisis-planning interventions compared with usual care, a finding that was found to be robust in multiple sensitivity analyses. In contrast, there was no evidence for a reduction in voluntary admissions or total psychiatric admissions, and the pooled estimate for voluntary admissions showed a trend towards increased risk following crisis-planning interventions. It may be that crisis-planning interventions do not prevent admissions entirely but can reduce compulsory admissions rates by shifting some of these to voluntary admissions.
Our findings are in keeping with a previous systematic review that examined interventions to reduce compulsory psychiatric admissions.Reference De Jong, Kamperman, Oorschot, Priebe, Bramer and van de Sande16 That review identified four RCTs investigating the effectiveness of crisis-planning interventions (including advance statements and joint crisis plans), with searches conducted in April 2015. Our review updates this previous review, including one additional trial of an intensive crisis-planning interventionReference Lay, Kawohl and Rossler22 and provides further details on the characteristics of the interventions and the secondary outcomes of these trials. These details are important for clinicians considering implementing crisis-planning interventions or for researchers planning future studies in this area. Implications for research and clinical practice are described in the final section of this discussion.
Although the pooled estimate shows that crisis-planning interventions were effective in reducing compulsory admissions, there was variation between individual studies both in the characteristics and the effectiveness of the crisis-planning interventions. All of the included RCTs found a trend for a positive effect of crisis-planning interventions but this was not statistically significant in three of the five original studies. The meta-analysis is therefore an important contribution to the evidence base as consideration of the trials individually might have led to more cautious conclusions about the effectiveness of crisis-planning interventions.
Thornicroft et al Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21 found no evidence that their intervention was effective in reducing compulsory admissions. This is the largest included study and was assessed to have low risk of bias in all domains, so the null finding could reduce confidence in the overall positive conclusion from our meta-analysis. Thornicroft et al themselves considered potential explanations for their null finding, which was in contrast with the Henderson et al Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10 trial that followed a highly similar protocol in a smaller sample. In the Thornicroft et al trial, it was found that almost 50% of the crisis plans were developed during usual clinical review meetings as staff had not made themselves available to discuss the crisis plan at a specific time. Qualitative interviews conducted with participants in Thornicroft et al's trial suggested that this had an impact on the patients' experiences, as many could not remember the crisis-planning meeting as being distinct from other routine meetings, and also commented that the content of their plans was not followed during subsequent crises. Problems with implementation of the crisis-planning intervention were also reported in other studies, for example, Ruchlewska et al reported that only 57% of the clinician-facilitated crisis plans were completed.Reference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11 It is notable that the pooled estimate showed a positive impact of crisis-planning interventions given these implementation challenges.
Methodological strengths and limitations
This review provides an updated account of the effects of crisis-planning interventions for people with psychotic illness or bipolar disorder, and highlights that these interventions may be effective in reducing risk of compulsory hospital admissions. However, the conclusions of this review are limited by the small number of studies included, particularly in some subgroup analyses, and the fact that all included trials were conducted in Europe. The review was limited to RCTs because these represent the gold standard when evaluating interventions.Reference Higgins and Green19 Observational studies and studies using routine hospital data may also generate valuable evidence about the effectiveness and implementation of these interventions outside experimental conditions and could be included in future reviews. A strength of this review was the inclusion of secondary outcomes such as quality of life, psychiatric functioning, perceived coercion and therapeutic alliance, which were not examined in the earlier systematic review of interventions to reduce compulsory admissions.Reference De Jong, Kamperman, Oorschot, Priebe, Bramer and van de Sande16 However, these were not widely assessed in the included trials, thus limiting our ability to draw conclusions about the effectiveness of crisis-planning interventions for these outcomes.
Several trials included in this review reported that a high proportion of the patients approached were either ineligible or declined to participate. Low rates of recruitment are common for trials on psychotic illness or bipolar disorder, where there is often a multitude of factors that can prevent a person from taking part in research.Reference Howard, de Salis, Tomlin, Thornicroft and Donovan28 Nevertheless, recruitment rates can be an important indicator of the acceptability of an intervention, and low recruitment rates may also suggest that participants are not representative of the target population. Three out of the five trials included in this review reported a lower number of compulsory admissions in the control arm than was initially predicted from local routine data, which may be the result of systematic differences between those who agreed to participate in the trials and those who did not. Only studies conducted in Europe were identified so our findings may have limited generalisability to other settings. In addition, changes in clinical practice and service funding over time may limit the applicability of studies such as Henderson et al's (published in 2004)Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler10 to the current context.
Our review focused on crisis-planning interventions for individuals with psychotic disorders and bipolar disorder, meaning that we are unable to draw conclusions about the effectiveness of crisis-planning interventions for other groups at risk of compulsory admission. However, there is very little evidence for other disorders. One previous pilot RCT examined crisis-planning interventions for individuals with a diagnosis of personality disorderReference Borschmann, Barrett, Hellier, Byford, Henderson and Rose29 but did not include compulsory admissions as an outcome. In addition, none of the RCTs included in this review examined advance decisions that were legally binding, so it is not clear what impact the legal basis would have on risk of compulsory hospital admissions.
Loss to follow-up is also a common problem for RCTs; however, this had limited impact on the primary outcome of this review that was collected from routine records for the majority of the trials. The exception to this is Lay et al,Reference Lay, Kawohl and Rossler22 who only had readmission data for participants who completed the follow-up interviews. This study was rated as having high risk of attrition bias as there was substantial loss to follow-up that was unbalanced between study groups. However, we examined multiple different assumptions for imputing missing data in sensitivity analyses and these did not alter the overall conclusions, so we believe our findings are robust to the missing data in this study.
All studies had low or unclear risk of bias in the other domains assessed, with the exception of masking of outcome assessors. In addition, no studies included masking of participants or study personnel, because of the nature of the intervention. Lack of masking is unlikely to lead to bias for the primary outcome, for which data on compulsory admissions was extracted from medical records but may have led to bias in the secondary outcomes.
Implications for research and clinical practice
The recent Independent Review of the Mental Health Act emphasised the need to reduce compulsion and for individuals to have greater choice and autonomy in their care.9 Our systematic review was part of the evidence considered for the Mental Health Act review, which recommended that crisis-planning interventions (referred to as advance choice documents) should be used, and that ‘in the future, a request for a treatment that might be less than optimal, but still possible, should be honoured’9 (if clearly made by a person with decision-making capacity).
In this systematic review and meta-analysis, we found that crisis-planning interventions are effective for reducing compulsory admissions among adults with psychotic illness or bipolar disorder who have experienced previous psychiatric admissions or crisis contacts with mental health services. Economic evaluations of two trials also reported a high likelihood that crisis-planning interventions are cost-effective. Therefore, our review highlights the importance of offering support to patients to make crisis plans if they have had previous compulsory admissions or are identified as being at high risk. This is particularly important as a recent systematic review of RCTs of any interventions to reduce compulsory psychiatric admissionsReference De Jong, Kamperman, Oorschot, Priebe, Bramer and van de Sande16 found no evidence for the effectiveness of other interventions including community treatment orders, compliance enhancement or integrated treatment.
Greater knowledge of the mechanisms by which crisis-planning interventions reduce compulsory admissions is required. Although data for secondary outcomes was limited in this review, individual studies that assessed these outcomes reported no impact on psychiatric functioning, perceived coercion or service engagement, and minimal impact on patient-reported therapeutic alliance. The lack of substantial impact on therapeutic alliance was unexpected but may relate to the fact that only two included studies assessed therapeutic allianceReference Ruchlewska, Wierdsma, Kamperman, van der Gaag, Smulders and Roosenschoon11,Reference Thornicroft, Farrelly, Szmukler, Birchwood, Waheed and Flach21 and, as discussed above, in both of these studies the clinicians' commitment to the crisis-planning intervention was found to be limited. There was also no evidence that crisis-planning interventions reduced the risk of voluntary psychiatric admissions; in fact, there was a trend for these to be higher among participants in the intervention than control groups. Therefore, rather than preventing hospital admissions, crisis plans may reduce compulsory admissions by making patients and/or clinicians more willing to consider voluntary admission when a crisis occurs. Potential reasons for this could include greater awareness and acceptance that relapse indicators for admission are occurring, or greater confidence by the patient that their views and treatment preferences will be respected following admission, but future research in this area is required (see Box 1 Commentary).
The optimal models of crisis-planning interventions also require further investigation, including the extent of clinician involvement and ongoing monitoring required for interventions to be effective. One study included in this reviewReference Lay, Kawohl and Rossler22 incorporated relatively intensive ongoing monitoring within the intervention, but it is unclear the extent to which additional monitoring occurred in the other clinician-facilitated crisis-planning interventions. Fidelity to a core set of intervention components may enhance the effectiveness of crisis-planning interventions but stakeholder consultations and future comparison studies of different models of crisis-planning interventions are required to determine the most effective models. We only included interventions with a primary focus on crisis planning, meaning that broader self-management or recovery planning interventions with some overlap in content were excluded, but could be examined in future reviews.
Further trials of well-defined crisis plan models are desirable and large-scale naturalistic evaluations that may be more able to assess the effectiveness of crisis plans in practice with representative patient populations. Studies should also examine whether the effectiveness of crisis-planning interventions differs based on ethnicity, gender or other characteristics of patients. This was not examined in the majority of trials included in this review despite, for example, known higher risk of compulsory admissions among people from Black, Asian and minority ethnic backgrounds in England and other countries.Reference Bhui, Stansfeld, Hull, Priebe, Mole and Feder30,Reference Mulder, Koopmans and Selten31
Several studies faced challenges in the implementation of the crisis-planning intervention that may have limited their effectiveness. It is essential that future research examines and addresses these barriers to intended delivery, for example taking a behaviour-change perspective to address clinician engagement.
Box 1 Commentary by Patrick Nyikavaranda and Rachel Rowan Olive from the Lived Experience Working Group in the National Institute for Health Research Mental Health Policy Research Unit
It is reassuring that the study concludes with the observation that in some cases, crisis-planning interventions substantially reduce the risk of compulsory admissions. Better understanding of crisis planning among patients may increase willingness to plan.
It would be of note to see how the Triangle of Care (https://carers.org/article/triangle-care) can increase the likelihood of having carers and patients increase participation in joint crisis planning. However, it must be acknowledged that there are a lot of individuals who use services who do not want their carers involved in joint crisis planning, and provision should be given to support them as much as possible to take up crisis planning.
We note with caution that two studies showed an economic benefit. We hope that should larger studies on cost-effectiveness show that joint crisis planning brings about an economic benefit then those savings are invested into better and radical crisis support interventions, both pre- and post-crisis.
While a 25% decrease in compulsory admissions is significant, the lack of effect on overall and voluntary admissions also matters. Having experienced both voluntary and compulsory admissions, voluntary admissions are often de facto detentions – ‘Come in voluntarily or we will section you’ – lacking legal safeguards.
Further cause for caution comes from the scope of the systematic review – limited to patients with bipolar disorder or psychosis – and of the included studies. Although Black, Asian, minority ethnic patients are disproportionately likely to be detained, most studies did not break down results by ethnicity. Moreover, the three English studies largely pre-date austerity, the latest being Thornicroft et al (2013), the only study showing no impact on detentions. Detentions rose by 40% between 2004/5 and 2015/16 (https://www.cqc.org.uk/sites/default/files/20180123_mhadetentions_report.pdf); our experience is that compulsory admissions often relate directly to lack of resources, intersecting with specific needs. For instance, one author was sectioned despite consenting to admission to a community-based women's crisis house or women's ward as per her advance directive. Both were full; she was detained to a mixed-gender ward.
Significant further research is therefore needed before drawing firm conclusions from this review.
(P. Nyikavaranda and R. Rowan Olive, personal communication, 2019)
Funding
This paper is based on independent research commissioned and funded by the National Institute for Health Research Policy Research Programme, through the Mental Health Policy Research Unit. The views expressed are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research, the Department of Health and Social Care or its arm's length bodies, and other Government Departments.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2019.28.








eLetters
No eLetters have been published for this article.