Clinical trials identifier: Netherlands Trial Register, trial NL6049 (NTR6188):https://www.trialregister.nl/trial/6049.
Nursing home residents, like patients in hospitals, are at increased risk of developing infections from microorganisms such as norovirus and pneumonia-causing pathogens.Reference Juthani-Mehta and Quagliarello1 To avoid transmission of pathogens, the World Health Organization (WHO) recommends following their hand hygiene (HH) guidelines.2 We already knew that hand hygiene compliance (HHC) in hospitals and child care centers is often suboptimal, but we did not have much insight into (Dutch) nursing home compliance and what methods could increase compliance.Reference Zomer, Erasmus and Looman3,Reference Erasmus, Vos and Richardus4
Only a few rigorous HHC studies have been conducted in nursing homes.Reference Chuang, Tsang and Keung5–Reference Smith, Carusone and Loeb9 In a recent Cochrane review on HH interventions, 90 articles were considered for inclusion, and only 5 of these clearly referred to nursing home care, 3 of which had inadequate days of data collection.Reference Ho, Seto, Wong and Wong6,Reference Gould, Moralejo, Drey, Chudleigh and Taljaard10–Reference Vinci, Bunson, Govednik and McGuckin14 Although these studies showed that HHC could increase after an intervention, none were a large-scale study.
We hypothesized that HHC in Dutch nursing homes (skilled nursing facilities with residential care) could be increased through a multimodal intervention specifically designed for nursing homes. We developed the HANDSOME intervention using literature, interviews at nursing homes, and intervention mapping principles to identify relevant determinants, methods, and strategies.Reference Teesing, Erasmus and Petrignani15
The effect of this intervention in nursing home units in the Netherlands was assessed in a cluster randomized controlled trial. Here, we report the primary outcome measure of the trial: HHC of nurses to the WHO guidelines. The secondary outcome measure of the HANDSOME study, the incidence of healthcare associated infections in residents, will be reported elsewhere.
Methods
Trial design
The HANDSOME intervention is a cluster randomized controlled trial in Dutch nursing home units, designed to increase nurses’ HHC after a multimodal intervention. Nursing homes in the intervention arm received the intervention at a predetermined moment. Nursing homes in the control arm received no intervention. The trial was conducted from October 2016 through October 2017.
HHC was measured through unobtrusive direct observation. Observations took place during weekdays, starting at 8 a.m. and lasting ~4.5 hours. Observations started during the mornings because we expected to see the most care activities during this period and to observe the most nurses per unit. All measurements were recorded at the same time of day to foster homogeneity between the observations. At least 3 nurses were observed in every unit, each for a maximum of 1.5 hours. When there were <3 nurses working at the unit, either the observers continued observations at an additional ward (who also received the intervention if in the intervention arm) or they stopped observing. We did not necessarily observe the same nurses at every observation period; the goal was to see an overall behavioral change and not behavioral change per nurse. We also did not collect identifying information about the nurses so they would not be concerned about us reporting their behavior to their supervisors and therefore would exhibit their regular behavior. The turnover rate of nursing staff in the year before intervention commencement was 13% (n = 28 nursing home units). Nursing homes were observed at baseline (October 2016), after completion of the first lesson in the intervention units (February 2017), after completion of all lessons in the intervention units (May 2017), and 1 year after the baseline (October 2017) (Fig. 1).
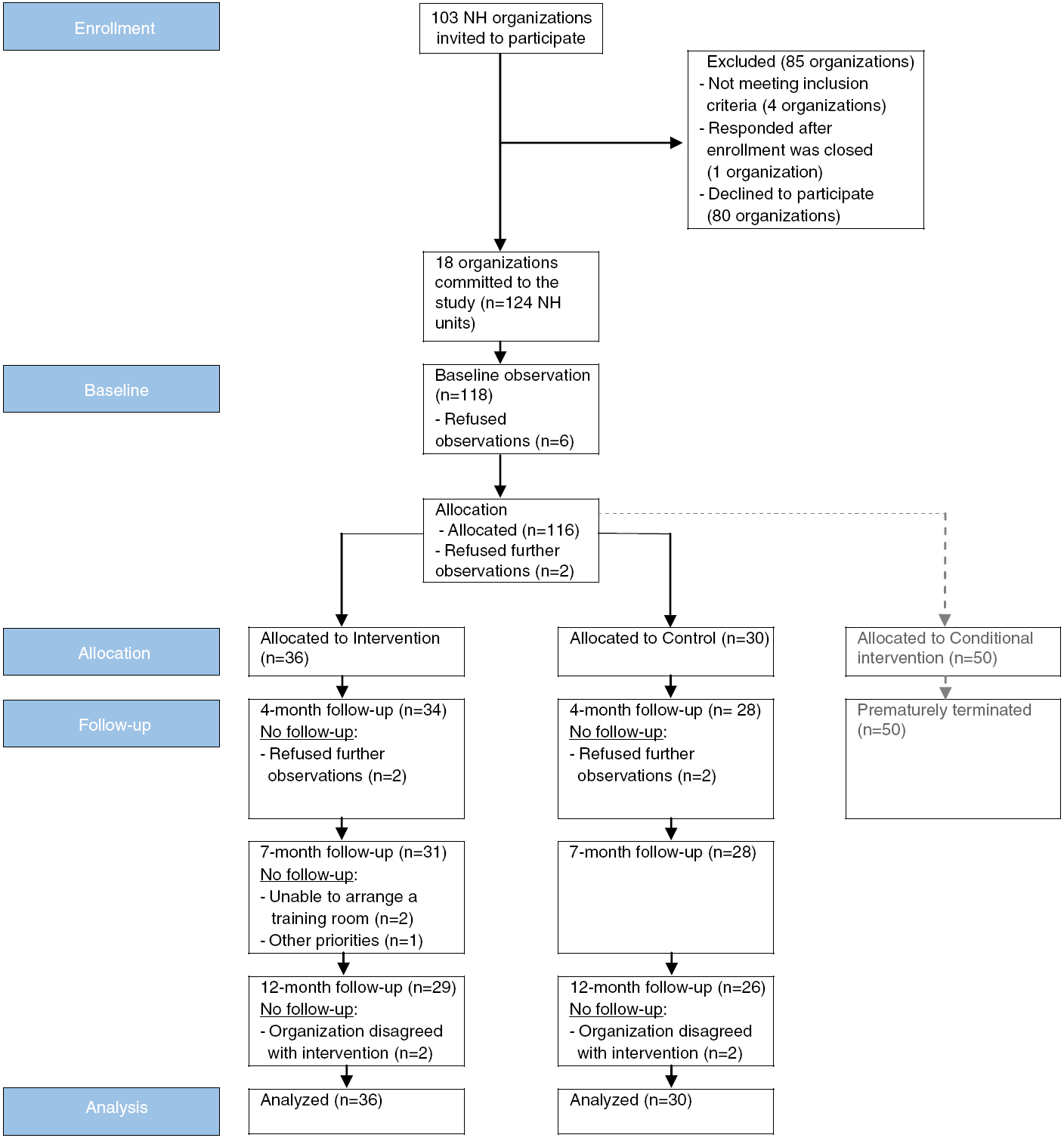
Fig. 1. Study design flow diagram.
All HHC opportunities were registered according to the WHO-defined HH moments (Fig. 2).2 HH was only registered as compliant if the HH occurred immediately before (ie, moments 1 and 2) or after (ie, moments 3, 4, and 5) an HH opportunity without touching another object, such as a door handle. HHC, along with at which HH moment it occurred, was registered in an application on a computer tablet. Consecutive opportunities, such as touching a resident (moment 1) and performing an aseptic task (moment 2) without any activity in between, were only registered once and according to a protocol (Fig. 2).
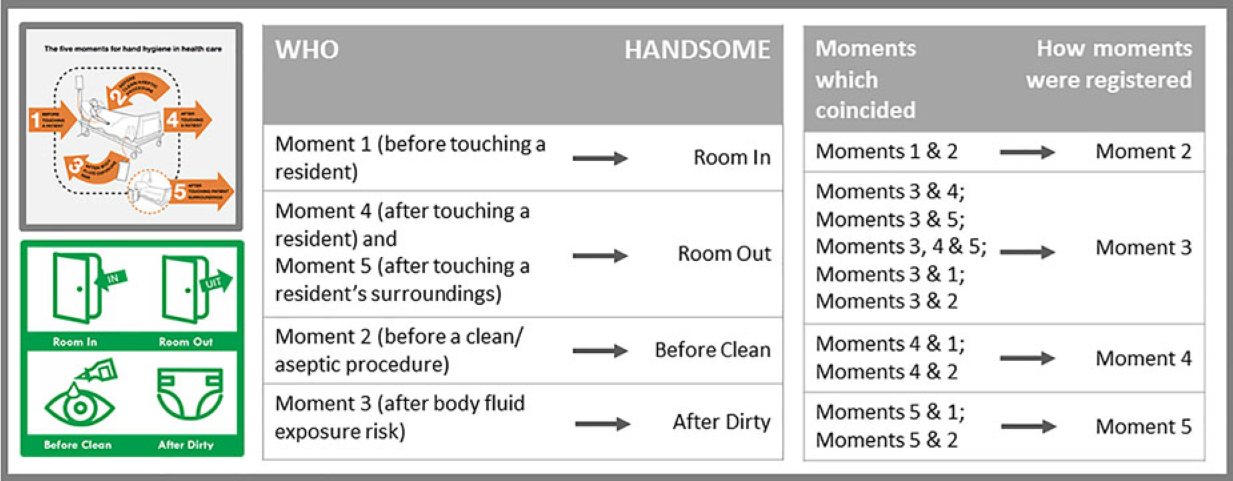
Fig. 2. Comparing the WHO method and the HANDSOME method and protocol for registering combined hand hygiene opportunities.
Study setting and eligibility criteria
We invited 103 nursing home organizations in 8 provinces in the Netherlands to participate in this study. The nursing homes were required to commit 2 nursing home units to the study. Study participants were nurses working in publicly funded skilled nursing facilities in the Netherlands providing intense psychogeriatric and/or somatic care to geriatric residents. Low-care residential facilities (verzorgingshuizen) were excluded from the study. Units were defined as one or multiple wards within a nursing home. When necessary, wards were linked to create units containing the minimum of 3 nurses working during the observation hours (8 a.m. to 1:30 p.m.). Nurses all attended or were attending a 3- or 4-year nursing program (verzorgenden or verpleegkundigen). HHC of other healthcare workers, residents, and visitors was not recorded.
Intervention
The HANDSOME intervention included activities for changing nursing home policy and individual behavior. Nursing home policy changes were achieved through an audit with explanations about HH materials and personal hygiene rules. Nurses and other healthcare workers were subject to 3 different live on-site HH lessons, access to an e-learning program, posters for the nursing home wards, and the opportunity to participate in an HH photo competition (Table 1). The details and background of this intervention can be found elsewhere.Reference Teesing, Erasmus and Petrignani15 During the lessons, nurses were taught the 5 moments of the WHO recommendations using a novel method, namely Room In (moment 1), Room Out (moments 4 and 5 combined), Before Clean (moment 2), and After Dirty (moment 3).Reference Teesing, Erasmus and Petrignani15 This method comprises the same 5 HH moments as the WHO standard, but it is more suitable for to the nursing home setting, is easy to remember (ie, 1 slogan), and is easy to visualize (Fig. 2). All intervention units participated in all aspects of the intervention, except those that withdrew from the study.
Table 1. Overview of Most Important HANDSOME Intervention Componentsa
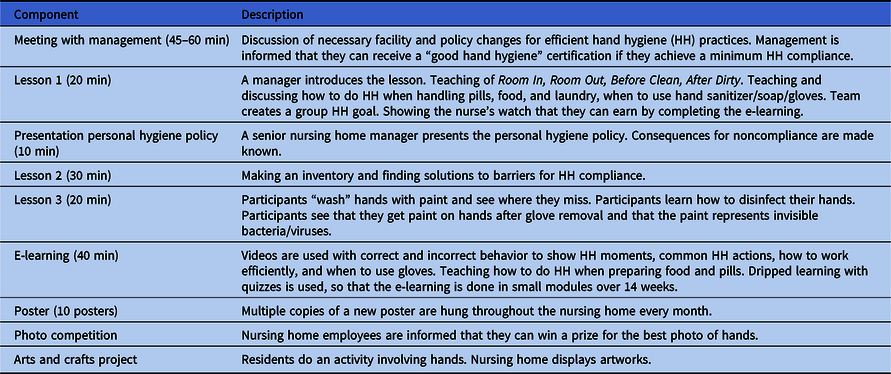
a The full intervention is outlined in Teesing et al.Reference Teesing, Erasmus and Petrignani15
Outcome measures
The primary outcome measure was HHC of nurses to the WHO guidelines. HHC is defined as the number of times that HH is performed at a WHO-defined HH opportunity, divided by the total number of times that it should be performed, expressed as a percentage. We registered HH as compliant if hand sanitizer was used, or soap, water, and a paper towel.
Sample size
The HH intervention was expected to increase HH compliance from 35% during the preintervention period to 50% in the postintervention period. We made a sample size calculation based on 80% power with a 2-sided α of 0.05, taking into account the clustering of observations within nursing homes, assuming an intraclass correlation of 0.1. We determined that a sample size of 15 participating nursing homes in each arm (30 units per arm) would be sufficient.
Randomization
The nursing home was the unit of randomization. Each nursing home was assigned an identification number and was then computer randomized to one of the arms by the primary investigator. All nursing homes in the control arm also had a nursing home from the same organization in the intervention arm. We used a cluster-randomized design because certain aspects of the intervention were aimed at the entire nursing home.
Blinding
It was not possible to blind the primary investigator to the intervention arm because this researcher also taught on-site lessons. Nurses were blinded by giving distinct names to the lessons (The New Way of Working) and the observations (HANDSOME), so that they appeared to be different projects. Furthermore, nurses were told that the observers were registering the frequency of health care activities, rather than HHC. HH observers were not informed which nursing homes received the intervention.
Statistical analyses
Background characteristics of all randomized nursing homes were tested for statistically significant differences between the study arms. We computed HHC for each arm for every observation round, as well as for the total follow-up. Analysis was on intention-to-treat basis through multilevel analyses, controlling for statistically significant differences (P < .05) in background characteristics between the study arms and for clustering of observations within nursing homes and nurses. We calculated odds ratios (ORs) for HHC in a multilevel model with 95% CIs, comparing baseline with each follow-up round and the total follow-up in each arm, and comparing the intervention and control arms at each round. Additionally, we calculated overall odds ratios comparing the increase in HHC in the intervention arm with the increase in the control arm. This was calculated for total HHC and per WHO-defined HH moment. HH moments before and after a HH-indicated activity were also statistically compared. We also examined the difference between nurse and student nurse HHC. All calculations were done in SPSS version 25 software (IBM, Armonk, NY).
Adjustments after commencement of the trial
This study originally had an additional “conditional” intervention arm to test a separate hypothesis that implementing a HH intervention following an infectious disease outbreak would have a higher and/or more sustained effect than implementation at a predetermined date, due to an increased sense of infection risk and urgency after an outbreak. The conditional arm was randomized, along with the control and conventional intervention arms, in November 2016, and received the same intervention as the conventional intervention arm, but only after an infectious disease outbreak.
In September 2017, we terminated the conditional intervention arm prematurely for the following reasons: (1) Two nursing homes in this arm were not able to implement the intervention after an outbreak because they had no funds for paying wages for employees to attend the lessons. (2) In 4 cases, the intervention would have taken place during a spring or summer holiday season, during which all available staff was needed at the wards. And (3) observers were not available for some projected observation periods. Due to the premature termination, only half of the nursing home units we aimed to include participated (15 instead of 30 nursing home units), and no 12-month follow-up observations were performed. We did not perform analyses of observations in this arm because we did not achieve the necessary cohort size and because of selection bias.
Ethical considerations
Ethical approval for the study was waived by the Medical Ethics Review Committee of Erasmus MC, University Medical Center Rotterdam (reference no. 58158) because it was not a medical-scientific investigation and because no experiments were conducted on human subjects. A manager at each nursing home approved the study before randomization, including observations. No identifying information was collected about the nurses or residents. We only observed nurses when the residents receiving care did not object to the observations.
Results
Nursing homes were recruited from April through August 2016, and 18 nursing home organizations joined the study, yielding 36 intervention units (938 beds) and 30 control units (865 beds) (Fig. 1). Reasons for dropout were refusal to admit observers, inability to schedule lessons in an appropriate room, other priorities, and disagreement with the intervention content.
We compared background characteristics between the study arms. The only statistically significant difference between the study arms was the size of the nursing home with the control arm having more large nursing homes (P = .01) (Table 2). The size variable was therefore incorporated in all multilevel calculations.
Table 2. Comparison of Baseline Characteristics Between Study Arms (n = 66 Nursing Home Units)
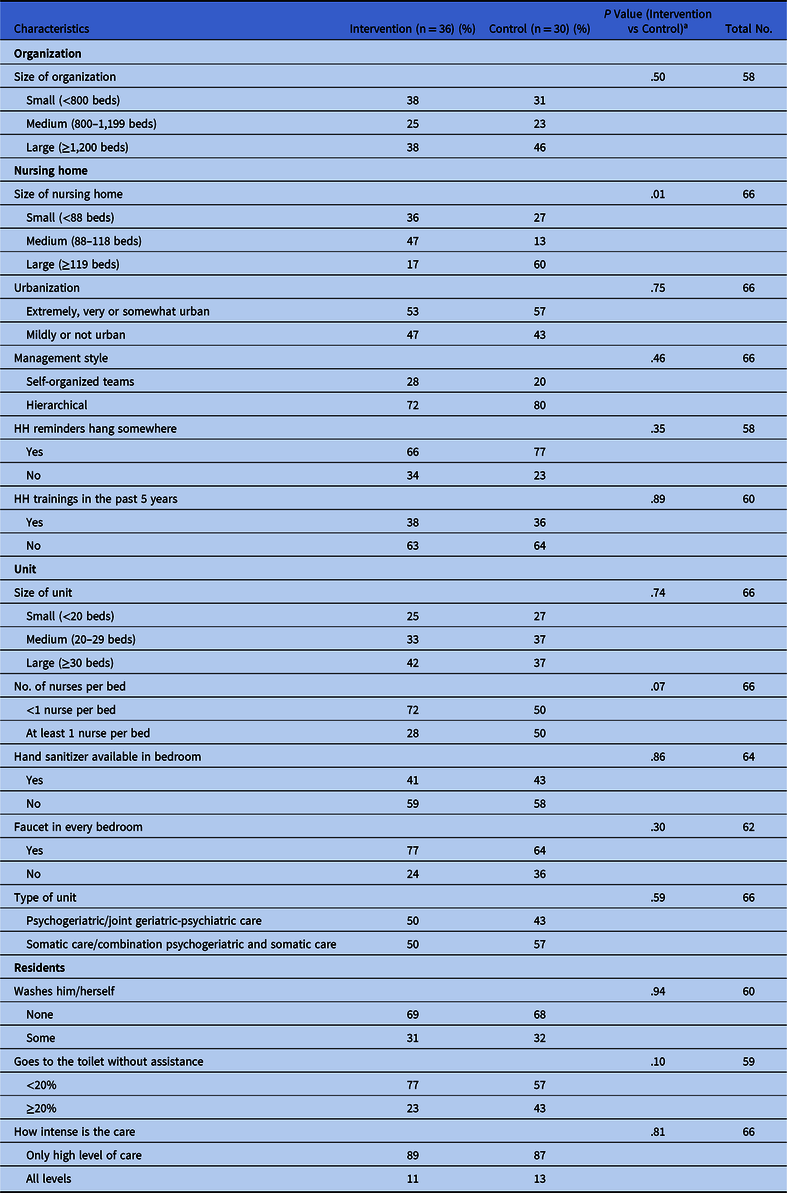
a Pearson χ2 test.
HHC increased over time in both study arms (Fig. 3): HHC increased from 12% to 36% in the intervention arm and from 13% to 21% in the control arm. The largest increase in HHC in the intervention arm occurred after the first lesson (at the 4-month follow-up), whereas the control arm steadily increased by 3% at every observation round.
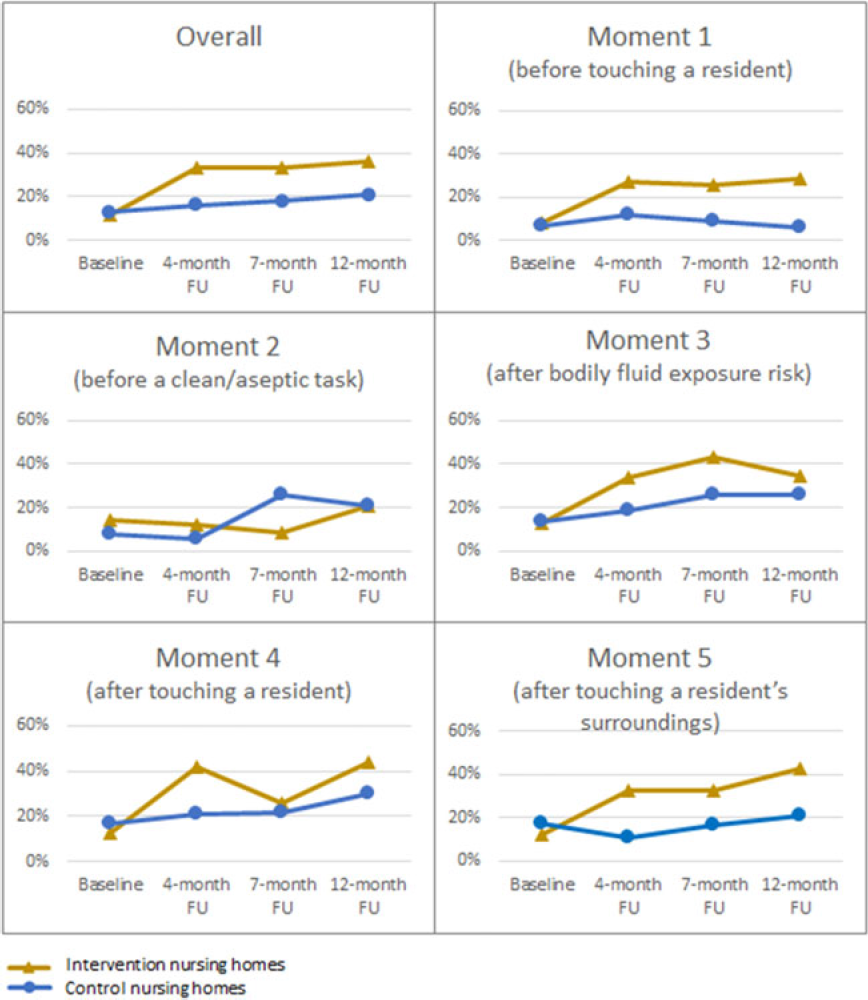
Fig. 3. Hand hygiene compliance and in nursing homes per trial arm during baseline and follow-up, overall and per WHO-moment.
We observed ~1,000 HH opportunities with 100 nurses per arm per observation round (Table 3), totaling 8,671 potential HH moments with 782 nurses, of which 17% were nursing students. We detected no significant difference in HHC at baseline between the study arms. For the intervention arm, HHC was statistically significantly higher during all follow-up measurements than at the baseline, and the OR increased gradually from 3.48 to 4.29. The control arm had a statistically significantly higher HHC during the 7- and 12-month follow-ups than at baseline, but with lower ORs than the intervention arm (ORs, 1.55 and 1.79, respectively). The control arm received no intervention; 60% of the nursing homes in the control arm took their own initiatives to increase HHC (data not shown). Overall, the intervention nursing homes showed a statistically significantly higher increase in HHC during the total follow-up versus the baseline period than the control nursing homes (OR, 2.28; 95% CI, 1.67–3.11).
Table 3. Hand Hygiene Compliance in Nursing Homes per Trial Arm, During Baseline and Follow-Up
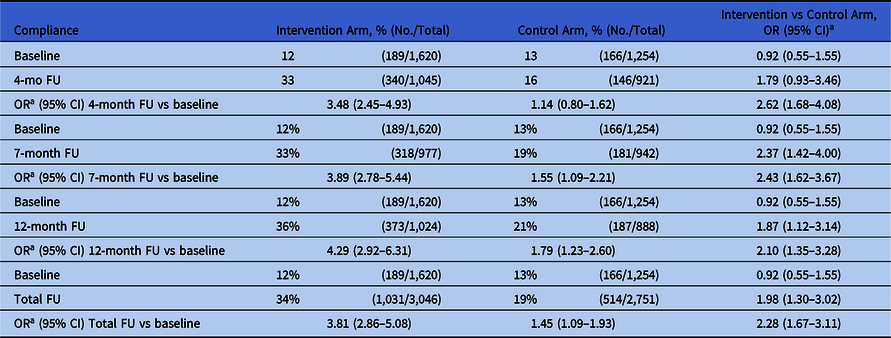
Note. OR, odds ratio; FU, follow-up.
a OR was corrected for size of the nursing homes as well as clustering of observations within nurses and nursing homes in a multilevel analysis. The intraclass correlation (ICC) for the level nurse was 0.25 and the ICC for the level nursing home was 0.01.
In the intervention arm, HHC increased for both nurses (from 12% to 34%) and students (from 11% to 32%). Similarly, we saw an increase in the control arm for both nurses (from 14% to 21%) and students (from 11% to 14%, data not shown).
HHC per WHO-defined moment during the 4 observation rounds is depicted in Figure 3. HHC increased more for the intervention arm than for the control arm for each moment, except for moment 2. HHC at moment 2 appeared random and retained a low compliance (with a low sample size).
For each of the 5 WHO-defined moments, we compared HHC for the total follow-up with the baseline measurement, for both arms (Table 4). HHC per WHO moment ranged from 8% to 14% at baseline, indications before an activity (moments 1 and 2) showing a lower HHC than indications after an activity (moments 3, 4, and 5) (OR, 2.05, 95% CI, 1.63–2.57, data not shown). We detected no statistically significant difference in HHC at baseline between the intervention and the control arms at each WHO moment. For the intervention arm, HHC statistically significantly increased (19%–25%) during follow-up versus baseline at 4 of the 5 WHO moments, except for the sparsely observed moment 2. HHC in the control arm increased significantly at moments 3 and 4. HHC was statistically significantly higher during follow-up at 3 of the 5 WHO moments in the intervention arm compared to the control arm. The largest increases in HHC in the intervention arm compared to the control arm occurred at moment 5 (OR, 3.30; 95% CI, 2.04–5.32) and moment 1 (OR, 3.20; 95% CI, 1.95–5.26). At follow-up, HHC for the intervention arm remained statistically significantly higher (OR, 1.93; 95% CI, 1.59–2.34) for indications after an activity (37% to 39%) than for indications before an activity (14% to 27%) (results not shown).
Table 4. Hand Hygiene Compliance in Nursing Homes per Trial Arm, During the 5 WHO-Defined Moments (n = 8,671 Hand Hygiene Opportunities)
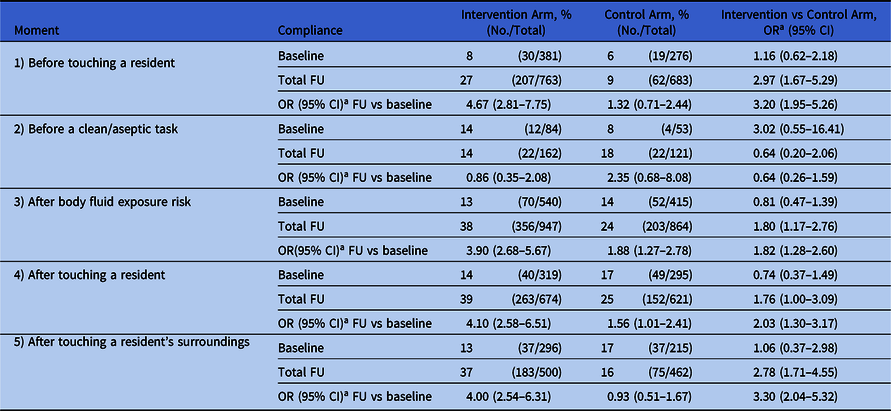
Note. WHO, World Health Organization; OR, odds ratio; CI, confidence interval; FU, follow-up.
a OR was corrected for size of the nursing homes as well as clustering of observations within nurses and nursing homes in a multilevel analysis. The intraclass correlation (ICC) for the level nurse was 0.25 and the ICC for the level nursing home was 0.01.
Discussion
The HANDSOME intervention demonstrates that a multimodal intervention can increase HH in nursing homes. Adherence to HH guidelines increased significantly during the intervention and remained higher 6 months after the intervention but remained suboptimal. HHC in the intervention arm increased significantly at 3 of the 5 HH moments compared to the control arm, and HHC was better after an HH-indicated activity than before an HH-indicated activity.
This study has several strengths: (1) It is one of the first randomized controlled HH trials in a nursing home. (2) It registers HH moments using direct observation. (3) It is a large-scale study, registering >8,500 HH opportunities. And (4) we studied the long-term effect of an HH intervention. The strengths of the HANDSOME intervention include the following: (1) It involves a minimum time commitment from the nurses for lessons. (2) It provides an audit of the prerequisites for HH at nursing homes. (3) It is tailored to nursing homes. And (4) it includes supplementation with online learning.
The study also has several limitations. We only observed HH on weekday mornings and early afternoons. HHC in all study arms may have been influenced by a national HH campaign in 2016–2017 for nursing homes.16–25 There may also have been some contamination from the intervention nursing homes to the control nursing homes, since all control nursing homes had a nursing home from the same organization in the intervention arm. Although the nursing homes in the control arm did not receive any intervention, 60% of nursing homes in the control group took their own action to increase HHC. Nevertheless, we saw better HHC in the intervention arm than in the control arm. Another possible limitation is bias. First, ward managers sometimes refused to keep observations blinded, so some nurses in both trial arms were informed of the purpose of the observations. Secondly, observers could figure out which units received the intervention if they saw the HANDSOME posters, causing potential observer bias. Lastly, the Hawthorne effect may have affected different nurses in different ways, depending upon the number of observation rounds that each nurse experienced.Reference Larson26 At the same time, because this is an RCT, we believe that the biases were generally equal in both arms, with the possible exception of observer bias.
In this study, HHC increased in the intervention group from 12% to 36%. The highest increase came directly after the first HH lesson. The continuation of the HH intervention (with expanded explanations and repetition) may have been instrumental in capturing a long-term effect and possibly a culture change, considering staff and student turnover.
Although HHC tripled, it remained well below the idealized 100%. At the same time, this is comparable with 3 other Dutch intervention studies in hospitals, which also had a low baseline compliance (20% to 22%) and yielded a 15%–33% increase in HHC.Reference Huis, Schoonhoven, Grol, Donders, Hulscher and van Achterberg27,Reference Beeck, Vos, Beeck, Boog, Erasmus and Polinder28
Studies in nursing homes outside the Netherlands showed a baseline compliance of 6% to 27%.Reference Chuang, Tsang and Keung5–Reference Smith, Carusone and Loeb9 Two of these studies also demonstrated the effectiveness of HH interventions (HHC increased from 6% to 46%, 27% to 61%, and 22% to 49%).Reference Chuang, Tsang and Keung5,Reference Ho, Seto, Wong and Wong6 Studies investigating the long-term effects of one-off HH interventions in nursing homes remain scarce.Reference Ho, Seto, Wong and Wong6
The 5 HH moments have distinctive infection prevention goals. Moments 1 and 2 prevent contamination not only from the nurse’s topical flora to the resident but also prevent contamination of microorganisms from other residents. Moment 2 is considered a high-risk moment for the resident because the nurse has contact with the resident’s open skin or mucous membranes.29 Moments 3, 4, and 5 prevent contamination from the resident to the nurse. Moment 3 is also important for the resident because it reduces the chance of microorganisms going from a colonized site on the resident to a noncolonized site. In the literature, primarily regarding hospital care, moment 4 generally has the highest compliance, followed by moment 3.29–Reference Kuruno, Kasahara and Mikasa38 These are both moments after an HH-indicated activity. These moments may be prioritized because the healthcare provider wants to protect himself or herself.
In the HANDSOME intervention, the highest compliance at baseline occurred at moment 4, followed by moment 5, the two moments that protect the healthcare provider and prevent the spread of disease to other residents. These results are comparable to results from other Dutch studies showing that HHC is better after a HH-indicated activity than before such an activity.Reference Zomer, Erasmus and Looman3,Reference Erasmus, Vos and Richardus4,Reference Liu, Liang, Wu and Chuang7
A few other intervention studies distinguished differences in HHC at the different HH moments, although none of these studies had a control arm.Reference Grayson, Stewardson and Russo35–Reference Kuruno, Kasahara and Mikasa38 The HHC in the HANDSOME intervention was consistently low for all moments at baseline, whereas the other studies showed high fluctuations among the different moments.29,Reference Grayson, Stewardson and Russo35–Reference Kuruno, Kasahara and Mikasa38 The largest gains in other studies were generally at moments 1 and 5. In our study, the largest differences between the control and intervention arms occurred in the follow-up period at moments 1 and 5, but the largest absolute gains in the intervention arm occurred at moments 3, 4, and 5.
In conclusion, the HANDSOME intervention yielded a substantial increase in HHC 4 months after the beginning of the intervention, and this improvement was sustained in the long term. Part of its success may be due to our slogan: Room In, Room Out, Before Clean, After Dirty. This slogan is easy to remember, evokes imagery, and contains all the WHO moments. Nursing homes can easily implement the intervention, and it requires little time commitment from the nurses. Because we included a balanced mix of large and small nursing homes and in urban and nonurban settings, we believe that our results could be duplicated in other nursing homes.
Acknowledgments
We thank Jennifer Bloem for her coordination work and assisting in the observer training. We also thank Elise Van Beeck for assisting with detailed specifications of the hand hygiene moments, and we thank the nursing homes for allowing us to perform this RCT.
Financial support
This study was funded by the Netherlands Organization for Health Research and Development (ZonMw, grant no. 522002010). Essity provided small bottles of sanitizer for the hand hygiene lessons during the study.
Conflicts of interest
The authors state that they have no conflict of interests related to this article.










