Introduction
Early detection and treatment of clinical high-risk for psychosis (CHR-P) states are not only relevant for preventing the onset of the first episode of psychosis, but also for achieving remission of CHR-P symptoms and other comorbidities, and for avoiding impairments in psychosocial functioning (Addington et al., Reference Addington, Stowkowy, Liu, Cadenhead, Cannon, Cornblatt, McGlashan, Perkins, Seidman, Tsuang, Walker, Bearden, Mathalon, Santesteban-Echarri and Woods2019; Caballero et al., Reference Caballero, Machiraju, Diomino, Kennedy, Kadivar and Cadenhead2023; Campion et al., Reference Campion, Bhui and Bhugra2012; Schmidt et al., Reference Schmidt, Schultze-Lutter, Schimmelmann, Maric, Salokangas, Riecher-Rössler, van der Gaag, Meneghelli, Nordentoft, Marshall, Morrison, Raballo, Klosterkötter and Ruhrmann2015; Schultze-Lutter and Meisenzahl, Reference Schultze-Lutter and Meisenzahl2023; Worthington and Cannon, Reference Worthington and Cannon2021). In clinical samples, many CHR-P patients who do not develop psychosis within follow-up – so-called ‘non-converters’ – do not experience remission from CHR-P symptoms. Furthermore, they continue to suffer from non-psychotic mental disorders at follow-up – mainly mood and anxiety disorders – (Beck et al., Reference Beck, Andreou, Studerus, Heitz, Ittig, Leanza and Riecher-Rössler2019), which are the most frequent comorbid disorders reported for CHR-P states at baseline (Solmi et al., Reference Solmi, Soardo, Kaur, Azis, Cabras, Censori, Fausti, Besana, de Pablo G and Fusar-Poli2023). Irrespective of comorbidities, half of clinical CHR-P samples show a poor psychosocial outcome (Carrión et al., Reference Carrión, McLaughlin, Goldberg, Auther, Olsen, Olvet, Correll and Cornblatt2013; Lin et al., Reference Lin, Wood, Nelson, Beavan, McGorry and Yung2015), even when CHR-P symptoms remit (Addington et al., Reference Addington, Stowkowy, Liu, Cadenhead, Cannon, Cornblatt, McGlashan, Perkins, Seidman, Tsuang, Walker, Bearden, Mathalon, Santesteban-Echarri and Woods2019), with CHR-P state at follow-up (either newly developed or maintained) being associated with significantly lower functioning (Lin et al., Reference Lin, Wood, Nelson, Beavan, McGorry and Yung2015; Michel et al., Reference Michel, Ruhrmann, Schimmelmann, Klosterkötter and Schultze-Lutter2018a; Schmidt et al., Reference Schmidt, Schultze-Lutter, Schimmelmann, Maric, Salokangas, Riecher-Rössler, van der Gaag, Meneghelli, Nordentoft, Marshall, Morrison, Raballo, Klosterkötter and Ruhrmann2015). Therefore, regardless of conversion, the CHR-P state itself clearly possesses clinical significance warranting support and care in help-seeking individuals (Fusar-Poli et al., Reference Fusar-Poli, Salazar de Pablo, Correll, Meyer-Lindenberg, Millan, Borgwardt, Galderisi, Bechdolf, Pfennig, Kessing, van Amelsvoort, Nieman, Domschke, Krebs, Koutsouleris, McGuire, Do and Arango2020; Ruhrmann et al., Reference Ruhrmann, Schultze-Lutter and Klosterkötter2010; Solmi et al., Reference Solmi, Soardo, Kaur, Azis, Cabras, Censori, Fausti, Besana, de Pablo G and Fusar-Poli2023).
A challenge to the understanding of CHR-P states and their course is the heterogeneous clinical picture. This difficulty has been tackled by various methods, from identifying specific risk profiles linked to neural mechanisms, to building multivariate models that predict heterogeneous outcomes (Caballero et al., Reference Caballero, Machiraju, Diomino, Kennedy, Kadivar and Cadenhead2023; Solmi et al., Reference Solmi, Soardo, Kaur, Azis, Cabras, Censori, Fausti, Besana, de Pablo G and Fusar-Poli2023; Worthington and Cannon, Reference Worthington and Cannon2021). A common method to parse out heterogeneity by way of clinical profiles is latent class analysis (LCA) (Healey et al., Reference Healey, Penn, Perkins, Woods, Keefe and Addington2018; Ryan et al., Reference Ryan, Addington, Bearden, Cadenhead, Cornblatt, Mathalon, McGlashan, Perkins, Seidman, Tsuang, Woods, Cannon and Walker2018; Valmaggia et al., Reference Valmaggia, Stahl, Yung, Nelson, Fusar-Poli, McGorry and McGuire2013; van Tricht et al., Reference van Tricht, Bour, Koelman, Derks, Braff, de Wilde, Boerée, Linszen, de Haan and Nieman2015). Considered a ‘person-centred’ approach to reduce heterogeneity, LCA operates on the notion of finding ‘hidden’ homogenous groups within heterogeneous populations (Rosato and Baer, Reference Rosato and Baer2012). Studies applying LCA to clinical CHR-P samples generally used baseline data only, and characterized groups by transition rates to psychosis, while other relevant outcomes (e.g., non-psychotic mental disorders) were not considered (Healey et al., Reference Healey, Penn, Perkins, Woods, Keefe and Addington2018; Ryan et al., Reference Ryan, Addington, Bearden, Cadenhead, Cornblatt, Mathalon, McGlashan, Perkins, Seidman, Tsuang, Woods, Cannon and Walker2018; Valmaggia et al., Reference Valmaggia, Stahl, Yung, Nelson, Fusar-Poli, McGorry and McGuire2013; van Tricht et al., Reference van Tricht, Bour, Koelman, Derks, Braff, de Wilde, Boerée, Linszen, de Haan and Nieman2015). They have reported between two and five classes differing in parameters included for class selection (e.g., only positive symptoms or additional negative symptoms, or neurophysiological parameters) (Healey et al., Reference Healey, Penn, Perkins, Woods, Keefe and Addington2018; Ryan et al., Reference Ryan, Addington, Bearden, Cadenhead, Cornblatt, Mathalon, McGlashan, Perkins, Seidman, Tsuang, Woods, Cannon and Walker2018; Valmaggia et al., Reference Valmaggia, Stahl, Yung, Nelson, Fusar-Poli, McGorry and McGuire2013; van Tricht et al., Reference van Tricht, Bour, Koelman, Derks, Braff, de Wilde, Boerée, Linszen, de Haan and Nieman2015). To date, no study has attempted to determine if and how people might change class membership between baseline and follow-up, or examined stability of classes over time. Moreover, earlier studies were carried out in selected samples of only, or mostly, help-seeking CHR-P patients defined exclusively by ultra-high risk (UHR) criteria, who commonly receive treatment (Healey et al., Reference Healey, Penn, Perkins, Woods, Keefe and Addington2018; Ryan et al., Reference Ryan, Addington, Bearden, Cadenhead, Cornblatt, Mathalon, McGlashan, Perkins, Seidman, Tsuang, Woods, Cannon and Walker2018; Valmaggia et al., Reference Valmaggia, Stahl, Yung, Nelson, Fusar-Poli, McGorry and McGuire2013; van Tricht et al., Reference van Tricht, Bour, Koelman, Derks, Braff, de Wilde, Boerée, Linszen, de Haan and Nieman2015) and who must therefore be assumed a non-representative minority of the CHR-P population. Consequently, the classes and natural course (i.e., potentially without treatment) of clinician-assessed CHR-P symptoms in the wider community using the whole spectrum of CHR-P criteria and symptoms, i.e., both UHR and basic symptom (BS) criteria (Schultze-Lutter et al., Reference Schultze-Lutter, Michel, Schmidt, Schimmelmann, Maric, Salokangas, Riecher-Rössler, van der Gaag, Nordentoft, Raballo, Meneghelli, Marshall, Morrison, Ruhrmann and Klosterkötter2015), is largely unknown.
To address this gap in knowledge (van Os et al., Reference van Os, Schaub and Carpenter2021), the aims of this study were twofold. First, to ascertain CHR-P symptom-based classes of community participants using the whole spectrum of CHR-P symptoms (i.e., attenuated (APS) and brief intermittent psychotic symptoms (BIPS) and criteria-relevant BS), and to examine their clinical and socio-demographic correlates. Second, to explore the stability of these classes longitudinally; specifically, to determine how class membership itself might change, or how individuals might ‘move between’ baseline and follow-up classes.
Methods
Participants
The sample included participants from both the baseline and follow-up assessments of the ‘Bern Epidemiological At-Risk’ (BEAR) study (Schultze-Lutter et al., Reference Schultze-Lutter, Michel, Ruhrmann and Schimmelmann2018, Reference Schultze-Lutter, Schimmelmann and Michel2021; for further details, see eTexts 1, 2). At baseline, we evaluated CHR-P symptoms and criteria in a representative random sample of the 16- to 40-year-old Bernese community (N = 2,683; response rate: 63.4%), using procedures comparable with clinical assessment (Schultze-Lutter et al., Reference Schultze-Lutter, Michel, Schmidt, Schimmelmann, Maric, Salokangas, Riecher-Rössler, van der Gaag, Nordentoft, Raballo, Meneghelli, Marshall, Morrison, Ruhrmann and Klosterkötter2015). A selected, CHR-P symptom-enriched sample (N = 834; response rate: 66.4%) was followed up approximately 3 years later, and only the N = 829 non-converters were included in the present analyses (Schultze-Lutter et al., Reference Schultze-Lutter, Schimmelmann and Michel2021). For a detailed overview of the participant selection process, including reasons for exclusion, please refer to Fig. 1. Participation was voluntary and required informed consent at each time point. The human research ethics committee of Canton Bern approved the study (ID PB_2018-00132).

Figure 1. Flowchart of participant recruitment, selection and follow-up in the BEAR study.
Assessments
CHR-P symptoms (eTable 1) were assessed using semi-structured interviews with good interrater reliability (McGlashan et al., Reference McGlashan, Cannon, Walsh and Woods2010; Schultze-Lutter et al., Reference Schultze-Lutter, Addington and Rurhmann2007). The Structured Interview for Psychosis-Risk Syndromes (SIPS) (McGlashan et al., Reference McGlashan, Cannon, Walsh and Woods2010) was used for UHR symptoms, i.e., five APS/BIPS, and the Schizophrenia Proneness Instrument, Adult version (Schultze-Lutter et al., Reference Schultze-Lutter, Addington and Rurhmann2007) for the 14 BS included in the two BS criteria (Schultze-Lutter et al., Reference Schultze-Lutter, Michel, Schmidt, Schimmelmann, Maric, Salokangas, Riecher-Rössler, van der Gaag, Nordentoft, Raballo, Meneghelli, Marshall, Morrison, Ruhrmann and Klosterkötter2015). For the present analyses, CHR-P symptoms were defined by the presence of APS or BIPS, and/or criteria-relevant BS at baseline, irrespective of the onset/worsening and/or frequency requirements of related CHR-P criteria. The five positive SIPS-items were recoded into binary items: 1 (presence) was assigned to scores between 3 and 6 (indicating presence of APS or BIPS) and 0 (absence) to scores between 0 and 2 (indicating absence of APS and BIPS). Similarly, BS-scores between 1 and 6, and 8 (indicating presence of BS) were recoded as 1 (presence), while 0 (absence) was assigned to BS-scores of 0, 9 and 7 (respectively indicating absence of BS, their only questionable presence, or that the symptom has always been present in the same frequency, making it a trait feature, not a BS). Present DSM-IV non-substance-related axis-I disorders, including affective, anxiety (including specific phobia), eating, somatoform, obsessive-compulsive and post-traumatic stress disorder were assessed using the Mini-International Neuropsychiatric Interview (Sheehan et al., Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs, Weiller, Hergueta, Baker and Dunbar1998), which was previously successfully applied in telephone interviews of community samples, demonstrating good reliability, concurrent and predictive validity (Schultze-Lutter et al., Reference Schultze-Lutter, Michel, Ruhrmann and Schimmelmann2018; Sheehan et al., Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs, Weiller, Hergueta, Baker and Dunbar1998; Wang et al., Reference Wang, Adair and Patten2006).
Clinician-rated global level of psychosocial functioning, independent of overall symptom severity, was estimated on the Social and Occupational Functioning Assessment Scale (SOFAS; American Psychiatric Association (APA), 1994), which showed good psychometric properties, including good interrater reliability and construct validity (Hilsenroth et al., Reference Hilsenroth, Ackerman, Blagys, Baumann, Baity, Smith, Price, Smith, Heindselman, Mount and Holdwick2000; Rybarczyk, Reference Rybarczyk, Kreutzer, Deluca and Caplan2011). Over a 0–100 range, lower SOFAS-scores represent lower functioning, with a score of ≤70 indicating presence of a functional deficit (American Psychiatric Association (APA), 1994; Morosini et al., Reference Morosini, Magliano, Brambilla, Ugolini and Pioli2000; Schimmelmann et al., Reference Schimmelmann, Michel, Martz-Irngartinger, Linder and Schultze-Lutter2015; Michel et al., Reference Michel, Schnyder, Schmidt, Groth, Schimmelmann and Schultze-Lutter2018b).
Statistical analyses
Analyses were conducted in R (Version 4.2) and RStudio (Version 2022.07.0). To identify the best fitting LCA model for each assessment point, different models were estimated, and subsequent classes were added using the R package poLCA (Linzer and Lewis, Reference Linzer and Lewis2011). For each model, the Akaike Information Criterion (AIC), the Bayesian Information Criterion (BIC) and the relative entropy were calculated. Lower AIC and BIC values indicate better fit, and higher entropy values indicate better accuracy with the defined classes (Weller et al., Reference Weller, Bowen and Faubert2020). After identifying the best-fitting LCA model for both baseline and follow-up data, each individual was assigned to a specific class based on the probabilities of class membership obtained from the analysis.
Differences between classes regarding ratio data and categorical variables were tested using ANOVAs and chi-squared tests, respectively. Effect sizes were calculated using eta-square and Cramer’s V. Significant ANOVAs were additionally tested using pairwise Bonferroni corrected comparisons. For significant chi-squared tests, the standardized residuals (≥|1.96|) were calculated as a measure of significant cell difference between observed and expected values.
Results
Sample characteristics at baseline and follow-up
The mean follow-up time was 40.60 months (SD = 8.35, Mdn = 39.00, range: 21.00–68.00). Participants were on average 29.8 years old at baseline and 33.3 years old at follow-up (eTable 2). At both time points, the sample was 53.2% female, predominantly Swiss and in regular employment (>95%), with most participants (84.1%) pursuing or holding moderate to high educational qualifications (ISCED ≥ 4); roughly half of the sample was single (eTable 2). At both time points, the proportion of participants with a functional deficit remained stable at around 7%, while the rate of axis-I disorders significantly decreased from 17.0% at baseline to 13.3% at follow-up, primarily due to reductions in affective and other disorders (e.g., eating disorders, somatoform disorders; eTable 2). All symptoms decreased in number over time or maintained a low frequency (eTable 2), except for perceptual symptoms, which showed an increase at follow-up (eTable 2).
LCA at baseline
At baseline, three LCA models were tested and compared by goodness of fit.
Although a two-class solution showed the best BIC, which is generally considered the most reliable fit statistic in LCA (Sinha et al., Reference Sinha, Calfee and Delucchi2021; Weller et al., Reference Weller, Bowen and Faubert2020), its AIC and entropy value were the poorest. Therefore, the two-class solution was discarded.
Overall, the best fitting model was a three-class solution (eTable 3), showing the lowest AIC, the second-lowest BIC and the second-highest entropy (Fig. 2a), indicating clear separation between the classes. Classes 1 and 2 of the three-class solution were mostly characterized by a high probability of BS and of APS/BIPS, respectively. Class 3 was characterized by a low probability of any CHR-P symptom (Fig. 2a).

Figure 2. Latent class profiles of basic symptoms and (attenuated) psychotic symptoms at baseline (a) and follow-up (b).
Baseline characteristics of the Baseline Classes
Baseline Class 1 was the smallest (n = 19, 2.3%), including participants who, compared to the other classes, showed the highest rate of lower education level as well as unemployment or sheltered/temporary employment. Additionally, they showed high rates of functional impairment and were the most affected by axis-I disorders (Table 1). In comparison, Baseline Class 2 was slightly bigger (n = 25, 3.0%), comprising individuals with similar rates of functional impairment, but fewer, although still frequent, axis-I disorders (Table 1). Baseline Class 2 members were also the oldest, and least likely to be single. Finally, Baseline Class 3 was the largest (n = 785, 94.7%), characterized by the highest rate of regular full-time/part-time employment, and the lowest rates of psychosocial deficits, axis-I disorders and divorce (Table 1).
Table 1. Baseline socio-demographic and clinical characteristics of the three Baseline Classes (N = 829)

Note: SOFAS: Social and Occupational Functioning Assessment Scale.
In [bold], cells with standardized residuals ≥|1.96|. This equals significant deviation from the expected cell frequency. An adjusted residual of 1.96 indicates that the number of cases in that cell is significantly larger than would be expected if the null hypothesis were true, with a significance level of 0.05. An adjusted residual that is <−1.96 indicates that the number of cases in that cell is significantly smaller than would be expected if the null hypothesis were true.
P: positive-symptom scale; BS: basic symptom.
There were no differences between the Baseline Classes in terms of sex, nationality or family history of mental disorders.
Follow-up characteristics of the Baseline Classes
At follow-up, participants in Baseline Class 1 continued to show the highest rates of unemployment or sheltered/temporary employment, lower education level and axis-I disorders. Newly, they showed the highest rates of functional impairment (Table 2). Baseline Class 2 remained the oldest, showing intermediate rates of functional deficits and any axis-I disorder. Among its members, rates of regular full- or part-time employment decreased compared to baseline, while other types of employment were now highly frequent (Table 2). Finally, participants in Baseline Class 3 continued to report the highest levels of education and regular full- or part-time employment, as well as the lowest rates of axis-I disorders and functional impairment (Table 2).
Table 2. Follow-up socio-demographic and clinical characteristics of the three Baseline Classes (N = 829)
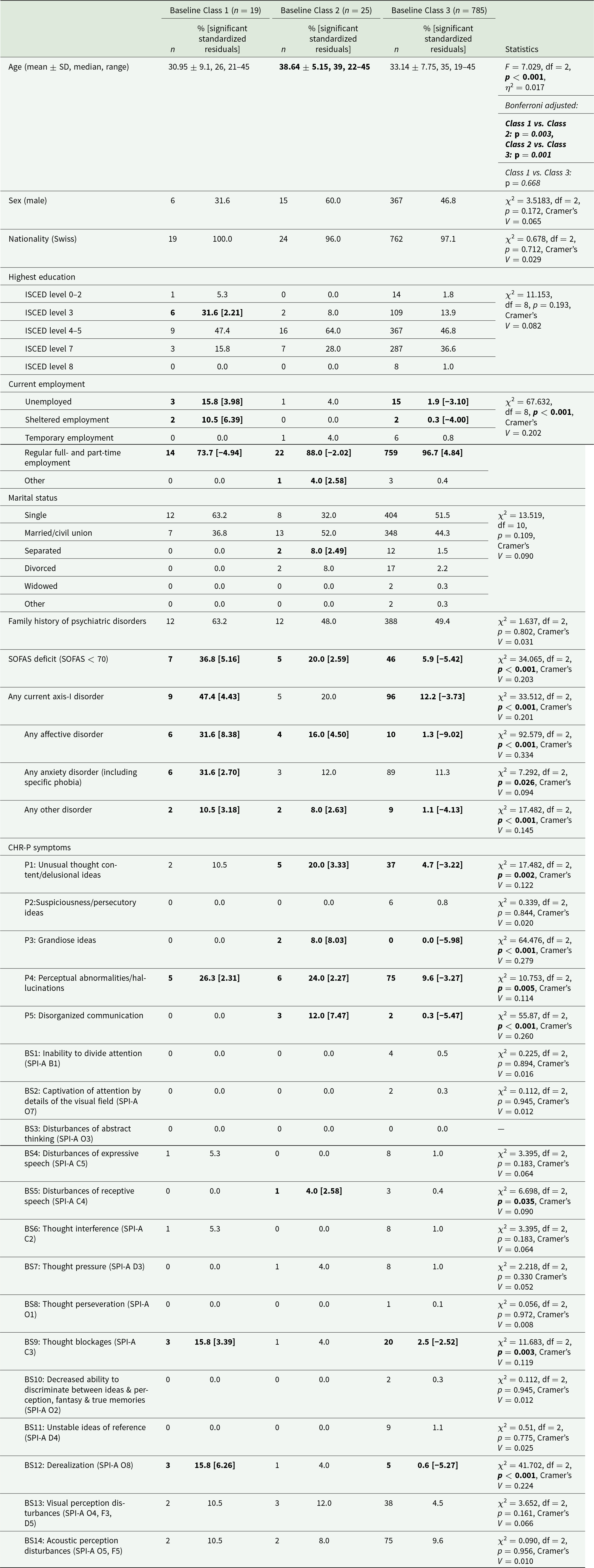
Note: SOFAS: Social and Occupational Functioning Assessment Scale.
In [bold], cells with standardized residuals ≥|1.96|. This equals significant deviation from the expected cell frequency. An adjusted residual of 1.96 indicates that the number of cases in that cell is significantly larger than would be expected if the null hypothesis were true, with a significance level of 0.05. An adjusted residual that is <−1.96 indicates that the number of cases in that cell is significantly smaller than would be expected if the null hypothesis were true.
P: positive-symptom scale; BS: basic symptom.
New LCA for the follow-up time point
For the follow-up data, three new LCA models were tested and compared by goodness of fit.
Again, a three-class solution was the best fitting model, showing the lowest AIC and BIC values, yet had relatively low relative entropy (see eTable 4, Fig. 2b), indicating higher within-classes homogeneity at this time point compared to baseline.
Follow-up characteristics of Follow-up Classes
Overall, Follow-up Class 1 (6.3% of sample) resembled Baseline Class 1, showing the highest rates of lower education and axis-I disorders. However, Follow-up Class 1 members showed only an intermediate rate of functional deficits and had the highest rate of separated persons (Table 3). With the exception of four BS, they showed a high likelihood of perceptual and cognitive BS, and of perceptual abnormalities/hallucinations (P4).
Table 3. Follow-up socio-demographic and clinical characteristics of the three Follow-up Classes (N = 829)
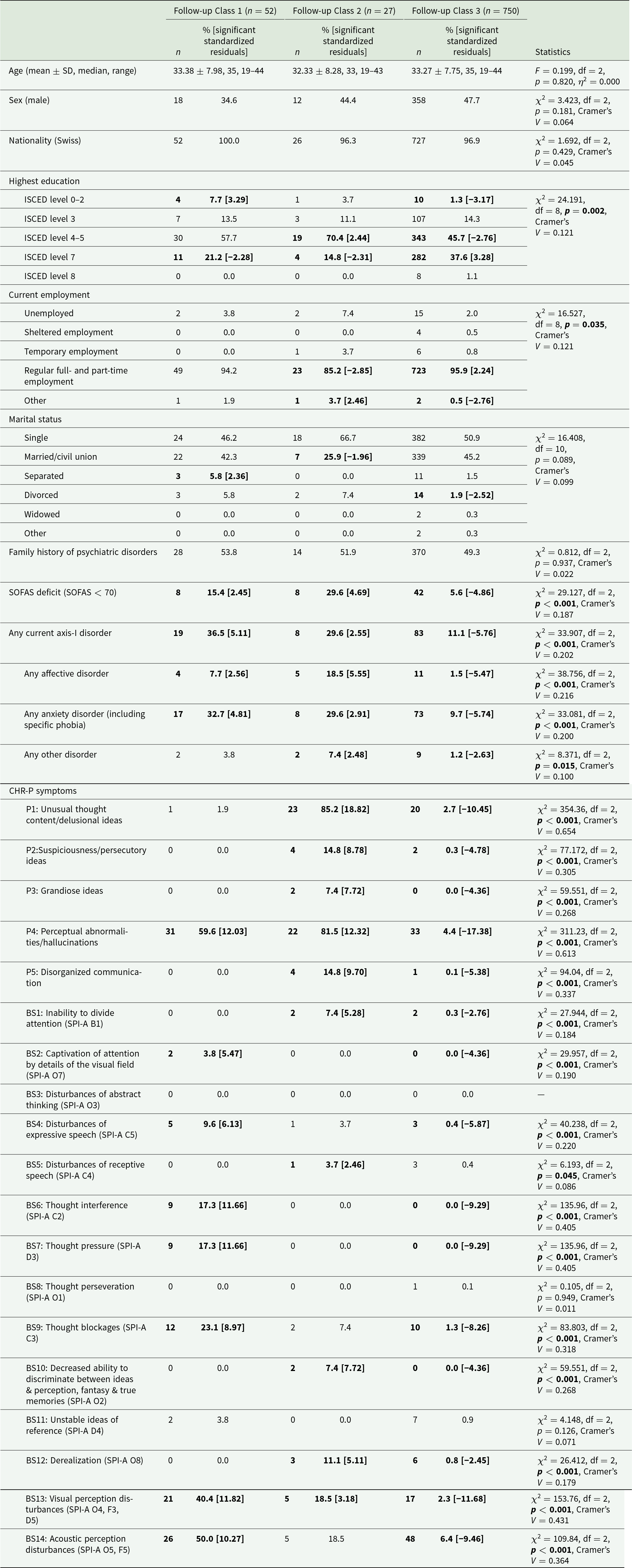
Note: SOFAS: Social and Occupational Functioning Assessment Scale.
In [bold], cells with standardized residuals ≥|1.96|. This equals significant deviation from the expected cell frequency. An adjusted residual of 1.96 indicates that the number of cases in that cell is significantly larger than would be expected if the null hypothesis were true, with a significance level of 0.05. An adjusted residual that is <−1.96 indicates that the number of cases in that cell is significantly smaller than would be expected if the null hypothesis were true.
P: positive-symptom scale; BS: basic symptom.
Follow-up Class 2 (3.3% of sample) partially resembled Baseline Class 2, showing an intermediate rate of axis-I disorders and the highest probability of all APS/BIPS at follow-up (Table 3). In contrast with Baseline Class 2, members of Follow-up Class 2 additionally had the highest probability of exhibiting four BS (inability to divide attention, disturbance of receptive speech, derealization and decreased ability to discriminate between ideas & perception, fantasy & true memories), as well as an elevated rate of visual perception disturbances, which was, however, still lower than in Follow-up Class 1. Further, they showed the highest rates of psychosocial deficits among Follow-up Classes, as well as the lowest rate of regular full- and part-time employment, and of married persons (Table 3). Overall, Follow-up Class 2 had a moderate educational level.
Aligning with Baseline Class 3, Follow-up Class 3 was the largest (90.5% of sample), showing a low probability of CHR-P symptoms (Fig. 2b), along with the lowest rates of psychosocial deficits and axis-I disorders among Follow-up Classes. Moreover, Follow-up Class 3 had the highest rate of regular employment, the lowest divorce rate and, newly, the highest educational level (Table 3).
Finally, similarly to Baseline Classes, the Follow-up Classes did not differ in distribution of sex, nationality, or family history of mental disorders, and, additionally, also not in age.
Movement between classes from baseline to follow-up
In absolute terms, more participants (n = 79) were included in the two more impaired Classes 1 and 2 at follow-up than had been at baseline (n = 44). However, less than a quarter (n = 8) of Baseline Class 1 or 2 members stayed in, or moved to, the corresponding Follow-up Classes 1 or 2. Instead, the majority of participants in the more impaired Baseline Classes 1 and 2 (73.7% and 88.0%, respectively) moved to the ‘healthy’ Follow-up Class 3, which still included most (91.0%) members of the ‘healthy’ Baseline Class 3 (Fig. 3). In contrast, 9.0% of members (n = 71) of the least impaired Baseline Class 3 moved to the more impaired Follow-up Classes 1 or 2 (6.1% and 2.9%, respectively; Fig. 3).
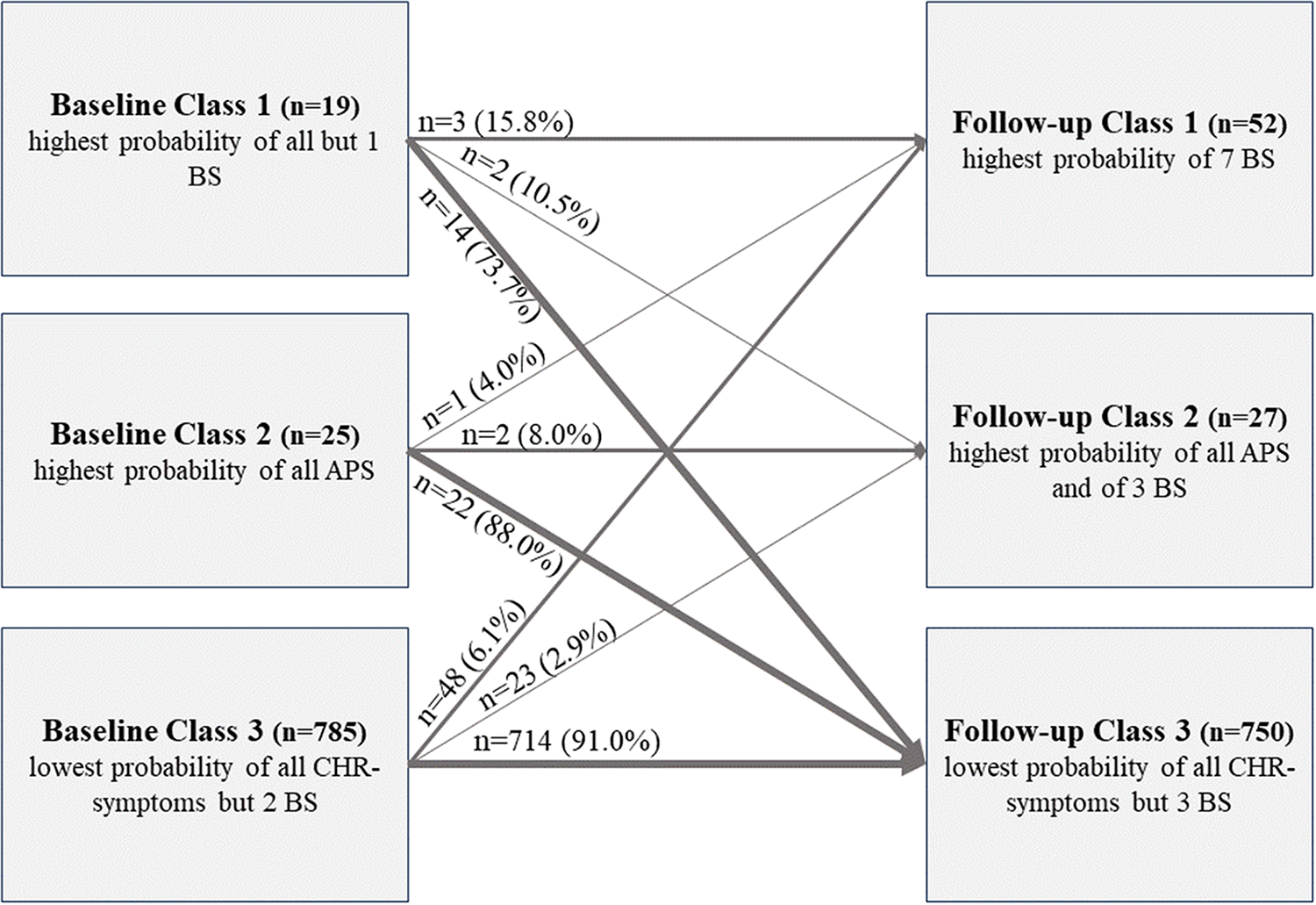
Figure 3. Changes of class membership over time.
Demographic and socio-economic characteristics across CHR-P classes
The classes differed little in distribution of sex, nationality, family history of psychiatric disorders and age, although participants in Baseline Class 2 were the oldest at both baseline and follow-up. Across time points, Class 3 had the highest rate of regular employment.
The distribution of education and marital status showed more variation. While there was less distinction between Baseline Classes at either time point, Follow-up Class 3 showed significantly higher education and lower divorce rates than Follow-up Classes 2 and 1. In turn, Follow-up Class 2 participants were most frequently unmarried, while Follow-up Class 1 members were most often separated. Finally, the education level in Follow-up Class 2 was slightly higher than in Follow-up Class 1.
Changes and class characteristics of CHR-P symptoms
CHR-P symptom profiles showed some relevant changes across classes and time points.
At follow-up, Baseline Classes 1 and 3 showed a more than twofold increase in the rate of (attenuated) hallucinations. As a result, Baseline Class 1, whose members also exhibited increased rates of thought blockage and derealization, now showed a similar rate of (attenuated) hallucinations to Baseline Class 2. Despite this, the rate of (attenuated) hallucinations in Baseline Class 3 remained significantly smaller than in both symptomatic classes. Similarly, perceptual BS had more than doubled, with the increase being particularly pronounced in Baseline Class 3, thus leading to a lack of significant class differences in perceptual BS at follow-up. In summary, while perceptual symptoms had little influence on class identification at baseline, their increase at follow-up turned them into highly influential symptoms for the definition of both symptomatic classes.
Conversely, unusual thought content (SIPS P1), which had been highly influential on class separation at baseline, did not maintain this role for Class 1 at follow-up. However, it remained highly influential for Class 2, which continued to show the overall highest rate of any APS/BIPS at this time point. Newly, Follow-up Class 2 also showed the highest prevalence rates of four BS: inability to divide attention, disturbance of receptive speech, decreased ability to discriminate between ideas/perception and fantasy/true memories, and derealization. Additionally, visual perception disturbances occurred more frequently in Follow-up Class 2, although still less frequently than in Follow-up Class 1. This was a notable change compared to the baseline assessment, where no BS had been most frequent in Class 2, although disturbance of receptive speech, derealization and thought pressure had occurred frequently.
Discussion
To the best of our knowledge, this is the first longitudinal study of classes of a comprehensive collection of CHR-P symptoms in the community, and the first that not only examines homogeneous classes of individuals at baseline but also their stability and change in class membership over time.
Symptomatic characteristics of classes over time
Our three-class solution aligns with earlier LCA studies of UHR patients, which predominantly reported three classes (Healey et al., Reference Healey, Penn, Perkins, Woods, Keefe and Addington2018; Ryan et al., Reference Ryan, Addington, Bearden, Cadenhead, Cornblatt, Mathalon, McGlashan, Perkins, Seidman, Tsuang, Woods, Cannon and Walker2018), though some found four (Valmaggia et al., Reference Valmaggia, Stahl, Yung, Nelson, Fusar-Poli, McGorry and McGuire2013) or five (Ryan et al., Reference Ryan, Addington, Bearden, Cadenhead, Cornblatt, Mathalon, McGlashan, Perkins, Seidman, Tsuang, Woods, Cannon and Walker2018). Most focused solely on UHR patients, with only one (Healey et al., Reference Healey, Penn, Perkins, Woods, Keefe and Addington2018) including healthy controls, making it most comparable to ours. Healey et al. also identified a three-class solution with a ‘mild’ class similar to our Class 3. However, unlike our study, APS/BIPS were not highly influential in their results, possibly due to UHR criteria favouring positive symptoms. The influential role of negative symptoms in earlier studies contrasts with our study’s emphasis on APS/BIPS, possibly due to the exclusion of negative symptoms in our analysis.
The differentiation of symptomatic classes in our community study into one characterized mainly by APS/BIPS, and one characterized mainly by BS, is in line with previous reports of SIPS positive items and BS mostly clustering in different classes (Jimeno et al., Reference Jimeno, Gomez-Pilar, Poza, Hornero, Vogeley, Meisenzahl, Haidl, Rosen, Klosterkötter and Schultze-Lutter2020, Reference Jimeno, Gomez-Pilar, Poza, Hornero, Vogeley, Meisenzahl, Lichtenstein, Rosen, Kambeitz, Klosterkötter and Schultze-Lutter2022). In a recent network cluster analysis (Jimeno et al., Reference Jimeno, Gomez-Pilar, Poza, Hornero, Vogeley, Meisenzahl, Haidl, Rosen, Klosterkötter and Schultze-Lutter2020), only hallucinatory symptoms (SIPS-P4) had joined the cluster of BS; this being broadly in line with Follow-up Class 1 that was characterized by seven BS and (attenuated) hallucinations (SIPS-P4). However, APS/BIPS and BS were best separated at baseline.
Baseline class characteristics remained consistent over time, with notable exceptions, particularly an increase in perceptual symptoms in Class 1 at follow-up. Given earlier findings linking (attenuated) hallucinations and BS to younger age (Schimmelmann et al., Reference Schimmelmann, Michel, Martz-Irngartinger, Linder and Schultze-Lutter2015; Schultze-Lutter et al., Reference Schultze-Lutter, Hubl, Schimmelmann and Michel2017, Reference Schultze-Lutter, Ruhrmann, Michel, Kindler, Schimmelmann and Schmidt2020a, Reference Schultze-Lutter, Schimmelmann, Flückiger and Michel2020b; Schultze-Lutter and Schmidt, Reference Schultze-Lutter and Schmidt2016; Walger et al., Reference Walger, Antonucci, Pigoni, Upthegrove, Salokangas, Lencer, Chisholm, Riecher-Rössler, Haidl, Meisenzahl, Rosen, Ruhrmann, Kambeitz, Kambeitz-Ilankovic, Falkai, Ruef, Hietala, Pantelis, Wood, Brambilla, Bertolino, Borgwardt, Koutsouleris and Schultze-Lutter2020), this increase was unexpected. Future studies should examine features related to this increase to better understand the course of perceptual symptoms in the community. Further, the cross-class occurrence of thought pressure, derealization and visual perception disturbances, as well as suspiciousness/persecutory ideas, may be attributed to their transdiagnostic nature, not observed in other CHR-P symptoms or criteria (Schultze-Lutter et al., Reference Schultze-Lutter, Walger, Franscini, Traber-Walker, Osman, Walger, Schimmelmann, Flückiger and Michel2022).
Associated features over time and class solutions
Interestingly, despite the sample’s generally reduced symptom load at follow-up, which is in line with other studies (Bergé et al., Reference Bergé, Carter and Smucny2024; Salazar de Pablo et al., Reference Salazar de Pablo, Soardo, Cabras, Pereira, Kaur, Besana, Arienti, Coronelli, Shin, Solmi, Petros, Carvalho, McGuire and Fusar-Poli2022), the number of members in the two symptomatic classes increased from baseline to follow-up. Comparing the socio-demographic and clinical features between assessment times and LCA solutions, however, revealed some small changes in distribution of axis-I disorders that tended to be most frequent in Class 1, and least frequent in Class 3 over time, and across solutions. This was despite a decline in axis-I disorders over time, in particular in affective and other disorders (i.e., eating disorders, somatoform disorders, etc.), that aligns with reports of a decline of comorbid mental disorders over time from clinical CHR-P samples (Solmi et al., Reference Solmi, Soardo, Kaur, Azis, Cabras, Censori, Fausti, Besana, de Pablo G and Fusar-Poli2023). The combination of CHR-P symptoms and non-psychotic mental disorder is considered a particularly ‘risky’ form of CHR-P state, with poorer outcome compared to CHR-P symptoms in isolation (Hasmi et al., Reference Hasmi, Pries, Ten Have, de Graaf, van Dorsselaer, Bak, Kenis, Richards, Lin, O’Donovan, Luykx, Rutten, Guloksuz and van Os2021). This might explain the poor outcome of Baseline Class 1 members who had the highest rate of baseline axis-I disorder and, at follow-up, had the highest rates of axis-I disorders and functional deficits.
Functional deficits demonstrated little change in overall frequency over time, and were generally lowest in Class 3, but differed between the symptomatic classes in distribution over time and solutions. While functional deficits were similarly frequent in Baseline Classes 1 and 2 at baseline, at follow-up, they were most frequent in Baseline Class 1 and in Follow-up Class 2. This lack of a significant improvement in functioning is in contrast to reports from follow-up studies of CHR-P samples that commonly report significant functional improvement over time (Salazar de Pablo et al., Reference Salazar de Pablo, Soardo, Cabras, Pereira, Kaur, Besana, Arienti, Coronelli, Shin, Solmi, Petros, Carvalho, McGuire and Fusar-Poli2022). The difference in findings may be related to a difference in samples, with far fewer participants with functional deficits in our community sample and/or to the assessment of functioning – dichotomized data in our study, and continuous raw data in most clinical studies (Salazar de Pablo et al., Reference Salazar de Pablo, Soardo, Cabras, Pereira, Kaur, Besana, Arienti, Coronelli, Shin, Solmi, Petros, Carvalho, McGuire and Fusar-Poli2022). Overall, the generally maintained disadvantages of the symptomatic classes over time, despite symptomatic improvements, underscore the importance of preventive approaches not only with regard to mental disorders but also functional deficits and vocational-educational disadvantages (Campion et al., Reference Campion, Bhui and Bhugra2012; Porru et al., Reference Porru, Schuring, Hoogendijk, Burdorf and Robroek2023).
Membership changes between Baseline and Follow-up Classes
In line with the general symptomatic, clinical and socio-demographic stability of Class 3 over time, this class showed the lowest rate of changes into any symptomatic class, indicating that most participants remained ‘healthy’ over time. Furthermore, the highest rate of class membership changes of the two symptomatic classes were into Follow-up Class 3, indicating health improvement and an attenuation of most CHR-P symptoms over time (Addington et al., Reference Addington, Farris, Devoe and Metzak2020). In absolute numbers, however, more participants moved from the large Baseline Class 3 into one of much smaller symptomatic Follow-up Classes; with a third of them into Follow-up Class 1. The unexpected transition from ‘healthy’ to psychopathological symptoms suggests that even those with few or no symptoms may be at risk for later development of CHR-P symptoms. This broadens the focus of early detection efforts beyond solely ‘at-risk’ individuals with CHR-P symptoms, prompting exploration of hidden factors including (neuro)biological and psychosocial influences, such as inflammatory processes and negative life events (de Koning et al., Reference de Koning, Kuzminskaite, Vinkers, Giltay and Penninx2022; Trotta et al., Reference Trotta, Murray and Fisher2015). Understanding these factors beyond genetic predisposition is crucial for comprehensively addressing psychopathology development.
Follow-up Class 1 also showed higher membership stability compared to Follow-up Class 2 (16% vs. 8%). This broadly aligns with reported changes of CHR-P criteria in a clinical sample of an early detection service over 1–10-year follow-up (Michel et al., Reference Michel, Ruhrmann, Schimmelmann, Klosterkötter and Schultze-Lutter2018a), in which most non-converters had remitted from CHR-P status (72%), and more non-converters with the baseline BS criterium ‘Cognitive Disturbances’ than with baseline UHR criteria maintained their risk status (18% vs. 12%). Furthermore, 91% of CHR-P-negative patients remained CHR-P-negative (Michel et al., Reference Michel, Ruhrmann, Schimmelmann, Klosterkötter and Schultze-Lutter2018a). Overall, our results support the fluctuating nature of CHR-P symptoms.
Practical recommendations
Based on our findings, we propose several practical steps to improve early detection and intervention for CHR-P symptoms. Community-based prevention efforts should prioritize targeted mental health literacy programmes aimed at the public, healthcare providers and educators. These programmes should focus on increasing awareness of early CHR-P symptoms – such as perceptual disturbances, cognitive difficulties and social withdrawal – while addressing stigma to promote timely help-seeking.
In primary care settings, integrating brief and validated CHR-P screening tools, such as the Prodromal Questionnaire-Brief (PQ-B; Loewy et al., Reference Loewy, Pearson, Vinogradov, Bearden and Cannon2011) or the Community Assessment of Psychic Experience (CAPE; Mossaheb et al., Reference Mossaheb, Becker, Schaefer, Klier, Schloegelhofer, Papageorgiou and Amminger2012), into routine clinical practice can facilitate earlier identification of individuals at risk. Training primary care professionals to recognize key indicators of CHR-P, including comorbid mood or anxiety symptoms, is essential for appropriate referral to specialized services.
For individuals with functional impairments or symptomatic profiles, targeted interventions such as cognitive-behavioural therapy, stress management techniques and resilience-building programmes should be offered. Family psycho-education and support can also play a critical role in improving social and functional outcomes.
Given the heterogeneity of CHR-P presentations, personalized preventive strategies are crucial. These should be informed by comprehensive assessments of psychosocial factors (e.g., trauma history, family dynamics), neurocognitive deficits (e.g., executive dysfunction) and biological risk markers (e.g., sleep disturbances or neuroinflammation). Tailoring interventions to individual risk profiles increases their precision and effectiveness.
Lastly, longitudinal monitoring of individuals with mild or subthreshold symptoms is vital to detect emerging risk states. This can be achieved through structured follow-ups and the use of digital tools, such as Ecological Momentary Assessment and telehealth platforms, which allow real-time tracking of symptom trajectories and functional outcomes. Such continuous monitoring enables adaptive and timely interventions that may prevent progression to fully manifest psychosis.
By implementing these strategies, we can enhance the early identification of CHR-P states, provide timely and individualized interventions, and ultimately improve long-term outcomes for at-risk individuals.
Strengths and limitations
Our symptom selection is both a strength and limitation. While our study is the first LCA study to include the full spectrum of CHR-P symptoms (Schultze-Lutter et al., Reference Schultze-Lutter, Michel, Schmidt, Schimmelmann, Maric, Salokangas, Riecher-Rössler, van der Gaag, Nordentoft, Raballo, Meneghelli, Marshall, Morrison, Ruhrmann and Klosterkötter2015), it did not include non-CHR-P-relevant symptoms, such as negative symptoms, which have been shown to differentiate classes (Healey et al., Reference Healey, Penn, Perkins, Woods, Keefe and Addington2018; Ryan et al., Reference Ryan, Addington, Bearden, Cadenhead, Cornblatt, Mathalon, McGlashan, Perkins, Seidman, Tsuang, Woods, Cannon and Walker2018; Valmaggia et al., Reference Valmaggia, Stahl, Yung, Nelson, Fusar-Poli, McGorry and McGuire2013). However, the shift towards a stepwise psychosis detection approach, assessing CHR-P criteria first (Schultze-Lutter and Meisenzahl, Reference Schultze-Lutter and Meisenzahl2023, Reference Schultze-Lutter and Meisenzahl2024; Woods et al., Reference Woods, Parker, Kerr, Walsh, Wijtenburg, Prunier, Nunez, Buccilli, Mourgues-Codern, Brummitt, Kinney, Trankler, Szacilo, Colton, Ali, Haidar, Billah, Huynh, Ahmed, Adery, Marcy, Allott, Amminger, Arango, Broome, Cadenhead, Chen, Choi, Conus, Cornblatt, Glenthøj, Horton, Kambeitz, Kapur, Keshavan, Koutsouleris, Langbein, Lavoie, Diaz-Caneja, Mathalon, Mittal, Nordentoft, Pasternak, Pearlson, Gaspar, Shah, Smesny, Stone, Strauss, Wang, Corcoran, Perkins, Schiffman, Perez, Mamah, Ellman, Powers, Coleman, Anticevic, Fusar-Poli, Kane, Kahn, McGorry, Bearden, Shenton, Nelson, Calkins, Hendricks, Bouix, Addington, McGlashan and Yung2023), suggests our classes may reflect early diagnostic steps. Strengths of our study include clinical assessments by trained psychologists and a large, well-representative sample (Schultze-Lutter et al., Reference Schultze-Lutter, Michel, Ruhrmann and Schimmelmann2018). Still, the small size of symptomatic classes warrants caution in interpretation. Additionally, like earlier studies, we did not account for the impact of treatment, which could have influenced class development. Treatment may be particularly influential, as higher symptom loads often lead to increased help-seeking (Michel et al., Reference Michel, Schmidt, Schnyder, Flückiger, Käufeler, Schimmelmann and Schultze-Lutter2019).
Conclusion and future directions
Our results suggest that CHR-P symptoms cluster similarly in the community as in clinical samples, despite their fluctuation over time, underpinning the largely distinct and, therefore, complementary nature of the BS and symptomatic UHR approaches (Schultze-Lutter et al., Reference Schultze-Lutter, Ruhrmann, Michel, Kindler, Schimmelmann and Schmidt2020a). In addition, the association of the two symptom classes with axis-I disorders and functional deficits emphasizes the clinical significance of CHR-P symptoms beyond a potential bias towards higher clinical relevance in patient samples (Fusar-Poli et al., Reference Fusar-Poli, Schultze-Lutter, Cappucciati, Rutigliano, Bonoldi, Stahl, Borgwardt, Riecher-Rössler, Addington, Perkins, Woods, McGlashan, Lee, Klosterkötter, Yung and McGuire2016; Ruhrmann et al., Reference Ruhrmann, Schultze-Lutter and Klosterkötter2010; Schmidt et al., Reference Schmidt, Schultze-Lutter, Schimmelmann, Maric, Salokangas, Riecher-Rössler, van der Gaag, Meneghelli, Nordentoft, Marshall, Morrison, Raballo, Klosterkötter and Ruhrmann2015).
These results emphasize the importance of preventive measures in general, and point to the need to improve mental health literacy in relation to CHR-P states and symptoms in the community (Kelly et al., Reference Kelly, Jorm and Wright2007). All the more so, as compared to other mental disorders, such as depression (Svensson and Hansson, Reference Svensson and Hansson2016), there is a significant lack of knowledge, misunderstanding and negative stereotyping of psychotic disorders, including their symptoms and risk stages (Doll et al., Reference Doll, Michel, Betz, Schimmelmann and Schultze-Lutter2022; Goodwin, Reference Goodwin2014; O’Keeffe et al., Reference O’Keeffe, Turner, Foley, Lawlor, Kinsella, O’Callaghan and Clarke2016; Patel, Reference Patel2004), in the healthcare system, the public and the media. Even those affected often lack a clear understanding of the CHR-P condition, which delays their help-seeking (Haidl et al., Reference Haidl, Seves, Eggers, Rostamzadeh, Genske, Jünger, Woopen, Jessen, Ruhrmann and Vogeley2019). At the clinical level, improved stepwise diagnostic approaches drawing from broad psychopathological, resilience, neurocognitive and biogenetic assessments for improved risk profiling for various outcomes and risk-adapted treatments should enable a more personalized, broader prevention approach that better fits the need of different person classes (Schultze-Lutter and Meisenzahl, Reference Schultze-Lutter and Meisenzahl2023, Reference Schultze-Lutter and Meisenzahl2024; Worthington and Cannon, Reference Worthington and Cannon2021).
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796024000891.
Availability of data and materials
Data will not be directly available on a public repository or in the supplements. However, it can be made available on request via the corresponding author (C.M.).
Acknowledgements
The authors thank their Australian colleague, Mrs. Madelyn Thomson, for her careful language editing.
Financial support
This study was supported by two project-funding grants from the Swiss National Science Foundation (SNFS), grant numbers 32003B_135381 and 32003B_155951 (to Drs. Schultze-Lutter and Schimmelmann).
Competing interests
Drs. Michel, Kindler, and Schultze-Lutter as well as Mr. Osman (M.sc.) and Mrs. Rinaldi (M.Sc.) have declared that they have no conflicts of interest in relation to the subject of this study.
Dr. Schimmelmann has been a consultant and/or advisor to, or has received honoraria from AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Janssen, Novartis, and Shire.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2013.








