Although mental health research has been conducted ‘globally’ for many decades (see for example Kleinman,Reference Ormel, VonKorff, Ustun, Pini, Korten and Oldehinkel2 Ormel et al Reference Ormel, VonKorff, Ustun, Pini, Korten and Oldehinkel2 and Demyttenaere et al Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess and Lepine3), the Lancet series published in 2007 helped establish ‘global mental health’ as a distinct field.Reference Prince, Patel, Saxena, Maj, Maselko and Phillips4 Among its contributions, the Lancet series made a call for action to scale up mental health services in low- and middle-income countries (LMICs),Reference Prince, Patel, Saxena, Maj, Maselko and Phillips4 and launched the Movement for Global Mental HealthReference Horton5 – ostensibly integrating and giving new direction to existing fields of study.
Rise in ‘global mental health’
Since 2007, there has been a sharp increase in the number of academic institutions and funding programmes adopting the term ‘global mental health’ in initiative names. These include multiple leading research centres, such as: Harvard University, Johns Hopkins University, King's College London, the London School of Hygiene & Tropical Medicine, Melbourne University, the New University of Lisbon and the University of Washington. Such institutions have crafted their own training programmes (for example King's College London,6 Johns Hopkins Bloomberg School of Public Health7 and Lisbon Institute of Global Mental Health8) and published specialised textbooks on global mental health (for example Patel et al Reference Patel, Minas, Cohen and Prince9 and Kohrt & MendenhallReference Kohrt and Mendenhall10). Institutional growth has come hand in hand with new funding streams for primary research and capacity building. Examples include the Grand Challenges Canada's Global Mental Health programme (CAD $42 million investment 2014–2017),11 the USA's National Institute of Mental Health ‘Grand Challenges in Global Mental Health’ (USD $2 million in 2013)12 and the UK's Medical Research Council call on Global Mental Health (GBP £15 million 2018–2023).13 In light of these major new initiatives, it is particularly important to pause and examine use of the term ‘global mental health.’
Implicit priorities of ‘global mental health’
Initial definitions of the term asserted that mental health should be part of global health, emphasising the lack of sufficient and equitable mental health resources.Reference Prince, Patel, Saxena, Maj, Maselko and Phillips4 These definitions emphasised providing evidence-based programmes and services in LMICs and/or low-resource settings (for example Bartlett et al Reference Bartlett, Garriott and Raikhel14). More recently, ‘global mental health’ has also more broadly been defined as improving mental health and achieving mental health equity for all people worldwide.Reference Patel and Prince15 Some, however, argue that no shared definition of the term has been providedReference Fernando16 or that the term will be impossible to ever define universally.Reference Summerfield17 Together, these conflicting definitions suggest consensus about the meaning of the term ‘global mental health’ has not yet been achieved.
This paper aims to review the scientific literature that self-identifies with the term ‘global mental health’ to identify the implicit priorities of those using the term. To that end, we systematically review all peer-reviewed publications from the past decade that explicitly use this term in the text of the article (title, abstract, text, keyword, header). This restriction to a single term is deliberately narrow. The paper is not a systematic review of all literature that could be considered to be ‘global mental health,’ but rather of the articles that explicitly choose to align themselves with the term by using ‘global mental health’ within their text. We included empirical studies, systematic reviews, commentaries and other original pieces to provide a more comprehensive understanding of how use of the term has changed over time. We also quantified the empirical studies to provide an empirical basis for understanding what types of research have self-identified as ‘global mental health’ including by geographic region(s) and mental health condition(s). This review provides a basis to evaluate what has happened under work that self-identifies as ‘global mental health’ thus far and to reflect on what the field hopes to achieve as it continues to evolve.
Method
We conducted a systematic review of all peer-reviewed articles containing the English term ‘global mental health’ in five databases (PubMed, PsycINFO, Embase, Web of Science, and WHO Global Index Medicus) from 1 January 2007 to 31 December 2016. The time period was chosen to correspond with the decade following the publication of the first Lancet series. For each database, all searchable fields were specified including full-text searches where available. For Embase and the WHO Global Index Medicus, the search was restricted to exclude articles indexed in PubMed. The final search yielded 542 articles in PubMed, 618 in PsycINFO, 527 in Embase, 482 in Web of Science, and 12 in the WHO Global Index Medicus. After deleting duplicate records, the final count was 1108 unique records.
We restricted our search to the English language because the term ‘global mental health’ is an English language construct stemming from ‘global health’Reference Patel18 and the majority of scientific writing is in English.Reference Gordin19 To our knowledge, there is no standardised translation of the term into other languages. To this end, we consulted with native speakers of French (V.d.M.) and Mandarin who do mental health research as well as conducted brief searches into potential translations of the term in French and Mandarin. Using the online dictionary Linguee.com, which trawls the web for published translations across all disciplines, we found six French translations of ‘global mental health’ based on 28 translations of the term. Over half the French translations (15/28) eliminated the adjective ‘global,’ translating the term as simply ‘santé mentale’ or ‘mental health’ – some of them placing the adjective global on a different noun (such as movement, alliance, call) and others removing it altogether (see supplementary Table 1 available at https://doi.org/10.1192/bjo.2019.39). Similarly, the Mandarin term (‘quánqiú xīnlı̌ jiànkāng’), used as a translation on the website of the World Federation for Mental Health, appears to have a broader definition closer to ‘well-being’ (H. Huang, personal communication, 15 February 2019). An exploratory search of the Mandarin term in PubMed identified 162 hit results between 2007 and 2016, but the vast majority of hits do not pertain to any type of mental health research. In the absence of standardised translations, we concluded that a search of the term across different languages would not be valid.
Review process
One reviewer (S.M.) screened all full-text articles for eligibility. Two independent reviewers (A.S., E.E.H.) then audited 10% of the records for quality assurance. All steps followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA),Reference Moher, Liberati, Tetzlaff and Altman20 and are enumerated in the PRISMA flow chart (Fig. 1).
Fig. 1 PRISMA flow diagram.
Inclusion/exclusion criteria
The review was restricted to peer-reviewed articles, including empirical studies, systematic reviews, commentaries and other original pieces. Entries were automatically excluded if they were an abstract, book or book chapter, conference proceeding, dissertation or editor's note; if they were not about research (for example book review, interview, profile, newsletter); not in English; not in humans; or outside the time range. After screening, 817 unique records were retained for full-text review.
Full-text review
Articles were eligible for inclusion if they included the term ‘global mental health’ anywhere in the title, abstract, text, keyword or header. Overall, 350 records (42.8%) were excluded: 62 records were removed because the term ‘global mental health’ was used to refer to a generic or non-specific measure of mental health (analogous to ‘global physical health’) rather than the field of ‘global mental health,’ and 288 records because the term did not appear anywhere in the article; for example, it only appeared in the author's affiliation (for example with a Department of or Centre for Global Mental Health) or in the article's references (such as in the title of a cited article). A total of 467 articles were retained for the analysis (see Supplementary File 1 for a full list of references).
Article classification
Each article was classified as an empirical study, systematic review, commentary, or other original piece (‘other’). Empirical studies described primary data collection and analysis; original research not describing a study sample was classified as ‘other’. Systematic reviews were restricted to those that described a systematic search process; narrative reviews that did not indicate a systematic search process were classified as ‘other’. Commentaries were restricted to those explicitly stated to be editorials, viewpoints, perspectives or letters to the editor; other pieces that included the authors’ opinions but did not explicitly indicate this were classified as ‘other’. Remaining pieces were also classified as ‘other’ if they included original thought but did not meet one of the three prior classifications, such as conceptual and theoretical frameworks, narrative summaries of some aspect of the field, or examples of successful training programmes. If classification was unclear, the two reviewers (S.M. and A.S.) discussed them until they arrived at consensus.
Data extraction
The range of formats in the non-empirical articles (for example reviews, editorials, theoretical frameworks, descriptions of programmes) precluded systematic classification so our main analysis is restricted to empirical studies that described primary data collection and analysis. For all articles, the two reviewers extracted the article title, first author, year of publication, journal title, and any explicit definitions of ‘global mental health.’ To identify explicit definitions, the article was searched for every instance of the term ‘global mental health’ or ‘GMH’ to determine whether it was embedded in a sentence that defined the term (for example ‘global mental health is…,’ ‘global mental health may be defined as…’). This excluded descriptions that only described a ‘focus’ or ‘emphasis’ of an aspect of global mental health but did not define the field at large.
All empirical studies were quantified by two metrics: the country(ies) where the research took place and the main mental health condition(s). For country, the studies were then classified as LMIC or high-income country (HIC) based on World Bank designations at the time of review.21 We selected World Bank regions because they aligned with common geographic boundaries and offered more granularity than other broader categorisations. In early 2018, LMIC economies were defined as those with a gross national income per capita of $12 235 USD or less and HIC economies were defined as those with a gross national income per capita of $12 236 USD or more. Next, the studies were classified into one of 11 World Bank geographic regions.21 The World Bank typically groups countries into seven regions, some of which we subdivided further: East Asia and Pacific (split into two), Europe and Central Asia (split into two), Latin America and Caribbean (split into two), Middle East and North Africa (split into two), North America, South Asia and Sub-Saharan Africa.
For main mental health condition, the studies ranged from diagnoses of ‘mental disorders’ and ‘mental illnesses’ to dimensional descriptions of mental symptomology to positive mental health and well-being. The studies were coded by mental health condition(s), and then classified based on categories from the World Health Organization's Mental Health Gap Action Programme (mhGAP) intervention guide and annex for mental, neurological and substance use disorders, which include: child and adolescent mental and behavioural problems; conditions specifically related to stress (which require exposure to stressors and include significant symptoms of acute stress; post-traumatic stress disorder; and grief and prolonged grief disorder); dementia; depression; disorders as a result of substance use; epilepsy; psychoses (i.e. psychosis and bipolar disorder); and self-harm and suicide.22,23 We selected the mhGAP categories because they are designed to be accessible to lay people and we did not want to be limited to diagnostic criteria (for example DSM, ICD) that might only be used in some places but not others. This allowed for inclusion of broader conceptions of mental health such as self-report measures and/or subthreshold symptoms. To ensure we were not limited by these categories, we additionally categorised all mental health conditions with at least three studies; conditions that appeared two or less times were classified as ‘other’. As some studies were conducted across multiple countries or assessed multiple mental health conditions, the total number of counts exceeded the total number of studies. In cases where the counts exceeded 15, studies were classified as ‘multiple.’
For empirical studies, we also quantified details about the study method (quantitative, qualitative, multimethod, case), study context, sample size and sample demographics. Unlike traditional systematic reviews, the goal of this analysis was not to analyse study quality and/or outcomes but to ascertain the types of data being collected in global mental health research. We selected the context and sample details as minimal reporting requirements based on the Cochrane Public Health Group's guide for developing a protocol for systematic reviews.24 The Cochrane-endorsed PROGRESS-Plus framework recommends details about place of residence, ethnicity/culture/language, occupation, gender, religion, education, socioeconomic status, social capital and personal characteristics associated with discrimination (for example age, disability).25 We defined study context as two binary items for whether or not the authors specified the region(s) within the country(ies) where the study took place and the language(s) in which the study was conducted. We defined sample sociodemographics as a series of binary items for whether or not they provided any details about age (for example mean age and standard deviation), gender (for example percentage female), ethnic identity (for example percentages by ethnicity, caste, tribe), socioeconomic status (for example household income; or if they were using a proxy variable, an explicit statement that it was a proxy variable such as education level), religious affiliation (for example percentages by religious groups) and sexual orientation (for example percentage sexual minorities).
Results
There was an almost ten-fold increase in the annual number of articles using the term ‘global mental health’ from 2007 to 2016 (Fig. 2). The second half of the period under review (2012–2016) accounted for 83.7% of the articles, with almost two-thirds (64.0%) occurring in the last 3 years (2014–2016). Despite the rapid increase in the use of the term, 91.2% of the 467 articles were missing an explicit definition of the term ‘global mental health.’
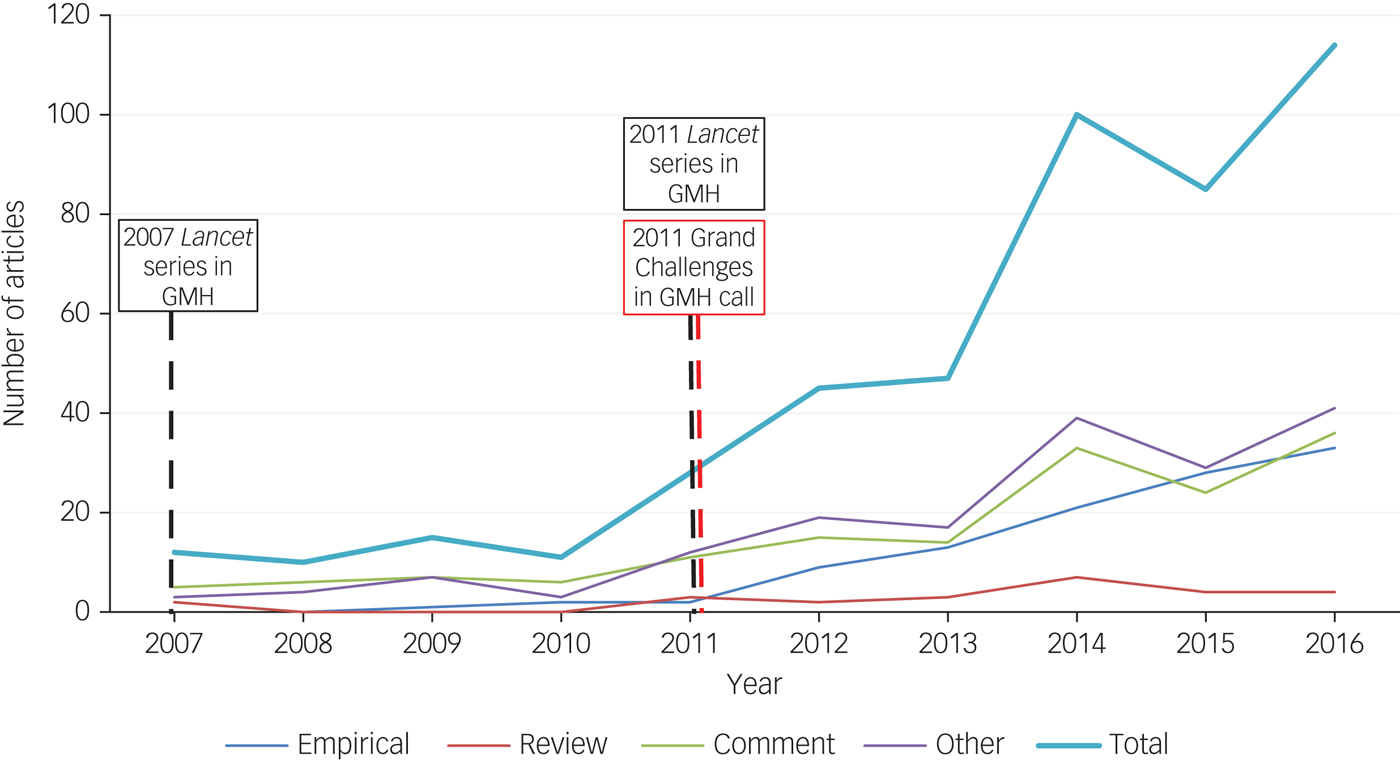
Fig. 2 ‘Global mental health’ term use by type of article over a 10-year period with select milestones in the field.
When broken down into categories by type of article, the majority (76.2%) of articles were non-empirical: more than a third (37.3%, n = 174) were classified as ‘other’, another third (33.6%, n = 157) were commentaries and the remainder (5.4%, n = 25) were systematic reviews. The final quarter (23.8%, n = 111) of articles were empirical studies.
Results from empirical studies
The number of empirical studies increased 16.5-fold over the decade, from 2 articles in 2007 to 33 articles in 2016, with a total of 111 articles over the 10-year span.
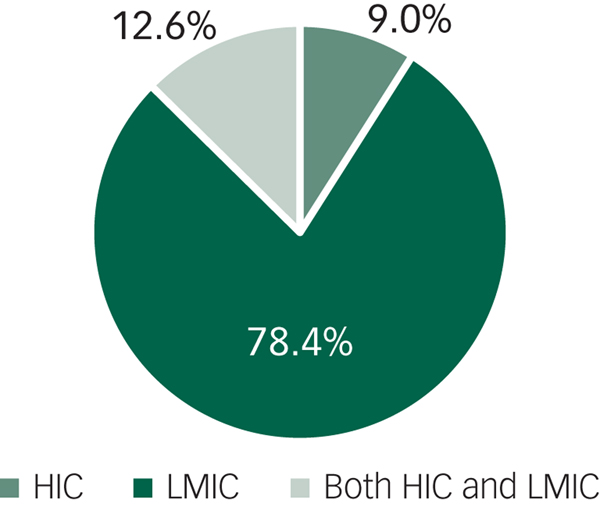
Studies by country
The majority of studies (78.4%) took place in LMICs, while 9.0% were in HICs, and 12.6% took place across both LMICs and HICs (Fig. 3). Some studies included multiple countries (denominator n = 141), with the majority in Sub-Saharan Africa (28.4%, n = 40) and South Asia (25.5%, n = 36) (Fig. 4). Within Sub-Saharan Africa, more than half of the studies (n = 22) took place in three countries: South Africa, Uganda and Ethiopia. In South Asia, three-quarters of the studies (n = 27) were from two countries: India and Nepal (see supplementary Table 2 for the number of studies per individual country). For the rest of the studies, less than 10% each were from Latin America (9.2%, n = 13), North America (5.7%, n = 8), and East Asia (5.7%, n = 8), less than 5% each were from the Middle East (4.3%, n = 6), the Pacific (4.3%, n = 6), the Caribbean (3.6%, n = 5), Europe (3.6%, n = 5) and North Africa (1.4%, n = 2), and none were from Central Asia.

Fig. 3 Ratio of high-income countries (HIC) to low- and middle-income countries (LMIC) in ‘global mental health’ empirical articles.

Fig. 4 Heat map of number of ‘global mental health’ empirical articles across 11 regions.
Studies by main mental health condition
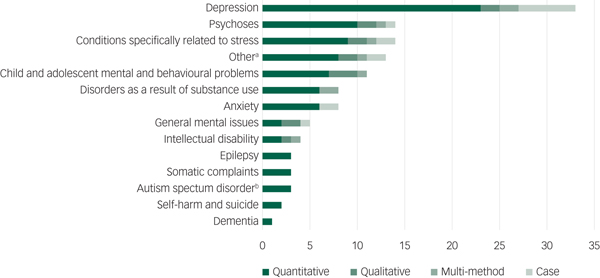
Among the empirical studies that focused on specific mental health conditions (69.4%, n = 77), depression was the most frequent mental health condition studied (29.7%, n = 33) followed by psychoses (12.6%, n = 14) and conditions specifically related to stress (12.6%, n = 14) (Fig. 5). Other mental health conditions covered included child and adolescent mental and behavioural problems (9.9%, n = 11), anxiety (7.2%, n = 8), disorders as a result of substance use (7.2%, n = 8), general mental health conditions (4.5%, n = 5) and intellectual disability (3.6%, n = 4). Based on the mhGAP categories, there were fewer empirical studies on epilepsy (2.7%, n = 3), self-harm and suicide (1.8%, n = 2) and dementia (0.9%, n = 1). Another 11.7% (n = 13) of studies were classified as ‘other’ with two or less studies per topic (for example catatonia, psychological flexibility). The remaining empirical studies (30.6%, n = 34) were not about any specific mental health condition but focused primarily on healthcare providers, consensus gathering activities with leaders in the field, or the development and assessment of academic training programmes.
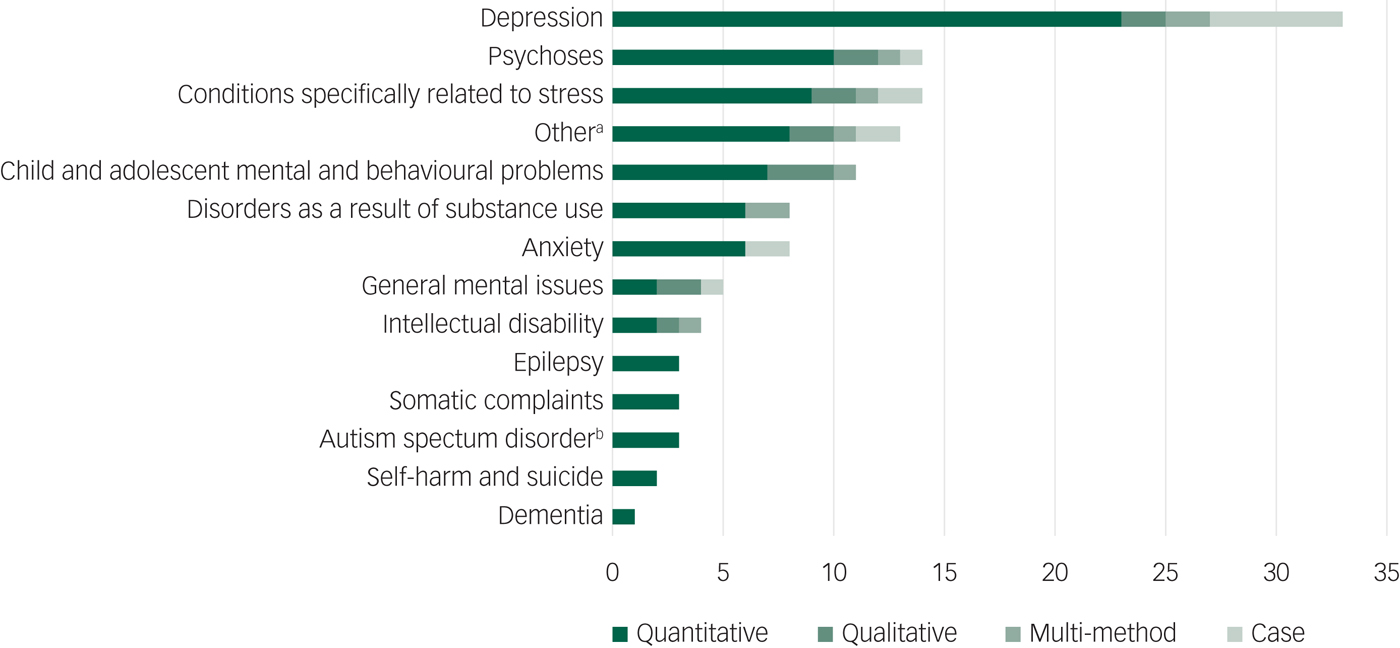
Fig. 5 Bar graph of number of ‘global mental health’ empirical articles by mental health condition.
Study methods
Almost half of the empirical articles were quantitative studies (48.6%), over a quarter were qualitative studies (27.9%), and the remainder were either multimethod studies combining both quantitative and qualitative approaches (12.6%) or were case studies that focused on one to four individuals (10.8%).
Study context, sample size and sample sociodemographics
The majority of empirical studies were missing information that we coded about the study context and sample (Table 1). Studies typically reported the sample size (9.0% missing), but were not as consistent at situating their work in the specific region(s) within a country (20.7% missing) or the specific language(s) in which the study was conducted (36.9% missing). For sample sociodemographics, the studies were relatively more likely to report gender (26.2% missing) and age (40.8% missing). However, there was limited data about ethnic identities (79.6% missing), socioeconomic status (85.4% missing), religious affiliation (89.3% missing) and sexual orientation (99.0% missing; a single study mentioned heterosexual couples).
Table 1 Missing data for contextual and sociodemographic details in in ‘global mental health’ empirical articlesa

a. Denominator for first three: n = 111; denominator for remainder n = 103 because eight studies at aggregate/group level did not include individual sociodemographic details.
Discussion
There has been exponential growth in the number of research publications using the term ‘global mental health’ over the 10-year span, signalling that global mental health is now a distinct field with its own body of literature – even though work in this area existed prior to the term. Our systematic review revealed four implicit priorities for those who self-identify with the term ‘global mental health’ in their publications.
(a) Non-empirical publications: during the first 5 years, the literature was dominated by commentaries and other conceptual pieces; although by 2015 the number of empirical articles using the term had increased and accounted for almost a third of all articles published each year.
(b) Priority regions: the majority of empirical studies were conducted in LMICs, with most taking place in Sub-Saharan Africa and South Asia, particularly in Ethiopia, South Africa, Uganda, India and Nepal.
(c) Priority conditions: depression was the primary focus of empirical studies followed by psychoses and conditions specifically related to stress.
(d) Undefined populations: empirical studies were characterised by a lack of contextual information (for example geographic region, urban versus rural) and sociodemographic detail (for example language, religion).
Results from empirical studies
The universality of place and condition implied in the word ‘global’ masks inequalities in geographic and mental health focus. In terms of geography, our review revealed that the majority of empirical studies using the term ‘global mental health’ were conducted in LMICs, and that not all LMICs were studied equally. The majority of studies occurred in a handful of countries in Sub-Saharan Africa and South Asia, namely Ethiopia, South Africa, Uganda, India and Nepal. The volume of publications from these five countries is driven in part by three collaborations: the European Union's Emerging mental health systems in low and middle-income countries (Emerald) project, the PRogramme for Improving Mental Health CarE (PRIME) trial, and the AFrica Focus on Intervention Research for Mental Health (AFFIRM) initiative.Reference Semrau, Evans-Lacko, Alem, Ayuso-Mateos, Chisholm and Gureje26–Reference Lund, Alem, Schneider, Hanlon, Ahrens and Bandawe28 There was a complete absence of empirical studies in Central Asia, which parallels findings from other reviews.Reference Michalopoulos, Meinhart, Yung, Barton, Wang and Chakrabarti29,Reference Winkler, Krupchanka, Roberts, Kondratova, Machů and Höschl30 The low number of studies for the Middle East might be in part because half are classified as HICs,21 and for the Caribbean and Pacific, might follow from their small populations.31
In terms of mental health conditions, the majority of empirical studies focused on three conditions: depression, psychoses and conditions specifically related to stress. The predominant focus on depression is consistent with its high contribution to the global burden of disease, as measured in years of life lost and years lived with disability. But there were relatively few studies on anxiety despite its high global burden from years lived with disabilityReference Whiteford, Degenhardt, Rehm, Baxter, Ferrari and Erskine32 and its frequent co-occurrence with depression. Other conditions that contribute significantly to burden of disease that are less represented include child and adolescent mental and behavioural problems, disorders as a result of substance use, dementia and suicide.Reference Whiteford, Degenhardt, Rehm, Baxter, Ferrari and Erskine32 Finally, the phrase ‘mental health’ implies a spectrum from mental ill health to mental well-being, but only 2 of the 77 empirical studies about mental health conditions were about mental well-being.
Beyond questions of research focus lay questions of research quality. Much of the empirical literature using the term ‘global mental health’ was missing data on basic variables of study context and sample sociodemographics. One in three articles did not report the language in which the study was conducted, even in countries with multiple official and unofficial languages. One in five articles did not situate their study within the specific region of a given country, even for studies from large countries like Brazil or India. Gender and age were the most consistently reported sociodemographic variables, but even these were not available for all empirical studies. Finally, there was limited information on ethnic identities and socioeconomic status. Given that the majority of the research in this review took place in LMICs with limited resources, there are understandable trade-offs in choosing what data to collect. However, such thin reporting of social context and sample sociodemographics both limits the quality of the work produced and suggests that the universality inherent in the adjective ‘global’ translates in practice to research that is partially blind to variation between populations and environments. The omission of grounding in local context limits the interpretation and application of these findings.
Limitations
Restricting our search to the use of the English term ‘global mental health’ was deliberate as our goal was to systematically review the literature that explicitly uses that term. Two categories of publication are excluded: (a) ‘false negatives,’ i.e. articles by researchers who self-identify as doing work on global mental health, but did not use the term in their publications; and (b) ‘true negatives,’ i.e. articles by researchers working on mental health that meets one of the definitions of ‘global mental health’ but who would not adhere to the label ‘global mental health.’ Most significant for this review are the ‘true negatives.’
Examples of such research that are not captured by this review but considered central to the field include researchers who identify with the field but do not use the term in every article they publish. It also includes projects that are widely considered to fall under the banner of ‘global mental health’ because they align with dominant definitions of the term – such as closing the ‘treatment gap’ by providing access to affordable, evidence-based services in LMICs.Reference Fernando16 Iconic examples of ‘global mental health’ research not captured in our review include training lay health workers to treat anxiety and depression in India,Reference Patel, Weiss, Chowdhary, Naik, Pednekar and Chatterjee33 the task-shifting intervention known as ‘Friendship Bench’ from Zimbabwe,Reference Chibanda, Bowers, Verhey, Rusakaniko, Abas and Weiss34 the Global Campaign Against Epilepsy demonstration project in rural China,Reference Wang, Wu, Dai, Ma, Yang and Wang35 and an epidemiological survey for prevalence of mental disorders in Nigeria.Reference Gureje, Lasebikan, Kola and Makanjuola36 As some leaders in the field start to broaden the definition of the term to refer to an area of research and practice aimed at improving mental health for all people worldwide,Reference Patel and Prince15 it remains to be seen how empirical research will align with the term.
Implications
In peer-reviewed publications that use the term ‘global mental health,’ the implicit priorities appear to be non-empirical pieces with growing interest in empirical studies, a focus on specific regions and mental health conditions, and limited reporting on the heterogeneity of the populations under study. If closing the treatment gap for depression, psychoses and conditions specifically related to stress in LMICs is the intended priority, then the current body of work may accurately reflect that goal. By extension, if those doing work in other regions or on other conditions should also be self-identifying with ‘global mental health’, then explicit strategies can be developed to address these gaps. Some examples include hosting a special issue of a journal focused on the burden and treatment of anxiety disorders globally or hosting a conference that brings together researchers of the more commonly studied mental health conditions (such as depression, psychoses, conditions related specifically to stress) with researchers of the less commonly studied mental health conditions (such as epilepsy, self-harm and suicide, dementia). Targeted funding calls could enumerate specific regions and even priority countries within those regions to expand coverage. Across all of this, there is an urgent need for increased rigor in reporting information about study context and sample both to maintain the standards of good-quality research and also to consider the vast differences that exist within national boundaries, not just between them.
Our review took a unique approach to bypass predefining the parameters of ‘global mental health’ by focusing exclusively on explicit use of the term. As entities are starting to emerge to synthesise findings in the field, this will require defining the parameters of what ‘global mental health’ entails. The Cochrane Global Mental Health database for systematic reviews launched in 2017 explicitly stated a focus on mental health in LMICs,Reference Barbui, Purgato, Churchill, Adams, Amato and Macdonald37 and the Countdown Global Mental Health, a multistakeholder monitoring and accountability collaboration announced in 2019, has committed to tracking mental health in all countries with a priority of decreasing population-level disparities.Reference Saxena, Kestel, Sunkel, London, Horton and Patel38 Clearly, there is still work to be done to arrive at common consensus about what the term means. Determining this is necessary to identify the body of work that is relevant to ‘global mental health’. Future reviews such as ours could also evaluate the use of the term ‘global mental health’ by funding mechanisms or training programmes, since the lag time between funding or training and publication means that the direction of current research may have shifted relative to current publications.
After more than a decade, the work self-identifying as global mental health has evolved. There is a rapidly increasing number of research publications that use this term as part of their work, including many more empirical studies than at the outset. The term ‘global mental health’ has served as a unifying force to incorporate mental health into traditional global health work. It has also become a common label for academic training programmes, funding streams, conceptual pieces and empirical research. Although the research under the banner of ‘global mental health’ by no means captures the breadth of work and practice being done to improve the mental health of populations around the world, it clearly shows there is progress being made to include mental health in the mainstream global health agenda.
Funding
This work was supported by the Stanley Center for Psychiatric Research at the Broad Institute of MIT and Harvard. In addition, S.M. is supported by NIH T32 MH 017119 and the Barry R. and Irene Tilenius Bloom Fellowship. E.E.H. is supported by NIH K01 MH116335.
Acknowledgements
Thank you to Alex Cohen for reviewing an earlier draft of this manuscript.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2019.39.







eLetters
No eLetters have been published for this article.