With respect to circadian functionality, individuals differ as to optimal time of day. Those with a preference for activities in the morning are known as ‘morning chronotypes’ whereas those with preferences for evening activities are characterised as ‘evening chronotypes’ (see for example Mueller & HaagReference Mueller and Haag1). The majority of individuals are intermediate in this respect. As early as 1991, Drennan and co-workers showed that patients with depression are mainly characterised with evening chronotypes;Reference Drennan, Klauber, Kripke and Goyette2 however, the studies relating chronotype to a clinical diagnosis of depression are inconsistent.Reference Mueller, Cabanel, Olschinski, Jochim and Kundermann3 More specifically, ‘eveningness’ seems to relate to the severity of the disease as well as indicated by a higher occurrence of suicidal thoughts.Reference Gaspar-Barba, Calati, Cruz-Fuentes, Ontiveros-Uribe, Natale and De Ronchi4 A recent prospective study demonstrated that evening chronotype measured in adolescence predicted the occurrence of depressive episodes 1 year later.Reference Haraden, Mullin and Hankin5 However, beside stability and moderate heritability of the individual chronotype, variance in overt behaviour can be observed due to different factors. There is a clear shift with age, chronotype moving later in adolescence and switching to earlier after 20, gender differences and seasonal modulation.Reference Allebrandt, Teder-Laving, Kantermann, Peters, Campbell and Rudan6 Within a given chronotype time periods of activity can markedly differ according to work or leisure time.Reference Roenneberg, Wirz-Justice and Merrow7 Even a treatment such as cognitive–behavioural therapy, can move patients with depression toward more ‘morningness’.Reference Boland, Bertulis, Leong, Thase and Gehrman8 Thus, day-to-day changes in activity preferences as a result of social cues and the seasonal, and the therapeutic modifiability of the otherwise relatively stable chronotype point to a dynamic and complex synchronisation process.
As circadian mood and activity fluctuations are among the core symptoms of depression (at least in ‘melancholic’ subtypes) we investigated whether patients with depression differ according to their chronotype in consecutive twice-daily mood assessments on weekdays and weekends. For this kind of research question a standardised setting is optimal because the time points of measurements (such as mood ratings) can be planned and controlled. We, therefore, studied only in-patients with depression. We expected interactions between chronotype and weekends (corresponding to leisure time in healthy samples) with the pattern of more negative affect in the morning occurred in those with evening chronotypes and more negative affect in the evening in those with morning chronotypes. For weekdays this pattern will be masked because of therapeutic sessions or other reasons.
Method
A total number of n = 30 patients (all diagnosed with ICD-F32,9 in particular F32.2) between 18 and 50 years old (mean 32.2, s.d. = 8.4, 17 men and 13 women) were compared with a healthy control group of 13 men and 19 women (mean age 32.0, s.d. = 8.3). All participants were fully informed about the study and gave informed written consent. All patients had hospital leave on Saturday and Sunday. This study was part of a larger research project (sleep, circadian rhythmicity, mood and pain perception in patients with affective and affect regulation disorders and healthy controls) and was approved by the ethics committee of the medical faculty of the Justus-Liebig-University of Giessen, Germany. The study is registered in the German Clinical Trials Register (DRKS00010215).
Patients were not entirely free from medication. Treatment consisted of selective serotonin reuptake inhibitors (n = 14), Serotonin-noradrenaline reuptake inhibitors (n = 4), agomelatine (n = 3), tricyclic antidepressants (n = 1) or no medication (n = 8). Patients had a mean Beck Depression Inventory (BDI-II)Reference Beck, Steer and Brown10 score of 26.5 (s.d. = 10.8).
Participants completed the German version of the ‘Morningness-Eveningness Questionnaire’ (MEQ), which has been demonstrated to be reliable and valid.Reference Griefhan, Künemund, Bröde and Mehnert11 The proportion of patients and controls in chronotype categories based on Horne & ÖstbergReference Horne and Ostberg12 with only three categories (moderate evening chronotypes + definite evening chronotype; intermediate; moderate + definite morning chronotype) of the MEQ were: evening type (range 16–41): 5 in the patient group and 5 in the control group; intermediate type (range 42–58): 19 in the patient group and 16 in the control group; and morning type (range 59–86): 6 in the patient group and 11 in the control group. As frequencies especially for the evening chronotype were fairly low, we classified individuals into morning chronotype or evening chronotype according to median split of the MEQ within each group but we also show our results for the three-group classification.
Subjective well-being was measured by a Likert-scale with 14 items having loadings on three factors: negative affect, lack of energy and well-being.Reference Janke, Hüppe and Erdmann13 The present study primarily relates to ‘negative affect’ although ‘lack of energy’ will be used to demonstrate the validity of the grouping used for chronotype. Ratings on emotional states were obtained in the morning (07.00–09.00 h) and in the evening (18.00–20.00 h) starting on Tuesday evening until Thursday 1 week later. Results were calculated only for the 2 days before the weekend, 2 weekend-days and 2 days after the weekend (in the morning and evening, respectively) in order to guarantee that all participants had become familiar with the procedure, which could increase reliability. The design, therefore, consists of two independent factors with two levels each (patients/controls and morning chronotype/evening chronotype) and two within factors with three levels for schedule (weekdays prior weekend/weekend/weekdays after weekend) and two levels for time of day (morning/evening). Data were, therefore, analysed with analysis of variance for repeated measures.
Results
We were able to demonstrate the validity of the MEQ and the way we defined evening chronotype and morning chronotype. A main effect across all time points of measurement and both groups (patients and controls) revealed a higher lack of energy in those with morning chronotypes in the evening and in those with evening chronotypes in the morning (F = 5.7, d.f. = 1,58, P < 0.05). Within-patients chronotype did not relate to severity of disease in our participants as indicated by non-significant differences in BDI (data not shown, t(30) = −0.2, P = 0.8). Moreover, different treatment or gender was not related to chronotype (data not shown).
Regarding ‘negative affect’ a significant three-way-interaction (F = 4.5, d.f. = 2,57, P < 0.05) between group, chronotype and schedule occurred indicating different mood states depending on chronotype and week–weekend schedule especially in patients. These results are nearly identical when excluding the three patients with melatonergic medication (F = 4.63, d.f. = 2,53, P < 0.05). Additionally, we looked at the results based on the categorial classification.Reference Horne and Ostberg12 These are in the same direction but failed to reach significance. For a direct comparison of the two approaches see Fig. 1.
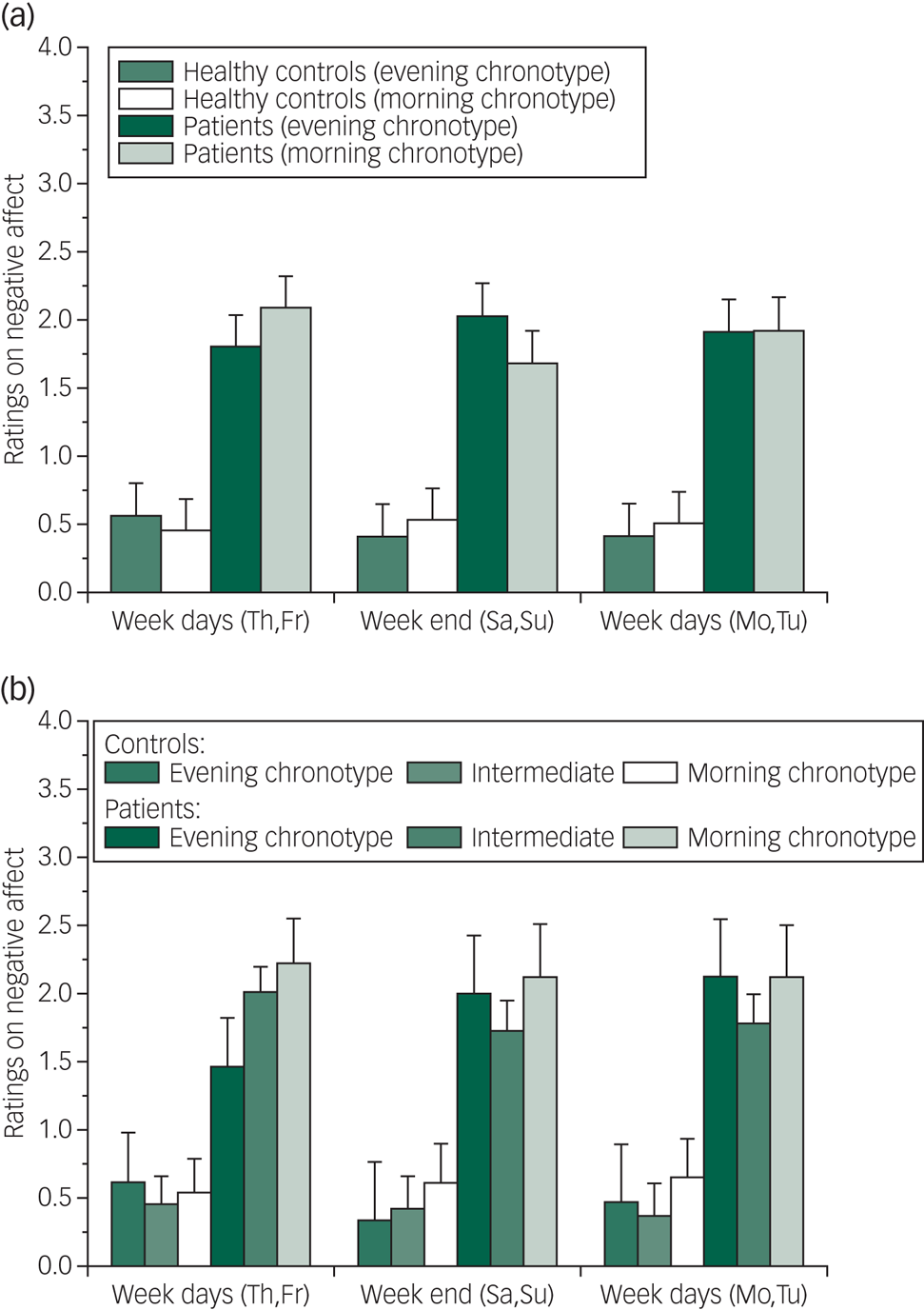
Fig. 1 Negative affect rating in the in-patient and control groups by chronotype and schedule.
Figure 1a indicates that patients with a late chronotype (evening chronotypes) got worse at weekends whereas those with a early chronotype improved. No systematic differences could be statistically confirmed in the healthy control group. In contrast, in patients post hoc tests (for dependent samples) reveal that especially those with morning chronotypes significantly improved at weekends (t(31) = 2.1, P < 0.05) whereas evening chronotypes may get worse at weekends but this contrast did not reach significance. Based on a categorial grouping into evening chronotypes, intermediate and morning chronotypes, the direction of effects is similar but fails to reach statistical significance (presumably because of low numbers in the evening- chronotype and morning-chronotype subgroups).
Discussion
Our results demonstrate that the concept of chronotype may go beyond different preferences and/or activities in the morning or evening. In general, we were able to show that individuals with evening chronotypes complain about less energy in the morning, whereas those with morning chronotypes feel less energetic in the evening. The notion that severity of depression may be more pronounced in patients with a late chronotype could not be confirmed in our study. A direct comparison of BDI-II scale values in patients with depression between those with evening chronotypes and morning chronotypes only indicates somewhat higher values in the evening-chronotype subgroup but this difference did not reach statistical significance.
Our main finding is that the morning chronotype subgroup improved during weekends whereas ratings on negative affect rose in those in-patients in the evening-chronotype subgroup. Note, that all patients had hospital leave on Saturdays and Sundays. Ratings on sleep quality obtained daily for the whole study period did not differ by chronotype (data not shown, so different sleep quality cannot account for the results obtained on mood).
A recent study in patients with bipolar disorders demonstrates that a combination of sleep deprivation and light therapy results in significant decreases in depression symptoms with a better improvement in those with evening chronotypes compared with morning chronotypes or intermediate types.Reference Dallaspezia, Suzuki, Clara, Colombo and Benedetti14 It can be speculated that individuals with evening chronotypes in our study may have an advantage in a clinical setting with therapeutic regimens starting in the early morning. The need to get up early may, therefore, result in (partial) sleep deprivation in those with evening chronotypes, which does not take place at weekends. However, further studies with a larger sample size and grouping into evening chronotypes and morning chronotypes based on the categorial approachReference Horne and Ostberg12 have to address this question explicitly.
The fact that suicide attempts are more frequent and mediated by depression in individuals with evening chronotypesReference Park, Lee and Lee15 means the inclusion of chronotype in the diagnostic process can be recommended.Reference Rumble, Dickson, McCall, Krystal, Case and Rosenquist16 If the finding that in-patients with evening chronotypes probably worsen during weekend hospital leave can be replicated in larger samples (sample size is of course a limitation of our pilot study), special attention is required as many studies demonstrated that suicides peak on Mondays.Reference Massing and Angermeyer17
Acknowledgements
We thank one anonymous reviewer for the constructive and helpful comments.
Author contributions
M.J.M., N.C. and B.K. designed the study and wrote the protocol for the whole research project entitled ‘Sleep, circadian rhythmicity, mood and pain perception in patients with affective and affect regulation disorders and healthy controls’. A.-M.S. and S.F. undertook coordination and gathering of the data. K.F.B. and J.H. analysed and interpreted the data, and wrote the first draft of the manuscript. All authors revised the manuscript, gave final approvement and agreed to be accountable for all aspects of the work.




eLetters
No eLetters have been published for this article.