Introduction
Allergic rhinitis is a common disease affecting up to 50 per cent of the population, with increasing prevalence.Reference Demoly, Fokkens, Terreehorst, Georgalas and Fokkens1 The Allergic Rhinitis and its Impact on Asthma initiative has published treatment recommendations based on a new classification.Reference Bousquet, Khaltaev, Cruz, Denburg, Fokkens and Togias2,Reference Brożek, Bousquet, Baena-Cagnani, Bonini, Canonica and Casale3 This classification categorises allergic rhinitis as intermittent or persistent (based on the number of symptomatic days per week and consecutive weeks per year), and mild or moderate to severe (based on the effect on quality of life). The management of allergic rhinitis includes patient education on the avoidance of allergens, and the use of pharmacotherapy and allergen-specific immunotherapy. Nasal irrigation using saline solutions is also recommended as a complementary treatment for allergic rhinitis, as it can improve symptoms, quality of life and mucociliary clearance time.Reference Hermelingmeier, Weber, Hellmich, Heubach and Mösges4
Hyaluronate is a large non-sulphated glycosaminoglycan that is a key component of the extracellular matrix. Hyaluronate has an important role in mucociliary clearance through the epithelial surface, and in the processes involved in wound healing and mucosal surface repair.Reference Forteza, Lieb, Aoki, Savani, Conner and Salathe5,Reference Manzanares, Monzon, Savani and Salathe6 The addition of intranasal sodium hyaluronate to the pharmacotherapy of allergic rhinitis has been shown to reduce the number of neutrophils seen in the nasal cytology, and to improve several clinical and endoscopic parameters in patients with rhinitis.Reference Gelardi, Iannuzzi and Quaranta7 Pulmonary surfactant works as an expectorant by decreasing the ability of sputum to adhere to the epithelial layer, and by increasing the efficiency of energy transfer from the cilia to the mucus layer, thus improving the mucociliary clearance.Reference Rubin8 Nasal irrigation solutions with surfactant have been shown to effectively improve post-operative symptoms in patients undergoing functional endoscopic sinus surgery.Reference Chiu, Palmer, Woodworth, Doghramji, Cohen and Prince9
Although nasal irrigation solutions with surfactant, sodium hyaluronate and saline have a positive effect on the nasal mucosa, no comparative studies on these three solutions have been published. We aimed to investigate the effect of nasal irrigation with sodium hyaluronate and surfactant solutions on mucociliary clearance time in patients with mild persistent allergic rhinitis when given as an adjunctive treatment.
Materials and methods
A total of 120 patients diagnosed with mild persistent allergic rhinitis were enrolled in this prospective study between March and July 2016. The reason for including only mildly affected patients was to obtain a homogeneous group, as the vast majority of allergic rhinitis patients in our clinic had mild persistent allergic rhinitis. Patients with ciliary dysfunction, marked septum deviation, history of prior nasal surgery, and symptoms of acute or chronic upper airway infection were excluded. The diagnosis of persistent mild allergic rhinitis was confirmed in all patients based on: clinical history (at least a one-year history of symptoms of sneezing, watery rhinorrhoea and nasal blockage), physical examination, positive skin prick test results and positive serum-specific immunoglobulin E (IgE) findings. The skin prick test was considered positive when the wheals were larger than 3 mm at 15 minutes after the test, and the control skin site (tested using saline) was completely negative.Reference Bousquet, Khaltaev, Cruz, Denburg, Fokkens and Togias2 Serum-specific IgE was measured using enzyme-labelled anti-IgE. A cut-off serum IgE level greater than 0.35 kU/l was considered positive.Reference Bousquet, Khaltaev, Cruz, Denburg, Fokkens and Togias2 A combination of a few major recombinant allergens, such as grass or pollen, was used for both the skin prick test and the serum-specific IgE measurement.
Mucociliary clearance time was measured using the saccharine clearance test method described previously in the literature.Reference Inanli, Ozturk, Korkmaz, Tutkun and Batman10 The patient was asked to sit with their head upright. A particle of saccharine, 1.5–2 mm in diameter, was placed on the inferior turbinate, 1–1.5 cm posterior to its anterior end. The patient was then asked to breathe quietly through the nose, and to refrain from sniffing, bending or sneezing. The patient was instructed to swallow continuously at 30 second intervals. The time of the initial perception of a sweet taste was recorded in minutes and accepted as the mucociliary clearance time. In order to avoid placing the saccharine onto the squamous epithelium, all mucociliary clearance time measurements were performed by the same experienced physician using a 0 degree endoscope. This physician was blinded to the type of irrigation solution used. The test was performed before and after the treatment period of one month.
All patients received oral H1 antihistamine (desloratadine, 5 mg daily) and intranasal steroid sprays (triamcinolone acetonide, 256 μg per day, administered as one puff per nostril once daily in the morning) for 30 days, as per the treatment protocol. The patients were allocated randomly to the saline, sodium hyaluronate or surfactant nasal irrigation group. Simple randomisation was performed using computer-generated lists.
The patients were provided with an instruction sheet for nasal irrigation and a commercially available kit, which included a 240 ml irrigation bottle and ready-made sachets for the surfactant, sodium hyaluronate or saline solutions (Abfen Farma, Ankara, Turkey). The saline solution kits included only sachets to prepare the buffered saline (0.9 per cent sodium chloride) nasal irrigation solution. The sodium hyaluronate kits included sachets of saline containing 9 mg sodium hyaluronate. The surfactant solution contained sodium lauryl ether sulphate, cocamidopropyl betaine and polyethylene glycol 200 sorbitan laurate, all of which have the same properties as the surfactants contained in baby shampoo formulations, and the concentrations were measured to comply with the 1 per cent concentration for the nasal irrigation solution. In the surfactant solution kits, one sachet of saline and 2 ml of surfactant solution were added to 240 ml water. The subjects were asked to prepare the irrigation solution using the given instructions and to irrigate their nose (half of the bottle for one nostril and the other half for the other nostril) twice daily for the treatment period of one month.
Statistical analysis
Statistical analysis was conducted using SPSS software, version 15.0 (SPSS, Chicago, USA). The Wilcoxon signed rank test was used to compare the pre- and post-treatment mucociliary clearance times within the groups. Improvements in the mucociliary clearance time were converted to absolute values. The Kruskal–Wallis test was used to compare the post-treatment mucociliary clearance time and the improvement in mucociliary clearance time between the groups. A p-value of less than 0.05 was considered statistically significant. This study was approved by the ethics committee of our institute.
Results
Among the 120 patients enrolled in the study, 38 were assigned to the saline, 40 to the sodium hyaluronate and 42 to the surfactant nasal irrigation group. Five patients from the saline group, 8 from the sodium hyaluronate group and 11 from the surfactant group did not return for the follow-up examination and were excluded from the statistical analysis (Figure 1).
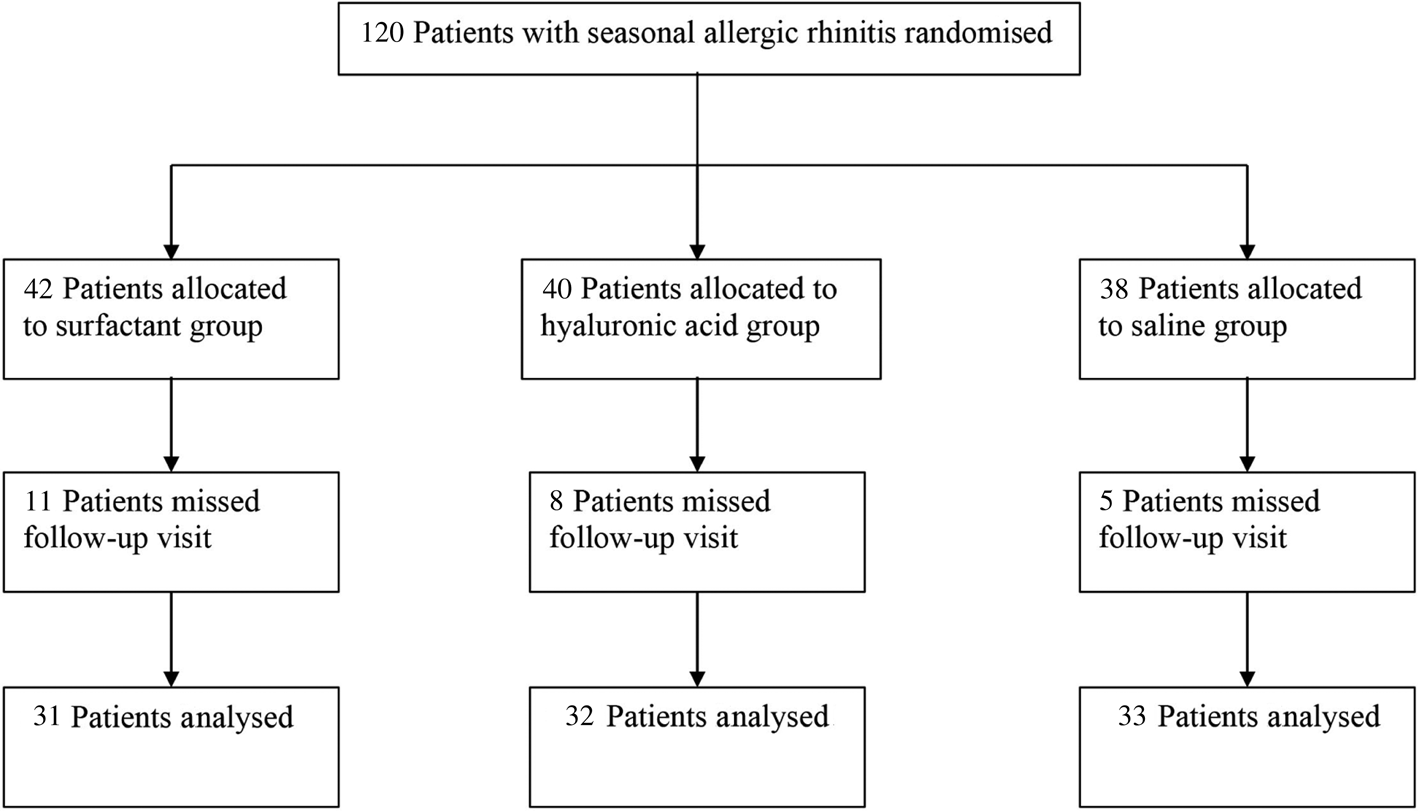
Fig. 1. Flow chart showing distribution of study patients.
The demographic data for each patient group are summarised in Table 1. The pre-treatment mean mucociliary clearance time values were 15.8, 16.3 and 16.2 minutes for the saline, sodium hyaluronate and surfactant groups, respectively (p < 0.05). For all the three groups, a statistically significant improvement was recorded post-treatment compared with pre-treatment (Table 2). When the improvements in the mean mucociliary clearance time were compared among the three groups, the improvement in the surfactant and sodium hyaluronate groups was significantly greater than in the saline group (p < 0.01). Furthermore, the mean post-treatment mucociliary clearance time of the surfactant group was significantly shorter than that of the saline group (p < 0.001) and the sodium hyaluronate group (p = 0.03). A decrease in symptoms was noted for all patients, and no side effects or intolerability were observed.
Table 1. Demographic data for each patient group

Table 2. Mucociliary clearance times for each patient group

Data represent mean (standard deviation) mucociliary clearance times, in minutes.
* Indicates significant difference (p < 0.01) between pre- and post-treatment values.
Discussion
The sodium hyaluronate, surfactant and saline nasal irrigations were all effective in improving mucociliary clearance. However, the sodium hyaluronate and surfactant nasal irrigations had better outcomes in terms of mucociliary clearance time than the saline nasal irrigation when given as an adjunctive treatment in allergic rhinitis patients.
Mucociliary clearance is an important primary defence mechanism that is essential to sustain the normal physiology of the nasal mucosa.Reference Nimsakul, Ruxrungtham, Chusakul, Kanjanaumporn, Aeumjaturapat and Snidvongs11 Moreover, it is an important indicator of nasal physiology and a healthy mucosa. In allergic rhinitis, it can also help in the rapid elimination of allergens from the nasal mucosa. Mucociliary activity can be measured using direct (stroboscopy or micro-oscillography) or indirect (rhinoscintigraphy or saccharine test) methods.Reference Munkholm and Mortensen12 The saccharine clearance test, which was used in our study, is accurate and easy to perform, does not require sophisticated equipment, and does not cause discomfort.Reference Valía, Valero, Pardo, Rentero and Monte13
Saline nasal irrigation using isotonic solutions has been used as an effective complementary treatment for allergic rhinitis.Reference Hermelingmeier, Weber, Hellmich, Heubach and Mösges4 In a systematic review, Hermelingmeier et al. found that saline nasal irrigation in allergic rhinitis patients was well tolerated, inexpensive, easy to use and safe.Reference Hermelingmeier, Weber, Hellmich, Heubach and Mösges4 Surfactant and sodium hyaluronate solutions may have a positive effect on respiratory mucosa because of their molecular features. These solutions increase hydration in the sol layer and enhance mucociliary function. Furthermore, the improvement in ciliary beat activity enables cilia to effectively transport mucus and particles.Reference Randell and Boucher14
Hyaluronate, a basic component of the extracellular matrix, has an important role in mucociliary clearance.Reference Forteza, Lieb, Aoki, Savani, Conner and Salathe5,Reference Manzanares, Monzon, Savani and Salathe6 Gelardi et al. showed that the addition of 9 mg intranasal sodium hyaluronate twice a day as an adjunctive therapy reduced the number of neutrophils seen in the nasal cytology findings of patients with and without allergic rhinitis.Reference Gelardi, Iannuzzi and Quaranta7 Moreover, sodium hyaluronate nasal irrigation was associated with reduced mucociliary clearance times after endoscopic sinus surgery performed to treat nasal polyps.Reference Gelardi, Guglielmi, De Candia, Maffezzoni, Berardi and Quaranta15
Surfactant decreases the ability of sputum to adhere to the epithelial layer, and increases the efficiency of energy transfer from the cilia to the mucus layer, thus improving mucociliary clearance.Reference Rubin8 Chiu et al. found symptomatic improvement after surfactant nasal irrigation (with 1 per cent baby shampoo twice daily) in patients after endoscopic sinus surgery.Reference Chiu, Palmer, Woodworth, Doghramji, Cohen and Prince9 Issacs et al. showed a deterioration in mucociliary clearance time in 27 healthy subjects after nasal irrigation with 50 ml saline solution containing 1 per cent baby shampoo as the surfactant solution.Reference Isaacs, Fakhri, Luong, Whited and Citardi16 They measured the mucociliary clearance time at 15 minutes after the surfactant irrigation and administered it only once. This result can be interpreted as the surfactant having a positive effect on mucociliary clearance time with continuous or long-term use.
The current literature lacks studies that compare sodium hyaluronate and surfactant nasal irrigation solutions. In our study, we compared both solution types and found that surfactant nasal irrigations resulted in a better mucociliary clearance time in allergic rhinitis patients. To the best of our knowledge, this study is the first to show the superiority of surfactant nasal irrigation over sodium hyaluronate solution. The mechanism of this positive effect on the nasal mucosa is considered to depend on alteration of the airway mucus viscosity, thereby making it easier to clear by either coughing or ciliary movement.Reference Fahy and Dickey17 However, histological and further randomised controlled studies confirming the positive effects are needed.
One limitation of this study is the lack of a group of patients treated without any nasal irrigation solution. However, as the positive effects of saline nasal irrigation on allergic rhinitis had been studied previously,Reference Hermelingmeier, Weber, Hellmich, Heubach and Mösges4 we did not include a control group that did not receive any nasal irrigation solutions in the study design. Instead, the patients receiving the saline nasal irrigation served as the control group, because we aimed to evaluate the effects of sodium hyaluronate and surfactant nasal irrigations compared with those of saline nasal irrigation. Another limitation is the absence of quality of life and olfactory measurements for examination of clinical improvement. Nevertheless, we recorded symptom relief in all patients in each group.
Chiu et al. reported two patients who discontinued using surfactant nasal irrigation: one terminated use because of nasal burning and discomfort, and one because of a rash.Reference Chiu, Palmer, Woodworth, Doghramji, Cohen and Prince9 Turner et al. associated surfactant nasal irrigation with the increased prevalence of congestion and clinically meaningful loss of olfactory acuity.Reference Turner, Wu, Dorminy and Chandra18 According to the literature, nasal irrigation solutions are generally well tolerated, except for some mild and temporary adverse events, such as local irritation.Reference Head, Snidvongs, Glew, Scadding, Schilder and Philpott19 Although we did not measure olfactory functions and quality of life, none of our surfactant group patients experienced any side effects or discomfort. According to our data, surfactant and sodium hyaluronate solutions were well tolerated.
In summary, surfactant and sodium hyaluronate nasal irrigation solutions served as effective and safe alternatives to saline nasal irrigation when used as an adjunctive treatment for allergic rhinitis. Both surfactant and sodium hyaluronate have been shown to have important effects on the respiratory mucosa. Nonetheless, our data indicated that surfactant nasal irrigation solution resulted in better mucociliary clearance time in patients with allergic rhinitis.
• This study evaluated the effect of nasal irrigation with sodium hyaluronate and surfactant solutions on mucociliary clearance time in mild persistent allergic rhinitis patients
• Mucociliary clearance time improvements were significantly higher in the surfactant and sodium hyaluronate groups than in the control group
• Surfactant and sodium hyaluronate nasal irrigation solutions may both be used as adjunctive treatments for allergic rhinitis
Competing interests
None declared





