Introduction
Individuals living with serious mental illness (SMI), inclusive of major depressive disorder, schizophrenia and bipolar disorder, experience premature mortality [Reference De Hert, Correll, Bobes, Cetkovich‐Bakmas, Cohen and Asai1], increased morbidity (e.g., type 2 diabetes [Reference Stubbs, Vancampfort, De Hert and Mitchell2], metabolic syndrome, and cardiovascular disease [Reference Correll, Solmi, Veronese, Bortolato, Rosson and Santonastaso3]), and higher rates of obesity [Reference Pearsall, Smith, Pelosi and Geddes4,Reference Firth, Siddiqi, Koyanagi, Siskind, Rosenbaum and Galletly5] are compared with the general population.
Reducing the premature death rate by targeting the physical health conditions experienced by people living with SMI is complex and multifactorial. One way to address this mortality gap is by modifying behavioral risk factors [6–8], including physical inactivity (or sedentary behavior). Physical activity (PA), encompassing the wider domains of exercise and sport, may have a crucial role in addressing the health inequalities experienced by people living with SMI, in addressing premature mortality, in preventing the onset of comorbidities, and in improving the overall health and wellbeing of this population [Reference Ashdown-Franks, Williams, Vancampfort, Firth, Schuch and Hubbard9].
The benefits of PA for people living with SMI include improvements in psychiatric symptoms, quality of life, physical fitness, cardiometabolic risk factors, body mass index, and weight [Reference Stubbs, Vancampfort, Hallgren, Firth, Veronese and Solmi10]. There is also promising evidence that community-based PA (in a group situation) can reduce social isolation, stigmatization, and can enhance social identity in people living with SMI [11–14]. Indeed, the World Health Organization’s Mental Health Action Plan 2013–2020 called for the provision of mental health services integrated in communities for service users and families [15]. People living with SMI, however, engage in significantly less PA and greater amounts of sedentary behavior compared with the general population [6–8,Reference Ussher, Stanbury, Cheeseman and Faulkner16,Reference Vancampfort, Firth, Schuch, Rosenbaum, Mugisha and Hallgren17]. For example, half of the people living with SMI do not meet the guidelines of 150 min per week of moderate intensity PA [Reference Vancampfort, Firth, Schuch, Rosenbaum, Mugisha and Hallgren17]. This is despite research showing that people living with SMI want to undertake PA [Reference Mishu, Peckham, Heron, Tew, Stubbs and Gilbody18,Reference Firth, Rosenbaum, Stubbs, Gorczynski, Yung and Vancampfort19].
A better understanding of how to promote PA in a way that is engaging, appealing, and socially supportive for people living with SMI is much needed. With this in mind, the purpose of this review is to explore the initiation of community-based group PA in people with SMI. We define initiation as “the period in which people start being more physically active (also referred to as “adoption” and “uptake”)” (p. 3) [Reference Quirk, Crank, Harrop, Hock and Copeland20]. Given the range of barriers faced by people living with SMI when trying to engage in PA (e.g., low mood, stress, or lack of support) [Reference Firth, Rosenbaum, Stubbs, Gorczynski, Yung and Vancampfort19], a thorough exploration of the lived experience of initiation, rather than maintenance of PA, appears important. To achieve this, we undertook a meta-synthesis [Reference Hannes and Lockwood21] of qualitative studies adopting a meta-ethnographic approach [Reference Noblit and Hare22]. Meta-ethnography seeks to uncover a new understanding of a phenomenon that is greater than that contained within individual studies. Its strength lies in its attempt to preserve the interpretive properties of the original qualitative data. Specifically, our meta-ethnography aimed to:
-
• Systematically search and appraise qualitative research on the experience of initiating community-based group PA for adults living with SMI.
-
• Synthesize findings from existing research regarding the experience of initiating community-based group PA and key features of social support within these contexts for people living with SMI.
-
• Identify from participants’ experiences the active ingredients that could inform future interventions to improve uptake of community-based group PA among people living with SMI.
Methods
Detailed information on the methods undertaken in this review are published in the protocol [Reference Quirk, Crank, Harrop, Hock and Copeland20]. The review was registered in the International Prospective Register of Systematic Reviews: CRD42017059948. Noblit and Hare’s (1988) meta-ethnography approach comprises seven stages, with the review authors moving back and forth between stages four and six as ideas for translation and synthesis are explored. The review is reported in accordance with eMERGe meta-ethnography reporting guidance [Reference France, Cunningham, Ring, Uny, Duncan and Jepson23]. The findings of the review were discussed with two individuals living with SMI with the purpose of sense checking themes and findings. This involved one reviewer (HQ) having an informal conversation with each individual in which the initiation journey was discussed. Individuals were asked to comment on whether the review team’s interpretation of the data was clear and easy to understand.
Search strategy
The bibliographic databases searched were ASSIA (ProQuest), CINAHL (EBSCO), Cochrane Central Register of Controlled Trials (Wiley), Health Technology Assessment Database (Wiley), MEDLINE (EBSCO), PsycINFO (ProQuest), Sociological Abstracts (ProQuest), SportDiscus (EBSCO), and Web of Science (Thomson Reuters, now Clarivate). Reviewers searched the author list and reference lists of all papers included in the review for other potentially eligible papers. No date limits were applied. Only papers published in the English language were included. The search strategy is identical to that published in the protocol [Reference Quirk, Crank, Harrop, Hock and Copeland20], with the addition of two new terms “autobiographical” and “mental health” that the team recognized as necessary after initial searches.
Search processes
Literature searches were undertaken in November 2017 by an experienced Information Scientist (DH). All results from the literature searches were exported to the bibliographic software, RefWorks (Ex Libris). This tool, instead of EndNote (Clarivate) as indicated in the protocol, was selected as a majority of the review team were familiar with this resource. RefWorks was also used to remove duplicate papers.
Selecting primary studies
The selection process was divided equally among four reviewers (DH, EH, HC, and HQ) with a fifth reviewer (RC) available to advise on the overall approach. All papers were screened by one of the reviewers and 10% were independently double checked by a second reviewer. Eligibility criteria are described in detail by Quirk et al. [Reference Quirk, Crank, Harrop, Hock and Copeland20]. In brief,
-
• Population—adults (≥18 years) living with SMI, defined as a primary diagnosis (as described in the studies) of schizophrenia, bipolar affective disorder, major depressive disorder, personality disorder, severe anxiety (including phobia and obsessive–compulsive disorder), schizophreniform disorder, or psychosis. If the population was described as those with SMI, but the specific condition was not reported, the paper was considered for review.
-
• Intervention—community-based group PA (inclusive of sport and exercise and any frequency, intensity or duration). The PA needed to take place in the community (i.e., those that take place outside of hospital, clinical, residential, or care settings), with a group being defined as a minimum of three people. If the intervention was multicomponent, PA needed to be a main component and the findings needed to be attributable to the PA.
-
• Comparison—if an intervention was described, no comparator condition was needed. Where a comparison was made, the comparator could be no activity or any other activity.
-
• Outcomes—qualitative data from the perspective of the participant living with SMI reporting the experience of initiating community-based group PA. Initiation was defined as the period in which people first start to engage in a PA. The initiation period could represent the first participation occasion or period of PA engagement, as long as findings could be attributable to the early phase of participation.
-
• Setting—community-based group setting.
Outcome of study selection
The database searches yielded 18,727 papers. After the removal of duplicates, there were 11,804 unique papers. All were screened using the title and abstract against the eligibility criteria. Following this process, 366 papers were retained for full-text screening. Sixteen papers met the eligibility criteria and were included in this review. A summary of the search and screening process is shown in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (Figure 1).

Figure 1. PRISMA flow diagram.
Data extraction and quality appraisal
The data extraction method is outlined by Quirk et al. [Reference Quirk, Crank, Harrop, Hock and Copeland20]. The extraction and quality appraisal document were piloted by the four members of the review team using two of the papers included in the review. Verbatim quotes from the findings and primary author statements were extracted and grouped into themes and subthemes, being careful to keep these distinct from the reviewers’ own comments or interpretations. Each reviewer’s data extraction tables were cross-checked by a second reviewer and any disagreement or discrepancies were resolved via discussion between the review team. The quality of each of the papers was assessed using the Critical Appraisal Skills Program (CASP) Qualitative Checklist [24]. Critical appraisals of all papers were cross-checked by a second reviewer and any discrepancies resolved via discussion among the review team.
Translating second-order concepts
The outcomes extracted from primary studies were used to determine how studies were related (as per Noblit and Hare [Reference Noblit and Hare22]) and identify the “key concepts”. The “key concepts” were themes that seemed particularly salient to the initiation of community-based group PA for people living with SMI. Each reviewer identified the key concepts in the studies they extracted and appraised. The key concepts were then copied into a “key themes and concepts” table, again preserving the meaning and source of the original text by copying quotes and study author comments verbatim and highlighting original participant quotes as first-order concepts, study author comments as second-order concepts, and reviewer interpretations as third-order concepts [Reference Britten, Campbell, Pope, Donovan, Morgan and Pill25]. The “key themes and concepts” table helped the review team to identify patterns and relationships within and between studies. Translating second-order concepts was entirely grounded in the data. It was not guided by theory nor was the intention to substantiate or compare against previous theories or models of behavior change. For the same reason, our definition of initiation did not derive from any specific theory of behavior.
Translating studies into one another
To generate third-order concepts, an Excel spreadsheet was created for each paper included in the study. The Excel spreadsheet outlined the first- and second-order concepts and a third column allowed the reviewer to add their own conceptualization of the theme/subtheme. Reviewers (HC, DH, EH, and HQ) followed step 5 of Noblit and Hare’s approach by exploring how the key themes and concepts related to each other. This was an iterative process determined by how much the studies agreed or disagreed with each other.
Synthesizing translations
In meta-ethnography, the product of synthesis is the translation of study findings into one another to reach a new interpretation of the phenomenon being studied [Reference France, Cunningham, Ring, Uny, Duncan and Jepson23]. A series of review team meetings were held to synthesize the third-order concepts for each theme/subtheme. To ensure conceptualizations remained grounded in the original papers, cross-checks were continually made to the first- and second-order concepts. According to Noblit and Hare, studies can relate to one another in three ways: they may be directly comparable (reciprocal translations); they may stand in opposition to one another (refutational translations); or taken together they may represent a line of argument. A “line of argument” synthesis approach was used because the papers focused on different types of PA experiences that could usefully be brought together to construct overarching arguments about phenomena (stage 6; [Reference Noblit and Hare22]). We did not identify any cases where concepts were strongly contested across papers (i.e., refutational translations [Reference Noblit and Hare22]). Where findings from studies refuted other studies, these were noted.
Expressing the synthesis
Key concepts identified across the papers, combined with a priority to retain the individual voice of people living with SMI, led to presenting this as a “journey” to visualize the complexity of the findings and identify potential phases of PA initiation. The phases of a person’s journey in the initiation of community-based PA were identified as: thinking about being active, planning and preparing for the activity, getting to the activity, and beginning the activity. In this case, the process of moving through the phases was cyclical, with people moving back and forth between phases as well as being static for extended periods of time. The service users viewed our interpretation as an accurate reflection of their own experience and likened our proposed journey to the “SMI recovery journey”.
Confidence in cumulative evidence
Two reviewers applied the Confidence in the Evidence from Reviews of Qualitative Research (CERQual) tool to the review findings [Reference Lewin, Booth, Glenton, Munthe-Kaas, Rashidian and Wainwright26]. CERQual assesses confidence in evidence based on four components contributing to each review finding: the methodological limitations, the relevance, the coherence, and the adequacy of the data. The assessment of each component allows for a judgment of confidence; high, moderate, low, or very low. High confidence in a finding would suggest that it is highly likely that the review finding is a reasonable representation of the phenomenon of interest [Reference Lewin, Booth, Glenton, Munthe-Kaas, Rashidian and Wainwright26].
Results
Description of included studies
Sixteen studies (of 198 participants) were included for review. An overview of the characteristics of the studies is provided in Table 1. The studies were published between 2003 and 2017 and were conducted in the United Kingdom (n = 9), the United States (n = 3), Canada (n = 1), and Sweden (n = 1). Two did not report the location. A range of different PA types, interventions, and participants were represented. Nine studies included people living with a range of diagnoses [Reference Carless and Sparkes13,Reference Carless and Douglas29,Reference Carless and Douglas32,Reference Graham, Larstone, Griffiths, de Leeuw, Anderson and Powell-Hellyer36,Reference Hodgson, McCulloch and Fox37,39–41]. Five studies included people living with schizophrenia or schizoaffective disorder [Reference Bizub, Joy and Davidson27,Reference Carless28,Reference Evans34,Reference Faulkner and Sparkes35,Reference Hoffmann38] and four studies did not report the specific diagnosis, but instead reported a diagnosis of SMI [Reference Carless and Douglas30,Reference Carless and Douglas31,Reference Crone33].
Table 1. Study characteristics of included studies.

Abbreviations: BMI, body mass index; DSM-IV, 4th edition of the Diagnostic and Statistical Manual; NA, not applicable; NHS, National Health Service; NR, not reported; NS, (gender) not specified; PTSD, post-traumatic stress disorder; SMI, serious mental illness; UK, United Kingdom; USA, United States of America.
PA interventions varied across studies and included the following: walking group [Reference Crone33], walking and swimming [Reference Faulkner and Sparkes35], horse-riding [Reference Bizub, Joy and Davidson27], golf [Reference Carless and Douglas29], swimming [Reference Evans34], low impact walking and yoga [Reference Graham, Larstone, Griffiths, de Leeuw, Anderson and Powell-Hellyer36], and various activities including team sports [Reference Carless28,30–32,37–41]. The majority involved PA facilitated by an instructor or leader (n = 9). Five interventions were self-directed activities. In three studies, level of facilitation was unclear. See Table 2. for intervention characteristics. Descriptions of the interventions can be found in Supplement 1.
Table 2. Intervention characteristics of included studies.
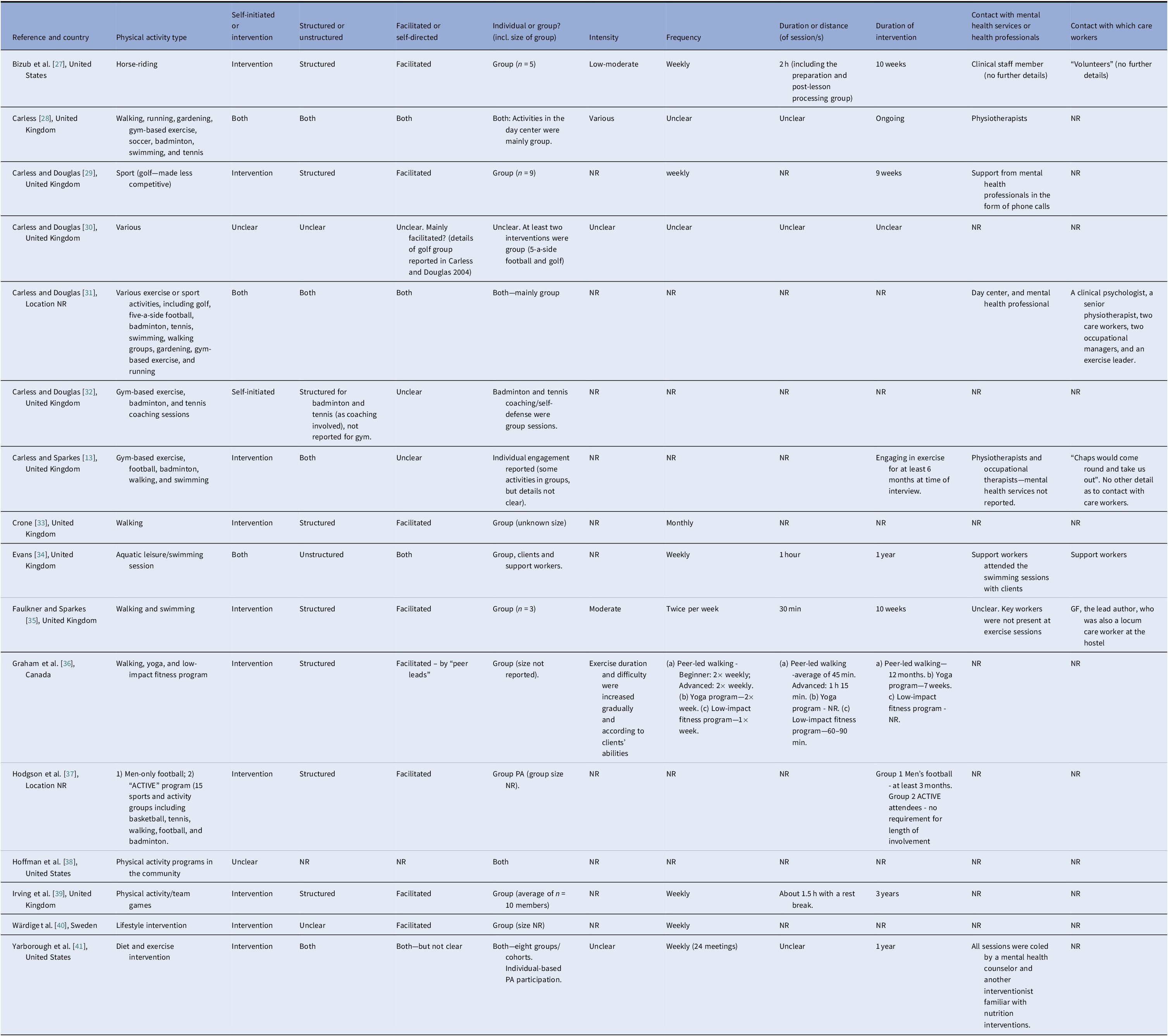
Abbreviations: h, hour(s); min, minute(s); NR, not reported; PA, physical activity; SMI, serious mental illness; UK, United Kingdom; USA, United States of America.
Quality of included studies
Using CASP, we judged that qualitative methods were appropriate in all studies and most studies had a clear statement of aims, an appropriate research design, data collection in a way that addressed the research issue, a clear statement of findings, and value in terms of practical application, and aiding our understanding of community-based PA for people living with SMI. Study quality varied in terms of having an appropriate recruitment strategy to support the aims, whether ethical issues were taken into consideration and if data analysis was sufficiently rigorous. Most studies did not adequately consider the relationship between researcher/s and participants. A summary of the methodological quality of studies is provided in Supplement 2.
Synthesizing translations/line of argument
Table 3 shows a list of all the second-order constructs, using the original authors’ own words or a paraphrase to maintain the language used in each study [Reference Soundy, Kingstone and Coffee11,Reference Doyle42]. When grouping second-order constructs into broader categories, we noticed a temporal sequence or “journey”. The “journey” captured a long sequence of phases which, although presented sequentially, is not linear in practice (Figure 2).
Table 3. First- and second-order construct table.
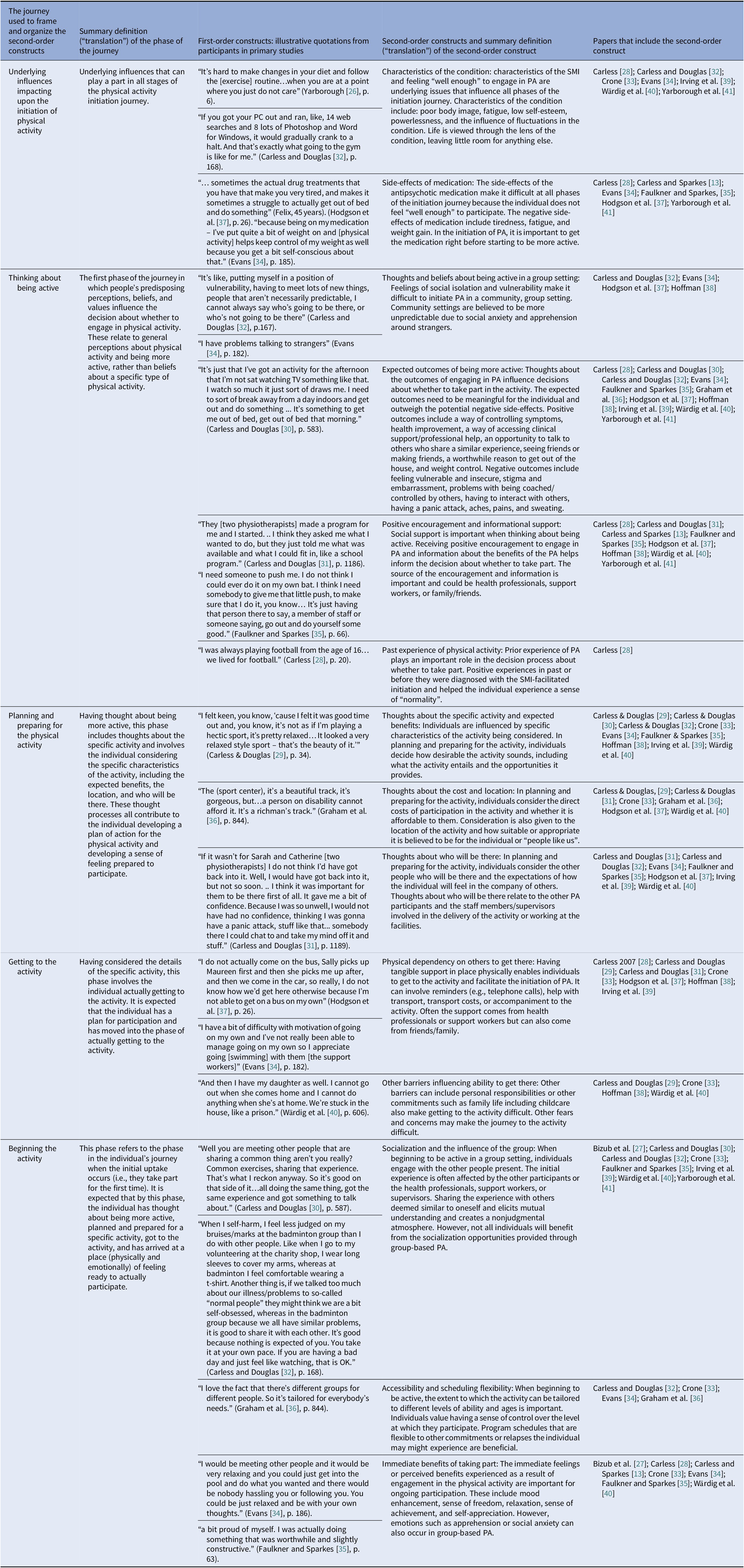
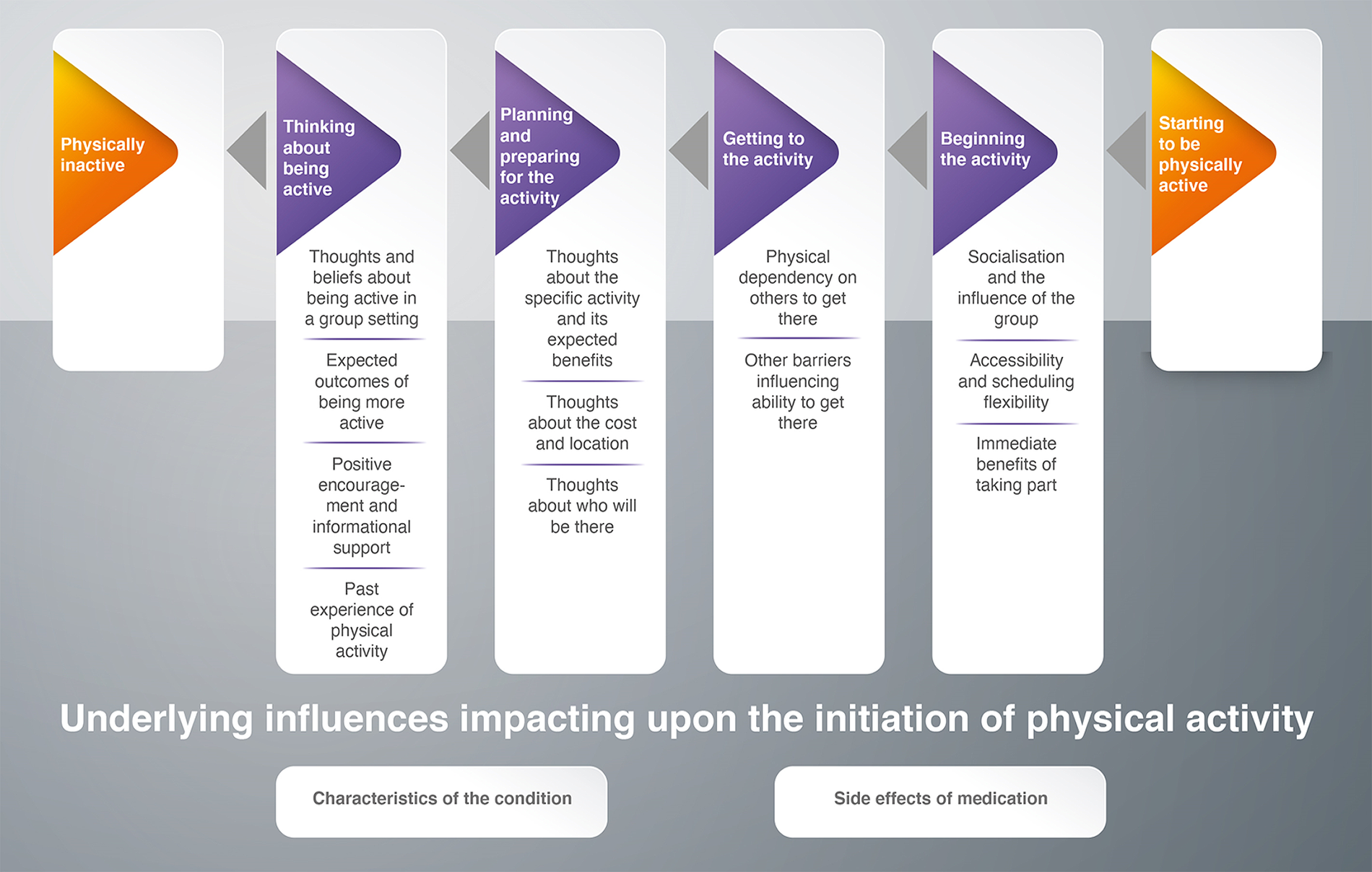
Figure 2. The journey of physical activity initiation for people living with SMI.
The journey of PA initiation for people living with SMI
Table 3 gives a narrative “translation” of each second-order construct.
Underlying Influences Impacting upon the Initiation of PA
Two subthemes were identified representing underlying influences that play a part across the initiation journey. Characteristics of SMI that affected people’s ability to initiate PA were low self-esteem, feelings of failure, and/or powerlessness—especially after a failed attempt at initiating PA [Reference Evans34,Reference Wärdig, Bachrach-Lindström, Foldemo, Lindström and Hultsjö40,Reference Yarborough, Stumbo, Yarborough, Young and Green41]. For some people dealing with SMI was all-consuming and left little space in their life for anything else [Reference Carless and Douglas32,Reference Wärdig, Bachrach-Lindström, Foldemo, Lindström and Hultsjö40].
Another challenge was side-effects of medication that caused people to lack motivation, feel drowsy and sluggish, or too ill to participate in PA [Reference Carless and Sparkes13,Reference Evans34,Reference Faulkner and Sparkes35,Reference Hodgson, McCulloch and Fox37,Reference Yarborough, Stumbo, Yarborough, Young and Green41]. Getting the medication right to feel “well enough” to partake in PA was important to reduce any setbacks in PA initiation [Reference Carless and Sparkes13,Reference Carless28]. Weight gain or being overweight was considered a side-effect of medication and was spoken about in relation to feelings of poor body image and insecurity [Reference Carless and Douglas32,Reference Evans34,Reference Faulkner and Sparkes35].
Thinking About Being Active
In the first phase of the journey, predisposing perceptions, beliefs, and values influence the decision to engage in PA. These relate to perceptions about PA in general, rather than beliefs about a specific type of PA, which come later in the journey. Four subthemes were identified within this phase of the journey: thoughts and beliefs about being active in a group setting, expected outcomes of being more active, positive encouragement and informational support, and past experience of PA. People living with SMI talked about feeling vulnerable in unpredictable group settings due to social anxiety, embarrassment, and apprehension around strangers [Reference Carless and Douglas32,Reference Evans34,36–38,Reference Wärdig, Bachrach-Lindström, Foldemo, Lindström and Hultsjö40].
While the perceived benefits of PA varied across studies (e.g., a worthwhile reason to get out of the house [or other residential setting] [Reference Carless and Sparkes13,Reference Carless28,Reference Evans34,Reference Irving, Flockton and Webster39] and weight control [Reference Carless28,Reference Faulkner and Sparkes35,Reference Hoffmann38,Reference Wärdig, Bachrach-Lindström, Foldemo, Lindström and Hultsjö40,Reference Yarborough, Stumbo, Yarborough, Young and Green41]), expected outcomes needed to be meaningful and outweigh the perceived negative effects for individuals to move to the next step in the journey. Positive encouragement from trusted sources was important when people were thinking about increasing PA [Reference Carless and Douglas31,Reference Faulkner and Sparkes35]. This included initial awareness-raising via information-giving from health professionals (e.g., about the benefits of PA) and verbal persuasion [Reference Carless and Sparkes13,Reference Carless28,Reference Carless and Douglas31,Reference Hoffmann38]. On the whole, people living with SMI understood the benefits of PA [Reference Hoffmann38,Reference Yarborough, Stumbo, Yarborough, Young and Green41], so information about what was available in their local community and encouraging people to engage with what was available was most beneficial. Finally, having a previous positive experience of PA was also beneficial when thinking about being active, providing a sense of “normality” for those who had been active prior to their SMI diagnosis [Reference Carless28].
Planning and Preparing for the PA
Having thought about being more active, the planning and preparing phase of the journey involves developing an action plan and preparing for the activity. Three themes were identified within this phase: thoughts about the specific activity and its expected benefits, thoughts about cost and location, and thoughts about who will be there. In thinking about activities, people living with SMI considered how desirable the specific activity seemed compared to alternative options [Reference Carless and Douglas29,33–35]. Often, the expected benefits of community-based PA related to having something to do and somewhere to go, rather than specific to the activity itself; doing something is better than doing nothing [Reference Carless and Douglas30,33–35,Reference Irving, Flockton and Webster39].
People living with SMI often felt unable to participate due to the activity being financially or physically inaccessible [Reference Carless and Douglas31,Reference Hodgson, McCulloch and Fox37,Reference Wärdig, Bachrach-Lindström, Foldemo, Lindström and Hultsjö40]. Activities had to be affordable to be perceived as sustainable [Reference Carless and Douglas29,Reference Graham, Larstone, Griffiths, de Leeuw, Anderson and Powell-Hellyer36]. People living with SMI benefited from feeling familiar with the location and easily being able to travel the distance to get there, as well as feeling they belong at the location [Reference Graham, Larstone, Griffiths, de Leeuw, Anderson and Powell-Hellyer36].
Thinking about socializing with others, including staff delivering and facilitating the session, was appealing to some [Reference Carless and Douglas32,Reference Faulkner and Sparkes35,Reference Hodgson, McCulloch and Fox37], but others felt apprehensive about having to have conversations with other people [Reference Evans34,Reference Irving, Flockton and Webster39,Reference Wärdig, Bachrach-Lindström, Foldemo, Lindström and Hultsjö40]. The presence of trusted and known health professionals or members of the mental health support team was valued and believed to instill confidence among people living with SMI initiating a new PA [31–33,Reference Faulkner and Sparkes35].
Getting to the Activity
The next phase involves putting plans into action. Two themes were identified within this phase of the journey: physical dependency on others to get there and other barriers influencing ability to get there. People living with SMI often depended on intensive support from other people to get out of the house (or other residential setting) and to the activity (e.g., reminders, transportation, travel expenses [Reference Hoffmann38], and accompaniment [Reference Carless28,Reference Carless and Douglas29,Reference Carless and Douglas31,Reference Crone33,Reference Irving, Flockton and Webster39]). Personal responsibilities or other commitments such as family life and childcare also made getting to the activity difficult [Reference Crone33,Reference Hoffmann38,Reference Wärdig, Bachrach-Lindström, Foldemo, Lindström and Hultsjö40].
Beginning the Activity
This phase refers to taking part for the first time. Three themes were identified: socialization and the influence of the group, accessibility and scheduling, and immediate benefits of taking part. The first experience was influenced by the other people present. A supportive atmosphere and feeling safe in the company of others fostered connectedness and mutual understanding [Reference Carless and Douglas30,32–35,Reference Wärdig, Bachrach-Lindström, Foldemo, Lindström and Hultsjö40,Reference Yarborough, Stumbo, Yarborough, Young and Green41]. Welcoming and supportive staff instilled confidence [Reference Bizub, Joy and Davidson27,Reference Carless and Douglas32,Reference Crone33,Reference Faulkner and Sparkes35,Reference Irving, Flockton and Webster39]. People living with SMI benefited from knowing what to expect before arriving and from knowing that the schedule was adaptable to their needs (e.g., symptoms, health relapses, and ability). They also valued autonomy to decide their level of participation [32–34,Reference Graham, Larstone, Griffiths, de Leeuw, Anderson and Powell-Hellyer36]. The immediate perceived benefits of taking part such as enjoyment or mood enhancement, relaxation, and sense of achievement were important contributors to the successful initiation of PA [Reference Carless and Sparkes13,Reference Carless28,33–35,Reference Wärdig, Bachrach-Lindström, Foldemo, Lindström and Hultsjö40].
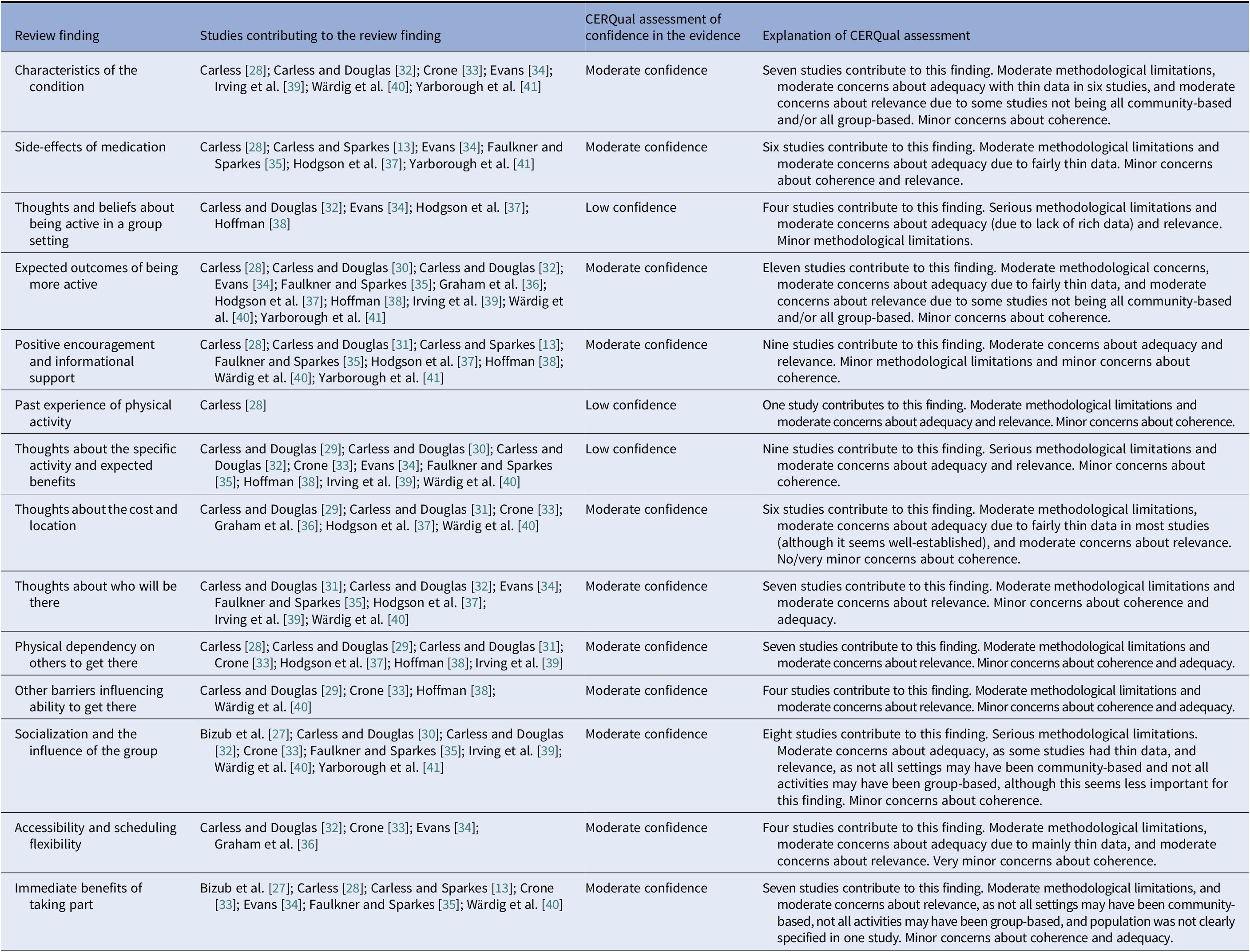
Confidence in the cumulative evidence
The CERQual assessment of our level of confidence in the findings indicated that more and/or better quality primary research is needed in this area. On the basis of our CERQual assessment of the review findings, we have moderate confidence in 11 findings and low confidence in three findings (see Table 4. for the CERQual assessment).
Table 4. CERQual summary of qualitative findings table.
Discussion
The current review aimed to explore how adults diagnosed with SMI experience the initiation of community-based group PA and key features of social support within these contexts. Findings illustrate that initiation of PA in community group-based contexts is not a simple step from intention to participation. The journey is not always linear, but a slow process with challenges or setbacks at every phase. Similar to Soundy et al. [Reference Soundy, Kingstone and Coffee11], our findings demonstrate the challenges, complex processes, and facilitators that exist before PA even begins for people with SMI. These are associated with thinking about being active, planning and preparing for PA, getting to the activity, and beginning the activity. The journey we present enhances the existing evidence base by providing in-depth exploration of the complexities of the initiation process specific to community-based group PA.
We identified some of the benefits and challenges that characterize group PA in the community setting for people living with SMI. Beneficial qualities include having a reason to get out of the house (or other residential setting), socializing, and feeling connected with others. Challenges involve feelings of vulnerability and social anxiety, dependency on others to provide or pay for transport, and the perceived appropriateness of the activity setting. Furthermore, the cost of some activities (e.g., golf) may preclude participation compared to lower cost activities. People also benefited from knowing what to expect from the activity and facilities prior to attending and we identified a need for a supportive, safe, and nonjudgmental atmosphere. Flexibility in scheduling of PA was also important, as reflected in the UK practitioner guidelines for people working in mental health services [Reference Grant43].
The current review highlighted the importance of taking an individualized approach to PA promotion in people with SMI. This could be likened to a person-centered care approach [44, Reference Blomqvist, Sandgren, Carlsson and Jormfeldt45] and in that it takes into consideration an individuals’ values, self-identify, family situation, social circumstances, past experiences, beliefs, and preferences as well as medication, motivation, available support, and cost of the activity (including transport and other associated costs). Expectations about the outcome of the activity can impact whether or not, how, and when people living with SMI initiate PA. Previous findings from quantitative studies in this population have identified health-related outcomes as important motivators for PA engagement [Reference Firth, Rosenbaum, Stubbs, Gorczynski, Yung and Vancampfort19]. Our findings support health-related outcomes such as weight control as important motivators, but also suggest that the desired outcome of the PA might be more about having somewhere to go and something to do.
The intensive nature of the social support required during the initiation of community-based group PA for people living with SMI is a key outcome from this study. The need for instrumental and informational support has been demonstrated previously [Reference Soundy, Freeman, Stubbs, Probst, Coffee and Vancampfort14], as has emotional support [Reference Soundy, Freeman, Stubbs, Probst, Roskell and Vancampfort46]. We identified that sources of support need to come from someone who is valued and respected by the person living with SMI and someone who knows them well and is well known to them, which supports previous findings [Reference Soundy, Freeman, Stubbs, Probst, Roskell and Vancampfort46]. Consistent with previous research, this could be provided by mental health professionals such as physiotherapists and occupational therapists [Reference Mason and Holt47]. While some people with SMI are comfortable in accepting support from professionals, others do not want this [Reference Raine, Truman and Southerst48] and prefer support from trusted caregivers, friends, and family [Reference Lassenius, Arman, Söderlund and Wiklund-Gustin49].
Social support from others living with SMI was also found to be important as it provided a supportive and “safe” atmosphere. This was particularly important for those with low self-image and confidence, providing a sense of togetherness and shared identity of doing something “normal” without feeling judged or stigmatized. This supports previous findings about the importance of shared identities by people attending group-based PAs [Reference Soundy, Kingstone and Coffee11,Reference Crone33,Reference Soundy, Freeman, Stubbs, Probst, Roskell and Vancampfort46]. Providing people with SMI with a safe environment within which to make choices and decisions about their participation could translate into benefits in different areas of life [Reference Soundy, Kingstone and Coffee11,Reference Soundy, Freeman, Stubbs, Probst, Coffee and Vancampfort14,Reference Soundy, Freeman, Stubbs, Probst, Roskell and Vancampfort46]. Carless and Douglas [Reference Carless and Douglas50] likened this to having a door opened that is usually shut for people living with SMI.
Implications for Future Research
This review has demonstrated the importance of intensive social support in the initiation of community-based group PA. It is not clear, however, how long this intensive support and close interaction is needed to facilitate successful initiation of the activity. Further research should explore whether the support needs to be consistent for the duration of participation and the implications of a break or change in the level of support provided. Carless [Reference Carless28] suggests that progress from initiation to maintenance of PA among people living with SMI can take years rather than weeks or months (as per a more traditional definition of initiation [Reference Prochaska, Redding and Evers51]). Using qualitative research to really understand the unique experience of the journey preceding each PA session is needed to help ensure the sustainability of programs and related outcomes. Further research exploring the continuation of PA, to establish the extent to which the factors involved are similar to those for initiation, appears warranted.
Many of the findings included in our review were derived from bespoke interventions that involved services that would not normally be available for people living with SMI in the community (e.g., golf lessons and exclusive access to a swimming pool). A recent position statement for PA as treatment for SMI by Stubbs and colleagues [Reference Stubbs, Vancampfort, Hallgren, Firth, Veronese and Solmi10] has called for “replicable and scalable methods for delivering PA interventions to people living with SMI, in a format which is accessible, engaging, and effective for large numbers of patients” (p. 140). It is currently unclear whether PA is a cost-effective treatment option for people living with SMI and more work is needed to establish whether the financial implications are offset by the benefits [Reference Stubbs, Vancampfort, Hallgren, Firth, Veronese and Solmi10]. This raises important questions about the extent to which the findings included in this review can be generalized to the broader community of people living with SMI and suggests that further research is needed to explore the experience of community-based PA initiation in everyday life.
Strengths and Limitations
This study benefits from a rigorous application of method, conducted according to the Noblit and Hare meta-ethnography approach. The manuscript also adheres to the reporting guidelines by France et al. [Reference France, Cunningham, Ring, Uny, Duncan and Jepson23] and guidance such as [Reference Campbell, Pound, Morgan, Daker-White, Britten and Pill52]. Most notably, service users felt reassured that the way the review captured the initiation of PA (e.g., a slow complex process rife with problems, barriers, and setbacks that is heavily reliant on the support of others) was a “real life” representation [Reference Topor, Borg, Di Girolamo and Davidson53]. This is a particular strength of this study.
The findings should be considered in light of some methodological limitations. Our inclusion of manuscripts written in English language may have missed important research reported in other languages. Similarly, all studies were conducted in western, developed countries with no studies conducted in developing countries. The demographic characteristics (e.g., ethnicity) of participants were reported poorly, in part due to the need to protect confidentiality of participants. This means there has been no exploration of differences in the experience of initiation of PA by demographic variables, which is worthy of further research.
This review included papers with combined results and discussion sections, which makes meta-ethnographic analysis difficult due to a lack of clarity about what is a finding (first-order concept) and what is the primary authors’ interpretation (second-order concept), limiting the ability to make third-order interpretations. Despite this, as far as possible, we distinguished between first and second-order constructs in the data extraction phase and can demonstrate that the papers with mixed results and discussion sections have added value (e.g., Carless [Reference Carless28]; Crone [Reference Crone33]). Crone [Reference Crone33] argued that the integration of findings and discussion allows the development of links between analytic categories and wider issues of theory.
Recommendations for Practice
We make the following recommendations for practice based on the findings from the current review. Extra support and resource allocation may be necessary in the “getting to the activity” phase of the journey, while ensuring that there is no disadvantage toward individuals in terms of cost of participating in the activity or ongoing participation. Financial cost has been a strong theme in previous literature [Reference Stubbs, Vancampfort, Hallgren, Firth, Veronese and Solmi10,Reference Soundy, Kingstone and Coffee11].
Promotion of PA would benefit from taking an individualized approach that is “pitched” appropriately and takes into consideration the person as a whole and the social support networks they have around them.
Providers should be sure that people living with SMI have their preferred level of support throughout the journey, both physically and emotionally, and that facilities are welcoming, nonstigmatizing, and make users feel safe and secure. The people providing support should ideally be known to the individual with SMI, preferably valued, and respected by them.
Flexibility regarding attendance, scheduling, and rate of progression appears central to PA initiation. Priority should also be given to promoting enjoyment, choice, autonomy, and decision making in the very early phases of the PA initiation journey. To allow for this flexibility, traditional measures of success for PA programs may need to be changed. For example, focusing on attendance rates may not be an ideal indicator of success in a program with flexible scheduling and relaxed attendance expectations.
Conclusion
The outcomes and subsequent “journey” presented in this review provide an authentic narrative of the lived experience of the initiation of community-based group PA for people living with SMI. It illustrates that initiation of PA is a complex process rife with challenges. It is not a simple step from intention to participation. The process of initiating PA among people with SMI and the facilitating factors demonstrated here should be fully understood before issues of ongoing participation can be addressed. The literature has demonstrated that alongside the complexity of the journey and the need to take an individualized approach to PA initiation, encouraging people living with SMI into community-based group PA requires high resource, in terms of time, transport, cost, and professional supervision. In particular, intensive social support from a trusted source (health professionals, providers, friends, and family) has an important role in getting people to the activity both physically and emotionally. This review provides recommendations for practice that could inform future PA programs and optimize the uptake of community-based group PA among people living with SMI.
Acknowledgments
We acknowledge the service users who made a valuable contribution to our interpretation of the findings.
Financial Support
The systematic review and meta-ethnography was funded by Sheffield Health and Social Care NHS Foundation Trust (UK). The funding enabled researchers to undertake the review. The funder was involved in determining the scope of the review with respect to which long-term serious mental illnesses are included in the review. The funder approved the proposed qualitative methodology and MH, representing the funder, made a significant contribution to the writing of the manuscript. The lead author (HQ) is currently funded by an NIHR School for Public Health Research (SPHR) post-doctoral Launching Fellowship, hosted at the School of Health and Related Research (ScHARR) at the University of Sheffield.
Conflicts of Interest
M.H. is employed by the funder, Sheffield Health and Social Care NHS Foundation Trust. All other authors declare no conflicts of interest.
Supplementary Materials
To view supplementary material for this article, please visit http://dx.doi.org/10.1192/j.eurpsy.2020.93.









Comments
No Comments have been published for this article.