Vitamin A is an essential nutrient needed for the normal functioning of the visual system, maintenance of cell function for growth, red blood cell production, immunity and reproduction( Reference Sommer and West 1 , Reference Semba 2 ). Globally, in 2013 one-third of children aged 6–59 months had vitamin A deficiency with one of the highest rates (48 %) observed in sub-Saharan Africa (SSA)( 3 ). Furthermore, in the regions of South Asia and SSA, vitamin A deficiency accounted for about 2 % of child deaths( Reference Stevens, Bennett and Hennocq 4 ).
The WHO recommends semi-annual high-dose vitamin A supplementation (VAS) for children aged 6–59 months in countries where vitamin A deficiency is recognised as a public health problem and in countries with under-5 mortality rate above 70 per 1000 live births( 5 ). According to a previous study, vitamin A supplements can improve a child’s chance of survival by 12 to 24 %( Reference Imdad, Herzer and Mayo-Wilson 6 ). Recent food-based approaches, such as food fortification and consumption of foods rich in vitamin A, are ongoing and are essential to ending vitamin A deficiency in the long term. However, until such programmes are sustained at a large scale, delivery of high-dose supplements remains the principal strategy in use for controlling vitamin A deficiency for children aged 6–59 months, despite its inability to maintain normal serum retinol levels( 7 , Reference Mason, Ramirez and Fernandez 8 ). In addition, VAS has been proven to be safe, with a cost:benefit ratio of 17:1 for South Asia, East Asia and SSA, and an equitable way of reaching the most vulnerable children( 7 , Reference Horton, Begin and Grieg 9 ). Ensuring universal VAS coverage (100 %) in SSA or at least effective coverage (≥80 %) needed to improve child survival is important( 10 ) and is also a central component of the child survival agenda in the region. In the literature, some studies have been done with the aim of identifying differentials for uptake of VAS among children aged 6–59 months( Reference Janmohamed, Klemm and Doledec 11 – Reference Thapa 24 ). Identifying these differentials for vitamin A uptake among children aged 6–59 months in SSA will aid international efforts aimed at increasing VAS coverage in SSA. Thus, the present study’s objective was to give an overall view of the pattern of high-dose VAS coverage for the surveys we included as well as examine factors associated with receipt of VAS among children aged 6–59 months.
Methods
Study sample
Out of fifty-four countries in Africa, forty-six are listed as sub-Saharan Africa( 25 ). We used pooled cross-sectional data from the Demographic and Health Surveys (DHS) conducted in twenty-three SSA countries from 2011 to 2015, with the countries selected based on availability of comparative data( 26 ). The pooled DHS data have a hierarchical structure with individuals nested within countries. Our study sample was restricted to children aged 6–59 months and the sample size ranged from 4279 in Namibia to 25 607 in Nigeria (Table 1).
Table 1 The Demographic and Health Surveys conducted from 2011 to 2015 in the sub-Saharan African countries included in the present study

* Unweighted case numbers.
† Individual countries’ sample weight numbers and percentages.
‡ Based on pooled sample weights, derived from women's individual weights and population size of women aged 15–49 years for respective countries.
Vitamin A supplementation
Our outcome variable VAS was defined as receipt of VAS in the last 6 months prior to the survey and was expressed as a dichotomous variable, with category 1 for receipt of VAS and category 0 for non-receipt of VAS. Explanatory variables were chosen based on previous studies and grouped into individual-level and contextual country-level variables. Individual-level variables included the following: mother’s age; mother’s educational status; mother’s occupational status; marital status; place of residence; sex of household head; sex of child; age of child; and media exposure score, which was created from the variables (i) frequency of reading newspapers or magazines, (ii) frequency of listening to the radio and (iii) frequency of watching television. To each of these variables, a score of 0 was given if the response was ‘not at all’, 1 if the response was ‘less than once a week’ and 2 if the response was ‘at least once a week or almost every day’ (five countries additionally measured response for ‘almost every day’). The three variables were later summed up to create the variable ‘media exposure score’. Contextual country-level factors included gross domestic product per capita based on purchasing power parity( 27 ) and proportion of respondents with media exposure score of 0 in the country.
Statistical analysis
The demographic and socio-economic characteristics of respondents are given as unweighted case numbers and percentages, whereas the overall prevalence of VAS among children aged 6–59 months in SSA and receipt of VAS according to demographic and socio-economic characteristics of respondents are reported as weighted percentages based on women’s individual weights and population size of women aged 15–49 years in the respective countries(
28
). Due to the hierarchical structure of the data, for the multivariable analysis we applied a multilevel logistic regression to explore factors associated with VAS among children aged 6–59 months using MLwiN multilevel software(
Reference Charlton, Rasbash and Browne
29
); mother–children pairs made up the first level, while countries made up the second level. Parameter estimates using MLwiN were based on the second-order predictive (or penalized) quasi-likelihood procedure. The proportion of the variance in VAS among children aged 6–59 months due to differences between countries, the intra-country correlation coefficient, was calculated as
![]() $\rho {\equals}{{\sigma _{{\mathop{u}\nolimits} }^{2} } \mathord{\left/ {\vphantom {{\sigma _{{\mathop{\rm u}\nolimits} }^{2} } {\left( {\sigma _{u}^{2} {\plus}\sigma _{{\mathop{\rm e}\nolimits} }^{2} } \right)}}} \right. \kern-\nulldelimiterspace} {\left( {\sigma _{u}^{2} {\plus}\sigma _{{\mathop{e}\nolimits} }^{2} } \right)}},$
where
$\rho {\equals}{{\sigma _{{\mathop{u}\nolimits} }^{2} } \mathord{\left/ {\vphantom {{\sigma _{{\mathop{\rm u}\nolimits} }^{2} } {\left( {\sigma _{u}^{2} {\plus}\sigma _{{\mathop{\rm e}\nolimits} }^{2} } \right)}}} \right. \kern-\nulldelimiterspace} {\left( {\sigma _{u}^{2} {\plus}\sigma _{{\mathop{e}\nolimits} }^{2} } \right)}},$
where
![]() $\sigma _{{\mathop{u}\nolimits} }^{2} $
is the total variance at the country level and
$\sigma _{{\mathop{u}\nolimits} }^{2} $
is the total variance at the country level and
![]() $\sigma _{{\mathop{e}\nolimits} }^{2} $
is the total variance at the individual level. In multilevel logistic regression model, the level 1 residuals, e
ij
, are assumed to follow a standard logistic distribution with a mean of 0 and variance
$\sigma _{{\mathop{e}\nolimits} }^{2} $
is the total variance at the individual level. In multilevel logistic regression model, the level 1 residuals, e
ij
, are assumed to follow a standard logistic distribution with a mean of 0 and variance
![]() $\sigma _{{\mathop{e}\nolimits} }^{2} {\equals}\pi^2/3$
(
Reference Hedeker and Robert
30
). Country-level residuals were used to explore country-level variations in VAS among children aged 6–59 months by constructing simultaneous 95 % CI using caterpillar plots. The width of the interval to achieve a 5 % significance was set at 1·39σ
(
Reference Goldstein and Michael
31
). Countries whose 95 % CI did not overlap were considered significant at the 5 % level. The simultaneous CI were constructed before (Model 0) and after controlling for individual and contextual factors (Model 1).
$\sigma _{{\mathop{e}\nolimits} }^{2} {\equals}\pi^2/3$
(
Reference Hedeker and Robert
30
). Country-level residuals were used to explore country-level variations in VAS among children aged 6–59 months by constructing simultaneous 95 % CI using caterpillar plots. The width of the interval to achieve a 5 % significance was set at 1·39σ
(
Reference Goldstein and Michael
31
). Countries whose 95 % CI did not overlap were considered significant at the 5 % level. The simultaneous CI were constructed before (Model 0) and after controlling for individual and contextual factors (Model 1).
Ethics
The surveys were reviewed and approved by the Ethics Committee of ICF International at Calverton, MD, USA and by the National Ethics Committee of the various countries involved in the study. Permission to use and analyse the data set was obtained by registering the study on the DHS website.
Results
VAS coverage among children aged 6–59 months for the surveys we included was 59·4 % (Table 1). Of mothers, 27·9 % were in the age bracket 25–29 years old and 43·8 % had no formal education. A higher proportion of mothers were working mothers, 65·5 %, and 67·9 % resided in rural areas. Most (45·2 %) mothers had a media exposure score of 1–3 and males headed the majority of households (80·2 %). The majority of mothers were currently in a union/living with a man (88·1 %); male (50·2 %) and female children (49·8 %) were more or less equal; and the majority of children were in the age group 36–47 months (Table 2).
Table 2 Characteristics of children aged 6–59 months who received vitamin A supplementation (VAS), by demographic and socio-economic characteristics, in twenty-three sub-Saharan African countries, 2011–2015, using pooled cross-sectional data from Demographic and Health Surveys

* Unweighted case numbers and percentages.
† Based on pooled sample weights, derived from women’s individual weights and population size of women aged 15–49 years for respective countries.
Descriptive, unadjusted associations with vitamin A supplementation in twenty-three sub-Saharan African countries
VAS coverage was higher among children whose mothers were in the age group 30–34 years (Table 2). However, this varied considerably by country (see online supplementary material, Supplemental Table 1). At 69·3 %, VAS coverage was highest among children whose mothers had secondary or above educational status (Table 2). Coverage increased significantly with higher maternal education in sixteen countries (Supplemental Table 1). Coverage was also significantly higher in fourteen countries among children who had working mothers (Supplemental Table 1). Compared with male-headed households, in seven countries, female-headed households had significantly higher VAS coverage among children aged 6–59 months; on the other hand, in five countries, coverage among children aged 6–59 months was observed to be significantly higher in male-headed households (online supplementary material, Supplemental Table 2). Coverage was significantly higher among children aged 12–23 months in eighteen countries (online supplementary material, Supplemental Table 3). Overall, coverage was observed to be higher among children living in urban areas, children whose mothers had a media exposure score of 4 or above, children whose mothers were never in a union/formerly in a union and among male children (Table 2).
Country variations
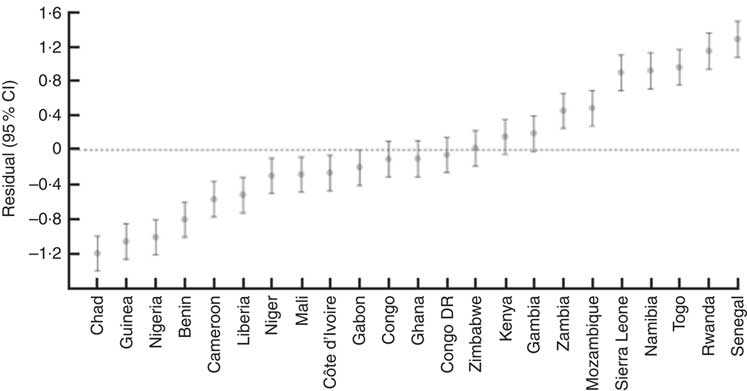
In Model 0 (null model), the intra-country correlation was 12·9 %; however, after taking account of background sociodemographic characteristics (Model 1), approximately 9·9 % of the total unexplained variation in VAS could be attributed to unobserved country-level factors. Figure 1 shows the simultaneous CI of country-level residuals in the null model (Model 0). Senegal had significantly higher likelihood of having received VAS than the remaining countries except Rwanda, Togo, Namibia and Sierra Leone, with which the simultaneous CI overlapped. Figure 2 shows the simultaneous CI of country-level residuals after controlling for contextual country-level factors (Model 1). Sierra Leone had significantly higher likelihood of coverage among children aged 6–59 months than the remaining countries with the exception of Senegal, Togo and Namibia, with which the simultaneous CI overlapped.
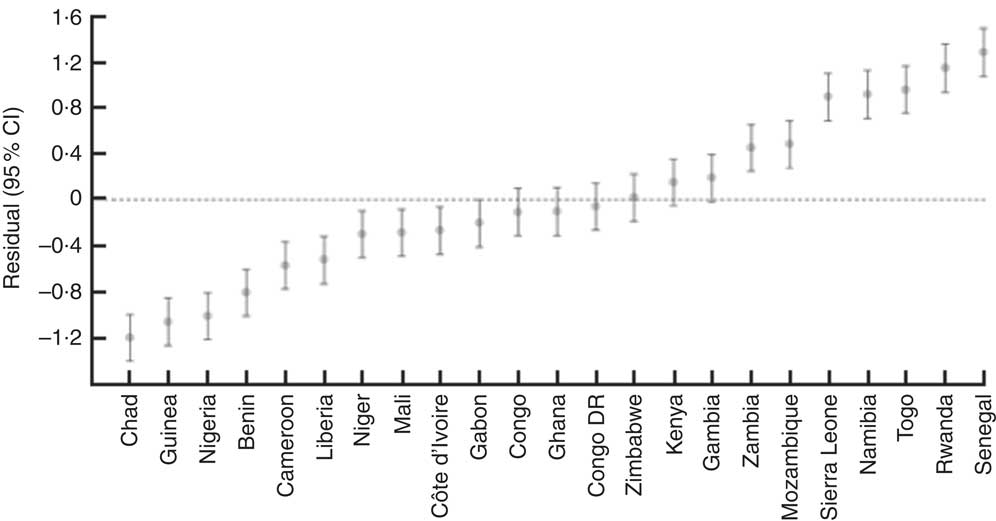
Fig. 1 Simultaneous 95 % CI (vertical bars) for country-level residuals (![]() ) of vitamin A supplementation among children aged 6–59 months (n 215 511) in twenty-three sub-Saharan African countries, 2011–2015, using pooled cross-sectional data from Demographic and Health Surveys: Model 0 (null model)
) of vitamin A supplementation among children aged 6–59 months (n 215 511) in twenty-three sub-Saharan African countries, 2011–2015, using pooled cross-sectional data from Demographic and Health Surveys: Model 0 (null model)
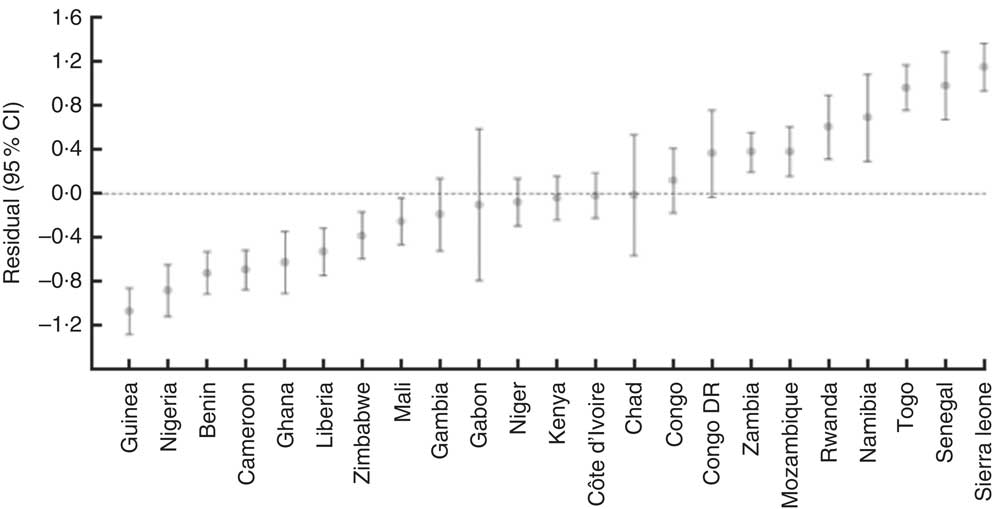
Fig. 2 Simultaneous 95 % CI (vertical bars) for country-level residuals (![]() ) of vitamin A supplementation among children aged 6–59 months (n 215 511) in twenty-three sub-Saharan African countries, 2011–2015, using pooled cross-sectional data from Demographic and Health Surveys: Model 1 (controlling for individual-level and contextual country-level factors)
) of vitamin A supplementation among children aged 6–59 months (n 215 511) in twenty-three sub-Saharan African countries, 2011–2015, using pooled cross-sectional data from Demographic and Health Surveys: Model 1 (controlling for individual-level and contextual country-level factors)
Explanatory factors associated with vitamin A supplementation among children aged 6–59 months
Table 3 shows the adjusted associations between VAS and explanatory variables. Children with older mothers were significantly more likely to receive VAS than children with mothers aged 15–19 years. Children whose mothers had primary education and children whose mothers had secondary or above educational status had higher likelihood of receiving VAS than children whose mothers had no formal education. Children who resided in urban areas were significantly more likely to receive VAS compared with children living in rural areas. Children with working mothers were more likely to receive VAS compared with children who had non-working mothers. Children whose mothers had a media exposure score of 1–3 and of 4 or above had higher likelihood of receiving VAS compared with children whose mothers had a media exposure score of 0. Finally, older children were significantly more likely to receive VAS than those aged 6–11 months. At the country level, lower media exposure score was significantly associated with lower coverage.
Table 3 Multilevel logistic regression analysis for the receipt of vitamin A supplementation among children aged 6–59 months in twenty-three sub-Saharan African countries, 2011–2015, using pooled cross-sectional data from Demographic and Health Surveys

GDP, gross domestic product, PPP, purchasing power parity.
Discussion
Achieving substantial reductions in child mortality means that all children aged 6–59 months living in affected areas need to receive high-dose vitamin A supplements every 4–6 months. UNICEF strives for at least 80 % coverage as a measure of strong and effective VAS programming( 10 ). The overall VAS coverage based on our data was 59·4 %, which is below this recommended minimal coverage level and indicates a need for policy makers and public health practioners in the region to scale up VAS among children aged 6–59 months.
The factors significantly associated with receipt of VAS among children aged 6–59 months were maternal age, maternal education, place of residence, maternal occupational status, media exposure index and age of child. Furthermore, at the country level, media exposure also affected VAS.
We observed that children with older mothers were more likely to receive VAS than children with teenage mothers. This finding is similar to that in a study by Aremu et al., which revealed that children with younger mothers were less likely to receive VAS( Reference Aremu, Lawoko and Dalal 15 ). These results may be explained by the fact that on the mother’s part, nutritional knowledge may increase with age( Reference De Vriendt, Matthys and Verbeke 32 ).
From our study, it is also envident that the mother’s educational status had a role in the reciept of VAS among children aged 6–59 months. Previous studies have also linked higher maternal educational status with receipt of VAS( Reference Choi, Bishai and Hill 17 , Reference Grover, de Pee and Sun 19 , Reference Semba, de Pee and Sun 22 ). A plausible explanation for this finding is that formal education increases health and nutritional awareness vis-à-vis increasing awareness on the benefits of VAS.
Another study also found that rural children were approximately 10 % more likely never to have received a vitamin A supplement compared with their counterparts in urban locales( 7 ). The reasons for the disparity in VAS coverage between the two settings might be attributed to differences in accessabilty to health information and heath services, infrastructures and technological advancements.
In agreement with previously published studies( Reference Haile, Biadgilign and Azage 13 , Reference Aremu, Lawoko and Dalal 15 ), children with working mothers where more likely to receive VAS compared with children with non-working mothers. This might be explained by the fact that working mothers have more access to information about the advantages of VAS and its use from sources such as peers in their workplace, or increased access to community mobilization efforts( Reference Haile, Biadgilign and Azage 13 ).
In line with our study, previous studies have also shown an association between access to media and VAS coverage( Reference Janmohamed, Klemm and Doledec 11 , Reference Bendech, Cusack and Konaté 20 , Reference Ayoya, Bendech and Baker 21 ). Gebremedhin( Reference Gebremedhin 23 ), in twenty-eight SSA countries, also reported that children in the age group 6–11 months had a lower likelihood of VAS. These results warrant further investigation in order to understand the factors leading to the age differential observed in the receipt of VAS.
The intra-country correlation coefficients suggest that 9·9 % of the total unexplained variation in VAS is attributable to unobserved country-level factors. Some other variables unaccounted for in the present study might have had an additional effect. Furthermore, after controlling for all study explanatory variables, Sierra Leone had a significantly higher likelihood of VAS than all but three of the other countries. This finding may be attributed to Sierra Leone having a higher proportion of women in the higher risk subgroup of VAS coverage with respect to background characteristics.
Study limitations and strengths
Coverage estimates from the DHS may be affected by the time interval between survey and mass supplementation and in addition, also subject to recall bias; however, estimates from the DHS can help inform improvements in routine coverage monitoring. It is also worth noting that difference in VAS delivery mechanisms between countries not accounted for in the present study might impact coverage. Future studies looking at VAS delivery mechanisms and coverage in SSA will help in enriching the knowledge on VAS in SSA. Futhermore, the cross-sectional nature of the data makes it possible to establish an association between VAS and explanatory variables but cannot establish causality. Although we controlled for potential confounding variables, there may have been confounding by other factors not included in the study. The main study’s strength lies in the fact that it is based on data that are nationally representative. In addition, information obtained from the study could be used in informing international efforts aimed at increasing VAS in SSA.
Conclusion
The coverage of VAS among children aged 6–59 months based on our data is not optimal and below the recommended minimal coverage level. The study highlighted groups at risk of non-receipt of VAS. Efforts are needed to scale up coverage in this region, mostly focusing on young, low-literate, rural and non-working mothers. It is also important to maximize the utilization of media channels during VAS campaigns.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1368980018004056
Acknowledgements
Acknowledgements: The authors would like to acknowledge Measure DHS for making available the data set for this study and Dr Nicole Claasen for her valuable suggestions and contribution to the manuscript. Funding source: This study received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: None. Authorship: A.S.B., P.B. and I.M.K. planned the study; A.S.B. wrote the manuscript; P.B. and I.M.K. made contributions to the interpretation of results and revised the manuscript; all authors read and approved the final version. Ethics of human subject participation: The Ethics Committee of ICF International at Calverton, MD, USA and the National Ethics Committee of the various countries involved approved the DHS analysed in this study. Measure DHS gave permission to use and analyse the data set.