Electroconvulsive therapy (ECT) has always courted controversy. The mechanism of action remains unknown, which attracts criticism. Currently, the most widely accepted theory is that ECT alters the postsynaptic effects of central nervous system neurotransmitters. 1,Reference Martin2 Despite this lack of understanding, there is a wealth of evidence for ECT’s effectiveness, mainly from studies comparing ECT with simulated ECT and with pharmacotherapy. These studies have found that ECT is effective in treating patients with severe depressive episodes, particularly with psychotic symptoms; Reference Brandon, Cowley and McDonald3-9 there is also evidence for its effectiveness in treating mania, catatonia and schizophrenia. Reference Mukherjee, Sackheim and Schnur10-Reference Tharyan and Adam12 However, not all research in this field supports these findings. For example, a non-systematic review by Read & Bentall concluded that the benefits of ECT are minimal and are outweighed by adverse effects. Reference Read and Bentall13 Variations in study conclusions may be due to methodological differences or biased interpretations. Reference Rose, Fleischmann, Wykes, Leese and Bindman14
ECT in Scotland
In Scotland, use of ECT has been gradually decreasing over recent years. This began in the 1970s; an estimated 60 000 patients received ECT in the UK in 1972 and by 1979 this figure had halved. Reference Fergusson, Hendry and Freeman15 This remained relatively stable over the subsequent years until it took another sharp decline in the mid 1990s. Reference Fergusson, Hendry and Freeman15 The Scottish ECT Accreditation Network (SEAN), an organisation that audits ECT use in Scotland, carried out their first audit for the years 1997-1999 and showed that 1511 patients received ECT over this 2-year period. A subsequent audit was carried out for 2005-2008 and revealed that ECT use had fallen significantly since the previous audit and had continued to fall during the audit period; 511 patients received ECT in 2005 and just 362 in 2008. 16 Another finding of SEAN’s most recent audit (2005-2008) was that the main diagnosis of individuals receiving ECT was a depressive episode, whether single, recurrent or as part of bipolar disorder; only 5% had alternative diagnoses. The principal reason for ECT prescription was resistance to antidepressants, applying to 45% of patients. There were significant discrepancies in use across Scotland; nearly half of patients who received ECT were treated in just 5 of the 20 hospitals which provide it. The Scottish ECT Accreditation Network assessed the effectiveness of ECT as used over this period with the Montgomery-Åsberg Depression Rating Scale (MADRS). A significant response is defined as a reduction in MADRS score by 50% or more; according to this, 74% of patients with capacity and 86% of those without capacity had a significant response. 16
Assessing psychiatrists’ attitudes to ECT
Some of the previous studies looking at psychiatrists’ attitudes to ECT have found them to be relatively positive. Of the American psychiatrists studied by Finch et al, Reference Finch, Sobin, Carmody, DeWitt and Shiwach17 92.3% said they would consider ECT for a friend or family member if it were clinically indicated. Van der Wurff et al Reference van der Wurff, Stek, Hoogendijk and Beekman18 studied the attitudes of Dutch psychiatrists to ECT. As in many other Western European countries, ECT prescription rates in The Netherlands are significantly lower than even the UK, yet the majority of psychiatrists surveyed felt that ECT was effective (92.1%), safe (90%) and acceptable to patients (91.2%). This shows that positive attitudes do not necessarily equate to high prescription rates. Other studies have found attitudes to be less positive; 32% of the Hungarian psychiatrists studied by Gazdag et al Reference Gazdag, Kocsis, Tolna and Lipcsey19 said they would not receive ECT themselves if they had a psychiatric disorder.
Some studies have looked at other reasons for falling ECT prescription rates. In terms of the psychiatrists themselves, year of graduation, Reference Hermann, Ettner, Dorwart, Hoover and Yeung20 knowledge, Reference Papakosta, Zervas, Pehlivanidis, Papadimitriou and Papakostas21 experience Reference Finch, Sobin, Carmody, DeWitt and Shiwach17 and gender Reference Papakosta, Zervas, Pehlivanidis, Papadimitriou and Papakostas21 were found to be significant, along with patient perception and media portrayal. Reference Walter, McDonald, Rey and Rosen22,Reference Dowman, Patel and Rajput23
Knowledge of existing guidelines
The National Institute for Health and Care Excellence (NICE) guidelines on the use of ECT, 1 released in 2003, recommended ‘the use of ECT only in certain restricted circumstances’. They were endorsed by NHS Quality Improvement Scotland, making them applicable to Scotland. The guidelines recommend that ECT only be used to provide a rapid, short-term improvement in those with severe, life-threatening depression in whom other treatments have been unsuccessful. They specifically recommend that it not be used as maintenance therapy for depressive episodes or the treatment of schizophrenia. It was explained that these guidelines were drawn in response to reports from patients who felt that the distress caused by ECT outweighed its clinical benefit. They are, however, purely recommendations and healthcare professionals can practise out with them based on their own clinical judgement. The NICE guidance relating to ECT in depression was updated in 2009. 24 This new guidance stated that ECT should be considered in patients with moderate depression in whom multiple-drug and psychological therapies have been unsuccessful as well as in those with severe, life-threatening depression. As these guidelines were released after the administration of this survey, they will not have affected its results. The impact that the NICE guidelines have had on ECT prescription remains unknown.
This study aims to look for possible causes for the decrease in ECT prescription rates in Scotland, in particular psychiatrists’ attitudes.
Method
In 2009 a self-administered, 19-item survey (available as online supplement DS1) was created to be completed by Scottish psychiatrists. They were asked about demographics, training, familiarity with NICE guidelines and their own attitudes to ECT. Questions about their current practice followed: how many times they had prescribed ECT in the past 2 years and how their prescription has changed over the past 5 years, or since they began prescribing it (whichever was shorter). If their prescription had decreased, they were asked to choose from a list of possible reasons those they felt were attributable. They were given scenarios and asked whether they would prescribe ECT in each of them, followed by questions about ECT prescription in relation to the NICE guidelines. Finally, there was a section designed to assess the psychiatrists’ attitudes to ECT and additional comments regarding ECT were invited. The survey was hosted on the University of Dundee website. The Royal College of Psychiatrists hosted a link to the survey on their website too, with a brief description; as response was poor, the psychiatric postgraduate secretaries for the four largest NHS boards - Greater Glasgow, Lothian, Tayside and Grampian - were requested to send emails to the psychiatrists in their areas with a link to the survey. When results were collated, there was only one respondent from the Lothian area, so it is assumed that the Lothian secretary did not send the email.
Two of the psychiatrists completing the survey did not answer the demographics questions; their questionnaires were not included in the analysis. Not all questions were answered by all psychiatrists therefore analysis reflects the number of responders to each specific question.
An ECT prescription score (EPS) was calculated for each of the scenarios. A score of +1 was given for each scenario the psychiatrists answered ‘yes’ to, a score of 0 for each one they answered ‘maybe’ to and a score of –1 for each one they answered ‘no’ to; the scores for all the scenarios were added together.
Data were statistically analysed using SPSS, PASW Statistics 18.0.1 in Windows. Gender was compared with both the psychiatrists’ estimated prescription rate and their EPS. The Mann-Whitney U-test was applied to determine whether there was a statistically significant difference between gender means of estimated prescription rates. The independent t-test helped determine whether there was a statistically significant difference between gender means of EPS.
Year of graduation and the number of years spent practising psychiatry were both compared with the psychiatrists’ estimated prescription rate and their EPS. Spearman correlations were used to determine the relationship between these variables. A scatter plot of these comparisons was created to look for periodic variation.
The estimated prescription rate and EPS for psychiatrists specialising in old age and those specialising in other areas were compared. Trainee psychiatrists had worked in multiple subspecialties over the past 5 years therefore only consultant data were used for this particular statistical analysis. The Mann-Whitney U-test was carried to determine whether there was a statistically significant difference in mean estimated prescription rate; the independent t-test was used to determine whether there was a statistically significant difference in mean EPS.
Statistical analyses (method and results) for all these factor comparisons are available in online supplement DS2.
Results
Of the psychiatrists who work in Scotland, 91 completed the survey. The majority were male (60%), consultants (61%), and had graduated in the UK (88%). There was relatively equal distribution throughout Greater Glasgow, Tayside and Grampian. The median year of graduation was between 1989 and 1990. The median number of years worked in psychiatry was 16. Respondents worked in various psychiatric subspecialties: general adult, child and adolescent, old age, liaison, learning disability, substance misuse, psychotherapy and rehabilitation. Many worked in multiple subspecialties making further analysis of these data difficult. The majority (89%) had received formal training in ECT administration.
The number of times psychiatrists estimated they had prescribed ECT in the past 2 years is shown in Fig. 1; the mean was twice and 34% had not prescribed it at all.
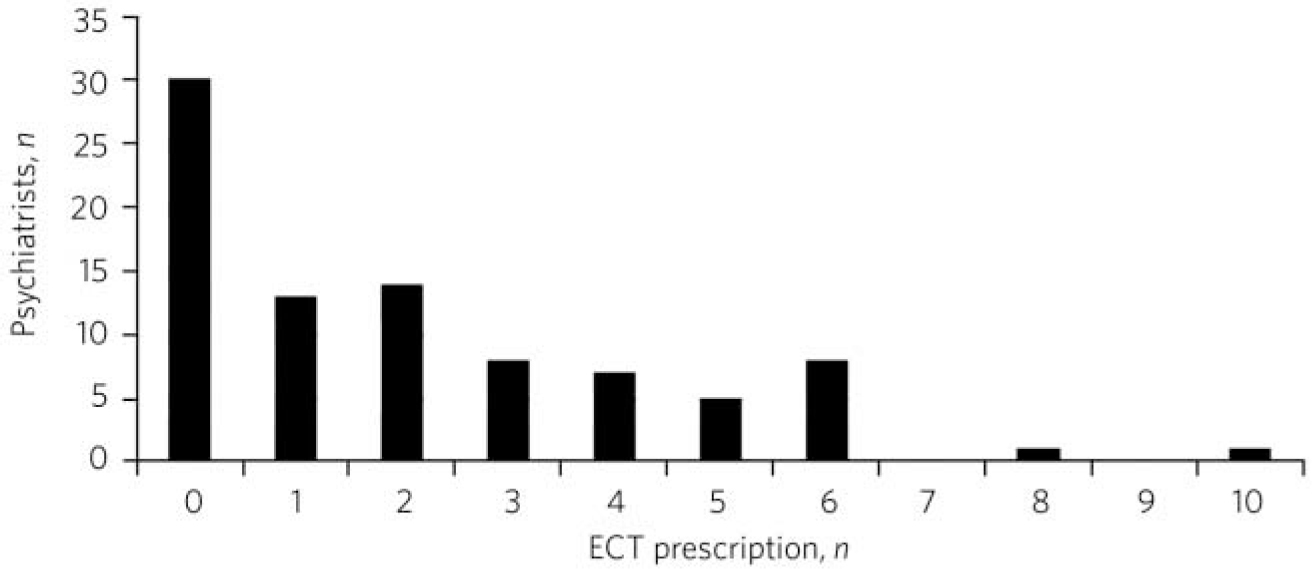
Fig 1 Estimated number of electroconvulsive therapy (ECT) prescriptions over the past 2 years.
The majority of psychiatrists felt that their prescription rates had either remained constant (51%) or decreased (43%) over the past 5 years. The reasons given by those who felt they are now prescribing less are shown in Fig. 2.
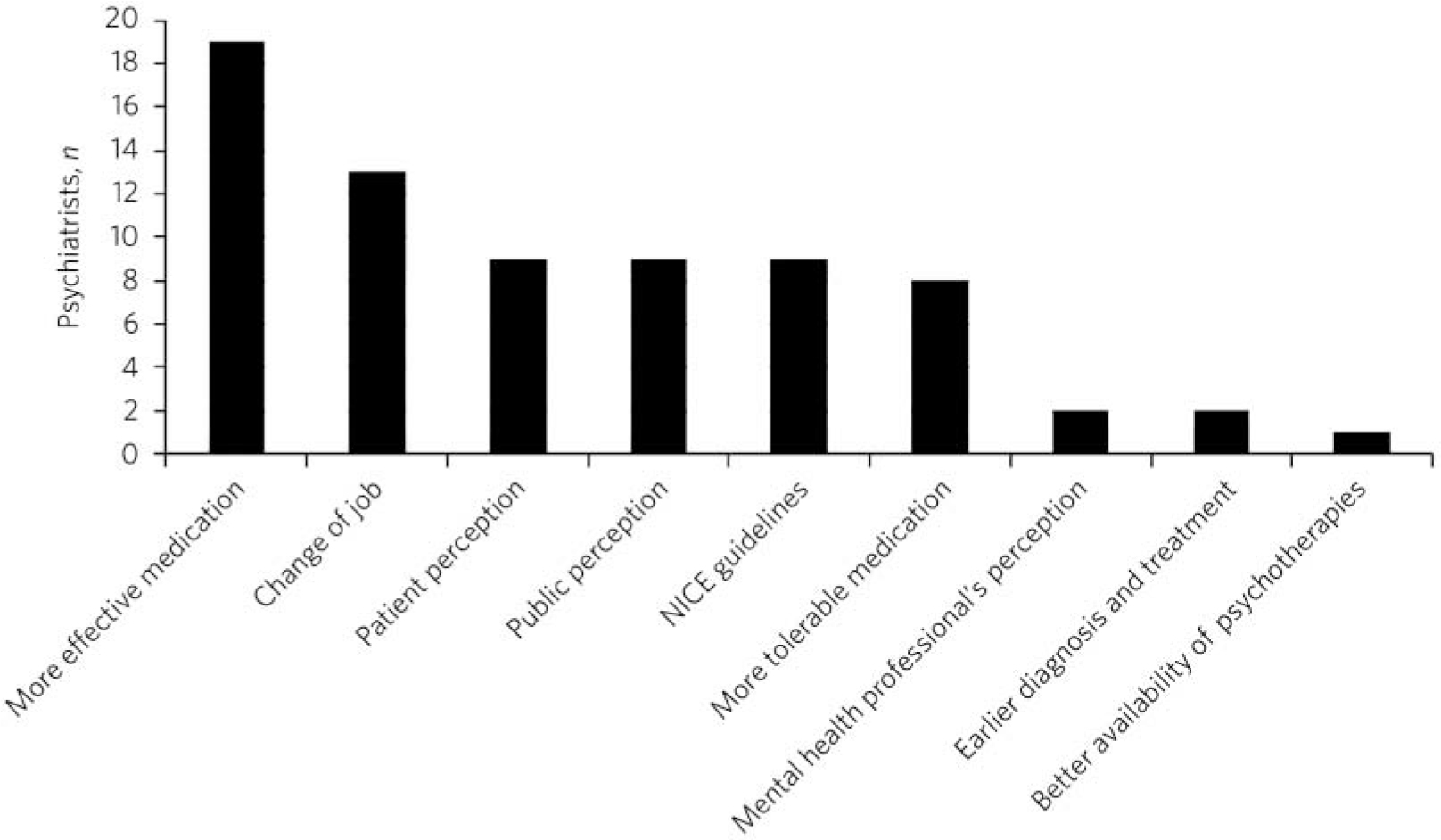
Fig 2 Reasons given by psychiatrists for their decreasing electroconvulsive therapy (ECT) prescription rates. NICE, National Institute for Health and Care Excellence.
The impact of the psychiatrists’ gender on ECT prescription was investigated (Fig. 3). Estimated prescription rates in male doctors were significantly higher than those in female doctors (P = 0.004). Detailed study of the data did not reveal any obvious demographic differences between the genders which could account for this. However, EPS between genders was not found to be significantly different.
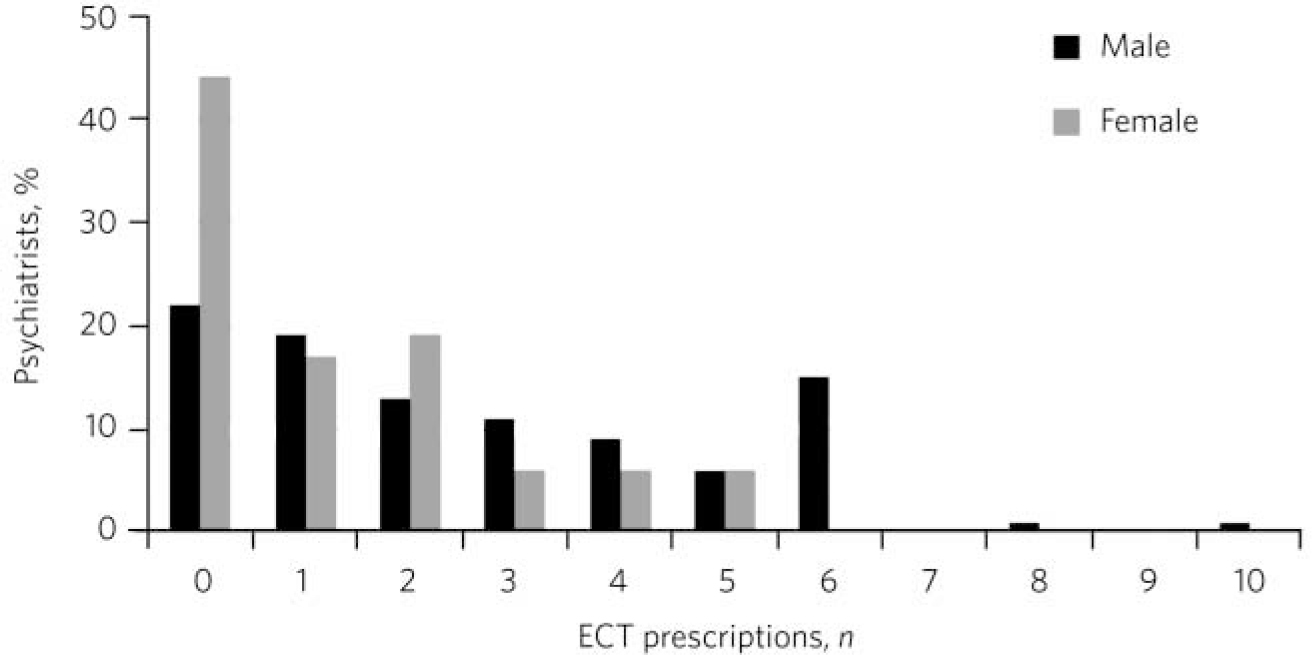
Fig 3 Estimation of electroconvulsive therapy (ECT) prescriptions in the past 2 years based on psychiatrists’ gender.
The impact of years worked in psychiatry and time since graduation was also investigated; neither was found to be significant. The ECT prescription of consultant psychiatrists specialising in old age was compared with that of consultant psychiatrists specialising in other areas; it was not found to be significantly different. The psychiatrists’ responses to whether or not they would prescribe ECT in various scenarios are shown in Table 1.
Table 1 Psychiatrists’ responses to whether or not they would prescribe ECT in various scenarios
| n (%) | |||
|---|---|---|---|
| Yes | Maybe | No | |
| A patient with moderate to severe depression who is refusing food and fluids | 72 (82) | 14 (16) | 2 (2) |
| A patient with moderate to severe depression who is actively suicidal | 39 (44) | 39 (44) | 10 (12) |
| A patient with moderate to severe depression who is not a risk to themselves or others but who is not responding to a range of treatments | 23 (26) | 30 (34) | 35 (40) |
| A patient with moderate to severe depression who previously had a good response to ECT and who wishes to have it again, despite not having tried all other treatment options | 62 (70) | 23 (26) | 3 (4) |
| A patient with schizophrenia who is unresponsive to antipsychotics | 19 (21) | 48 (55) | 21 (24) |
| A patient who you think will benefit from ECT but who is unable to consent and who is actively refusing it | 32 (36) | 48 (55) | 8 (9) |
ECT, electroconvulsive therapy.
With regard to NICE guidelines on ECT awareness, 49% of psychiatrists stated that they were aware of them and the remainder were partially aware or unaware. The psychiatrists’ responses to how they prescribe ECT for depression, schizophrenia, mania and catatonia in relation to the NICE guidelines are shown in Table 2.
Table 2 Psychiatrists’ practices in prescribing ECT for depression, schizophrenia, mania and catatonia in relation to the NICE guidelines
| n (%) | ||||
|---|---|---|---|---|
| Disorder | Practice was consistent with the NICE guidelines prior to their introduction |
Moderated practice in response to the NICE guidelines |
Practice out with the NICE guidelines |
Not familiar with NICE guidelines |
| Depression | 44 (51) | 17 (20) | 12 (14) | 14 (15) |
| Schizophrenia | 46 (53) | 10 (11) | 7 (8) | 24 (28) |
| Mania | 42 (50) | 14 (17) | 5 (6) | 23 (27) |
| Catatonia | 41 (48) | 10 (12) | 5 (6) | 30 (35) |
ECT, electroconvulsive therapy; NICE, National Institute for Health and Care Excellence.
The majority (80%) of psychiatrists said they would be willing to receive ECT themselves if it were clinically indicated. About 46% of psychiatrists thought that ECT has long-term effects on memory, whereas 41% were unsure. The vast majority (97%) thought that ECT has a place in current psychiatric practice. A minority (4%) felt that ECT is overprescribed, whereas 40% thought that it is underprescribed.
Discussion
Psychiatrists’ estimations of the number of times they had prescribed ECT over the past 2 years were generally low, the mean being just twice (Fig. 1), and a significant proportion (43%) felt their prescription rate had decreased over recent years. These findings reflect those of SEAN. 16 The psychiatrists gave various reasons for this fall in ECT prescribing (Fig. 2). The most frequently given was ‘more effective medication’. Psychiatric medications have undoubtedly become more effective over recent years, Reference Goode25 yet there continues to be debate over their effectiveness compared with ECT. Scott Reference Scott26 carried out a meta-analysis of studies comparing the effectiveness of ECT with antidepressant medications using the Hamilton Rating Scale for Depression (HRSD); he found a difference of 5.2 in the HRSD score in favour of ECT. However, these studies had a major omission; none of them included newer-generation antidepressants such as selective serotonin reuptake inhibitors, venlafaxine or mirtazapine.
Some psychiatrists felt that ‘more tolerable medication’ was a significant reason. Psychiatric medications have become more tolerable over recent years, although they continue to have some distressing adverse effects. Reference Goode25 On the other hand, ECT has its own distressing adverse effects, in particular cognitive; the SEAN audit found that 28% of those who received ECT experienced a headache, 19% had memory problems and 17% acute confusion. 16 It is difficult to compare tolerability as it is subjective.
The second most significant factor to which psychiatrists attributed their decrease in use of ECT was to a ‘change of job’. This is considered to be a reason for a decrease in personal prescription rate which should not affect the overall prescription rate.
One psychiatrist stated that, ‘Changes in the practice of ECT are more likely to reflect changing public and political perception than psychiatrists’ views’. Several psychiatrists gave both ‘public’ and ‘patient’ perception of ECT as a reason for their less frequent ECT prescribing. The public views ECT in a generally negative light. Reference Dowman, Patel and Rajput23 One reason for this attitude is its negative portrayal in the media; examples include Return to Oz, The Hudsucker Proxy and One Flew over the Cuckoo’s Nest, in which unmodified ECT is used as punishment. Walter et al Reference Walter, McDonald, Rey and Rosen22 studied the influence of media on the attitudes of British and Australian medical students. They were assessed before and after watching scenes from films portraying ECT in a negative light: a third showed less support for ECT after having watched the films. There are also various anti-ECT movements throughout the world, including the UK, which campaign against ECT. Reference Dowman, Patel and Rajput23
A literature review of patients’ attitudes to ECT carried out by Rose et al Reference Rose, Fleischmann, Wykes, Leese and Bindman14 found there was a significant discrepancy between the benefit perceived by patients and that perceived by healthcare professionals. Many patients felt that adverse cognitive effects outweighed clinical benefits. Reference Rose, Fleischmann, Wykes, Leese and Bindman14 Another review by Dowman et al Reference Dowman, Patel and Rajput23 found multiple studies showing that patients were afraid before undergoing ECT; one particular study found this applied to 60% of patients.
In the present study, 51% of the psychiatrists were only ‘partially aware’ or completely ‘unaware’ of the NICE guidelines on ECT. This will limit the impact of these guidelines on prescription. Despite this, the guidelines were cited by nine psychiatrists as a reason for their decreasing ECT prescription. Although the majority stated that their ECT prescription was consistent with NICE guidelines before their introduction, a significant proportion had adjusted their prescription to be consistent with guidelines for schizophrenia, mania, catatonia and in particular depression. Therefore it appears that the NICE guidelines may have contributed to the decrease in ECT prescription rates.
In this study male psychiatrists’ estimated prescription rates were significantly higher than those of female psychiatrists (Fig. 3), however, there was no significant difference in EPS between genders. Therefore, the impact of gender on ECT prescription remains uncertain and is an area that would benefit from further research. If gender does indeed have an effect, with psychiatry becoming increasingly female dominated, this will have consequences for ECT prescription rates. Reference Ramsay27 Previous studies have found differences in male and female psychiatrist and medical students’ attitudes to and administration of ECT. Hermann et al Reference Hermann, Ettner, Dorwart, Hoover and Yeung20 found that male psychiatrists were significantly more likely to have experience administering ECT than female psychiatrists (P<0.0001). 16 Gazdag et al Reference Gazdag, Kocsis-Ficzere and Tolna28 found that 48.5% of male Hungarian medical students would receive ECT themselves if it were clinically indicated, compared with just 29.4% of female medical students.
When considering whether time of training and years worked in psychiatry had an impact on the participating psychiatrists’ prescription of ECT, neither was found to be significant. Hermann et al Reference Hermann, Ettner, Dorwart, Hoover and Yeung20 found that ECT prescription was significantly higher in those American psychiatrists who have had longer experience practising psychiatry (P<0.006). Some psychiatrists in this study considered this to be relevant, with one stating: ‘I fear that […] younger psychiatrists view [ECT] with a suspicion born out of prejudice’. Studies have also shown that knowledge and experience of ECT lead to more positive attitudes of psychiatrists. Reference Finch, Sobin, Carmody, DeWitt and Shiwach17,Reference Papakosta, Zervas, Pehlivanidis, Papadimitriou and Papakostas21
Regarding treatment outcomes, ECT has been found to be particularly effective in treating depression in elderly patients. Mulsant et al’s meta-analysis of studies looking at the outcome of elderly patients treated with ECT found a significant improvement in 83% and remission in 62% of patients. Reference Mulsant, Rosen and Thornton29 The present study looked at whether the ECT prescription by consultant psychiatrists specialising in old age varied from that by consultant psychiatrists specialising in other areas and the differences were not significant, however, the numbers in each specialty were small.
The psychiatrists were divided over whether or not they would prescribe ECT to the patients in the scenarios presented in the survey. This may reflect a lack of uniformity in ECT prescribing or the complexity of decisions regarding ECT prescription.
The psychiatrists’ attitudes to ECT appeared to be generally positive; 97% stated that ECT has a place in current psychiatric practice. This would seem to suggest that attitudes do not have a significant effect on prescription rates. However, it may also reflect underreporting of psychiatrists’ true attitudes to ECT. With hindsight, the questions assessing attitude were too general and failed to elicit the subtleties of attitude. Some of these differences manifested themselves when the psychiatrists were asked to make additional comments on ECT. These varied from, ‘ECT is the safest, and most effective treatment with the least side-effects in psychiatry’, to ‘ECT has always been a treatment of last resort for me, because of the risk of permanent loss of episodic memories in some patients’. Interestingly, 40% of psychiatrists felt that ECT is underprescribed; this suggests that patients are being denied a valuable treatment because of psychiatrists’ reluctance to prescribe it.
The majority of psychiatrists (87%) answered ‘yes’ or ‘maybe’ to ECT having long-term effects on memory. This generally reflects the evidence. It is accepted that ECT causes short-term anterograde and retrograde amnesia, but the duration of these effects is not fully known. Reference Scott26 Some studies found that ECT has a long-term effect on memory, Reference Squire, Slater and Miller30-Reference Sobin, Sackeim and Prudic33 however, it is difficult to distinguish this from the cognitive impairment that occurs anyway following an episode of mental illness. Reference Brodaty, Berle, Hickie and Mason34 These adverse effects may influence psychiatrists’ prescription.
Overall, it was found that the psychiatrists’ estimated prescription rates of ECT were generally low and had decreased over recent years, despite the vast majority of psychiatrists stating that ECT has a place in current psychiatry. The most frequently given reason for this was more effective medication. Other reasons included more tolerable medication, a change of job, public and patient perceptions and the NICE guidelines. It was found that psychiatrists’ gender may also influence their prescription rates; however, the evidence for this was inconclusive. Attitudes to ECT were found to be generally positive; however, a more in-depth assessment is required to determine their effect on prescription rates.
Acknowledgements
We would like to thank Dr Richard Day, F.M.’s supervisor, for his support and guidance. We thank Alison Gray for putting the survey online, the Royal College of Psychiatrists for hosting a link to the survey on their website and the psychiatric postgraduate secretaries for Greater Glasgow, Tayside and Grampian for emailing psychiatrists regarding the survey.








eLetters
No eLetters have been published for this article.