1. Introduction
Adolescents have an elevated risk for medical complications in pregnancy compared to adult women [Reference Dalby, Hayon and Carlson1]. The rate of neonatal death for adolescent pregnancies, which includes stillbirth as well as infant death up to 28 days old, is roughly 3 times higher than adult pregnancies [Reference Klein2]. Moreover, teenage pregnancy also seems to heighten the risk of psychiatric disorders [Reference Baptista, Baptista and Torres3–Reference Vesga-Lopez, Blanco, Keyes, Olfson, Grant and Hasin5]. In this sense, the primary focus of extant literature is on depression, while anxiety disorders remain somewhat neglected.
Anxiety disorders during pregnancy are relatively common, with reported prevalence rates about 15%, and frequently associated with negative outcomes [Reference Dennis, Falah-Hassani and Shiri6]. Specially, generalized anxiety disorder (GAD) is one of the most prevalent anxiety disorders, only after specific phobia. The disorder is characterized by excessive and persistent anxiety and worry about daily activities. The diagnostic criteria covers physical and psychological symptoms of anxiety, causing significant impairment in social functioning [7]. Furthermore, anxious pregnant women have a higher risk to develop postnatal depressive symptoms [Reference Sutter-Dallay, Giaconne-Marcesche, Glatigny-Dallay and Verdoux8] and other psychiatric disorders after birth [Reference Martini, Knappe, Beesdo-Baum, Lieb and Wittchen9]. Antenatal anxiety disorders are also associated to a higher suicide risk (mainly attributed to generalized anxiety disorder) [Reference Farias, de J Pinto, Teofilo, Vilela, Vaz Jdos and Nardi10] and can bring adverse consequences for the baby [Reference Kingston, Tough and Whitfield11].
While Faisal-Cury, Menezes [Reference Faisal-Cury, Menezes, Araya and Zugaib12] reported that worry and anxiety are among the most common psychiatric symptoms during pregnancy, there are virtually no studies on GAD in pregnant adolescents. A cohort study with pregnant adults showed that 9.5% of them have suffered from this disorder at some point during pregnancy, when the highest rate of GAD was 7% in the first trimester [Reference Buist, Gotman and Yonkers13, Reference Ross and McLean14]. Another study reported an 8.5% prevalence rate in the third trimester of pregnancy [Reference Mitsuhiro, Chalem, Barros, Guinsburg and Laranjeira15]. Environmental factors such as being single and having lower education level [Reference Ma, Xiang, Cai, Lu, Li and Xiang16] may be important for the development of GAD in women [Reference Pigott17]. In addition, women with lower social support, history of child abuse and a past history of GAD in the family have greater risk of developing GAD in pregnancy [Reference Buist, Gotman and Yonkers13]. The perception of parenting styles have also been considered as relevant environmental risk factors for the development of psychiatric disorders, such as anxiety disorders [Reference Heider, Matschinger, Bernert, Alonso, Brugha and Bruffaerts18]. The transition to motherhood can refer to past relationships of parental bonds, especially in teenagers, whose social roles are still to be defined [Reference Coelho, Pinheiro, Silva, de Avila Quevedo, de Mattos Souza and de Matos19]. Although one study has found GAD patients to score both of their parents as uncaring and overprotective, this relationship has not been studied in pregnant adolescents [Reference León and León20].
Therefore, the main goal of this study was to determine if there is an association between the perception of parental bonding and generalized anxiety disorder in pregnant adolescents. Also, we aimed to verify the factors associated with GAD.
2. Materials and methods
2.1. Study type and sampling
This is a cross-sectional study with pregnant teenagers (up to 19 years old) who were using the public services for prenatal care under the Unified National Health System in the urban area of Pelotas, a city in southern Brazil. Data were collected in 47 primary healthcare units and in 3 public obstetric clinics, starting in October 2009 and ending in March 2011. The inclusion criteria were: to be pregnant, up to 19 years old and live in the urban area of Pelotas, RS (Brazil). The exclusion criteria were: present some physical or cognitive disability that did not allow the understanding of the questionnaire.
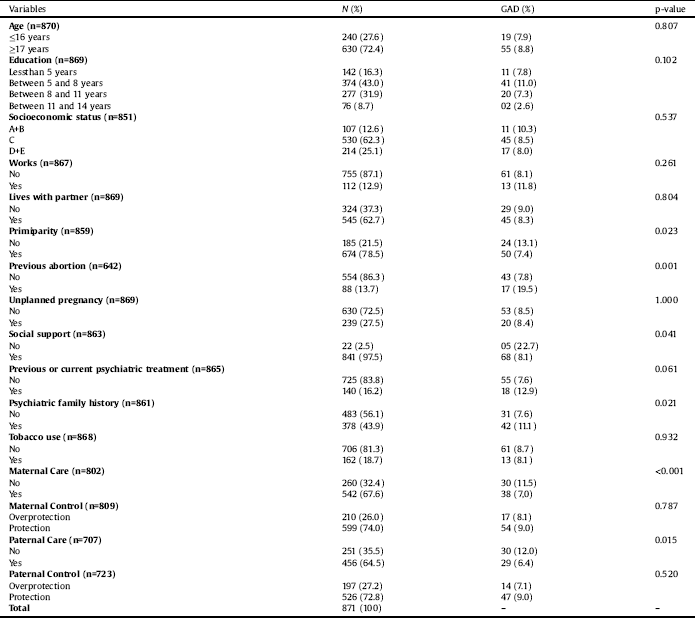
Table 1 Sample distribution according to socio-demographic characteristics, obstetric and behavioral variables and Generalized Anxiety Disorders in pregnant adolescents in the city of Pelotas.
We calculated the sample size with the STATCALC tool of the Epi-Info software [21]. With a confidence level of 95% and power of 80%, the prevalence of GAD estimated at 10% with estimated risk of 2.0, the sample size needed was 871.
2.2. Measures
The GAD was assessed by the Mini International Neuropsychiatric Interview (MINI) [Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs and Weiller22]. The MINI is a short structured interview based on DSM-IV and ICD-10 criteria with adequate validity and reliability [Reference Amorim23].
Parental bonding was assessed by the Brazilian validated version of Parental Bonding Instrument (PBI). This instrument is the most used to measure the contribution of parental behavior in the development of an adequate bond between parents and children [Reference Terra, Hauck, Fillipon, Sanchez, Hirakata and Schestatsky24]. The PBI is a self-report likert-type instrument (0–3) with 25 questions related to the subject’s father and mother. The subjects answer how a particular behavior was similar to their parents’ behavior until they were 16 years old. The instrument measures the following two dimensions of maternal and paternal bonds: [Reference Dalby, Hayon and Carlson1] care or lack of care (affection, warmth, availability, care, sensitivity versus coldness and rejection) and [Reference Klein2] control or protection/overprotection (control, intrusion versus encouragement of the autonomy) (25). It brings questions like “He/She spoke to me with a warm and friendly voice” and “He/She did not help me as much as I needed” for the care dimension and questions like “He/She let me do the things I liked doing” and “He/She liked me to make my own decisions” for the control dimension. The Brazilian version of PBI presented satisfactory internal consistency for both dimensions, with Cronbach's alpha of 0.91 for care in the maternal and paternal bonding and 0.87 and 0.85 for control/protection in the maternal and paternal bonding, respectively [Reference Teodoro, SPdC, Schwartz and Mônego26].
Table 2 Crude and adjusted analysis in a sample of pregnant adolescents with Generalized Anxiety Disorder.

We used a sociodemographic and economic questionnaire considering the following variables: age, education, socioeconomic status, works and living with a partner. The Brazilian Association of Research Companies criteria was used to assess the socioeconomic status of families [27]. This classification is based on the accumulation of material wealth and schooling of household head, classifying the subjects into five levels (A, B, C, D and E) in which the highest-income level is “A” and the lowest is “E”.
We collected obstetric information regarding parity, previous abortions and if the pregnancy was planned. Regarding the psychiatric history, we questioned about previous or current psychiatric treatment and if any family member have psychiatric history. Tobacco use was evaluated as the actual use.
2.3. Statistical analysis
For statistical analysis, we used SPSS (Statistical Package for the Social Science) program, version 13. Chi-square test was used to compare proportions. Logistic regression was employed to control for possible confounding factors.
The variables with p-value <0.20 [Reference Victora, Huttly, Fuchs and Olinto28] entered in the logistic regression analysis with a hierarchical multilevel approach, using the GAD as primary outcome. In the first level, sociodemographic and economic variables were included (age; educational years; socioeconomic status; work; lives with partner). In the second level, obstetric variables were included (primiparity; previous abortion; unplanned pregnancy). In the third level, emotional and behavioral variables (social support; previous or current psychiatric treatment; psychiatric family history; tobacco use; perception of maternal care; perception of maternal control; perception of paternal care; perception of paternal control).
2.4. Ethical aspects
The subjects signed a free and informed consent statement for the analysis and anonymous publication of the research findings. This project was approved by the Research Ethics Committee of the University, Brazil (protocol no. 2007/95).
3. Results
In this study, 870 pregnant adolescents were identified excluding 4.3% of losses and refusals. The prevalence of GAD was 8.5%. Regarding PBI maternal bonding styles, the prevalence of lack of care was 32.4% (n = 260) and overprotected control was 26% (n = 210). Regarding PBI paternal bonding styles, the prevalence rates were of 72.8% (n = 526) and 27.2% (n = 197), respectively.
Table 1 shows the sample´s overall distribution. The raw analysis showed that GAD was associated with primiparity (p = 0.023), previous abortion (p = 0.001), perception of family support (p = 0.041), familial history of psychiatric disorders (p = 0.021), maternal lack of care (p < 0.001) and paternal lack of care (p = 0.015).
After adjusting for possible confounding variables, as showed in Table 2, previous abortion (p = 0.018), familial history of psychiatric disorders (p = 0.019) and maternal lack of care (p = 0.036) was associated whit GAD. Pregnant women who had previous abortion were 3.71 (CI: 1.26; 10.95) times more likely to present GAD compared to those who had no previous abortion. For the pregnant who had familial history of psychiatric disorders, the chance of presenting GAD was 2.27 (CI: 1.14; 4.53) times higher than those who did not had familial history of psychiatric disorders. Pregnant teenagers who reported maternal lack of care were 2.08 (CI: 1.05; 4.12) times more likely to present GAD compared to those who reported adequate maternal care. In the adjusted analysis, the following variables were not significantly associated with GAD: education, primiparity, social support, previous or current psychiatric treatment and paternal care (p > 005).”
4. Discussion
Parental bonding encompasses the bonding style that both parents have with their children through attitudes related to care and protection. The ‘care’ dimension is composed by attitudes of affection, emotional warmth, availability, care and sensitivity. Thus, parents who demonstrate coldness and rejection characterize lack of care. The ‘protection’ dimension, on the other hand, is composed by attitudes of surveillance and promotion of autonomy. Parents who demonstrate extreme control and intrusion characterize overprotection [Reference Teodoro, SPdC, Schwartz and Mônego26]. The literature has shown that parental bonding styles plays an important role in the developing of psychiatric symptoms in adulthood [Reference Lima, Mello and Mari29].
For the main purpose of this study, we expected to find an association between generalized anxiety disorder and both maternal and paternal bonding. This relationship was partially found. Only the lack of maternal care in childhood was significantly associated to GAD in pregnancy, after adjusting for potential confounders. The association between parenting style and anxiety disorders was examined in a few studies. A study conducted in six countries found an association between lack of maternal care and the presence of GAD, social phobia, specific phobia and panic disorder. They also found an association between lack of paternal care and anxiety disorders, although this dimension of parental bonding acted differently across the anxiety disorders. Yet, maternal overprotection was not associated with GAD but with the other three disorders [Reference Heider, Matschinger, Bernert, Alonso, Brugha and Bruffaerts18]. The authors Lima, Mello [Reference Lima, Mello and Mari29] claim that parental dysfunction are risk factors for the development of anxiety disorders. However, we are not aware of other studies investigating this association within a population of pregnant teenagers.
According to Rubinchik, Kablinger [Reference Rubinchik, Kablinger and Gardner30] “pregnancy can bring to mind past painful events with their own parents” (p.100). It is possible that those GAD pregnant teenagers who perceived their parental bonding as unsatisfactory could be interpreting the memories regarding their parents in an anxious or pessimistic way, notwithstanding the actual childhood experience. Another possible explanation for the association of maternal bonding and GAD is that the way in which the child is raised could be considered a potential factor of vulnerability, whereas the first abstractions of the child's experience with their caregivers become mental representations of attachment relationships that reflect the way how the individual handles emotions [Reference Main, Kaplan and Cassidy31]. The internalization of this perceived lack of affection in childhood can give adolescents less ability to cope with life's stressful events [Reference Hauck, Schestatsky, Terra, Knijnik, Sanchez and Ceitlin25]. Although such relationship is evident, this information should be investigated more carefully, as depression can also interfere in this association [Reference Fentz, Arendt, O’Toole, Rosenberg and Hougaard32].
Another factor associated with GAD in pregnant teenagers was the presence of a previous abortion. A meta-analysis identified that women who underwent abortion had 81% risk of mental health problems, and that nearly 10% incidence of mental health problems are directly attributed to abortion [Reference Coleman33]. Women who have experienced an abortion in previous pregnancies can have greater fear to go through this situation again. Extreme concerns about the current pregnancy may also arise. Thus, it is necessary to have a special attention to these pregnant women. The prenatal care should integrate mental health actions to prevent or treat anxiety disorders.
As we expected, the pregnant that had familial history of psychiatric disorders had a higher chance of present GAD than those who did not had history of psychiatric disorders in family members. A review of risk factors for the onset of panic and generalized anxiety disorders found that a parental history of GAD [Reference Beesdo, Pine, Lieb and Wittchen34], depression [Reference Lieb, Isensee, Hofler, Pfister and Wittchen35], or other mental health problems [Reference Kessler and Wang36] were associated with GAD in their offspring. Furthermore, studies on psychiatric disorders in family members point out this issue as a risk factor for most psychiatric disorders. Regarding GAD, one third of the risk of presenting this disorder is of genetic origin [7]. Moreover, by witnessing the anxious and worried behavior of the parents, the child learns this behavioral pattern and begins to actually practice it, resulting in increased vulnerability to develop the disorder. The case revolves around the biological and environmental influences that interfere with the normal development of the individual, making it more susceptible to develop some mental disorder. Although the magnitude of the association between GAD and psychiatric family history is greater than the association with parental bonding, the latter one cannot be excluded, since even after adjusted analysis it remained significant.
The findings of our study should be interpreted in the light of its limitations. First, as with any cross-sectional study, causality could not be assessed. As parental bonding was measured retrospectively, we point out the risk of recall bias. Similarly, the pregnant with GAD can have assessed their parental bonding as negative as a result of their disorder and not because it was really negative [7]. A longitudinal study would be necessary to evaluate such relationship. On the other hand, previous research showed that the subject´s mood did not have a significant impact on PBI, which proved stable over time [Reference Murphy, Wickramaratne and Weissman37]. Another limitation concerns the lack of a control group of non-pregnant adolescents, but the comparison was not possible due to the logistics of the study. As our sample was recruited from public health services, there is the risk of selection bias. It was also not possible to collect information about other possible confounding factors drug use and family structure.
Even with such limitations, this study has relevance, considering that in Brazil about 20% of children were born from adolescent mothers each year, which confirms an increased need to supply this population with adequate healthcare [Reference Mitsuhiro, Chalem, Barros, Guinsburg and Laranjeira15]. Moreover, recent data showed that GAD has received little attention compared to other anxiety disorders, which demonstrates the importance of further studies related to the subject. Some studies suggest that environmental factors are involved in the development and maintenance of GAD, however, there is very few information in the literature.
Concluding, a perceived lack of maternal care under 19 years was associated with GAD, suggesting that the adequate maternal bond is a contributor for a psychological healthy development. The lack of care, as well as the absence of an adequate family structure during childhood may lead the individual to be more susceptible to the onset of psychiatric disorders.
Anxiety disorders in pregnancy may have a harmful impact on the health of pregnant teenagers, as it can lead to postpartum depression, low birth weight and premature birth, and, additionally, it may also have a negative impact on child development. This indicates the relevant need of early detection of these conditions, aiming to implement appropriate preventive measures [Reference Ma, Xiang, Cai, Lu, Li and Xiang16, Reference Rubinchik, Kablinger and Gardner30].
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The subjects signed a free and informed consent statement for the analysis and anonymous publication of the research findings. This project was approved by the Research Ethics Committee of the Catholic University of Pelotas, Brazil (protocol no. 2007/95).
Funding
This study was funded by Conselho Nacional de DesenvolvimentoCientífico e Tecnológico (CNPq).
Declaration of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.





Comments
No Comments have been published for this article.