The dietary approaches of veganism (VGN) and the ketogenic diet (KD) have become increasingly popular in recent years and were among the top five searched diets on Google between 2009 and 2014(Reference Kamiński, Skonieczna-Żydecka and Nowak1). Due to VGN and KD eliminating whole food groups, it is plausible that they may be devoid of key nutrients without careful planning. Given their rising popularity, the food industry has responded with a variety of specialty products, many of which are considered ultra-processed, marketed specifically at those adhering to KD and VGN. The impact on nutrient intake, when relying primarily on ultra-processed foods (UPF), for long-term adopters of these diets is unknown and warrants further investigation.
The recent publication of the EAT-Lancet diet has propelled the consumption of ‘plant-based’ into mainstream media(Reference Willett, Rockström and Loken2). Concerns have been raised about this diet’s cost and relative affordability, particularly in middle- and low-income countries(Reference Zagmutt, Pouzou and Costard3,Reference Hirvonen, Bai and Headey4) . While a universal definition for VGN has not been established, it is well known as a diet that excludes all animal products and by-products including meat, fish, dairy and honey in favour of eating predominantly fruits, vegetables, wholegrains, cereals, legumes, nuts and seeds(Reference Melina, Craig and Levin5). Studies suggest several health benefits are associated with vegan diets including a lower incidence of non-communicable diseases such as colon cancer, type 2 diabetes mellitus, obesity and non-alcoholic fatty liver disease(Reference Bakaloudi, Halloran and Rippin6). There is evidence indicating that, in the absence of supplementation and fortified foods, vegan diets are devoid of key nutrients including Ca, vitamin D, vitamin B12 and Fe(Reference Melina, Craig and Levin5,Reference Bakaloudi, Halloran and Rippin6) . The combined insufficient intake of Ca and vitamin D could result in an increased risk for poor long-term bone health. Some evidence exists (albeit limited) to suggest that vegan diets do not contain sufficient essential fatty acids and specific recommended daily intakes may be required(Reference Burns-Whitmore, Froyen and Heskey7). Concerns related to the application of the vegan diet in specific populations, including pregnant women and growing children, have been noted. A recent prospective observational study of vegan women indicated that they experienced a greater risk for small-for-gestational-age newborns and lower birth weight compared with children of omnivorous mothers(Reference Avnon, Paz Dubinsky and Lavie8). Moreover, even when consuming a well-planned nutritionist-designed diet, low levels of serum vitamin A, DHA and vitamin D have been reported in a cohort of Finnish children, which could be of concern for long-term visual health(Reference Hovinen, Korkalo and Freese9). These concerns are exacerbated by the explosion of processed meat and dairy analogues, which are often composed predominantly of soya and refined carbohydrates, and the growing availability of vegan convenience food, suggesting that such diets are not synonymous with health(Reference Boukid10–Reference Wickramasinghe, Breda and Berdzuli14).
The KD limits carbohydrate intake (≤50 g/d) while increasing fat intake (≥75 % total energy (TE)) with protein intake comparable to mainstream dietary patterns (15–20 % TE)(Reference Volek, Phinney and Krauss15). The purpose of the KD is to establish a state of nutritional ketosis where circulating ketone bodies, predominantly β-hydroxybutyrate, are the main source of fuel rather than glucose(Reference Volek, Phinney and Krauss15). Restricting carbohydrates below 50 g/d allows for the production of between 100 and 150 g of ketone bodies daily(Reference Volek, Phinney and Krauss15). Although the KD is rooted in therapeutic clinical practice and has been used safely and effectively for the past 100 years in the treatment of intractable epilepsy and diabetes, it is becoming a popular dietary approach adopted by many to lose weight and improve health(Reference Athinarayanan, Adams and Hallberg16–Reference Ludwig18). Aside from its long withstanding clinical application, the KD has been associated with favourable metabolic health outcomes in both the short and long term and recently recognised as a safe and effective treatment strategy for type 2 diabetes mellitus(Reference Volek, Phinney and Krauss15). These favourable outcomes are believed to be a result of the reduction of glycation, oxidative stress and inflammation. Further research is required to ascertain the applicability of KD for the treatment of several cancers, neurodegenerative and neuro-depressive diseases but the research to date is promising(Reference Ludwig18). There is limited evidence regarding the long-term adherence to a KD, an area that requires further investigation to understand the benefits and limitations of this approach for otherwise healthy individuals. Given its rising prevalence among the general population, close attention should be paid to the long-term effects on individuals living freely, especially within the context of the modern food environment where individuals have access to a wide variety of hyperpalatable UPF formulations marketed as being ‘low carbohydrate’ in an effort to ride the metaphorical health wave associated with lower carbohydrate diets. Understanding the effects of KD UPF on long-term health should be a public health priority.
There are concerns among academics and clinicians that a KD contains excessive saturated fat, insufficient fibre and is devoid of key micronutrients(Reference Volek, Phinney and Krauss15). While the debate regarding the 10 % TE threshold for saturated fat is ongoing, recent advances suggest that increased dietary fat intake may not be as detrimental as previously thought(Reference Astrup, Teicholz and Magkos19). The contention is underpinned by the saturated fat paradox of tribes, including the Maasai, Inuit and Native Americans who subsist almost exclusively on saturated fat for periods with no adverse cardiovascular outcomes(Reference Volek, Phinney and Krauss15). Meanwhile, the supposition that carbohydrate-restricted diets are devoid of fibre and key micronutrients remains contentious with mixed outcomes reported among research to date(Reference Bracci, Keogh and Milte20–Reference Zinn, Rush and Johnson22). Further studies are required to confirm whether long-term KD adherence negatively affects micronutrient intake and subsequent serum levels in healthy individuals. It is evident that there are potential shortcomings associated with both diets but when applied appropriately can result in improvements to health and prevention of chronic disease.
Significant resources are attributed to discovering ‘the best’ dietary pattern for longevity and health; however, it appears that studies illustrating positive outcomes have one key metric in common, a reduction in nutrient-poor UPF and a subsequent increase in whole and minimally processed foods. To date, research suggests that moving towards such healthier eating patterns (regardless of the chosen trend) is associated with a higher cost than current eating habits(Reference Jones, Tong and Monsivais23–Reference Verly-Jr, de Carvalho and Marchioni26). This is believed to largely be attributed to a reduction in the consumption of processed and UPF, which are mass produced food formulations that are cheaper than real, whole foods(Reference Vandevijvere, Pedroni and De Ridder27). While the cost of whole foods fluctuates seasonally, processed and UPF costs remain relatively stable across the year. To date, studies predominantly investigate the cost and impact of mainstream UPF, which are known to negatively impact health(Reference Chen, Zhang and Yang28,Reference Monteiro, Cannon and Lawrence29) . Despite the increasing availability of specialty products for restrictive dietary patterns, little is known about the impact their inclusion has on diet cost, nutrient status and long-term health(Reference Tso and Forde13,Reference Wickramasinghe, Breda and Berdzuli14,Reference Obrero30) . With an increasing awareness that the level of food processing affects health and limited understanding of the impact of processed specialty foods on health, it can be argued that this once niche area of nutrition requires further examination(Reference Marti31). The purpose of this case study was to assess the nutrient profile and cost of VGN and KD under two conditions, exclusion of all UPF specialty products and inclusion of UPF predominantly specialty products, to understand the effect these products have on the nutrient status and cost of these dietary patterns.
Methods
In this descriptive case study, four single-day hypothetical meal plans were formulated and costed for a young adult female not currently pregnant or lactating. A young adult female was chosen for this case study as women are commonly reported to be more health-conscious, therefore potentially more likely to engage in exclusionary-type diets like VGN and KD(Reference Grzymisławska, Puch and Zawada32). Demographic (height and weight) data were based on nutrient reference values threshold profiles available on the Australian National Health and Medical Research Council and New Zealand Ministry of Health (NHMRC and MOH) website(33). These profiles illustrate the estimated energy requirements for individuals within given age, height and weight-bound categories. For the purposes of this case study the 19–30-year-old age category was selected alongside a height of 1·7 m and weight of 63·6 kg, this is a common time for women to begin experimenting with diets and the chosen weight and height resulted in a healthy BMI. TE expenditure was calculated using the Schofield equation, inputting the demographic data and an activity level of 1·6 (lightly active)(Reference Schofield34). TE for the four hypothetical meal plans was intended to be isocaloric to maintain current weight and set in accordance with the calculated energy needs of the hypothetical subject (±10 %). Table 1 presents the demographic data used for this case study. The vegan and KD were chosen for examination due to their rising popularity(Reference Kamiński, Skonieczna-Żydecka and Nowak1).
Table 1 Case study demographics

PAL, physical activity level; EER, estimated energy requirement.
Two meal plans were created for VGN and KD, respectively. The following meal plans were created: whole food vegan (WFV), whole food ketogenic (WFKD), specialty vegan (SV) and specialty ketogenic (SKD). The formulation was based on popular vegan and KD meals with all recipes included in the sample diets available freely online. The vegan meal plans excluded all animal products and by-products and were formulated in accordance with the acceptable macronutrient distribution ranges (AMDR) for carbohydrates (45–65 %), protein (15–25 %) and fat (20–35 %), as per the Australian NHMRC and New Zealand MOH dietary guidelines(33). While geographically specific, these guidelines closely mirror those of the UK and USA. Comparatively, the ketogenic meal plans were formulated in accordance with ketogenic guidelines for macronutrient distribution: ≤50 g carbohydrate, 15–20 % protein and ≥75 % fat(Reference Volek, Phinney and Krauss15,Reference Kenig, Petelin and Poklar Vatovec21) . When creating the whole food-based diets, predominantly foods that are unprocessed or minimally processed were selected for inclusion, while UPF were excluded where practicable. For the vegan diet, a variety of fruits, vegetables, wholegrains, nuts, seeds and legumes were included, while for the KD low-carbohydrate, high-fat foods were included with a careful selection of foods that were anti-inflammatory and reduced oxidative stress(Reference Zinn, Rush and Johnson22). Examples of these foods include salmon, broccoli, berries, leafy greens, olive oil and coconut oil. When creating the specialty-based UPF meal plans, whole foods were minimised with the majority of foods selected being processed or UPF speciality marketed towards vegans and KD adopters. In both instances, foods that were convenient, acceptable and palatable were included with fresh, frozen and canned alternatives incorporated, while less commonly consumed options (like mussels and organ meats), dietary supplements such as MCT, nutritional yeast, protein powders and dietary supplement capsules or tablets were intentionally excluded. While ‘speciality products’ were those identified as being marketed specifically to a certain diet group (e.g. the packaging stated ‘vegan’ or ‘keto’), ‘ultra-processed products’ were defined in accordance with the NOVA food categorisation system. UPF are industrially processed foods that contain multiple ingredients, including additives and flavourings to create a highly palatable product with a long shelf life. Typical mainstream examples of UPF include sugary drinks, packaged snacks, frozen dinners and fast foods. Nutrition information for the specialty products was gathered from Countdown (a local New Zealand supermarket) online shopping website. Meal plans were analysed using FoodWorks Professional V.10 (Xyris software), which uses an Australian and New Zealand food database, a commonly used nutrient analysis software(Reference Bracci, Keogh and Milte20,Reference Zinn, Rush and Johnson22,Reference Zinn, North and Donovan35) .
The cost for each meal plan was calculated by the price per weight of food consumed(Reference Zinn, North and Donovan35). Items on special and home brands were not included; instead, popular brands were chosen. Free-range and grass-fed products were selected over traditionally farmed alternatives where possible. Cost data were gathered using Countdown (a local New Zealand supermarket) online shopping website.
Results
The vegan and KD meal plans and corresponding nutrient analyses are presented in Tables 2 and 3, respectively. All four meal plans met energy requirements. The WFV, WFKD and SKD meal plans met respective dietary macronutrient guidelines while the SV diet contained insufficient carbohydrate in accordance with the AMDR (41·7 %) and insufficient protein in accordance with the AMDR (11·6 %) but sufficient protein when using the g/kg/body weight recommended daily intake threshold (1 g/kg/body weight).
Table 2 Vegan and ketogenic sample meal plans
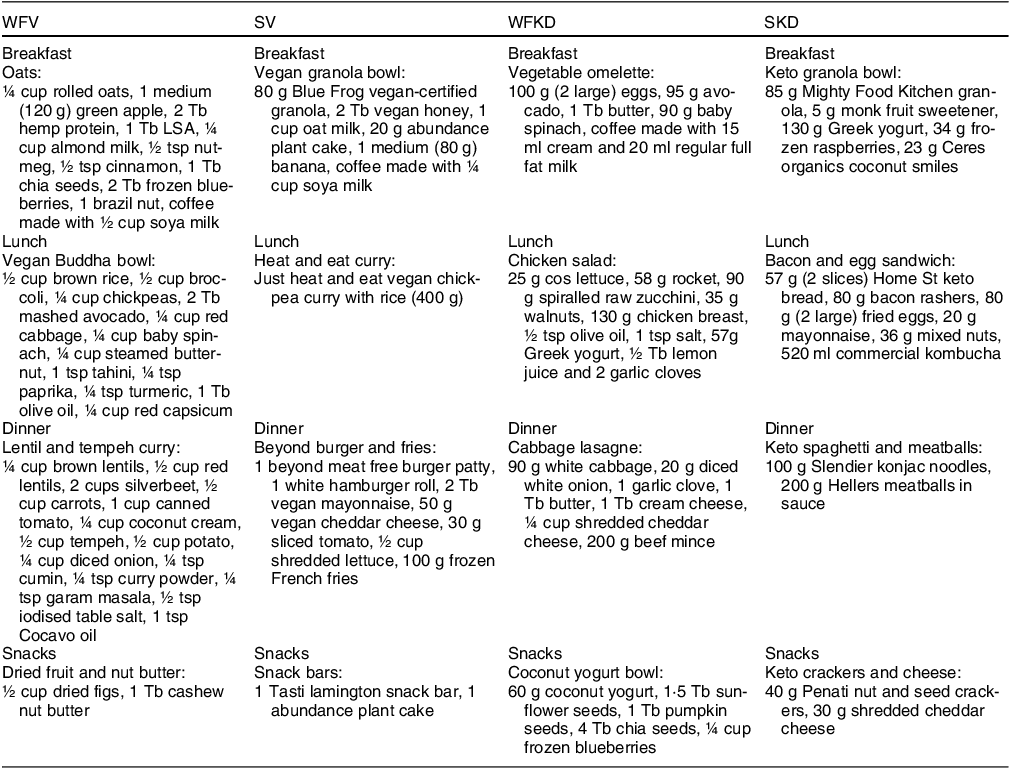
T, tablespoon; tsp, teaspoon.
Table 3 Nutrient analysis of vegan and ketogenic meal plans

NRV, nutrient reference value; RDI, recommended daily intake.
* WHO recommendation for trans fat.
† AI were used as RDI were unavailable.
‡ Mainstream AMDR used as guidelines for vegan sample diets and ketogenic specific guidelines used for ketogenic sample diets.
The WFKD met all micronutrient thresholds while the SKD did not meet several micronutrient thresholds (thiamine, niacin, vitamin C, vitamin A, folate, Ca, Fe and Mg). The WFV diet met all but one micronutrient threshold (vitamin B12), while the SV diet failed to meet any of the micronutrient thresholds. Fibre content was sufficient, meeting adequate intakes across all sample meal plans. The WFV meal plan contained more sugar than the SV meal plan (16·9 % and 9·1 %, respectively) while the WFKD meal plan contained less sugar than the SKD meal plan (2·7 % and 4·7 %). The WFV meal plan contained less saturated fat than the SV meal plan (8·1 % and 17 %, respectively) while the WFKD meal plan contained more saturated fat than the SKD meal plan (28·4 % and 24·4 %, respectively). Na intake surpassed the suggested dietary intake in three of the four meal plans (SV, WFKD and SKD).
Cost comparison for the four 1-d meal plans is presented in Fig. 1. Cost differential was most pronounced between the WFV ($17·04) and SV diets ($32·19). The WFKD ($22·24) and SKD ($24·07) diet costs were similar.

Fig. 1 Cost analysis of vegan and ketogenic meals plans
Discussion
The results of this case study illustrate that, regardless of dietary approach, micronutrient status and cost are negatively impacted by the inclusion and reliance on UPF specialty products. The whole food-based meal plans had a more favourable nutrient profile and cost less for both vegan and KD. The vegan meal plans contained the highest quantity of sugar (likely the result of greater carbohydrate content), beyond the WHO 5 % TE recommendation. In accordance with previous findings, a well-formulated whole food-based vegan diet met all requirements, except vitamin B12 (Reference Bakaloudi, Halloran and Rippin6). This is expected given the absence of animal foods, which are rich in vitamin B12. Comparatively, the SV meal plan contained the lowest total calories, insufficient protein (in accordance with AMDR) and inadequate levels of all key micronutrients. Concerns related to protein content and micronutrient status of vegan diets have previously been raised. When nutrient-dense foods such as meat and animal by-products are excluded from the diet, a larger total volume of food may need to be consumed to meet nutrient requirements, which may pose a challenge due to the satiating properties of high-fibre plant foods(Reference Clarys, Deliens and Huybrechts36). Moreover, when there are fewer calories available, it becomes challenging to meet requirements based on larger total calorie intakes. The WFKD meal plan met all requirements, a finding similar to that of a randomised control trial of obese adults on a KD and a recent case study analysis of low-carbohydrate diets(Reference Kenig, Petelin and Poklar Vatovec21,Reference Zinn, Rush and Johnson22) . Three of the four meal plans in the present case study exceeded the suggested daily threshold for Na (2000 mg).
There are differences between the two dietary patterns that warrant further discussion. Given the contention surrounding fibre, protein, saturated fat, micronutrients and their bioavailability and cost, these topics will be explored in further detail.
Fibre
Fibre consumption, which is known to support vascular and gut health, has been associated with a lower incidence of CVD. Population-based studies commonly report low intake of fibre, usually attributed to inadequate fruit and vegetable consumption(Reference Melina, Craig and Levin5). This case study showed that fibre requirements can be achieved with vegan and KD. The WFV meal plan contained more fibre than the SV meal plan (80 g and 27·5 g, respectively). This finding is in accordance with previous literature that illustrates vegans typically surpass fibre recommendations(Reference Melina, Craig and Levin5,Reference Bakaloudi, Halloran and Rippin6,Reference Elorinne, Alfthan and Erlund38,Reference Weikert, Trefflich and Menzel39) . The higher intake of fibre in the WFV meal plan is due to the variety of plant foods included in comparison with the UPF speciality products in the SV meal plan. While fibre has been highlighted as a potential concern with the KD, both the current case study and previous findings suggest that ample fibre intake can be achieved through the inclusion of a variety of nuts, seeds and vegetables(Reference Volek, Phinney and Krauss15,Reference Zinn, Rush and Johnson22) . The WFKD contained 41·1 g of fibre, while the SKD contained 78·2 g. The Hellers meatballs in sauce (dinner meal) were the greatest contributor with 29·60 g of fibre in a 200 g serving. This is surprising – as one would have expected the konjac noodles to be the greater provider of fibre; however, this is likely due to a low-carbohydrate filler like psyllium husk used in this product. The net carbohydrate content of this product is ∼3 g/200 g serving with ∼10·2 g of fibre. These findings are vastly different to those of Bracci et al. (Reference Bracci, Keogh and Milte20) whose case study results suggest that achieving sufficient fibre intake within the confines of the KD requirements is not possible. This inconsistency illustrates the impact that the types of foods chosen are an important factor in achieving sufficient fibre intake. The same can in fact be said for all nutrients, which is why careful planning and understanding the limitations and nutrients that may be challenging to obtain in each diet are important knowledge for adopters. These findings suggest that sufficient fibre intake can be achieved with vegan and the KD, which, given the importance of fibre for gut and vascular health, is important.
Protein
This study illustrates that whole food-based diets contain more protein than those that rely on UPF specialty products. The WFV and WFKD contained more protein (95·5 g and 142·8 g) than the SV and WKD meal plans (65·3 g and 125 g). As a result, three of the four meal plans contained sufficient protein in accordance with AMDR, with the SV meal plan not meeting the 15 % threshold. Previous research suggests that those adhering to vegan diets may be at risk of consuming insufficient protein and select essential amino acids (including tryptophan)(Reference Zinn, Rush and Johnson22,Reference Clarys, Deliens and Huybrechts36) . This is likely the result of the exclusion of animal products and by-products in the SV meal plan, which readily provide complete sources of protein containing all essential amino acids(Reference Bakaloudi, Halloran and Rippin6). For vegans, adequate protein intake can be achieved through careful consideration and the consumption of a variety of whole foods(Reference Melina, Craig and Levin5). This is shown in the present case study with the WFV diet containing 95·5 g or 16 % protein. When variety is reduced in favour of energy-dense specialty convenience products, protein content becomes a concern, with the SV diet containing 65·3 g or 11·6 % protein. It is also worth noting that the bioavailability of plant proteins is variable (50–70 %) and further affected by heating and cooking(Reference Bakaloudi, Halloran and Rippin6). Moreover, due to their relatively new introduction to the market, the digestibility of meat analogues is unknown and requires further study to understand(Reference Petersen, Hartmann and Hirsch12). These findings highlight the importance of a well-planned diet to achieve a specific macronutrient intake. When working with individuals adhering to a vegan diet, nutrition professionals can consider the inclusion of a plant-based protein supplement (e.g. hemp or pea protein) to enhance protein consumption should this be needed. It is worth noting that while a ‘food-first’ approach is often favoured, oftentimes when excluding key nutrients, the inclusion of supplements can enhance overall nutrient intake and make meeting thresholds more attainable.
Saturated fat
Saturated fat intake was beyond the 10 % TE threshold as recommended by the WHO in both the WFKD (28·4 %) and SKD (24·4 %) and the SV (17 %) meal plans(33). Based on previous research, and the nature of the KD, higher intakes of saturated fat were not unexpected with this dietary trend(Reference Bracci, Keogh and Milte20,Reference Zinn, Rush and Johnson22) . Although there is controversy and ongoing debate as to whether increased saturated fat intake negatively affects cardiovascular health, recent advances suggest that within the context of a whole food low-carbohydrate diet, saturated fat intake is not a key concern(Reference Volek, Phinney and Krauss15,Reference Astrup, Teicholz and Magkos19) . There is an acknowledgement among academics that food matrices and the overall dietary trend should be considered rather than isolating nutrients as this is not reflective of real life and the way that people consume food(Reference Cannon and Leitzmann40). In comparison, vegan diets are usually associated with lower intakes of saturated fat and higher intakes of carbohydrates (due to a reliance on fruits, vegetables, grains, cereals and legumes)(Reference Melina, Craig and Levin5,Reference Bakaloudi, Halloran and Rippin6) . However, with an increasing reliance on meat analogues, recent studies have shown an increase in saturated fat intake when convenience-type vegan diets are followed, illustrating the need to further understand the impact of food quality on health regardless of dietary pattern(Reference Tso and Forde13,Reference Wickramasinghe, Breda and Berdzuli14) . Given these findings, it is important that future research aims to quantify the effect of saturated fat on health in context of a high carbohydrate, predominantly processed food diet.
Vitamins and minerals
Both speciality meal plans (SV and SKD) did not meet Ca, vitamin A or Fe thresholds. Ca, alongside vitamin D, is crucial for maintaining bone health and preventing osteoporosis. Both Ca and vitamin D (which is affected by both nutrition and seasonal sunlight exposure) are commonly reported to be lower than recommended daily intakes in vegans(Reference Clarys, Deliens and Huybrechts36,Reference Elorinne, Alfthan and Erlund38,Reference Crowe, Steur and Allen41,Reference Karlsen, Rogers and Miki42) . Bioavailability and Ca absorption from plant-based foods is variable (5–50 %) vegans should aim for low-oxalate foods, including kale and bok choy, to maximise Ca absorption(Reference Melina, Craig and Levin5). To prevent vitamin D and Ca deficiencies, which can increase risk of fractures and have long-term health consequences (especially in females approaching menopause), the addition of a suitable supplementation regime on advice from a health professional can be considered. It should be noted that the inclusion of high-quality nutritional supplements would likely increase overall diet cost. Vitamin A (found predominantly in red and orange vegetables like carrots and bell peppers, beef liver, fish oil, milk and eggs) is crucial for supporting vision, immune function, reproduction and growth and development. A lack of whole foods in the specialty UPF meal plans is the likely cause of this observed shortfall and illustrates that relying on UPF can negatively impact nutrient intake, regardless of overarching dietary principles followed.
Fe is commonly reported as a nutrient of concern for vegans with absorption from non-haem sources varying from 1 to 23 % depending on Fe status and the presence of dietary enhancers and inhibitors(Reference Melina, Craig and Levin5,Reference Bakaloudi, Halloran and Rippin6) . With this knowledge, health-conscious vegans regularly supplement with Fe, pay careful attention to Fe absorption enhancers and inhibitors and closely monitor Fe status. It is worth noting that not all adopters of the vegan diet are motivated by health and that those who rely on UPF are at risk of falling short of Fe requirements. This could easily be corrected by including more whole foods. Fe intake in the SKD could be easily enhanced through the inclusion of green-lipped mussels or organ meats such as liver. These food sources were intentionally excluded from the sample meal plans as they are seen to be an acquired taste, but small amounts (i.e. 5 g) would suffice and organ meats could be frozen and grated into meals like bolognaise to enhance acceptability(Reference Zinn, Rush and Johnson22). Consumption of organ meats could also reduce overall diet cost due to their relative cost-effectiveness as an animal protein source.
When considering the shortfall of vitamin E, Zn and ALA in the SV plan, this is likely the result of a lack of whole food. This would be the reality for anyone relying predominantly on specialty UPF as the basis of their diet. To rectify these nutrient shortfalls for the SV and SKD plan, a supplement could be included or (in our opinion the more favourable approach) diet quality could be improved to include more whole foods. This illustrates the importance of diet quality in achieving optimal nutrient intakes.
Ultra-processed foods and health
The seemingly ever-increasing availability of UPF (both generic and speciality) is a public health concern as the consumption of these products in large quantities negatively affects health. A recent prospective longitudinal cohort study found that with each 10 % increment increase in UPF consumption, there was a corresponding 15 % increase in the risk of all-cause mortality(Reference Romero Ferreiro, Martín-Arriscado Arroba and Cancelas Navia45). While this research is based on mainstream UPF, given the similarities between these and niche or speciality foods, it is likely that these outcomes are transferable. There is a clear need for further exploration of the metabolic effects of a predominantly UPF diet, in the context of specialty dietary trends, with consideration on how satiety signalling is affected by elevated consumption of such products. Current evidence suggests a clear association between UPF consumption and non-communicable diseases; while the mechanisms at play are not yet known, due in part to the relatively recent introduction of these food formulations, it is believed to be multifaceted. First, these foods are formulated to be palatable and often include a combination of fat, sugar and salt, which drives overconsumption and is said to be linked to food addiction(Reference Chen, Zhang and Yang28). Due to manufacturers’ desires to enhance shelf life and promote long-term stability, the fats found in these foods are hydrolysed industrial trans fats, known to be harmful to health and promote inflammation(Reference Pipoyan, Stepanyan and Stepanyan46). It can be argued that replacing sugar with non-nutritive artificial sweeteners reduces overall calories and curbs consumption, but the evidence on this appears mixed(Reference Christofides47). Moreover, the potential implications of non-nutritive artificial sweeteners for gut health remain poorly understood. Second, processing and cumulative food additives appear to promote carcinogenicity and genotoxicity, adversely affecting the expression of genes and increasing risk of cancer(Reference Chen, Zhang and Yang28). Finally, high intakes of UPF adversely affect the gut microbiome, with evidence suggesting that they increase C-reactive protein and lipoprotein levels(Reference Chen, Zhang and Yang28). The inflammatory effect of UPF has received much attention in recent years; however, exact mechanisms of action require further exploration.
It is worth noting that when considering UPF, factors beyond the food formulations themselves are worth exploring, this includes but is not limited to the impact of additives and increased exposure to harmful chemical substances, which might cause endocrinological disturbances through both processing and packaging(Reference Muncke, Andersson and Backhaus48,Reference Pressman, Clemens and Hayes49) . Prolonged intake of an UPF diet is associated with biochemical alterations including oxidative stress, inflammation and intestinal dysbiosis as well as impaired immunological health(Reference Martínez Leo, Peñafiel and Hernández Escalante50). Research illustrates that chemicals in food packaging migrate to the foods we eat when they are in direct contact with one another, these are known as food contact chemicals and many have been linked to adverse health consequences(Reference Muncke, Andersson and Backhaus48). Toxicity thresholds are determined based on singular chemical components, this means that analyses do not take into account the cumulative impact of several different chemicals and their exposure(Reference Pressman, Clemens and Hayes49). Moreover, these thresholds are determined based on the chemical component but do not consider the by-products created during heating, cooling and storing for long periods of time which may also be toxic(Reference Pressman, Clemens and Hayes49). Finally, these toxic thresholds do not account for the effects which may exist at lower doses, particularly to the endocrine system(Reference Muncke, Andersson and Backhaus48,Reference Pressman, Clemens and Hayes49) . It is evident that the negative impacts of UPF are far reaching, beyond the nutrients themselves.
Cost
The whole food-based meal plans were cheaper than the specialty UPF meal plans for vegan and KD. The WFV and WFKD cost $17·04 and $22·24, respectively, while the SV and SKD cost $32·19 and $24·07, respectively. The cost differential is the result of the pre-prepared foods included in the specialty UPF meal plans like the frozen heat-n-eat meal for the SV ($13·00) and the pre-made meatballs in sauce for the SKD. The cost of the SV meal plan could be reduced by including cheaper convenience options like canned ‘nut meat’ and ramen noodles rather than pre-prepared options. However, it is worth considering that research suggests that consumers purchasing habits are trending towards an increased consumption of convenience foods such as meat analogues and heat-and-eat meals and away from singular items to prepare their own meals(Reference Gallagher, Hanley and Lane11,Reference Petersen, Hartmann and Hirsch12,Reference Wickramasinghe, Breda and Berdzuli14) . The KD meal plan cost was comparable for both the WFKD ($22·24) and SKD ($24·07), likely because there are not as many convenience options available for this dietary trend and both meal plans contain multiple meat and dairy products. The cost of the KD is poorly researched, to date there are no studies examining their cost and only two examining the cost of low-carbohydrate healthy fat diets(Reference Zinn, North and Donovan35,Reference Raffensperger44) . The findings of this case study are in accordance with previous research, indicating that lower carbohydrate diets tend to be more costly than regular diets. With the growing popularity of this dietary trend, further work should be conducted to assess the cost of this dietary approach.
The costs of both the KD and VGN diets could have been reduced by applying simple budgeting guidelines such as including items on sale or non-branded items, by pricing items at green grocers and butchers rather than from a supermarket exclusively and by shopping seasonally. Eating a predominantly whole food diet would reduce cost in this instance by reducing or removing specialty products. Interestingly, these findings contradict research regarding the cost of mainstream (i.e. not vegan or KD) UP foods, which suggests that high-quality diets are more expensive than low-quality diets(Reference Pedroni, Castetbon and Desbouys25). This may be in part due to the fact that VGN and KD specialty products are not yet produced on the same scale as mainstream UP foods; however, research indicates that for meat analogues at least this will not be the case for much longer(Reference Petersen, Hartmann and Hirsch12–Reference Wickramasinghe, Breda and Berdzuli14).
Conclusion
This case study highlights the importance of diet quality, regardless of the overall dietary pattern. There are several key limitations. First, despite the methods being used in other research, these hypothetical case studies are indicative of a single day. We believe that the meal plans are reflective of the eating patterns of those adhering to VGN and KD diets as they include realistic and familiar foods and the author’s own unpublished work found the foods included here are commonly consumed by those adhering to the vegan and KD. Second, this case study reflects intakes rather than serum levels. Serum levels may be more accurately indicative of the nutritional impacts of dietary trends. While they are not commonly measured in studies to date, predominantly due to associated costs, resources and the burden on participants, they might be an important consideration for future studies. Furthermore, meal plans were only created for a single demographic. Given anyone could adopt these dietary patterns, it is worth considering whether these diets would meet the nutrient requirements of populations other than non-pregnant adult females. Particularly, it is worth considering the applicability of these dietary patterns for children, pregnant women and the elderly given these populations require specific nutritional considerations.
Despite these limitations, this work highlights the importance of considering diet quality regardless of the perceived healthiness of a given dietary trend and illustrates a need to further understand the impact that specialty products have on nutrient density, nutrient intake, long-term health and the cost of food. Given the rising popularity of these types of products, it is a key public health consideration to establish whether these products are safe for long-term consumption. While there are evident, and widely reported differences between the KD and vegan diets, the purpose of this article is not to pit ketogenic and vegan approaches against one another but rather to highlight that the level of processing a food has undergone is an important consideration given the rapid changes in the modern food environment and the expected changes in coming years. Public health agencies should educate consumers to ensure they are choosing nutrient-rich and cost-effective food options. This choice will directly affect their risk of all-cause mortality and promote a longer more healthful life. While fortification is increasingly common, especially among speciality products, consumers should not rely on fortification for adequate micronutrient intake. Instead, public health agencies should equip consumers with adequate knowledge of the best whole food sources of various vitamins and minerals, as the bioavailability of micronutrients in fortified foods is not clearly established.
We do not advocate for a one-size-fits-all approach to nutrition and recognise the importance of context and that preferences, culture, religion and socio-economic factors all play a part in an individual’s dietary choices. We do believe that food quality, regardless of the chosen dietary trend, is an important consideration and that whole, unprocessed foods should form the basis of any diet, whether it be vegan, ketogenic or any other chosen approach.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authorship
K.-A.L.D.L.M. and C.Z. both contributed to the conception, design, drafting and final agreement of the version of the article to be published. K.-A.L.D.L.M. undertook the analysis and wrote the original manuscript draft.
Ethics of human subject participation
Not applicable. This study did not include any human subjects, and all work conducted was hypothetical in nature.







