The 2007 Royal College of Psychiatrists' campaign Images of Psychiatry had the aim of promoting psychiatry as a ‘modern, therapeutic medical discipline which supports recovery’. 1 The campaign's objectives included the development of undergraduate education in psychiatry, raising the proportion of UK medical students choosing psychiatry as their first-choice career to 10%, and reducing the stigma associated with psychiatry and mental illness. One target audience identified was doctors from disciplines other than psychiatry, with the objective of developing a positive and accurate understanding of psychiatry among them. Knowledge of attitudes of doctors from other disciplines towards psychiatry is vital in achieving the objectives listed above and in determining whether changes in attitudes towards psychiatry are needed among the medical profession.
The medical profession's attitudes to psychiatry appear to be negative, although the data are dated. Reference Harris2 Recent research on attitudes towards psychiatry within the medical profession itself is limited. Reference Buchanan and Bhugra3 There are more recent studies regarding attitudes of medical undergraduates towards psychiatry, and these suggest unfavourable attitudes towards psychiatry as a career compared with other medical disciplines. Reference Malhi, Parker, Parker, Carr, Kirkby and Yellowlees4 The need for proactive career advice and positive role models at an undergraduate level in order to encourage psychiatry as a career choice has been identified: Reference Maidment, Livingston, Katona, Whittaker and Katona5 only 4-5% of UK graduates make this choice currently, with 10-11% being the figure needed in order to sustain recruitment requirements into psychiatry. Reference Goldacre, Turner, Fazel and Lambert6
To date, undergraduate teaching in psychiatry has largely been by psychiatrists, although, with the introduction of hybrid curricula in medical schools such as that at Keele School of Medicine, 7 teaching may increasingly be provided in wider settings and by a broader group of professionals. Recent research has focused on undergraduate teaching of psychiatry in the primary care setting and indicates that general practitioners (GPs) may be in a good position to take a more active role in this. Reference Walters, Raven, Rosenthal, Russell, Humphrey and Buszewicz8 If GPs are to be the positive role models suggested, then their attitudes towards psychiatry may influence both their clinical practice and their ability to teach and promote the specialty.
There is little in the current literature with regard to GPs' attitudes towards psychiatry, and we were unable to find any prevalidated tool for assessing attitudes of the medical profession towards psychiatry. One well-validated tool that has been used extensively in research among undergraduates in measuring attitudes towards psychiatry is the Attitudes Towards Psychiatry (ATP-30) questionnaire. Reference Burra, Kalin, Leichner, Waldron, Handforth and Jarrett9 Although we noted that this tool was designed for an undergraduate population, we felt that the majority of questions remained relevant to a GP population and as such the tool has some face validity in our population. Previous use of the tool also allows a useful comparison of GPs' attitudes with published attitudes of student populations.
The primary aim of this study is to inform on current attitudes of GPs towards psychiatry as a discipline.
Method
Advice was sought from the National Research Ethics Service, which considered the study to be a service evaluation, and therefore ethical approval was not needed. The ATP-30 questionnaire was administered by the internal hospital mail system to all GPs within Shropshire listed within the primary care trusts as partners or salaried GPs (n = 239). They were asked to return the questionnaire by the same mail system within 1 month from the date of posting. All entries received by the closing date were entered into a prize draw for £150.
The ATP-30 consisted of 30 questions regarding attitudes towards psychiatry. Questions were designed to cover eight domains: psychiatric patients, psychiatric illness, psychiatrists, psychiatric knowledge, psychiatric careers choice, psychiatric treatment, psychiatric institutions and psychiatric teaching. These domains were not demonstrated to be valid by its creators, and the instrument has therefore been treated as having validity as a single scale. Reference Burra, Kalin, Leichner, Waldron, Handforth and Jarrett9 All response options were on a 5-point Likert scale (1, agree strongly; 5, disagree strongly). Positively phrased items (questions 4, 5, 9-12, 14, 15, 18, 20, 23, 25, 27-29) were reversed by subtracting the score from 6. A total score was calculated by adding all item scores (minimum score 30, maximum score 150). A high score indicates a positive attitude towards psychiatry. The ATP-30 scores were not calculated for respondents who omitted questions within the ATP-30. Demographic data (age and gender), years worked as a GP, experience in psychiatry, and current involvement in teaching of undergraduate psychiatry were also collected. All data were analysed descriptively using SPSS package 15.0 for Windows, and univariate analyses were used to find significant associations between ATP-30 scale and item scores and demographic data using the Mann-Whitney and χ2-tests respectively. Variables are reported to be significant if they showed 5% or more significance level. Corrections were made for type 1 errors using the Bonferroni method.
Results
The response rate was 61% (n = 145 from N = 239). The demographic data and results for experience in psychiatry and current involvement in teaching of psychiatry are shown in Table 1. The modal age range was 46-55 years (42.1%), followed by 36-45 years (32.1%); 62.4% of the respondents were male. The frequency distribution of number of years worked as a GP was fairly equal, but with the largest number in the category of 21 years worked as a GP (35.7%). Over half (52.1%) of the GPs had experience in psychiatry only as an undergraduate, while 47.9% reported postgraduate experience of working in psychiatry. More than a quarter of respondents (27.8%) were involved in teaching undergraduate psychiatry, 16.7% were not involved but would like to be, and 55.6% were not involved in teaching undergraduate psychiatry and did not wish to be.
Table 1 Demographic data
| Frequency | Valid % | |
|---|---|---|
| Age, years | ||
| < 35 | 20 | 14.3 |
| 36—45 | 45 | 32.1 |
| 46—55 | 59 | 42.1 |
| 56—65 | 16 | 11.4 |
| Total | 140 | 100.0 |
| Gender | ||
| Male | 88 | 62.4 |
| Female | 53 | 37.6 |
| Total | 141 | 100.0 |
| Time as GP, years | ||
| ⩽10 | 44 | 31.4 |
| ⩽20 | 46 | 32.9 |
| ⩾21 | 50 | 35.7 |
| Total | 140 | 100.0 |
| Experience in psychiatry | ||
| Undergraduate | 73 | 52.1 |
| Postgraduate | 67 | 47.9 |
| Total | 140 | 100.0 |
| Current teaching in psychiatry | ||
| Yes | 40 | 27.8 |
| No (would like to) | 24 | 16.7 |
| No (would not like to) | 80 | 55.6 |
| Total | 144 | 100.0 |
| GP trainer | ||
| Yes | 46 | 31.7 |
| No | 99 | 68.3 |
| Total | 145 | 100.0 |
Items from the ATP-30 were analysed individually, and a total score was derived from the summation of all items (with reciprocals of positively phrased items) as described earlier. The mean score for the ATP-30 was 113.9 (range 87-138, standard deviation 9.4 for the 134 participants for whom it could be calculated). Data were distributed normally, with no outliers; if 90 is considered to be the logical neutral point of the scale, then the results indicate a generally positive attitude towards psychiatry (Fig. 1).
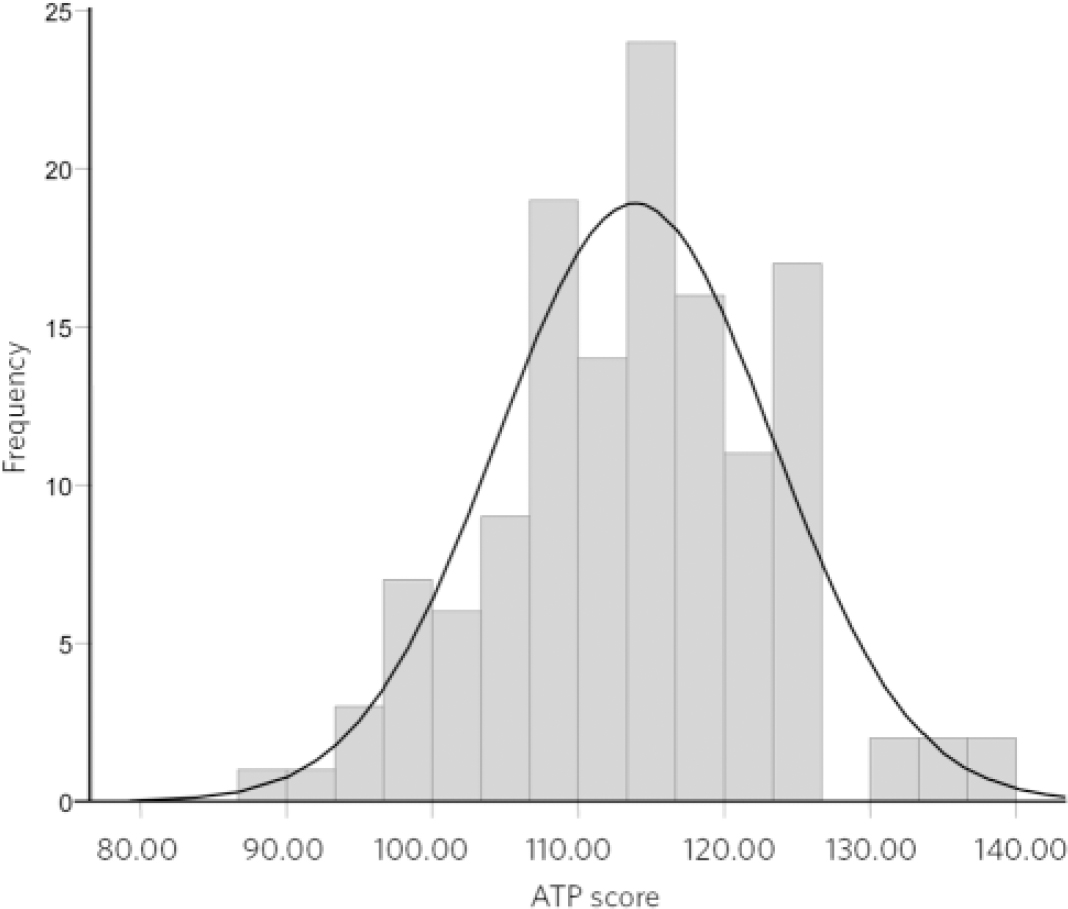
Fig 1 Attitudes Towards Psychiatry (ATP-30) scores. Mean score 113.89 (s.d. = 9.43), n = 134.
No significant associations were found between the demographic variables of age, gender, number of years worked, experience in psychiatry, teaching involvement in psychiatry and ATP-30 scores. There was an association found between GP trainers and higher ATP-30 scores (GP trainer: n = 40, mean rank 77.58; non-GP trainer: n = 94, mean rank 63.21; Mann-Whitney U-test statistic 1477.0, P = 0.050), but this was not significant when the Bonferroni correction for multiple testing (n = 6) was applied (threshold P = 0.008).
The three items from the ATP-30 scale that showed the most variability in responses and highest frequencies of negative responses are shown in Table 2, with 71.8% of respondents disagreeing or strongly disagreeing with item number 4 (‘I would like to be a psychiatrist’), 53.5% agreeing or strongly agreeing with item number 21 (‘If I were asked what I considered to be the three most exciting specialties, psychiatry would be excluded’) and 61.6% disagreeing or strongly disagreeing with item number 23 (‘Psychiatry is the most important part of the medical school curriculum’). Responses for all 30 items from the scale are shown in online Table DS1.
Table 2 Frequencies for item numbers
| Item | Response | Frequency | Valid % |
|---|---|---|---|
| 4 (‘I would like to be a psychiatrist’) | Strongly agree/agree | 15 | 10.4 |
| Neutral | 26 | 17.9 | |
| Disagree/strongly disagree | 104 | 71.7 | |
| Total | 145 | 100.0 | |
| 21 (‘If I were asked what I considered to be the three most exciting medical specialties, psychiatry would be excluded’) | Strongly agree/agree | 77 | 53.5 |
| Neutral | 26 | 18.1 | |
| Disagree/strongly disagree | 41 | 28.4 | |
| Total | 144 | 100.0 | |
| 23 (‘Psychiatry is the most important part of the medical school curriculum in medical schools’) | Strongly agree/agree | 10 | 7.0 |
| Neutral | 45 | 31.5 | |
| Disagree/strongly disagree | 88 | 61.5 | |
| Total | 143 | 100.0 |
Significant cross-tabulations made for associations between demographic data and individual response items on the ATP-30 scale are shown in Table 3. These were not significant when the Bonferroni correction for multiple testing (n = 180) was applied (threshold P = 0.0003).
Table 3 Correlations for demographic data and individual Attitudes Towards Psychiatry (ATP—30) items
| Demographic variable | ATP item number | χ2 | Degrees of freedom | P |
|---|---|---|---|---|
| Age | 14 (‘With the forms of treatment now at hand, most psychiatric patients now improve’) | 6.945 | 2 | 0.031 |
| 25 (‘In recent years, psychiatric treatment has become quite effective’) | 10.565 | 2 | 0.005 | |
| Number of years worked as a GP | 11 (‘Psychiatry is a respected branch of medicine’) | 9.821 | 4 | 0.044 |
| Experience in psychiatry | 15 (‘Psychiatrists tend to be at least as stable as the average doctor’) | 14.081 | 2 | 0.001 |
| 21 negatively phrased item (‘If I were asked what I considered to be the three most exciting medical specialties, psychiatry would be excluded’) | 7.933 | 2 | 0.019 | |
| Current teaching of psychiatry | 30 negatively phrased item (‘Psychiatry is so amorphous it cannot really be taught effectively’) | 9.769 | 4 | 0.045 |
| GP trainer status | 10 (‘The majority of students report that their psychiatric undergraduate training has been valuable’) | 8.063 | 2 | 0.018 |
| 28 (‘The practice of psychiatry allows the development of really rewarding relationships with people’) | 6.293 | 2 | 0.043 |
Discussion
The main finding from this study is that GPs in Shropshire have a generally positive attitude towards psychiatry. The positive attitude was independent of age, gender, number of years worked in general practice, experience in psychiatry, and involvement of the GP in undergraduate teaching in psychiatry. General practitioners who were trainers on the GP vocational training scheme may have higher scores. There were negative attitudes seen on individual items for the ATP-30, which appear to have some face validity. It should be remembered that the ATP-30 does not have proven validity for individual items (even in the population for which it was developed). It is, however, interesting to note that over 50% of our sample would exclude psychiatry from the three most exciting medical specialties.
There may be associations between individual scale item correlations and demographic data: older GPs, those who had worked for longer, those with postgraduate experience in psychiatry, those currently involved in undergraduate teaching, and GP trainers showed more positive attitudes on certain single-scale items. This may indicate that GPs who have had a longer career in general practice, GP trainers and GPs involved in undergraduate teaching value psychiatry more. These interpretations are tentative, as the scale has not been validated for individual items and threshold P values were not reached when corrections were made for multiple testing.
The demographic data shows a mature GP population, with 53.5% aged 46 years or over and 35.7% listed as working for 21 years or more in general practice. Postgraduate experience in psychiatry was relatively high, at 47.9%. It is interesting to note that 55.6% of GPs were not involved in teaching undergraduate psychiatry and did not wish to be, while 16.5% were not involved but would like to be. This may indicate an underused resource for student placements in Shropshire, and further exploration is warranted by local undergraduate course organisers, particularly as Shropshire has recently developed formal links with Keele School of Medicine. Shropshire has a relatively stable GP population, with high numbers of older GPs and low historic involvement with undergraduate teaching; this should be considered when generalising attitudes towards psychiatry to the wider GP population. The positive attitudes seen in our sample may reflect opinion regarding the quality of local mental health services; it is notable that Healthcare Commission reports rated Shropshire community mental health services as good 10 and Shropshire acute in-patient mental health services as excellent. 11
The study has other limitations. There is the possibility of a response bias: 61% of GPs responded, and those with unfavourable attitudes towards psychiatry may not have wished to participate in the study. There is also a question of validity of the tool for use in the chosen population. The ATP-30 was designed specifically for a medical student population, and a few of the questions did not relate well to practising doctors. The items listed in Table DS1 with particularly negative responses may not be valid for established practitioners and so may bias the results. The tool was designed in 1983 and some of the questions appear dated in their terminology. For example, question 23, which asks whether psychiatry is the most important part of a medical school curriculum, does not match contemporary approaches to curriculum development, and disagreement with this statement by GPs would not necessarily indicate a negative attitude to psychiatry; a positive response may indicate the tool's insensitivity rather than positive attitudes towards psychiatry. The ATP-30 was devised to measure the broad concept of ‘attitudes towards psychiatry as a discipline’. It is, however, possible that the attitudes shown here are reflecting something other than this. For example, practitioners' responses may reflect positive attitudes towards mental health rather than psychiatry as a whole. The scale does, however, by incorporating the eight domains stated in the Method, attempt to generate a broader opinion on psychiatry as a discipline. Notwithstanding considerations of validity, sensitivity and specificity, we consider that the comparisons with previous studies allowed by using the ATP-30 were more valuable than designing a new tool with no historical comparison data.
The mean ATP-30 score of 113.9 for this group of GPs compares favourably with scores from previous studies in sixth-form students (mean ATP-30 score 110.0), Reference Maidment, Livingston, Katona, Whittaker and Katona5 psychiatric residents (mean ATP-30 score 116.33) and medical students (mean ATP-30 score 103.76), Reference Malhi, Parker, Parker, Carr, Kirkby and Yellowlees4 and with a study showing pre- and post-psychiatry attachment mean ATP-30 scores in medical students of 102.6 and 107.7 respectively. Reference McFarland, Noble and Livingston12 This is reassuring, given the importance of psychiatry within the specialty, which may promote a more positive attitude among GPs than could be expected in other specialties. Further studies looking at the attitudes of doctors within other specialties would be useful and may also help to determine whether the ATP-30 is a sensitive discriminatory measure with regard to attitudes in practising doctors or whether a new tool needs to be designed for this purpose.
Funding
This study received partial funding from the Royal College of Psychiatrists' Images of Psychiatry campaign.







eLetters
No eLetters have been published for this article.