Introduction
Much has been written about how countries around the world responded to the COVID-19 pandemic and the resultant public health outcomes (Hu and Liu Reference Hu and Liu2022). One popular narrative is that the unfolding crisis allowed democratic/hybrid and authoritarian regimes to engage in democratic backsliding in the case of the former and further violate human rights and consolidate power in the latter. The most benign justification for these responses was that governments needed to take immediate and decisive actions to safeguard the health of their populations and, in so doing, infringements of individual rights were a small price to pay for the greater good. For example, tracking civilians through credit cards and CCTV is legalized in South Korea, Taiwan, Singapore, and China (Moon Reference Moon2020; Ha et al. Reference Ha, Araral and Wu2021). Another interpretation is that authoritarian regimes, in particular, used the pandemic to consolidate their grip on power and strengthen the position of autocratic leaders.
Freedom House (2020, p. 12), for example, noted that “the Covid-19 pandemic presents a grave threat to public health, but emergency measures adopted to combat the dangers can also have discriminatory impacts and harmful effects, and can be extended and repurposed after a crisis has passed.” This is particularly true in authoritarian regimes where restrictions can, prima facie, be heralded as protecting public health but, at the same time, impose greater infringement of civil liberties such as freedom of expression (free and independent media), associational rights (freedom of assembly), and personal autonomy (freedom of movement). All under the guise of safeguarding the public against the pandemic.
Authoritarian regimes claimed better public health outcomes, according to this popular narrative. China, for example, heralded the success of its communist regime in tackling the virus through draconian measures including locking down whole cities (Zhong et al. Reference Zhong, Liu and Christensen2022). Compare, for example, China’s statistics of 7.16 deaths per 100k population from the virus with the USA at 339.2 or the United Kingdom 322.9 (source: Johns Hopkins Coronavirus Resource Center at 20th February 2023). Other authoritarian regimes claimed similar success in tackling the pandemic using punitive measures. In Association of Southeast Asian Nations (ASEAN), for example, Vietnam fined people who posted Facebook comments on COVID-19 (Rüland Reference Rüland2021). Cambodia arrested people for spreading ‘false’ information on the pandemic. The Indonesian police criminalized defamation against the President and officials, and in the Philippines the National Bureau of Investigation summoned citizens for criticizing the Government’s response to the virus. In South America, the government of Nicolas Maduro (Venezuela) was accused by the United Nations Human Rights Council of using the state of emergency in response to COVID-19 to punish political opponents and exert further control over citizens.
These are examples of hard-line autocracies (Vietnam, Cambodia, Venezuela) or [highly] defective democracies (Indonesia and Philippines) which performed well in tackling the pandemic as measured by deaths per 100k population. Similarly, there are examples of democracies such as Japan, Australia, New Zealand, and hybrid regimes (Singapore, Pakistan) that had good public health outcomes in response to the pandemic. In parallel, (deficient) democracies such as the USA and Brazil whose leaders (former presidents Trump and Bolsonaro) lost public confidence through their inactions and performed very badly in dealing with the pandemic. A further explanation that gained popular appeal is that countries with Confucian traditions of respect for authority and compliance with rules performed better (Singapore, South Korea, Japan, Vietnam, and Taiwan). Yet several African countries (Tanzania, Nigeria, Congo, and the Central African Republic) with very good public health outcomes contradict this assertion.
Prima facie there appears to be no obvious relationship between regime type and their success in dealing with the pandemic. This merits further scientific enquiry. The aim of this paper is therefore to explore in some detail whether COVID-19 policy interventions in the form of stringency measures had different effects on COVID-19 outcomes, moderated by: (1) democracy level or regime type (authoritarian vs. democracy) and/or (2) the level of trust in government. The paper is structured as follows. In the next section, we locate the topic of enquiry in the existing literature on regime types and COVID-19 outcomes. From existing scholarship we develop hypotheses and test the relationships, using hierarchical regression models with cross-country data, between policy interventions (stringency measures) and public health outcomes. We control for population size and density, GDP per capita, and exposure to previous natural disasters and check for the moderating effects above. We conducted robustness checks with different outcomes such as the newly added infection rates, death rates, test rates, and excess mortality. Finally, we draw some conclusions and discuss policy lessons from the study.
Regime type and COVID-19 outcomes
Existing research breaks down into three broad thematic areas. First, there is a stream of scholarship that argues “there are unmistakable regressions into authoritarianism in governmental efforts to contain the virus” (Thomson and Ip Reference Thomson and Ip2020, p. 2). These were manifest in a variety of ways including restrictions on personal freedoms, an increase in monitoring and surveillance, and corruption in healthcare procurement and medical care delivery (Rapeli and Saikkonen Reference Rapeli and Saikkonen2020). Within existing authoritarian states, leaders used the pandemic to further consolidate their grip on power and control over their citizens. There are detailed country case studies that illustrate the extent of this abuse. In Southeast Asia, research on the Philippines showed how the Duterte regime used health checkpoints and lockdown rules (quarantines and curfews) to stop, detain, and arrest opposition activists and civil society workers involved in protecting the environment against the mining sector and illegal operators engaged in plundering the country’s natural resources (Dressler Reference Dressler2021). In Belarus, Lukashenko who had developed, over time, a working relation with civil society organizations involved in nonpolitical social and economic issues reverted to suppression and hostility during the pandemic. The state’s inactivity in responding to the COVID-19 crisis, indeed failure to recognize its very existence (described by Lukashenko as “panic” and “hysteria”), resulted in civil society filling the gap in public services. A mobilized civil society used its strength to launch a pro-democracy movement in the presidential election of 2020 and incurred the wrath of Lukashenko (Astapova et al. Reference Astapova, Navumau, Nizhnikau and Polishchuk2022). The pandemic therefore consolidated authoritarianism in autocracies such as China, Iran, Turkmenistan, Venezuela, Turkey, and Egypt but also in deficient democracies (Hungary) and working democracies (Egypt) through “violating the courts” independence, violating rights to mass protests or limiting the possibility to introduce constitutional changes due to the state of emergency’ (Machitidze and Temirov Reference Machitidze and Temirov2020, p. 73).
If, as the above literature suggests, there has been an increase in authoritarianism in response to the pandemic, has this resulted in better public health outcomes? The second strand of literature provides scholarship on this issue and is of direct relevance to the current research. Existing studies offer a diverse and sometimes contradictory range of evidence on the impact of regime type on the effectiveness of dealing with the pandemic. For example, the quality of healthcare facilities in democratic states resulted in better public health outcomes (Cepaluni et al. Reference Cepaluni, Dorsch and Branyiczki2020); death rates do not vary across regime types (Bosancianu et al. Reference Bosancianu, Dionne, Hilbig, Humphreys, KC, Lieber and Scacco2020; Cassan and Van Steenvoort Reference Cassan and Van Steenvoort2021); and “illiberal and authoritarian practices in response to the COVID-19 pandemic do not correlate with better public health outcomes” (Edgell et al. Reference Edgell, Lachapelle, Lührmann and Maerz2021, p. 1). Other studies are more nuanced suggesting that fewer COVID-19 deaths in authoritarian countries can be explained by lack of data transparency and manipulation of statistics (Annaka Reference Annaka2021; Kapoor et al. Reference Kapoor, Malani, Ravi and Agrawal2020). Additionally, scholars concluded that effectiveness in dealing with the natural disasters such as the pandemic is contingent on state capacity, the quality of implementing institutions, and technical and administrative readiness such as the capacity to govern data and digital platforms (Mazzucato and Kattel Reference Mazzucato and Kattel2020; Hanson Reference Hanson2015). Where institutional quality is low, more people seem to suffer in democracies than in authoritarian states (Persson and Povitkina Reference Persson and Povitkina2017). Other success factors in dealing with the pandemic include socio-demographic variables such as age, family structure (multigenerational family), and cultural attributes associated with institutional trust and civil obedience (Baniamin et al. Reference Baniamin, Rahman and Hasan2020).
The Lowy Institute (Australia) conducted an interesting study entitled ‘Deconstructing Pandemic Responses’ where they compared the comparative effectiveness of how countries had handled the pandemic by tracking six measures of COVID-19Footnote 1 in 116 countries for 43 weeks that followed their hundredth confirmed case, using data available up to March 2021 (Lowy Institute 2021). The study categorized the countries into authoritarian, hybrid, and democratic political systems based on the Economist Intelligence Democracy Index 2019. The researchers reasoned that the nature of political systems would influence how well or otherwise governments could enforce preventive or containment measures such as stay-at-home orders, lockdowns, and border closures. The study concluded that no single political system “stood out as being significantly or consistently more effective at managing the health crisis” (Lowy Institute 2021). Authoritarian regimes performed best at the beginning and end of the review period; democracies started badly, improved over time, and regressed in the later stages; and, many hybrid regimes appeared least able to meet the challenge.
The third and final strand of the literature introduces the concept of trust in government as a key factor influencing the effectiveness of state responses to the pandemic. A recent study of 136 countries on COVID-19 performance found that adopting more stringent control measures led to lower infection and death rates (Chen et al. Reference Chen, Li and Wu2022). However, the effects of restrictive policies are moderated by political trust and democracy levels – higher political trust and lower democracy levels result in lower infection and death rates. While the research stressed the importance of policy stringency and political trust, it cautioned against concluding that “authoritarian regimes are more conducive to policy effectiveness” (Chen et al. Reference Chen, Li and Wu2022, p. 918). The particular relevance of this reference to public trust is that in many post-Soviet countries, replete with authoritarian regimes (save for the Baltic states), citizens distrust government, politicians, and health care providers (Knox et al. Reference Knox, Janenova and Ha2023; McKee et al. Reference McKee, Murphy, Richardson, Roberts, Haerpfer and McKee2013; Sapsford et al. Reference Sapsford, Abbott, Haerpfer and Wallace2015; Laruelle et al. Reference Laruelle, Alexseev, Buckley, Clem, Goode, Gomza and Wishnick2021; Stancia et al. Reference Stancia, Crosby and Larson2023). Public trust is directly associated with compliance with government policy stringency measures (mask-wearing, social distancing, gatherings) during the pandemic and better public health outcomes (Bavel et al. Reference Bavel, Baicker, Boggio, Capraro, Cichocka, Cikara and Willer2020). Of particular interest is a recent study on governments’ responses to the pandemic and citizen assessments of how they managed the crisis in three post-Soviet states (Estonia, Georgia, and the Ukraine). The research team concluded that the most consistent factor influencing satisfaction with the COVID-19 response of the national government across the three countries was trust in institutions [President, Parliament, Cabinet ministries, and Ministry of Health] (Buckley et al. Reference Buckley, Clem and Herron2022). A similar study on post-Soviet Belarus, Kazakhstan, Moldova, Russia, and Ukraine (and Poland) found the efficacy of government agencies, compliance with stringency measures, and enforcement of violations to be key factors in how successful post-Soviet states tackled the pandemic (Zabuha et al. Reference Zabuha, Mykhailichenko and Rak2020; Knox Reference Knox2019; Knox and Janenova Reference Knox and Janenova2018).
Thus, two issues emerge from the literature which become the focus of this study. First, existing scholarship remains inconclusive or somewhat at odds as to whether authoritarian states performed better in tackling the pandemic than hybrid or democratic states. Second, the role played by stringency measures in the efficacy of the state response to the pandemic, particularly in authoritarian states, appears contingent on political trust which we know to be lacking in these regime types. We, therefore, hypothesize as follows:
H1: The relationship between stringency measures and pandemic outcomes is moderated by democracy level.
H1a: Authoritarian countries show better performance in reducing infection rates for their citizens than democratic countries, when increasing stringency measures
H1b: Authoritarian countries show better performance in reducing death rates for their citizens than democratic countries, when increasing stringency measures
H1c: Authoritarian countries show better performance in increasing test rates for their citizens than democratic countries, when increasing stringency measures
H2: The relationship between stringency measures and pandemic outcomes is moderated by political trust.
H2a: Countries with higher trust in government show better performance in reducing infection rate for their citizens than those with lower trust in government, when increasing stringency measures.
H2b: Countries with higher trust in government show better performance in reducing death rate for their citizens than those with lower trust in government, when increasing stringency measures.
H2c: Countries with higher trust in government show better performance in increasing test rates for their citizens than those with lower trust in government, when increasing stringency measures.
To sum up, the model is illustrated in Figure 1.

Figure 1. Model Diagram.
Data and methodology
To test the hypotheses above, we develop a cross-country dataset from several sources. The main source for policy interventions (stringency measures) and health policy outcomes is Our World in Data [OWID] website (Mathieu et al. Reference Mathieu, Ritchie, Rodés-Guirao, Appel, Giattino, Hasell, Macdonald, Dattani, Beltekian, Ortiz-Ospina and Roser2020). The OWID website has built 207 country profiles on the COVID-19 pandemic for every country in the world each day, including total deaths; newly added confirmed cases and deaths; total number of tests and new tests; and, government interventions as measured by the stringency index. Some of these data were used in several empirical articles including Chen, Li, and Wu (Reference Chen, Li and Wu2022), Leng and Lemahieu (Reference Leng and Lemahieu2021), and Wang (Reference Wang2022). We use the daily data up to December 10th, 2020 when the US Food and Drug Administration advisory panel endorsed the first Covid19 vaccine (American Journal of Managed Care January 2nd, 2021 report). In summary, our analysis therefore attempts to establish the relationship between policy interventions (stringency measures) and health policy outcomes with moderators in the early stages of COVID-19 before the introduction of the vaccine and its uptake.
In addition, we collected data for the moderators from two sources. First, the Freedom House Index (2020) is used as a measure of democracy, following the work by Frey, Chen, and Presidente (Reference Frey, Chen and Presidente2020). Second, for political trust, we used World Values Survey waves 5, 6 & 7, in line with research by Chen, Li, and Wu (Reference Chen, Li and Wu2022). To control other factors that might affect health policy outcomes: population size, population density, and per capita GDP in logarithms, are used as in scholarship by Chen, Li, and Wu (Reference Chen, Li and Wu2022) and Persson and Povitkina (Reference Persson and Povitkina2017). Finally, to account for the previous pandemic experience (Moynihan Reference Moynihan2008; Moon Reference Moon2020), we used the average number of bio-pandemic disasters from 2000 to 2019 taken from the International Disaster Database (EM-DAT) (Guha-Sapir et al. Reference Guha-Sapir, Below and Hoyois2016).
Dependent variables
The health outcome variables are infection rates, death rates, and test rates. The infection rate is measured by total number of confirmed cases of COVID-19 per 1 million people, on average. The death rate is measured by the total number of deaths attributed to COVID-19 per 1 million people, on average. The test rate is measured by total COVID-19 tests taken per 1 thousand, on average. For a robustness check, we also used as dependent variables: infection rates, death rates, test rates, or excess mortality. The daily data are taken from the website or GitHub website (Mathieu et al. Reference Mathieu, Ritchie, Rodés-Guirao, Appel, Giattino, Hasell, Macdonald, Dattani, Beltekian, Ortiz-Ospina and Roser2020). For example, Table 1 summarizes that average infection rate and death rate over the world are on average about 3,630 confirmed cases and 106 deaths per one million respectively up to Dec. 10, 2020. The test rate is on average about 104 per one thousand during the same period.
Table 1. Descriptive statistics

Note: + confirmed cases, deaths, or excess mortality per 1 million, ++COVID-19 tests per 1 thousand.
Independent variables
The main explanatory variable is the government policy interventions measured by the stringency index, part of the Oxford [Blavatnik School of Government, UK] COVID-19 Government Response Tracker (OxCGRT). The OxCGRT provides “a systematic cross-national, cross-temporal measure to understand how government responses have evolved over the full period of the disease’s spread” (Hale et al. Reference Hale, Petherick, Phillips and Webster2020, p. 3). It tracks government policies and interventions across a standardized series of 18 indicators (e.g. restrictions of gatherings; economic support; and, international travel controls). In our research (as per the GitHub codebook), to measure the government responses to COVID-19 across countries and time, we used the policy stringency index. This is a composite measure based on 9 (from 18) response indicators including school closures, workplace closures, travel bans and income support, rescaled to a value from 0 to 100 (100 = strictest policy implication) – see Appendix 1. Since the policy stringency index varies over time, we used the mean. Table 1 shows that the stringency index ranges from 13.83 to 88.84 on average over 162 countries and its mean is 59.65. Table 2 displays the correlations and pairwise significance among the variables in the model.
Table 2. Correlation among variables
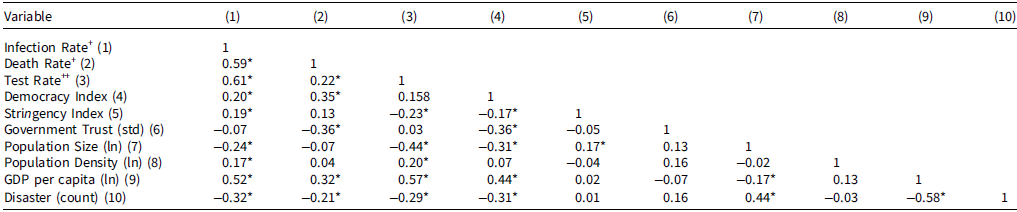
Note: * significant at 5 percent; +confirmed cases or deaths per 1 million, ++COVID-19 tests per 1 thousand.
Moderators
In our research, we focus on two moderators, democracy and trust in government, to see whether or how much these variables affect any relationships between policy interventions (stringency index) and policy outcomes (infection rate, death rate, or test rate). First, we utilized the Freedom House 2020 index to measure each country’s democracy level. The Freedom House 2020 index had been calculated before the COVID-19 pandemic occurred since “the 2020 edition covers developments in 195 countries and 15 territories from January 1, 2019, through December 31, 2019” (Freedom in the World 2020 Methodology, pg.1). The freedom index is an annual global report on political rights and civil liberties measured on a scale: 0 to 100 (100=the freest country). For example, Azerbaijan’s freedom index is 9 (categorized as not free), Malaysia scores 50 (categorized as partly free), and Denmark scores 97 (categorized as free). We divide the countries into two groups for analysis. A country is assigned as a “low freedom” group if its freedom index is below the mean, 55.8. Otherwise, it is assigned as a “high freedom” group. Second, to measure trust in government we draw on data from the World Values Survey, following Chen, Li, and Wu (Reference Chen, Li and Wu2022). Government trust is measured by citizens’ confidence in government (central or federal) on average by each country from wave 7 (Haerpfer et al. Reference Haerpfer, Inglehart, Moreno, Welzel, Kizilova, Diez-Medrano, Lagos, Norris, Ponarin and Puranen2020), wave 6 (Inglehart et al. Reference Inglehart, Haerpfer, Moreno, Welzel, Kizilova, Diez-Medrano, Lagos, Norris, Ponarin and Puranen2018b), and wave 5 (Inglehart et al. Reference Inglehart, Haerpfer, Moreno, Welzel, Kizilova, Diez-Medrano, Lagos, Norris, Ponarin and Puranen2018a) of the World Values Survey. It consists of 86 countries and is standardized with lowest trust (0) and highest trust (100). So, average trust in government is 37.22 with 22.16 standard deviation as outlined in table 1. This moderator was also predetermined before the pandemic for the same reason as the democracy level.
Control variables
The other control variables include: population size; population density or the number of people divided by land area (measured in square kilometers); and, GDP per capita at purchasing power parity (constant 2011 international dollars). These variables in logarithms are used as controls in Persson and Povitkina’s research (Reference Persson and Povitkina2017) which analyzed the effects of democracy and the quality of government on the extent of human suffering in natural disasters, including pandemics. Furthermore, according to Moynihan (Reference Moynihan2008) and Moon (Reference Moon2020), previous (failed) experience in handling a pandemic or disaster affects current preventive systems or agility to react which, in turn, results in better health outcomes. To take into account previous experience we used the average number of bio-pandemic disasters from 2000 to 2019 from the EM-DAT (Guha-Sapir et al. Reference Guha-Sapir, Below and Hoyois2016).
Methods
In order to test the above hypotheses, we used hierarchical regression models. This method allows for moderation effects to be recognized or tested by adding additional variables of interest, moderators, in the regression model (James and Brett Reference James and Brett1984; Baron and Kenny Reference Baron and Kenny1986; Cheong and Kim Reference Cheong and Kim2018; Ha and Park Reference Ha and Park2020). More specifically we can see any moderation effects of democracy levels (MO1) on the relationship between policy interventions (stringency measures) and health policy outcomes (infection, death, and testing rates) through M1∼M3 below. M1 refers to the regression model with only control variables; M2 with controls and independent variable (IV, stringency); and, M3 with a moderator (democracy level) in addition to the controls and IV. If the interaction term, stringency*democracy level (IVi*MO1i), in M3 is statistically significant, we can decide that there is a moderation effect. A moderation effect of government trusts level (MO2i), which can be tested on the interaction term, stringency*trust level (IVi*MO2i), is setup in M4. Finally, model 5 (M5) refers to a regression model of two moderators simultaneously. Depending on binary (low or high) democracy level and government trust level, each country can be categorized in four cases: low trust authoritarian state, low trust democratic state, high trust authoritarian state, and high trust democratic state. Table 3 displays the moderation effects and their coefficients in model 5 when the moderators are binary. In sum, the hierarchical regression models with two moderators are set up as follows:
M1: Yi = a1 + b1*Controls + ei
M2: Yi = a2 + b2*Controls + c2*IVi + ei
M3: Yi = a3 + b3*Controls + c3*IVi + d3*MO1i + e3*IVi*MO1i + ei
(or M3’: Yi = a3 + b3*Controls + (c3 + e3*MO1i) IVi + d3*MO1i + ei)
M4: Yi = a4 + b4*Controls + c4*IVi + f4*MO2i + g4*IVi*MO2i + ei
(or M4’: Yi = a4 + b4*Controls + (c4 + g4*MO2i) IVi + f4*MO2i + ei)
M5: Yi = a5 + b5*Controls + c5*IVi + d5*MO1i + e5*IVi*MO1i + f5*MO2i + g5*IVi*MO2i + ei (or M5’: Yi = a5 + b5*Controls + (c5 + e5 *MO1i + g5 *MO2i)IVi + d5*MO1i + f5*MO2i + ei), where Yi is the C19 outputs such as infection rate, death rate, test rate; IVi is the C19 policy responses (stringency index); MO1i is the first moderator, democracy level, and MO2i is the second moderator, government trust level; controls include population size, population density, and GDP per capita in logarithms, in addition to the number of prior disasters.
Table 3. Moderation effects by democracy level and trust level
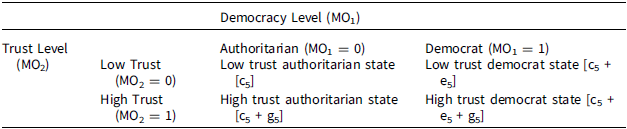
Note: [ ] refers to coefficients in M5 when moderators are binary.
Findings
Descriptive statistics
First, we analyzed the data in two groups, low democracy (authoritarian) vs. high democracy, by the democracy level measured by Freedom House 2020 index as explained above, to see whether authoritarian countries showed better health outcomes in terms of infection rate, death rate, and test rate, compared to democrat countries. Table 4 shows that authoritarian countries showed significantly lower infection rates and death rates, on average, in the first year of the C19 pandemic than democratic countries, 2622 vs. 4416 and 33 vs. 165, respectively. However, the policy interventions measured by stringency index are not significantly different on average, even though the authoritarian countries put more stringency measures in place to cope with the pandemic than democratic countries, 61 vs. 59 on 100 scale. Specific scatter plots with fitted lines by the two groups (Low vs. High democracy) are located in Appendix 4.
Table 4. Comparison by democracy level
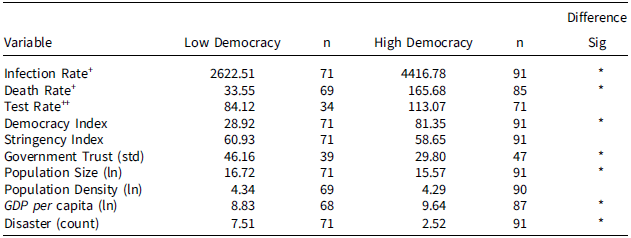
Note: n=number of country; * significant at 5 percent; + confirmed cases or deaths per 1 million, ++ C19 tests per 1 thousand.
In addition, these trends can be seen graphically in Appendix 3, displaying the infection rate, death rate, and test rate vs. democracy. For example, the trends of infection rate, death rate, and test rate are all increased as the democracy level increases. However, these trends are seen differently by the level of government trust. In other words, the positive slopes of infection rate and death rate vs. democracy are decreasing in the high-trust countries group.
Results from hierarchical regression models
For more rigorous analyses, we ran hierarchical regressions model. The results from the hierarchical model with binary moderators are shown in Table 5, where t statistics are calculated with robust standard error. Using the infection rate as the dependent variable which is measured by average confirmed cases per 1 million, model 1 (M1) implies that it is regressed only on the control variables, among which per capita GDP has a significantly positive relationship with the infection rate. Model 2 (M2) shows that the infection rate is significantly increased by about 88 cases per 1 million as the stringency index increases by 1 unit, ceteris paribus. The positive relationship implies that policy interventions (stringency index) are strongly enforced when the pandemic situation is worsening.
Table 5. Results from hierarchical model with binary moderators
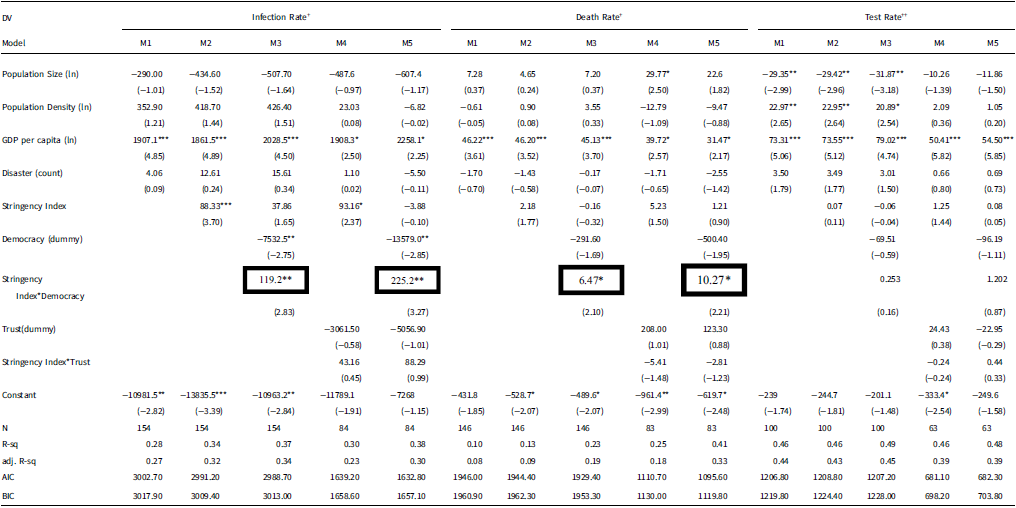
Note: t statistics in parentheses; * p < 0.05, ** p < 0.01, *** p < 0.001; + confirmed cases or deaths per 1 million, ++ C19 tests per 1 thousand.
Our main interest is the moderation effects of democracy level or trust level. Model 3 (M3), model 4 (M4), and model 5 (M5) refer to the moderation effects of democracy level, government trust level, and both, respectively. Only the democracy level has a significant positive moderating effect on the relationships between the stringency level (policy interventions) and infection rate or death rate (health policy outcomes). Specifically, since the moderator is binary, a democratic country has more infection rates by about 225 confirmed cases per 1 million on average than an authoritarian country, ceteris paribus, as seen in M5. For the death rate in M5, democratic countries have more death rate by about 10 deaths per 1 million on average, ceteris paribus. This result is similar to the result from Chen, Li and Wu (Reference Chen, Li and Wu2022). However, we did not find evidence of the government trust’s moderating effect on the relationships between the stringency level (policy interventions) and infection rate, death rate, or test rate (health policy outcomes). In other words, the interation terms (Stringency Index*Trust) in the model 3 (M3) or model 5 (M5) are not significant at the 5 percent significance level. In short we can, in part, confirm our research hypothesis that: authoritarian countries secure better public health outcomes in terms of infection rates and death rates for their citizens than democratic countries. This might be due to the directive powers of government, misuse of enforcement tools, and compliance of the public. To sum up, the H1a and H1b hypotheses are consistenly significant.
Robustness check Footnote 2
For the robustness check, we ran the hierarchical models with different types of moderators or different dependent variables such as average health outcomes newly added per day or excess mortality. First, we ran the hierarchical models with continuous moderators – see results in Appendix 5. Second, we changed the dependent variables with different measurements. Newly added confirmed cases, deaths, and tests per day, on average, are used as the dependent variables (DVs) for the hierarchical regressions model – see results in Appendix 6. Both results are similar to those in Table 5 explained above. However, the H1c hypothesis (test rate newly added) is confirmed only in Appendix 6 that summarizes the results from the hierarchical models with continuous moderators for the health outcomes newly added. Finally, we used a new dependent variable, excess mortality, instead of official COVID-19 health outcomes like death rate, in order to avoid the issue of ‘autocratic data fudging’ as Cassan and Van Steenvoort (Reference Cassan and Van Steenvoort2021) or Neumayer and Plumper (Reference Neumayer and Plümper2022) suggest. Excess mortality is defined by the World Health Organization (WHO) as “the mortality above what would be expected based on the non-crisis mortality rate in the population of interest” and considered a more objective and comparable measure due to the challenges such as ‘autocratic data fudging’ posed by using reported COVID-19 data. Following Neumayer and Plumper (Reference Neumayer and Plümper2022), we use the 2020 excess mortality estimates data over 159 countries as summarized in Table 1 (Global excess deaths associated with COVID-19).Footnote 3 The estimated results are displayed in Appendix 7 and show similar results as in Table 5. To sum up, the results are robust from the various robustness checks.
Discussion
This study dealt empirically with research questions on whether authoritarian countries that applied more stringent policies or interventions to fight against C19 showed better health performance in controlling infection and death rates from the pandemic while increasing the test rate. In addition, we tested the role of government trust in the relationships. We applied hierarchical regression with the data up to Dec. 10, 2020 before vaccines available on C19, a turning point in the pandemic. We focused on moderation effects of democracy level and government trust level on the relationships between the stringency level (an aggregate policy interventions index) and the infection rates, death rates, and test rates (policy outcomes). The results showed that the democracy levels have a significant moderation effect (hypothesis H1a and H1b confirmed). However, we did not find any evidence of trust in government’s moderation role in the relationships. These empirical results showed in part a similar result to Chen, Li and Wu (Reference Chen, Li and Wu2022). They indicated that the negative effects of restrictive policies on infection and death rates are moderated by political trust and democracy level. However, they did not conduct rigorous empirical tests on the moderation effects since they drew conclusions by showing the differences in the magnitudes that came from the separate regression results in two groups such as high vs. low democracy or trust groups. So, this research makes a contribution to the C19 pandemic study in terms of the moderation effects on policy interventions and public health outcomes between autocratic and democratic countries.
However, this research has some limitations. First, we used average aggregate data in the regression. In other words, the stringency index as an independent variable and policy outcomes such as infection rates, death rates, and test rates as dependent variables are averaged up to Dec. 10, 2020, even though we used additional data, daily added policy outcomes, as dependent variables for the robustness check. Second, from the same reason, we cannot control reverse causality. In other words, stringent policy interventions might induce better health outcomes, but poor health outcomes might also require stringent policy interventions. So, in order to overcome these limitations, further, more rigorous, studies will be required to see why authoritarian countries showed better performance in the control of infection rates and death rates, but there was no moderation effect of trust level on the relationships. First, we might construct panel data to control for the reverse causality as in Chen, Li and Wu (Reference Chen, Li and Wu2022) and Persson and Povitkina (Reference Persson and Povitkina2017). Using panel data, we might apply panel data analysis with lag variables or instrument variables. Second, to disaggregate stringency index, we might use a structural equations model estimating several policy variables and moderating or mediating variables simultaneously.
Conclusion
The data analysis provides evidence that authoritarian regimes have secured better health outcomes (a reduction on infection rates and deaths) in their response to the C-19 pandemic than democratic countries. There are a number of possible explanations for this conclusion. The first, and probably most important, is that there are limitations associated with the data. There is no standardized way of collecting and classifying cases and deaths resulting from the pandemic. Some countries count everyone who dies while infected with C-19 in their pandemic death toll, while others include cases in which the virus may have played a role. Still, others count deaths as those directly caused by complications from the virus, such as pneumonia. This can be illustrated through an example from Russia which has been accused of registering patients who die of a heart attack but have been diagnosed with C-19 by categorizing the former as the official cause of death. The death of people with underlying health conditions such as cancer, diabetes, and impaired kidney function may have been accelerated as a result of the virus, yet their deaths are not directly attributed to it. Similarly, with virus testing. Those countries that have participated in active testing where infections are uncovered will have a lower case-fatality ratio. There may also be systemic flaws in the ways in which data are collected and recorded. In many regions of Russia, for example, a death certificate must be presented to a local civil registry office, many of which were closed during lockdowns. The result is that some people simply buried their relatives without formal registration (Litinova and Isachenkov Reference Litinova and Isachenkov2020).
A second possible explanation for better health outcomes in authoritarian regimes is how autocrats have responded to the pandemic. Given fewer opportunities for ‘blame avoidance’ through distributive leadership now adopted in some democratic countries (where public health experts played a critical role), autocrats have increasingly adopted hard-line responses, reverting to type, by consolidating their repressive tactics. This has included the introduction of, or strengthening, existing laws to suppress protest, freedom of speech, and gagging negative social media commentary, in the absence of an independent press, on how leaders have handled the pandemic. Since citizens who live in these regimes, through legacy or learned behavior, are overwhelmingly passive, they tend to comply rationalizing these measures as a necessary public health response and out of fear of the authorities.
The final explanation is that international agencies such as the WHO and UN did not challenge low reporting of statistics on the pandemic. Hence in authoritarian regimes where it is relatively easy to massage or manipulate negative statistics, the role of WHO has simply been to report what information they receive rather than dispute it. WHO sees itself as an organization charged with coordinating the actions of the international community in combatting COVID-19, rather than one which confronts governments on how they report its prevalence.
What lessons can be drawn from the research? There is some learning from how authoritarian regimes have reacted to the pandemic. Autocrats have used the public health crisis as a way to legitimately consolidate their positions in the interests of protecting citizens. This has included more opportunities to silence their political critics under the guise of responding to the pandemic. Where this has included ‘emergency measures’, they are unlikely to reverse these excessive powers now available to them post-pandemic. The public health crisis also uncovered more opportunities for corrupt practice. Humanitarian medical products were being openly sold in pharmacies. Large government procurement contracts (with pharmaceutical companies, building contractors to provide new hospitals) had to be negotiated at relatively short notice, opening up significant opportunities for illegal and corrupt payments to politicians and officials. In addition, the informal economy in authoritarian regimes appears to be growing as repressive laws have driven more businesses underground and without proper regulation. In short, the development trajectory of authoritarian regimes may have been impeded or reversed, not simply because of the significant economic impacts resulting from the pandemic but also because their citizens feel cowered and disempowered even to express public criticism of those government services most needed during a pandemic – health care and social welfare.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0143814X24000163.
Data availability statement
Replication materials are available in the Journal of Public Policy Dataverse at https://doi.org/10.7910/DVN/HNCN4X
Acknowledgements
We wish to acknowledge the constructive feedback from anonymous referees, Dr Marika Csapo and Professor Charles Hankla.








