Child abuse and neglect in the context of primary attachment relationships are associated with detrimental long-term neurodevelopmental and psychosocial outcomes (Nelson & Gabard-Durnam, Reference Nelson and Gabard-Durnam2020; Sheridan & McLaughlin, Reference Sheridan, McLaughlin, Asmundson and Afifi2020). Children involved in the child welfare system have substantial exposure to this kind of interpersonal trauma and have disproportionate rates of emotional, behavioral, and psychological impairment (Tregeagle et al., Reference Tregeagle, Moggach, Trivedi and Ward2019). One of the central explanations for the link between maltreatment and developmental challenges is the disruption of attachment security, which plays an important role in systems of the brain responsible for threat assessment, emotion and behavioral regulation, and the formation of perceptions of self, others, and the world (i.e., internal working models) (Bowlby, 1969/Reference Bowlby1982; Cicchetti, Reference Cicchetti2016; Cyr et al., Reference Cyr, Euser, Bakermans-Kranenburg and Van Ijzendoorn2010; Schore, Reference Schore, Ford and Courtois2013). Further, insecure attachments can disrupt children’s readiness to engage in development-enhancing opportunities, impeding the acquisition of competencies and psychosocial strengths that become increasingly necessary for healthy functioning across the lifespan (Cicchetti, Reference Cicchetti2013). Indeed, studies consistently find that many maltreated children have fewer intra/interpersonal strengths (e.g., interpersonal skills, positive coping skills, creativity and optimism, sense of humor, affective and regulatory competencies, moral/spiritual strengths) than children without such histories of adversity (Barcons et al., Reference Barcons, Abrines, Brun, Sartini, Fumadó and Marre2012; Bevilacqua et al., Reference Bevilacqua, Kelly, Heilmann, Priest and Lacey2021; Carvalho et al., Reference Carvalho, Maciel and Basto-Pereira2020; Dorsey et al., Reference Dorsey, Burns, Southerland, Cox, Wagner and Farmer2012; Jorgensen et al., Reference Jorgensen, Cantio and Elklit2019; Kisiel et al., Reference Kisiel, Fehrenbach, Small and Lyons2009, Reference Kisiel, Fehrenbach, Torgersen, Stolbach, McClelland, Griffin and Burkman2014, Reference Kisiel, Summersett-Ringgold, Weil and McClelland2017).
The primacy of attachment security has facilitated the development of attachment-focused interventions to improve psychosocial outcomes among children and families who have experienced trauma. At the same time, given that strengths and positive coping skills among maltreated children are associated with fewer mental health problems and functional difficulties (Griffin et al., Reference Griffin, Martinovich, Gawron and Lyons2009; Kisiel et al., Reference Kisiel, Summersett-Ringgold, Weil and McClelland2017; Leon et al., Reference Leon, Ragsdale, Miller and Spacarelli2008; Lyons et al., Reference Lyons, Uziel-Miller, Reyes and Sokol2000), there are increasing calls for assessment and intervention to focus on identifying, leveraging, and building on children’s strengths to achieve better outcomes (Kisiel et al., Reference Kisiel, Summersett-Ringgold, Weil and McClelland2017; Noether et al., Reference Noether, Brown, Finkelstein, Russell, Vandemark, Morris and Graeber2007; Rashid & Ostermann, Reference Rashid and Ostermann2009; Simmons & Lehmann, Reference Simmons, Lehmann, Simmons and Lehmann2013; Tedeschi & Kilmer, Reference Tedeschi and Kilmer2005). Thus, while attachment security and strengths are important intervention targets to facilitate improvements to children’s functioning, there is a need to elucidate the relationship between these two constructs over time. It is plausible that increasing children’s attachment security will enable children to develop more strengths and positive coping skills; it may also be the case that children’s strengths mediate the relationship between interventions and attachment security, whereby children with more strengths more easily develop secure attachments with their caregivers in the intervention context. Alternately, these processes may co-occur, representing a transactional relationship (Leve & Cicchetti, Reference Leve and Cicchetti2016). To date, few prospective longitudinal studies have tested the interplay between attachment security and children’s psychosocial strengths among maltreated children involved in therapeutic services. Greater clarity on the directionality of associations between attachment security and psychosocial strengths may be informative for guiding clinicians and child welfare organizations in selecting appropriate interventions for children and families with histories of maltreatment and attachment disruption. Thus, in the present study we examined the trajectories of insecure attachment behaviors and psychosocial strengths in children involved with the child welfare system in Ontario, Canada as well as the interplay between insecure attachment behaviors and psychosocial strengths over time.
Psychosocial strengths and resilience
Strengths are multifaceted and have been widely defined (Peterson & Seligman, Reference Peterson and Seligman2004; Simmons & Lehmann, Reference Simmons, Lehmann, Simmons and Lehmann2013), though definitions point to strengths being individual characteristics and competencies that facilitate well-being and positive functioning in all domains of human life. Peterson & Seligman’s (Reference Peterson and Seligman2004) taxonomy of character strengths and virtues provides a comprehensive framework of individual strengths that parallels the existing deficit-oriented psychiatric nosologies (e.g., Diagnostic and Statistical Manuals of Mental Disorders, DSM) that predominates in clinical science and practice. This framework outlines several strengths, which individuals may develop over time and that typify the virtues of wisdom and knowledge (i.e., strengths include creativity, curiosity, judgment, love of learning, and perspective), courage (i.e., strengths include bravery, perseverance, honesty, zest), humanity (i.e., strengths include love, kindness, and social intelligence), justice (i.e., strengths include teamwork, fairness, and leadership), temperance (i.e., strengths include forgiveness, humility, prudence, and self-regulation), and transcendence (i.e., strengths include appreciation of beauty and excellence, gratitude, hope, humor, and spirituality). While resilience (i.e., responding to—and experiencing positive adaptation despite—exposure to significant adversity) is best understood as a dynamic process that depends on the interaction of constellation of stressors and resilience-challenging (risk) and resilience-promoting (protective) factors at multiple levels of analysis (e.g., Luthar et al., Reference Luthar, Cicchetti and Becker2000; Masten, Reference Masten2007, Reference Masten2018; Rutter, Reference Rutter2012), individual strengths have been identified as important resilience-promoting factors (Griffin et al., Reference Griffin, Martinovich, Gawron and Lyons2009; Hamby et al., Reference Hamby, Taylor, Jones, Mitchell, Turner and Newlin2018; Martínez-Martí & Ruch, Reference Martínez-Martí and Ruch2017). For example, Griffin and colleagues (2008) examined the moderating role of strengths in the relationship between traumatic experiences and risk behaviors in a sample of 8131 children entering the child welfare system in Illinois, found that, while children’s expression of risk behaviors increased as a function of the number of traumatic experiences they have had, the moderating effect of strengths also increased with the number of traumatic experiences. Thus, the more strengths children had developed, the less likely they were to engage in risky behaviors and the weaker the relationship between the number of traumatic experiences and risk behaviors.
Maltreatment, attachment security, and psychosocial strengths
Children who have experienced maltreatment are at risk of developing negative perceptions of self, others, and the world, such as viewing oneself as incompetent and unworthy, and others as being unavailable and untrustworthy (Cicchetti & Toth, Reference Cicchetti and Toth2016). Because the formation of attachment relationships occurs during early infancy and plays a key role in shaping neurodevelopmental and intra/interpersonal processes, attachment patterns tend to be moderately stable over time (Cicchetti, Reference Cicchetti2016; Opie et al., Reference Opie, McIntosh, Esler, Duschinsky, George, Schore, Kothe, Tan, Greenwood and Olsson2021; Van Ijzendoorn et al., Reference Van Ijzendoorn, Schuengel and Bakermans-Kranenburg1999). Attachment disruption has downstream impacts on children’s and adolescent’s ability to handle common demands in life and appropriately function in various environmental and social contexts. Moreover, attachment security may be an important protective factor contributing to resilience (i.e., adaptation in the context of adversity) (Rasmussen et al., Reference Rasmussen, Storebø, Løkkeholt, Voss, Shmueli-Goetz, Bojesen and Bilenberg2019; Valentino, Reference Valentino2017). However, insecure/disorganized attachments are considered a resilience-challenging (risk) factor, mediating the relationship between early trauma and adversity and later negative outcomes in various domains of functioning, including neurocognitive, psychological, social, academic, and vocational (Blaustein & Kinniburgh, Reference Blaustein and Kinniburgh2019; Kisiel et al., Reference Kisiel, Fehrenbach, Small and Lyons2009, Reference Kisiel, Fehrenbach, Torgersen, Stolbach, McClelland, Griffin and Burkman2014). Consequently, children who have experienced attachment-related trauma exhibit a wide range of symptoms often leading to comorbid diagnoses (Cicchetti & Doyle, Reference Cicchetti and Doyle2016; Cook et al., Reference Cook, Spinazzola, Ford, Lanktree, Blaustein, Cloitre, DeRosa, Hubbard, Kagan, Liautaud, Mallah, Olafson and Van Der Kolk2005; Farina et al., Reference Farina, Liotti and Imperatori2019; Tarren-Sweeney, Reference Tarren-Sweeney2007; Van Der Kolk, Reference Van Der Kolk2005) and fewer psychosocial competencies/strengths (Cicchetti, Reference Cicchetti2013; Dorsey et al., Reference Dorsey, Burns, Southerland, Cox, Wagner and Farmer2012; Jorgensen et al., Reference Jorgensen, Cantio and Elklit2019; Mikulincer & Shaver, Reference Mikulincer, Shaver, Schroeder and Graziano2013).
Blaustein and Kinniburgh (Reference Blaustein and Kinniburgh2019) posit that adverse outcomes corresponding to disrupted attachment are best understood as deficits in core developmental competencies pertaining to children’s intrapersonal (e.g., “sense of self and self-development”), interpersonal (e.g., “capacity to form and engage in relationships with others”), regulatory (e.g., “capacity to recognize and modulate emotional and physiological experience”), and neurocognitive (e.g., “capacity to engage executive functions and other cognitive abilities to act meaningfully in the world”) capacities (p. 18), which result in under-developed or limited strengths. In part, these difficulties can be attributed to reduced opportunities that insecurely attached children have, partly due to the child’s preoccupation with real or perceived threats in their relationships and environments.
In a cross-sectional study of children with complex trauma histories, Dorsey and colleagues (2012) examined the behavioral and emotional outcomes of 229 youth in 46 treatment foster care facilities with high rates of trauma exposure. Based on caregiver ratings on the Behavioural and Emotional Rating Scale (BERS; Epstein & Sharma, Reference Epstein and Sharma1998), which measures interpersonal strengths, intrapersonal strengths, affective strengths, family involvement, and school functioning, children with experiences of physical and sexual abuse and higher cumulative traumatic exposures had significantly fewer overall, interpersonal, and intrapersonal strengths. Kisiel and colleagues (2014) explored the outcomes of 16,212 children in the Illinois Child Welfare System who had experienced several types of trauma and were assessed using the clinician-report Child and Adolescent Needs and Strengths (CANS; Lyons et al., Reference Lyons, Uziel-Miller, Reyes and Sokol2000) tool. Children who had experienced both violent and non-violent trauma had more clinically elevated symptoms and higher levels of need in all areas of functioning than children with only one type of trauma or no trauma. These children had significantly lower levels of optimism and well-being and fewer interpersonal and vocational strengths. In a more recent longitudinal study, Bevilacqua et al. (Reference Bevilacqua, Kelly, Heilmann, Priest and Lacey2021) illustrated the developmental impact of early adversity on the acquisition and expression of psychosocial strengths, including prosocial behaviors (interpersonal competencies), in their survey of 19,000 children from the United Kingdom. Examining the relationship between exposure to family discord, parental psychosocial dysfunction, and harsh parenting practices, the authors found lower levels of prosocial behaviors at age 3 and flatter trajectories of the development of prosociality until age 14. This research indicates that children with experiences of maltreatment have fewer strengths and that their development of psychosocial strengths over time may also be impeded in the absence of intervention. Thus, attachment security and strengths may both be important targets for interventions among children and youth with histories of complex trauma exposure and attachment disruption.
Several longitudinal studies have examined the relationship between attachment security and psychosocial strengths in the context of attachment-focused interventions, such as Attachment and Biobehavioral Catch-Up (ABC; Dozier et al., Reference Dozier, Bernard, Roben, Steele and Steele2018), the Attachment, Regulation, and Competency (ARC; Blaustein & Kinniburgh, Reference Blaustein and Kinniburgh2019) framework, and Child-Parent Psychotherapy (CPP; Lieberman et al., Reference Lieberman, Ghosh Ippen and Van Horn2015). For example, Guild et al. (Reference Guild, Toth, Handley, Rogosch and Cicchetti2017) found that increased attachment security among 45 toddlers and mothers who received CPP was sustained and predicted the child’s social competence with peers at 9 years of age. This study demonstrated that increases in attachment security generalized outside the attachment relationship, whereby children had more psychosocial strengths, operationalized as teacher-reported social competence with peers in the classroom. Notably, most intervention-based studies have examined attachment security as the mediator between attachment-focused interventions and future positive psychosocial outcomes and increases in strengths, demonstrating that improving attachment security initiates a positive cascade (Masten & Cicchetti, Reference Masten and Cicchetti2010). Non-intervention longitudinal research has also conceptualized and modeled attachment security as a predictor of later strengths (Liu & Wang, Reference Liu and Wang2021; Mikulincer & Shaver, Reference Mikulincer, Shaver, Schroeder and Graziano2013). However, no studies have examined whether the relationship between attachment security and strengths may be transactional (Leve & Cicchetti, Reference Leve and Cicchetti2016).
The present study
The purpose of the present study is to test the directional relationship between attachment-related psychosocial challenges and psychosocial strengths in a sample of children involved in the Ontario child welfare system who have experienced at least one substantiated case of childhood maltreatment. Building on previous research, we sought to explore the initial and longitudinal trajectories of children’s insecure attachment behaviors and psychosocial strengths as well as the directional relationship between attachment-specific behaviors and strengths. Specifically, we sought to address the following questions: (1) ‘How are children’s insecure attachment behaviours and strengths initially and over time?’, and (2) ‘What is the directional association between insecure attachment behaviours and psychosocial strengths?’. For both questions we explored how age at first assessment (baseline age) and sex moderate expression of insecure attachment behaviors and strengths. We hypothesized that, consistent with previous research with a subset of the children involved in the current study (e.g., Smith et al., Reference Smith, Durham, Beatty, Price-Cameron, Kartusch, Shlonsky and Browne2022) and in other child welfare samples (e.g., Kisiel et al., Reference Kisiel, Fehrenbach, Small and Lyons2009) that older children at baseline would have more insecure attachment-related difficulties and fewer strengths at baseline. We also hypothesized that males would have more insecure attachment-related difficulties and fewer strengths overall, like the findings with a subset of adoptees in the present sample (Smith et al., Reference Smith, Durham, Beatty, Price-Cameron, Kartusch, Shlonsky and Browne2022). Finally, we predicted that improvements in attachment security would predict future improvements in children’s psychosocial strengths but not vice versa.
Method
Procedure
Sample. This study included caregiver-reported assessments for 555 children who received therapeutic services through the Therapeutic Family Care Program (TFCP) between the years 2000 and 2019. All children and youth had substantiated cases of maltreatment and were referred to TFCP by Children’s Aid Societies in three Southern Ontario catchment areas (Durham, Kawartha-Haliburton, and Highland Shores). The agency aims to support children’s healing from their traumatic experiences by fostering the development of secure caregiver–child relationships that are safe, accepting, and attuned to the child’s needs and histories. Throughout their involvement with TFCP, children’s caregivers completed assessments of their psychosocial functioning approximately every 6 months for TFCP’s standard monitoring and quality assurance procedures.
Most children (n = 313, 56.40%) resided in Foster Care at the time of their first assessment. Other children lived in kinship care (n = 116, 20.90%), adoptive care (n = 55, 9.91%), with a birth parent (n = 52, 9.37%), in a group home (n = 13, 2.34%), or in another placement (n = 6, 1.08%). Children were, on average, 9.57 years (SD = 3.51) of age at the time of their first assessment, and 229 (41.26%) were female. In terms of children’s baseline psychosocial functioning, children had an average of 3.12 (SD = 2.02) of the 10 domains of the Assessment Checklist for Children (ACC; Tarren-Sweeney, Reference Tarren-Sweeney2007) in the clinical range, and 356 (64.14%) children had clinically-elevated scores of the insecure interpersonal behaviour subscale (see below) at first assessment. This study was reviewed and approved by the University of Waterloo Ethics Board (ORE #41024).
Measures
Insecure Attachment Behaviors. The present study includes the attachment-specific subscale, insecure interpersonal behaviour, of the ACC. The subscale measures social behaviors and emotional difficulties related to insecure attachment and responsivity to severe stressors, including insecure, withdrawn, and overly conforming interpersonal behaviors. The full range of potential scores for the insecure interpersonal behavior scale is from 0 to 28, with scores below 4 indicating normative functioning, scores of 4 and 5 indicating sub-clinical symptoms, and scores of 6 and above indicating clinically significant impairment. Psychometric testing has found the insecure subscale have been found to be acceptable in previous studies (Tarren-Sweeney, Reference Tarren-Sweeney2007) and in the present sample: α = .78.
Child Strengths. In addition to the ACC, caregivers also completed the supplementary strengths checklist, the ACC+. The ACC+ is a 29-item caregiver-reported checklist of behaviors, emotional states, traits, and manners of relating to others, which suggest adaptive, pro-social functioning and well-being. While the measure was not specifically developed to reflect Peterson & Seligman’s (Reference Peterson and Seligman2004) taxonomy of character strengths, the items reflect several strengths within their framework, including creativity (e.g., “Engages in imaginative play”), bravery (e.g., “Stands up for him/herself”), perseverance (e.g., “Copes well with frustrating circumstances”), honesty (e.g., “Says when feelings are hurt”), zest (e.g., “Seems carefree (without concern or worries)”), love (e.g., “Is affectionate towards family or caregivers”), kindness (e.g., “Is kind or helpful to others”), social intelligence (e.g., “Keeps friends (maintains friendships)”), fairness (e.g., “Tolerates others receiving attention or praise”), prudence (e.g., “Sensible with strangers (appropriately wary, not overfamiliar)”), and self-regulation (e.g., “Seeks comfort or hugs from family or carers,” “Has a regular appetite”). Scoring of the ACC+ is opposite to the ACC, with higher scores indicating more positive outcomes for the child. Reliability for the ACC+ could not be calculated, given that the data available for this measure from TFCP did not include item-level scores. However, previous research has found the reliability for the ACC+ to be very good (α = .85 – .88) (Tarren-Sweeney, Reference Tarren-Sweeney2014)
Statistical analysis
We examined change in child clinical functioning using growth curve modeling, with the ACC+ and the insecure interpersonal behavior subscale from the ACC as the primary outcomes. We modeled repeated assessments as a function of time by calculating a continuous time variable (years since initial assessment) based on the date of each assessment. Additionally, we included age at first assessment and sex as moderators.
Next, we examined the longitudinal, directional associations between insecure attachment behaviors and psychosocial strengths using a random-intercepts, cross-lagged panel model (RI-CLPM; Hamaker et al., Reference Hamaker, Kuiper and Grasman2015). While panel models are typically run with measurement occasions being equivalent for all participants, the present data includes clinical data which were collected on a case-by-case basis rather than as part of a systematic and tightly scheduled data collection process. As such, there was considerable variation in the timing among the children within and between measurement occasions. Additionally, due to children’s natural attrition from the services, the number of measurements completed per child also varied. To overcome this challenge, we created 5 waves approximately every 6 months apart based on rounding the time since first assessment variable. The models included all children regardless of the number of assessments they received and full-information maximum likelihood (FIML) estimation was used to account for children with fewer than five assessments.
The RI-CLPM addresses problems associated with residual confounding commonly found in standard CLPMs by statistically isolating the between-person and time-invariant (stable) versus within-person and time-varying (dynamic) variance. Disambiguating stable and time-varying variance serves to reduce bias in directional estimates of associations and to more closely approximate causal inference (Berry & Willoughby, Reference Berry and Willoughby2017). We fit a series of nested models, beginning with a traditional CLPM and followed by a RI-CLPM with lagged regression parameters and within-time covariances constrained to equality over time and a RI-CLPM with no constraints on any parameters. We compared models with a chi square difference test to select the best fitting model before including sex and age at first assessment. In a RI-CLPM, the between-person (stable) factors were extracted from the repeated-measures of insecure interpersonal behaviors and strengths (ACC+) by constraining the factor loadings to 1, and these factors were permitted to covary. The covariance among the between-person factors reflects the association between attachment and strengths that is constant over time. The covariance also isolates the contribution of any between-person and/or time-invariant confounders that are associated with both attachment and strengths (e.g., child age at baseline) which would otherwise be conflated with the within-person component of the model. The within-person component comprises (1) autoregressions (i.e., lags), (2) within-time covariances, and (3) cross-lags. The autoregressions capture the within-person carry-over effect of constructs over time, while the within-time covariances capture the strength and sign of associations between attachment and strengths within persons at one time point, and the cross-lags capture the longitudinal and directional associations between insecure attachment and strengths within persons (Hamaker et al., Reference Hamaker, Kuiper and Grasman2015).
We conducted all analyses in RStudio version 1.3.959 (R studio Team, 2020). We used the lmer() function from the lme4 package (Bates et al., Reference Bates, Maechler, Bolker and Walker2015) for the growth curve analyses and the lavaan() function from the lavaan package (Rosseel, Reference Rosseel2012) for the RI-CLPMs.
Results
Trajectories of Insecure Attachment Behaviors and Strengths
Growth curve models are presented in Table 1 and Table 2 and visually depicted in Figure 1. Estimates (b) and 95% confidence intervals (95% CI) are presented in the text.
Table 1. Growth models for children’s insecure attachment behaviours
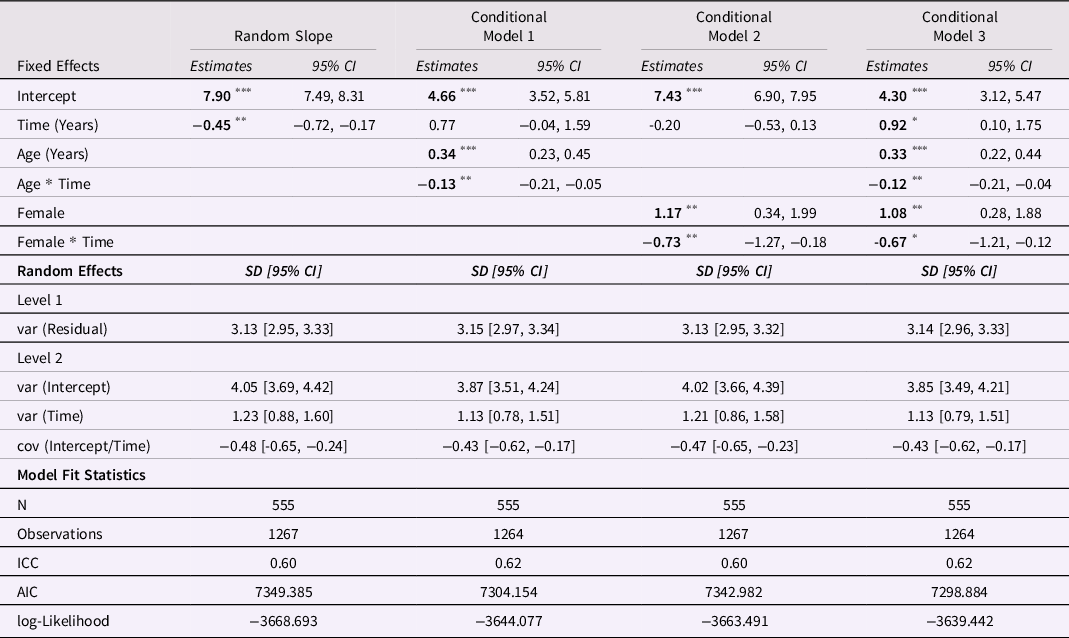
Note. var = variance. cov = covariance. * p < 0.05. ** p < 0.01. *** p < 0.001.
Table 2. Growth models for children’s strengths (ACC + scores)

Note. var = variance. cov = covariance. * p < 0.05. ** p < 0.01. *** p < 0.001.

Figure 1. Trajectories of insecure attachment behaviours and strengths over time.
Insecure Attachment Behaviors
Variance partitioning indicated that children’s insecure attachment behavior scores vary substantially between and within children. The intraclass correlation (ICC) from the null model (i.e., the random intercept model without any predictors) indicated that 54% of the variance in insecure attachment scores is due to individual differences. A random slope for time was added (see Table 1), suggesting that there were also significant individual differences in rates of change. Children started, on average, with clinically significant insecure attachment scores: b = 7.90, 95% CI = 7.49, 8.31. On average, children’s insecure attachment scores improved at a significant rate over time in the unconditional model (b = −0.45, 95% CI = −0.72, −0.17). The covariance between the random slope and intercepts for the children indicates that children who start off with the highest scores (i.e., those who exhibit the most insecure attachment challenges) show the most improvement (greatest decreases) over time (σu01 = −.49). In the adjusted models, child sex and baseline age significantly predicted children’s initial scores of insecure attachment behaviors, with females and older children starting off with higher (worse) scores (b _female = 1.08, 95% CI = 0.28, 1.88; b _baseline age = 0.33, 95% CI = 0.22, 0.44). In terms of trajectories, older children improved at a faster rate (b = −0.12, 95% CI = −0.21, −0.04). When gender was considered as a moderator of trajectories, females were improving significantly (b = −0.67, 95% CI = −1.21, −0.12) while males were getting worse (b = 0.92, 95% CI = 0.10, 1.75) (see Table 1, Conditional Model 3).
Strengths
Variance partitioning from the null model revealed that 53% of the variance in strengths scores are due to individual differences. After including the random slope for time (see Table 2) there was also significant between-person variability in rates of change. Children started with ACC+ scores of 60.18 (95% CI = 59.23, 61.12). Children’s ACC+ scores improved at a significant rate over time in the unconditional model (b = 1.24, 95% CI = 0.55, 1.93). Additionally, the covariance between the random slope and intercepts for the children indicates that children who start off with the fewest strengths show the most improvement over time (σu01 = −.33). However, this effect was non-significant in the adjusted models. In the adjusted models, baseline age was significant, with older children starting off with worse (lower) scores on the ACC+ measure (b = −0.48, 95% CI = −0.74, −0.21); however, baseline age did not predict children’s trajectories. There were also significant sex differences in ACC+ score at baseline, with females starting off with more strengths (b = 3.78, 95% CI = 1.90, 5.66). Sex did not predict trajectories of children’s strengths (see Table 2, Conditional Model 3).
Directional Association Between Insecure Attachment Behaviors and Strengths
Next, we fit a series of nested structural models, beginning with a CLPM, a RI-CLPM with lagged regression parameters and within-time covariances constrained to equality over time, and a RI-CLPM with no constraints on any parameters. While model fit indices revealed that all models fit the observed the data well, the RI-CLPM model with constraints fit best (see Figure 2): χ2(36) = 30.68, p = 0.72; root mean square error of approximation (RMSEA) < 0.00, 95% CI, <0.00, 0.02; Comparative Fit Index (CFI) = 1.000; standardized root mean square residual (SRMR) = 0.099. A nonsignificant chi square difference test supported the decision to opt for the more parsimonious model with constraints: Δχ2(15) = 9.16, p = 0.87. With this model selected, we added sex and baseline age as covariates; however, the inclusion of sex led to invalid results (i.e., negative variances). Thus, the final adjusted model only controls for children’s age at their first assessment. Notably, the relationship among the various model components (e.g., variance components, within-time covariances, autoregressions, and cross-lags) in the final model did not change after controlling for baseline age.
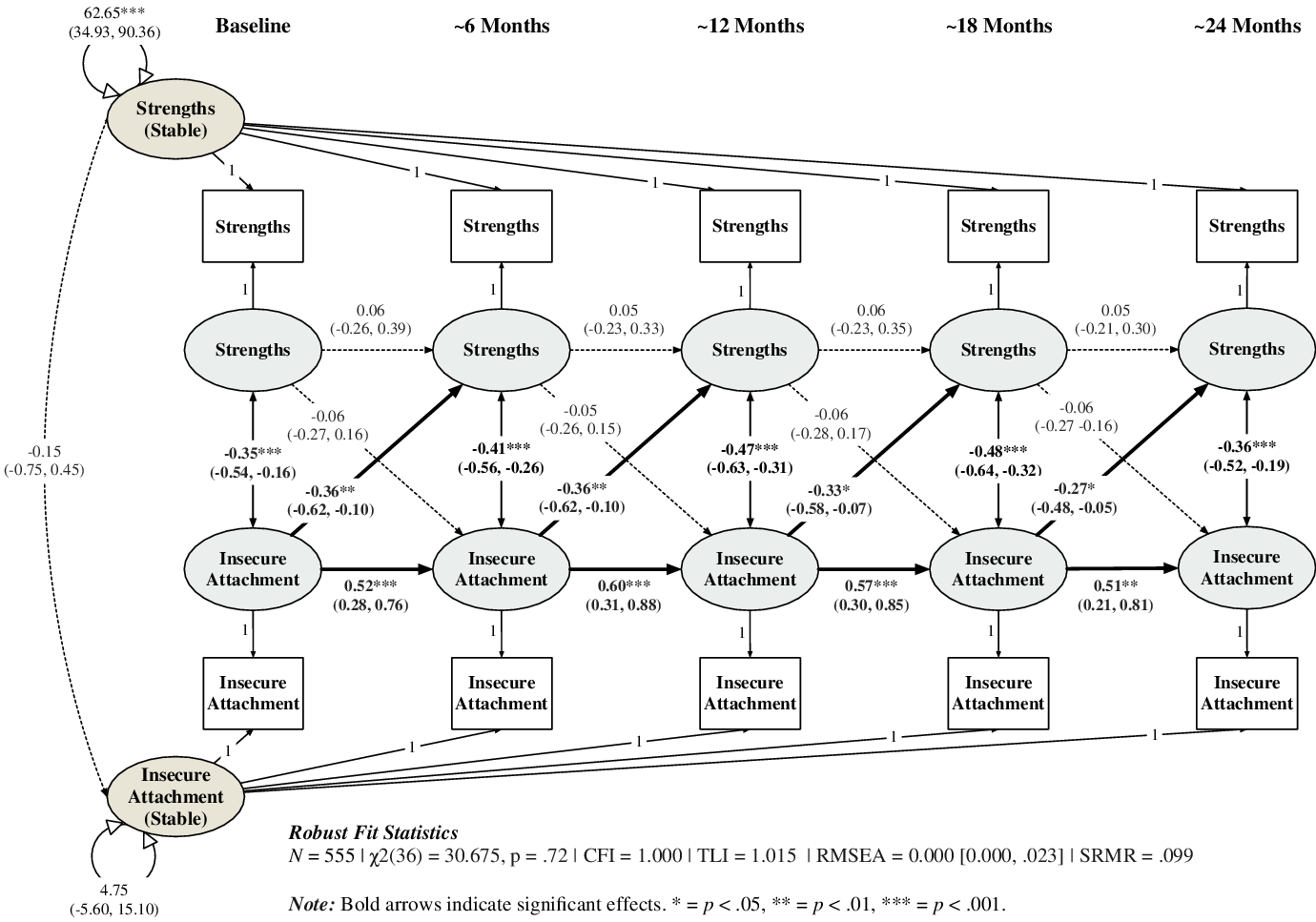
Figure 2. Random Intercepts, Cross-Lagged Panel Model of Insecure Attachment Behaviours and Psychosocial Strengths.
In the between-person part of the model, the statistically significant variance (i.e., random intercepts) for scores of strengths (σ2 = 60.85, 95% CI = 35.75, 85.95) reveals that, on average, some children/youth have more strengths than other children/youth irrespective of time. The non-significant negative covariance among the between-person components (cov = −0.12, 95% CI = −0.68, 0.43) suggests that children’s behavioral expressions of insecure attachment does not, on average and irrespective of time, predict children’s strengths and vice versa. Consistent with the growth models, baseline age significantly predicted the between-person components for both insecure attachment behaviors (b = 0.42, 95% CI = 0.07, 0.77) and strengths (b = −0.23, 95% CI = −0.35, −0.12).
In the time-varying component of the model, statistically significant autocorrelations and cross-lagged regressions for insecure attachment behaviors indicate substantial within-person variability over time for insecure attachment behaviors and strengths. Specifically, after controlling for baseline age, insecure attachment scores were stable approximately six months later (b = −0.52, 95% CI = 0.25, 0.80). After accounting for this within-person stability, the model identified significant and negative cross-lags linking lower insecure attachment behaviors with higher scores on strengths (b = −0.55, 95% CI = −0.97, −0.12). Also, within-time covariances were negative and significant at all time points (range cov = −0.34 – 0.47). These findings suggest that lower levels of insecure attachment difficulties, relative to a child’s average level, were associated with significantly more strengths approximately six months later, and that this relationship was constant across the 2 years of data included in the present study. The obverse direction of effects was not found. That is, strengths did not predict future levels of strengths, nor did they predict future expressions of insecure attachment behaviors.
Discussion
In the present study, we sought to examine insecure attachment behaviors and psychosocial strengths among child welfare-involved children and adolescents who have experienced maltreatment and are involved in caregiver-oriented and attachment-focused services. We had two objectives: first, to model the trajectories of insecure attachment behaviors and psychosocial strengths over children’s involvement in services and, second, to examine the longitudinal interplay between attachment insecurity and strengths. Given the deleterious effects of maltreatment on children’s attachment security (Cicchetti, Reference Cicchetti2016; Cyr et al., Reference Cyr, Euser, Bakermans-Kranenburg and Van Ijzendoorn2010) and competencies/strengths (Cicchetti, Reference Cicchetti2016; Masten & Cicchetti, Reference Masten and Cicchetti2010; Schore, Reference Schore, Ford and Courtois2013), we hypothesized that (1) children would initially have clinically-significant levels of insecure attachment behaviors and few strengths and (2) their insecure attachment behaviours would decrease, and their strengths would increase over time. Further, given the primacy of attachment disruption in the etiology of psychopathology and psychosocial dysfunction (Cicchetti & Doyle, Reference Cicchetti and Doyle2016), we hypothesized that there would be a directional effect driven by improvements in attachment security, which would lead to more psychosocial strengths in the future. The results of the present study partly supported these hypotheses.
The results supported our first hypothesis that, overall, children demonstrated fewer insecure attachment behaviors and more strengths over the course of their involvement in the services. Age was an important predictor for baseline levels of both insecure attachment behaviors and strengths, with older children/youth exhibiting more insecure attachment behaviors and fewer strengths, which is consistent with research in other child welfare contexts (e.g., Kisiel et al., Reference Kisiel, Fehrenbach, Small and Lyons2009). Interestingly, while age did not predict trajectories over time for strengths, older children/youth were found to improve more quickly over time with regards to their attachment security. The significant differential effect of sex at baseline (for both insecure attachment behaviors and strengths) and over time (for insecure attachment behaviors) is notable. The results suggested that females exhibited more symptoms of insecure attachment at baseline but earned security over time, whereas males’ insecure attachment behaviors increased over time. These results are consistent with a previous analysis, which included a subset of 81 children within the present sample who had experienced adoption (Smith et al., Reference Smith, Durham, Beatty, Price-Cameron, Kartusch, Shlonsky and Browne2022), indicating that the differential trajectories between males and females were not unique to adoptees or a product of the adoptive family environment. Additionally, this finding is consistent with some previous literature among children who had been late-adopted (M age at adoption = 5, SD age at adoption = 1.3) out of institutionalization or foster care (Pace et al., Reference Pace, Cavanna, Velotti and Cesare Zavattini2014), which found that males were significantly more insecurely attached and as having higher attachment disorganization compared to females.
The difference in male and female trajectories of insecure attachment behaviors points to the need for gender-sensitive clinical and child welfare practices, which would require a nuanced consideration of male and female socialization and emotional expression. Caregiver differential reporting may be due to males tending to externalize emotional distress thus resulting in more obvious expressions of attachment insecurity (American Psychological Association, Boys and Men Guidelines Group, 2018). Consequently, caregivers may have provided harsher reports for boys due to expectations of how males and females express their problems. This finding highlights the need for follow-up analyses to elucidate the factors that may explain the discrepancy between males’ and females’ responses to attachment-focused relational interventions. One consideration worthy of exploration, for example, is the role of father figures in the family system and in the relational interventions. Gender-sensitive practice guidelines call for the importance of fostering healthy child–father relationships and leveraging the unique contribution of fathers (American Psychological Association, Boys and Men Guidelines Group, 2018; Baum, Reference Baum2017). While including father figures (biological, foster, adoptive) has not been traditionally prioritized or encouraged within child welfare systems (Baum, Reference Baum2017; Freeark et al., Reference Freeark, Rosenber, Bornstein, Jozefowicz-Simbeni, Linkevich and Lohnes2005; Zanoni et al., Reference Zanoni, Warburton, Bussey and McMaugh2013), studies have documented positive outcomes for children with fathers who are involved and who provide high-quality care (Sarkadi et al., Reference Sarkadi, Kristiansson, Oberklaid and Bremberg2008; Yoon et al., Reference Yoon, Bellamy, Kim and Yoon2018; Zanoni et al., Reference Zanoni, Warburton, Bussey and McMaugh2013).
Our second hypothesis was supported: the analysis of the interplay between insecure attachment behaviors and strengths indicated a directional effect from attachment security to strengths but not vice versa. Thus, there was no evidence of a transactional relationship between the two constructs. Because the ACC+ includes an assessment of children’s ways of relating to his or herself as well as to others, including peers and non-caregiving adults, the directional relationship between improved attachment security and future improvements in strengths may indicate that children’s increased security is generalizing to contexts beyond the relationship with their caregiver. This finding supports theoretical and empirical work related to the role of cascading effects across development that can lead to psychopathology or resilience (Masten & Cicchetti, Reference Masten and Cicchetti2010; Cicchetti, Reference Cicchetti2013). Specifically, this study adds to the evidence pointing to the importance of the parent–child attachment relationship for children’s outcomes, indicating that insecure attachments lead to negative psychosocial outcomes and secure attachments lead to competence and well-being. The results of the RI-CLPM demonstrates the primacy of children’s attachments to their caregiver. Relatedly, the model supports previous theoretical and empirical work based on the connectionist framework of internal working models (Fraley, Reference Fraley2007), which suggests that one’s global attachment representations are not separate from relationship-specific attachment representations, but that global attachment representations represent an emergent feature of the way in which specific representations are constructed and used in social cognition (Gillath et al., Reference Gillath, Karantzas and Fraley2016). In other words, the benefits of fostering a more secure caregiver-child relationship extend beyond the scope of that specific caregiving relationship. Indeed, previous research has found a similar mechanism resulting from increasing parent-child attachment relationships (e.g., Bonds McClain et al., Reference Bonds McClain, Wolchik, Winslow, Tein, Sandler and Millsap2010; Guild et al., Reference Guild, Toth, Handley, Rogosch and Cicchetti2017), and this is the first study to examine the effects of attachment security on the development of positive psychosocial functioning among maltreated children in the context of the welfare system.
The present study was not designed to test the effectiveness of services and future randomized studies are needed to ascertain the directional relationship between intervention components, attachment security, and psychosocial strengths. Nevertheless, findings provide some basis for speculating upon these mechanisms. Our results imply that prioritizing attachment security could be a more efficient leverage point than focusing directly on building child competencies, given that caregiver–child and family relationships appear to have long-term, positive effects that generalize across domains of functioning. This is an important finding, which is supported by previous work illustrating that the attachment system is a central mechanism in the relationship between child maltreatment and psychopathology, due to its influence on social information processing and emotion regulation (McLaughlin et al., Reference McLaughlin, Colich, Rodman and Weissman2020; Schore, Reference Schore, Ford and Courtois2013). With that said, the directional effects seen in the present study may also be a product of TFCP’s emphasis placed on fostering secure caregiver-child relationships through the provision of caregiver-oriented, attachment-focused therapeutic services. Lastly, this study has relevance to policy makers within and beyond child welfare, supporting policies and initiatives that aim to enhance placement permanence, a position that has been enacted in Ontario via the Differential Response Model in Ontario (Ministry of Child and Youth Services, 2016) and advocated for based on the theoretical and empirical literature (Browne et al., Reference Browne, Johnson, Beatty, Cameron, Durham and Shlonsky2018; Tarren-Sweeney, Reference Tarren-Sweeney2021).
Limitations and future research
Despite the strengths of the present study, particularly the longitudinal nature of the data, sample size, and the sophisticated statistical analyses that enable approximations of causal relationships (Berry & Willoughby, Reference Berry and Willoughby2017), several limitations should be noted. First, the data used for this study were from the standard quality assurance and assessment procedures used at TFCP. Thus, we were limited to those variables already available in the dataset, which did not include several key covariates that would have been advantageous to include in the models of children’s trajectories and the RI-CLPMs. For example, it is clear from the literature that the accumulation of social and environmental risks can increase the complexity and severity of symptom presentations (Cook et al., Reference Cook, Spinazzola, Ford, Lanktree, Blaustein, Cloitre, DeRosa, Hubbard, Kagan, Liautaud, Mallah, Olafson and Van Der Kolk2005; Dorsey et al., Reference Dorsey, Burns, Southerland, Cox, Wagner and Farmer2012; Evans et al., Reference Evans, Li and Whipple2013). Including additional socio-demographic variables, race, and care setting, would be important to control for in future extensions of the present study’s analyses. Additionally, the types and chronicity of trauma that the children have experienced would be important variables to include in future research on the relationship between insecure attachment and psychosocial strengths, especially given the emerging evidence for the unique neurobiological and psychosocial and emotional impacts of different types of trauma (McLaughlin et al., Reference McLaughlin, Colich, Rodman and Weissman2020) and for single (acute) versus chronic and repeated (complex) trauma exposure (Cook et al., Reference Cook, Spinazzola, Ford, Lanktree, Blaustein, Cloitre, DeRosa, Hubbard, Kagan, Liautaud, Mallah, Olafson and Van Der Kolk2005; Ford et al., Reference Ford, Spinazzola, Van Der Kolk and Grasso2018). Similarly, given the breadth of strengths captured by the ACC+, future research should include more nuanced analyses whereby the relationship between attachment security and specific strengths is modeled in addition to a cumulative index of strength (i.e., poly-strengths; Hamby et al., Reference Hamby, Taylor, Jones, Mitchell, Turner and Newlin2018).
A second limitation of the research is the lack of comparison group who received an intervention that is not attachment-focused. It was therefore not possible for the current results to be interpreted as demonstrating the effectiveness of the intervention for improving children’s attachment security and strengths, as it did not compare these trajectories for children in a control condition. That said, given the results of other attachment-focused interventions such as CPP (e.g., Guild et al., Reference Guild, Toth, Handley, Rogosch and Cicchetti2017), ABC (e.g., Zajac et al., Reference Zajac, Raby and Dozier2020), and ARC (e.g., Bartlett et al., Reference Bartlett, Griffin, Spinazzola, Fraser, Noroña, Bodian, Todd, Montagna and Barto2018), this limitation does not negate the importance of the present findings. Additionally, due to the relative stability of attachment patterns over the life course in the absence of an attachment-focused intervention, it is conceivable that the improvements seen in children’s insecure attachment behaviors may be attributable to the intervention provided by TFCP. Alternatively, some research in community and foster care settings (e.g., Symanzik et al., Reference Symanzik, Lohaus, Job, Chodura, Konrad, Heinrichs and Reindl2019) has indicated that some children show improvements over time in dysfunctional attachments and associated problem behaviors without intervention, so the changes shown in the current study may have been partly the result of natural developmental processes. As such, the present analyses should be reproduced in a sample that can control for normative developmental change and various threats to internal validity (e.g., spontaneous remission, history).
Conclusion
In summary, children who have experienced maltreatment are more likely to develop insecure attachments and have fewer psychosocial strengths; however, the longitudinal interplay between insecure attachment and psychosocial strengths has received little empirical attention. While attachment patterns tend to be moderately stable over time, attachment security may be fostered in the context of enduring secure relationships with primary caregivers beyond infancy, which may support the development of strengths in multiple domains over time. On the other hand, children with more strengths may be better situated to develop more secure attachments in the context of stable and responsive caregiving relationships. The current study demonstrated the primacy of attachment security: children who exhibited more or fewer insecure attachment behaviors compared with their overall average tended to see subsequent and corresponding improvements or worsening in their insecure attachment behaviors and psychosocial strengths. Thus, the present study supported the use of attachment-focused relational interventions as a means of facilitating a positive cascade that begins with improving attachment security and permeates out to bolster children’s resilience and positive psychosocial functioning despite their experiences of maltreatment and involvement in the child welfare system.
Acknowledgments
We would like to thank the Therapeutic Family Care Program for sharing their data for the purposes of this research, the Durham, Kawartha-Haliburton, and Highland Shores Children’s Aid Societies, and the children and families whose experiences are represented in this research.
Author contributions
The authors confirm contribution to the paper as follows: study conception and design: JAS, DTB, DD, MPC; data collection: DD and MPC; analysis and interpretation of results: JAS and DTB; draft manuscript preparation: JAS, DTB, IS. All authors reviewed the results and approved the final version of the manuscript.
Funding statement
This research was financially supported by the Canada Research Chairs Program (DTB, #950-232347) and the Ontario Graduate Scholarship (JAS).
Conflicts of interest
None.
Ethical standards
This article was written and published in accordance with Cambridge University Press’ publishing ethics guidelines.







