High levels of psychiatric morbidity, Reference Teplin1-Reference Singleton, Melzer, Gatward, Coid and Deasey5 drug and alcohol dependence Reference Mason, Birmingham and Grubin6-Reference Brooke, Taylor, Gunn and Maden8 and rates of suicidal ideation Reference Borrill, Burnett, Atkins, Miller, Briggs and Weaver9 are found in prison inmates. Less research has been carried out in police custody. An observational study in London in the 1990s estimated the prevalence of serious mental disorder to be 2%. Reference Robertson, Pearson and Gibb10 More recent investigations have reported 16% with histories of self-harm and 7% who had been detained under the Mental Health Act 1983. Reference Payne-James, Green, Green, McLachlan, Munro and Moore11 There is also evidence linking the use of drugs and alcohol to the presentation of mental disturbance in custody, Reference Payne-James, Wall and Bailey12 along with the contribution of these factors to deaths in custody. Reference Leigh, Johnson and Ingram13,14 In a previous evaluation of consecutive custody records in London, we found evidence of mental disturbance in a third and psychosis in approximately 3% of detainees. Reference McKinnon and Grubin15 These prevalences are rather lower than those reported in prisons Reference Singleton, Melzer, Gatward, Coid and Deasey5 and are not dissimilar to those described in general practice. Reference Singleton, Bumpstead, O'Brien, Lee and Melzer16
Statutory responsibility for the welfare of detainees in police custody in England and Wales rests with the custody sergeant. 17 The sergeant must decide whether to refer a detainee to a healthcare professional. In addition, in the case of ‘mentally vulnerable detainees’ (a term employed within the Police and Criminal Evidence Act 1984), the sergeant should consider calling for an appropriate adult. 17 Sergeants are not clinically trained; in the London Metropolitan Police Service, new sergeants receive brief training on the identification of medical conditions requiring further assessment or treatment, but there is no ongoing training.
We have recently published data from the Health Screening in Police Custody (HELP-PC) project, demonstrating that current health screening procedures in London custody suites miss substantial amounts of general health morbidity. Reference McKinnon and Grubin18 In the current paper we concentrate on the psychiatric morbidity we observed in police custody detainees, the efficacy of police health screening procedures in identifying ‘at-risk’ individuals, and discuss the implications for managing detainees with mental disorder.
Method
The HELP-PC project is an evaluation of health screening procedures for custody detainees aged 18 and over in London, UK. It was carried out in two police stations. The method is described in detail in our previous paper. Reference McKinnon and Grubin18
In summary, the aim of the project is to obtain prevalence data from an unselected cohort of police custody detainees, and to judge the efficacy of the police health screen by comparing it with a clinical research interview by a psychiatrist. Full clinical assessment was limited to a maximum of 30 min because of the logistics of busy custody suites. Due to this limited time window the assessment of mental disorder employed a synthesis of symptom checklists adapted from ICD-10, 19 the 18-item Brief Psychiatric Rating Scale (BPRS-18) Reference Hafkenscheid20 and clinical judgement.
With regard to mentally vulnerable detainees who required an appropriate adult, we concentrated on detainees with suspected serious mental illness, intellectual disability and other cognitive problems judged not to be related primarily to the reversible effects of drugs or alcohol. The presence of any of these vulnerability factors was considered to require the presence of an appropriate adult during police interview of the detainee.
In total, 630 individuals were eligible for inclusion in the study, described in the flowchart in Fig. 1. Interviews with 237 individuals took place between April 2009 and September 2010. A further 11 who lacked capacity to consent to the formal interview as a result of mental disturbance were also included in the analysis. For the purposes of the evaluation of mental disturbance therefore, data from 248 detainees were available, representing a third of those who were eligible - others declined to take part, were unavailable or were deemed too violent for interview. The characteristics of the sample are described in Table 1.
Results relating to physical morbidity and injuries are described elsewhere. Reference McKinnon and Grubin18 Mental vulnerability as a result of intellectual disability, although referred to later, will be described in more detail elsewhere. Here we present results relating to psychiatric disturbance, suicide risk and morbidity related to the misuse of substances.
Ethical approval
Ethical approval was obtained from Newcastle and North Tyneside Research Ethics Committee in 2008 (08/H0906/130).
Results
Mental disorders
Based on clinical evaluation and capacity assessment, 96 detainees (39%) were assessed as presenting with some form of mental disorder (Fig. 2). The police screen detected a mental disturbance in 50 of the clinically recognised cases (52%, 95% CI 42-62).
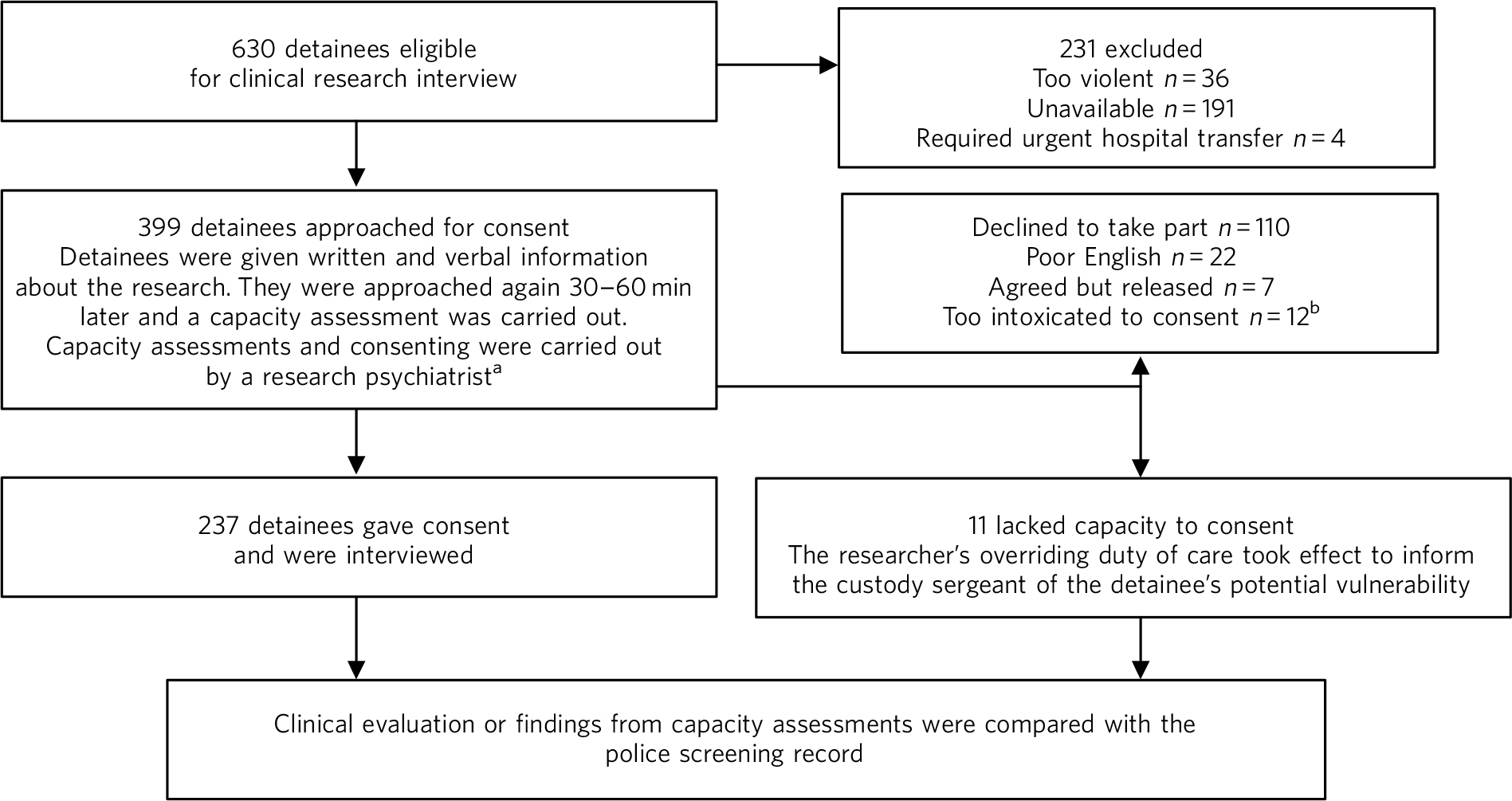
Fig 1 Flowchart describing the recruitment of eligible detainees.
a. Given the short amount of time for detainees to consider taking part, arrangements were made for retrospective withdrawal.
b. Intoxicated detainees were approached again to see whether they had sobered. This number refers to those who had not sobered sufficiently for consent to be obtained.
Table 1 Characteristics of detainees who consented to take part in the clinical research interview (n = 237)

| Characteristic | |
|---|---|
| Age, years: mean (median) | 33.3 (32) |
| Male, n (%) | 197 (83) |
| Ethnicity, n (%) | |
| Black and minority ethnic British | 29 (12) |
| White British | 94 (40) |
| Black and minority ethnic non-British | 68 (29) |
| White non-British | 42 (18) |
| Unemployed, n (%) | 132 (56) |
Eight detainees reported prior admission to psychiatric hospital, of whom five had been detained under the Mental Health Act.
Psychosis and non-psychotic affective disturbances
The number of detainees judged to have these mental disorders and the performance of the police screen in their detection is presented in Table 2.
No detainees in our sample satisfied ICD-10 criteria for severe depressive disorder. 19
Of the 19 detainees with psychosis, 14 completed the BPRS-18. Those with psychosis had significantly higher BPRS scores than the non-psychotic group (χ2-test for trend (d.f. = 1) 25.341, P = 0.000). Subscales for disorganisation, mannerisms, suspiciousness, unusual thought content and blunted affect were scored higher for the psychosis group (all P<0.001). The subscale for hallucinatory behaviour was also scored higher (χ2-test for trend (d.f. = 1) 4.279 (P<0.05). Detection rates of detainees with a mental disturbance related primarily to the effects of substances are presented in Table 3.

Fig 2 Mental status ascribed to 248 custody detainees. AA, appropriate adult.
We have previously reported the efficacy of the police screen in the detection of detainees who are current class A substance users and those at risk of alcohol withdrawal. Reference McKinnon and Grubin18 In summary, the majority of those at risk of alcohol withdrawal and those who had used crack cocaine prior to arrest were missed; those at risk of opiate withdrawal fared better.
Other disorders
In the time available it was not possible to ascribe personality disorder diagnoses to detainees. However, from the clinical history we judged that the effect of significant personality factors was a primary issue in seven individuals. Two of these detainees displayed behaviour disturbances so significant that they lacked capacity to consent to take part in the study, although there was no evidence of cognitive impairment. A mental disturbance was detected by the police screen in four of the seven cases, and although none were referred for an appropriate adult, all but one was referred to the healthcare professional.
Table 2 Detection and referral rates by the police screen and rate of calls for an appropriate adult

| Diagnosis | Number identified by clinical research evaluation |
Mental disturbance detected by police screen, n |
Proportion, % (95% CI) |
Number referred for assessment by healthcare professionalFootnote a |
Proportion, % (95% CI) |
Appropriate adult called, n |
Proportion, % (95% CI) |
|---|---|---|---|---|---|---|---|
| Psychosis | 19 | 15 | 79 (54-94) | 18 | 95 (74-99) | 8 | 42 (20-67) |
| Moderate depressive disorder | 13 | 9 | 69 (39-91) | 6 | 46 (19-75) | 0 | N/A |
| Mild depressive disorder | 23 | 11 | 48 (29-69) | 14 | 61 (39-80) | 1 | 4 (0-22) |
| Intoxicating effects of substances as primary cause of mental disturbance | 17 | 5 | 24 (7-50) | 13 | 76 (50-93) | 2 | 12 (1-36) |
| Personality factors as primary cause of mental disturbance | 7 | 4 | 57 (18-90) | 1 | 14 (0-58) | 0 | N/A |
N/A, not applicable.
a. The reason for referral did not necessarily relate to the mental disturbance.
False positives
The police screen identified mental disturbance in 59 of the 248 detainees from our sample; we found no evidence of mental disorder in 9 of these individuals (15%, 95% CI 7-27).
Suicidal ideation
In our recent paper, Reference McKinnon and Grubin18 we reported that the police screen detected between a third and a half of detainees who had previously attempted suicide or who had active suicidal ideation. From our current sample, 25 detainees disclosed current suicidal ideation on the Beck Scale for Suicide Ideation. Reference Beck and Steer21 Of these, 12 (48%, 95% CI 28-69) had any risk of suicide documented on the police screen; 6 of these referred to current risk. Of 44 detainees who disclosed a prior suicide attempt, 15 (34%, 95% CI 20-50) had risk of suicide noted.
Table 3 Referrals made by the police sergeants following screening for 19 detainees with psychosis

| n (%) | No
action taken, n |
Sergeant called
healthcare professional and appropriate adult,Footnote a n |
Sergeant
called healthcare professional only,Footnote b n |
|
|---|---|---|---|---|
| Mental disturbance detected by sergeant | 15 (79) | 1 | 8 | 6 |
| Mental disturbance not detected by sergeant | 4 (21) | 0 | 0 | 4 |
a. No cases had an appropriate adult called and no healthcare professional referral.
b. An appropriate adult was subsequently recommended by the healthcare professional for six of these ten detainees.
Mental vulnerability
Of the 28 detainees who were considered mentally vulnerable by the researcher and requiring an appropriate adult, 19 were assessed as being likely to have a psychotic disorder, 8 had clinical evidence of intellectual disability, and 1 had reported memory loss associated with an affective disturbance. An appropriate adult was called for 12 detainees in this group (43%, 95% CI 24-63).
Discussion
The HELP-PC project is a descriptive study of health morbidity and the efficacy of police health screening procedures within custody suites in London, UK. We considered, as far as possible, an unselected, consecutive sample of detainees. The sensitivity and specificity of the police screen was evaluated over a range of morbidities. As far as we are aware, this is the first study to use this method and procedure in this setting. Previous studies carried out among police custody detainees have relied on observational data Reference Robertson, Pearson and Gibb10 or pre-selected subgroups. Reference Payne-James, Green, Green, McLachlan, Munro and Moore11,Reference Shaw, Creed, Price, Huxley and Tomenson22,Reference Scott, McGilloway and Donnelly23
This paper considers the ability of standard police screening procedures to identify detainees with mental disorders. Although a mental disturbance was detected in 79% of cases of detainees with serious mental illness, an appropriate adult was called in only 42% of these cases. Although 95% of the detainees with psychosis were referred to the healthcare professional, examination of the custody records indicated that the reason for referral was not consistently documented. Moreover, even though two-thirds of detainees with moderate depressive disorder were described on the screen as having a mental disturbance, fewer than half were referred to the healthcare professional for further assessment.
With respect to the identification of detainees with significant mental health needs, our data suggest that the sensitivity of the screen can be improved. One approach may be to use evidence-based questions and observational cues within a screening package. A number of factors from the BPRS showed discriminatory potential in the identification of detainees with serious mental illness.
However, this is not the only consideration. As a series of undirected questions, the current screen lacks the scope to differentiate between categories of mental disorders. Even where a mental disturbance is acknowledged, the screen provides little assistance to the custody officer on what course of action to take. This appears to be reflected in the low rates of calls for appropriate adults, along with evidence that the referrals to the healthcare professional lack focus on the mental disorder.
Both a lack of and delays in obtaining appropriate adults have previously been identified as significant problems. Reference Nemitz and Bean24 It is unclear how much this influences sergeants’ decisions not to call for an appropriate adult where a mentally vulnerable detainee is identified. The absence of a specific definition for mental vulnerability under the Police and Criminal Evidence Act serves to compound this issue. 17
Only a third of detainees with a risk history of self-harm or who expressed current suicidal ideation were screened positive for risk of suicide. Sergeants have detainees’ self-reports, the police national computer and prior custody records at their disposal. Again, however, suicide risk and information from other sources were not systematically or consistently recorded. Furthermore, this part of the screen does not direct the sergeant to acknowledge mental disturbance detected elsewhere. Screening takes place at the custody desk: a busy, noisy environment, far from ideal for this type of enquiry. Although it is unlikely to be feasible to alter the circumstances in which this questioning takes place, there is scope to improve the documentation and communication of these risks among custody staff.
The low detection rate of detainees at risk of withdrawal from crack cocaine reflects our previous findings. Reference McKinnon and Grubin15 The custody suites where this study took place were drug-testing sites within the Metropolitan Police Service; we expected that a higher proportion of detainees would have divulged this information in the knowledge they were likely to be tested for drugs. At reception into custody, a detainee’s fear of harming their defence by divulging class A drug use may outweigh their concern about drug withdrawal hours later while still in custody. Drug withdrawal during police interview may have detrimental effects on a detainee’s ability to concentrate and give reliable evidence. Reference Sigurdsson and Gudjonsson25 It is unclear how changes to self-report screening for crack cocaine would benefit detection rates.
Limitations
We could only interview 38% of the available detainees, giving rise to the possibility of selection bias. Those with problems requiring the attention of a healthcare professional stayed in custody longer, and were thus more likely to be approached and have their consent obtained by researchers. It is not possible to say whether the group we missed had differing levels of morbidity than those we interviewed or whether psychiatric morbidly was missed by the police screen in these cases.
Relying on self-report as a key part of the method can lead to reporting bias in detecting psychiatric morbidity. However, obtaining detainees’ general practice or psychiatric records was not feasible.
The window of opportunity for recruiting and carrying out clinical evaluations of detainees while in custody is narrow: at most 30 min. We opted for a pragmatic, structured clinical history carried out by post-membership research psychiatrists. This has the drawback of lacking the robustness of validated tools and meant that we were not in a position to make judgements about the cause of psychosis where there was comorbid substance use. Despite the limitations of this approach in terms of diagnostic validity, it reflects the pragmatic approach that would be employed by a psychiatrist ‘on call’ attending a custody suite to give an opinion on mental disorder.
Implications for clinical practice
That the screen performed poorly in respect of detection and documentation of certain areas of psychiatric and associated morbidity is of considerable concern given the evidence linking psychiatric and drug-related mental disturbance to deaths in custody. 14,Reference Best, Havis, Strathdee, Keaney, Manning and Strang26
Other significant developments are changes to the provision of liaison and diversion services in police custody. Recent reports have highlighted the need to identify detainees at the earliest stages within the criminal justice system. Reference Bradley27,28 Dedicated liaison and diversion services are now emerging; it is conceivable that the role of screening for mental disorders may be assumed by these teams. However, the Police and Criminal Evidence Act requires the custody sergeant to assume overall responsibility for the detainee while in custody. Furthermore, there are other significant morbidities to consider, including physical health, injuries and risk of alcohol withdrawal, for which more robust screening is required as we have previously reported. Reference McKinnon and Grubin18 Taken together, there is still a need to improve overall screening procedures for detainees at reception by custody sergeants. Potential benefits include:
-
• improved identification and documentation of morbidity
-
• providing a well-defined pathway for detainees with health problems
-
• enhancing the police’s interactions with health services by way of more relevant clinical information being available
-
• improved safety of detainees within the custody suite by more effective highlighting of risks
-
• improved inter-agency communication of health and associated risk (e.g. courts, probation, prison services).
It should be acknowledged that custody sergeants are a heterogeneous group, with a wide range of experience. Some will have more proficiency in identifying detainees with mental disorder than others. Throughout the duration of this study, researchers observed that some sergeants would expand on screening questions to acquire a more detailed profile of a detainee; others tended to stick more rigidly to the questions on the screen. Researchers also observed that there was a wide range of opinions on how to effectively manage detainees with mental disorder.
As part of the wider reforms, the Metropolitan Police Service is beginning to introduce civilian staff to undertake activities on behalf of the custody officer; these include recording the health screening of custody detainees, under the supervision of a custody officer. Although these staff members receive training on the role of booking detainees into custody, many lack the hands-on experience of a police sergeant, which may further exacerbate the issue of missing significant cases. Therefore a more structured approach to identification along with observational cues may be of benefit.
Given these considerations, we recommend that modifications be made to police screening procedures to improve their efficacy, provide a method of documenting significant findings, and signpost appropriate pathways for detainees who screen positive. Care must be taken, however, not to avoid having an adverse effect on specificity leading to more false positive results; this could have significant resource implications for health cover within the custody suite. Additionally, given the time constraints in a busy custody suite, it will be important not to increase the time needed to carry out the health screen, particularly if any improvement is likely to be marginal. This process should be structured, based on the currently available evidence, and piloted with a robust evaluation of efficacy and impact on health and service outcomes. To evaluate the efficacy of such modifications, a pilot of a modified health screen is underway within the Metropolitan Police Service.
Acknowledgements
We wish to thank Sergeant Cathy Nicholson from the Metropolitan Police Service Custody Directorate who provided essential support to the research team during the data collection. Further thanks to Mr Graham Manfield, Superintendent Dave Imroth and Sergeant Alistair Morley for their support. Inspector John Phillips (Wimbledon Custody), Inspector Tony Rayner and Sergeant Michael Clayman (both Islington Custody) provided on-site assistance at their respective custody suites.
Dr Margaret Stark, Forensic Physician and formerly Medical Director of the Metropolitan Police Service, provided further medical advice to I.M. and D.G., orienting them to Police Medical Services in London. Dr Julie Thorp spent time assisting I.M. with data collection and preparation.








eLetters
No eLetters have been published for this article.