Introduction
Self-efficacy theory was described by Bandura in 1977 (Bandura, Reference Bandura1977). It proposes that a person's belief or self-confidence in the ability to undertake a task is a precursor for initiating behavioural change. Thus, it is a central concept in the self-care and self-management of a person's health.
Self-efficacy appears to be important (Lorig et al., Reference Lorig, Stewart, Ritter, Gonzalez, Laurent and Lynch1996). First, the strength of belief that a particular result can be achieved predicts motivation and behaviour. The higher a person's self-efficacy, the more likely they are to put effort into a task, and recover from setbacks in the process. Second, self-efficacy can be enhanced by acquiring skills (performance mastery), learning from others (modelling), re-interpretation of symptoms, as well as through social persuasion. Self-efficacy reflects a person's optimistic self-belief about being able to change and adopt a healthy lifestyle (Strecher et al., Reference Strecher, DeVellis and Rosenstock1986), and is strengthened when patients succeed in solving patient-identified problems (Bodenheimer et al., Reference Bodenheimer, Lorig, Holman and Grumbach2002). Third, enhanced self-efficacy leads to improved behaviour, motivation, thinking patterns and emotional well-being. Belief in one's efficacy to exercise control is thought to be a common pathway through which psychosocial influences affect health functioning (Bandura, Reference Bandura2004). Finally, self-efficacy, unlike dimensions of personality, seems to be specific to problems or situations (Gerin et al., Reference Gerin, Litt, Deich and Pickering1995). Enhancing self-efficacy in one domain does not increase it in another, and different measures are needed to assess self-efficacy for each health-related behaviour being studied.
Since Bandura's concept of self-efficacy was introduced, many scales have been developed to measure self-efficacy for particular aspects of health care. Two such examples are the Medication Adherence Self-Efficacy Scale (Ogedegbe et al., Reference Ogedegbe, Mancuso, Allegrante and Charlson2003) and the Self-Efficacy for Exercise Scale (Resnick and Jenkins, Reference Resnick and Jenkins2000). In this paper, we focus on self-efficacy in doctor–patient interactions, using the Perceived Efficacy in Patient–Physician Interactions Questionnaire (PEPPI) scale.
A database search of titles of published studies in peer-reviewed journals such as AMED, BNI, EMBASE, HMIC, MEDLINE, PsycINFO and CINAHL, using self-efficacy, communication, confidence, interaction and older, elderly, doctor, health care or professional as keywords, showed only 13 articles, none of which focussed on older people's self-efficacy or confidence in interactions with doctors.
To the best of our knowledge, this is the first study to explore factors associated with self-efficacy in doctor–patient interactions in older people.
However, there are many studies from different continents that use self-efficacy as a measurable variable, and which show that interventions can alter self-efficacy. Improvements in self-efficacy in a cohort of people with rheumatoid arthritis receiving educational programmes as part of routine clinical care were measured in one UK study (Hewlett et al., Reference Hewlett, Cockshott, Almeida, Richards, Lowe, Greenwood and Kirwan2008). Perceived self-efficacy has been found to predict outcomes of a controlled-drinking programme in Australia (Sitharthan and Kavanagh, Reference Sitharthan and Kavanagh1990), and self-efficacy has been proven to be a powerful personal resource in coping with stress (Lazarus and Folkman, Reference Lazarus and Folkman1987). Chambliss and Murray (Reference Chambliss and Murray1979) published a US study showing that people who were overweight were most responsive to behavioural treatment when they had a high sense of self-efficacy. Self-efficacy in older women receiving an exercise intervention significantly predicted exercise behaviour at follow-up when controlling for biological and behavioural influences (McAuley, Reference McAuley1993). Increases in physical activity over time were associated with greater improvements in self-efficacy, which was in turn associated with improved physical function performance (McAuley et al., Reference McAuley, Morris, Doerksen, Motl, Liang, White, Wójcicki and Rosengren2007).
Although there are no studies that focus on self-efficacy in communication or confidence in doctor–patient interactions in older people, many studies have shown that self-efficacy in communication is both measurable and modifiable. For example, patients’ ratings of the effectiveness of professionals’ communication are important predictors of the outcomes of diabetes self-management (Heisler et al., Reference Heisler, Bouknight, Hayward, Smith and Kerr2002).
The aim of the analysis reported in this paper is to measure self-efficacy in patient–doctor interactions in a sample of community-dwelling older people, and to explore factors associated with such self-efficacy, including the uptake of preventive care. Self-management may depend on the confidence an individual has in working with a doctor or a nurse as much as on their confidence in their own ability to initiate and sustain changes in their own behaviour. Self-efficacy in doctor–patient interactions is therefore a potentially important determinant of self-care for any given medical problem. Understanding factors associated with higher self-efficacy in doctor–patient interactions may be useful for clinicians to recognise and focus on those who have less confidence in their interactions with health-care professionals. In addition, it may be possible to measure the impact of interventions on modifying self-efficacy in doctor–patient interactions in older people.
Hypotheses
We hypothesised that lower self-efficacy in doctor–patient interactions would be associated with fewer years in education and lower income, higher consultation rates and lower uptake of preventive care. We hypothesised that there would be no significant associations with lifestyle (smoking, alcohol intake, high fat and low fibre intake), functional abilities and other demographic characteristics.
Methods
Three large group practices in suburban London were recruited to participate in a multi-centre, multinational randomised controlled trial investigating the effect of the Health Risk Appraisal for Older persons (HRA-O) on health behaviours and status (Stuck et al., Reference Stuck, Elkuch, Dapp, Anders, Iliffe and Swift2002). Practices were purposively selected for their interest in primary care for older people, location in London (suburban) and routine use of electronic medical recording systems in clinical encounters. Local research ethics committee approval was obtained from Brent Medical Ethics Committee and King's College Hospital Research Ethics Committee. A full account of the methodology of the study is available elsewhere (Stuck et al., Reference Stuck, Kharicha, Dapp, Anders, von Renteln-Kruse, Meier-Baumgartner, Iliffe, Harari, Bachmann, Egger, Gilman, Beck and Swift2007), including recruitment of practices and patients, training of general practitioners in health promotion with older people, use of reminders and the evidence justifying the preventive care recommendations given. For more information on the HRA-O study and papers derived from it on the topics of social isolation, living alone, the experience of pain and predicting disablement, go to http://www.ucl.ac.uk/pcph/dev/research-groups-themes/age-stud-pub/previous-research/6 (UCL website for the HRA-O study). This paper is the fifth in a series aimed at a primary care audience.
To identify eligible patients aged 65 years and over, practice lists were cleaned by general practitioners. Eligibility criteria were: those living at home, without a) evidence of need for human assistance in basic activities of daily living, b) high dependency due to major physical or psychiatric illness, or cognitive impairment or c) a terminal illness. Patients also had to have a sufficient knowledge of English to complete the questionnaires. This patient population was further evaluated using the Probability of Recurrent Admissions (Pra) questionnaire (Pacala et al., Reference Pacala, Boult and Boult1995) and asked to complete a consent form by post. The Pra measures risk of hospital admission, and stratifies the population by level of risk for future in-patient care, and was used in the main study as the basis for risk-stratified outcome analyses.
Eligible and consenting patients were posted the HRA-O questionnaire. The HRA-O is a multidimensional, self-completion questionnaire that collects information on health, functional status, health behaviours, preventive care and psychosocial factors in older people (see Table 2). The development of the HRA-O questionnaire, the derivation of the instruments used in it, the exact definitions of categories (eg, ‘low physical activity’) and the feasibility of its use in British primary care have been reported elsewhere (Iliffe et al., Reference Iliffe, Kharicha, Harari, Swift and Stuck2005). Non-responders to the initial mailing were sent a postal reminder. Those who responded, and those who did not report the need for human assistance in basic activities of daily living, were included in the study.
At the one-year follow-up, surviving participants were sent a HRA-O questionnaire with additional questions on health-care use. This follow-up questionnaire included all items required for outcome analysis. In addition, the one-year follow-up questionnaire was used for obtaining information on socio-economic information and self-reported chronic conditions among participants in the control and concurrent comparison groups. No reminders were sent to people not returning this questionnaire. To reduce the amount of missing information on preventative care, practices were asked to review patient medical records for information on preventative care use (vaccination coverage, blood glucose and cholesterol measurement, colon cancer screening) for patients who had returned the 1-year follow-up questionnaire but had incomplete information on some items of preventative care. In total, 97 patient records were used.
This questionnaire included five questions used to measure self-efficacy according to the PEPPI scale (see
Box 1). ‘Not confident’ responses were scored as 1, ‘confident’ answers were scored as 3 and a score of 5 was given for a ‘very confident’ answer. The lowest possible score was 5 and the highest was 25.
Box 1
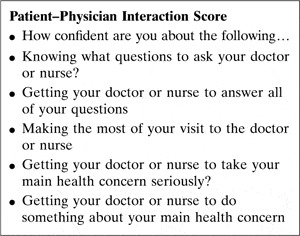
This was used to measure older patients’ self-efficacy in obtaining medical information and attention to their medical concerns from doctors. Maly et al. (Reference Maly, Frank, Marshall, DiMatteo and Reuben1998) concluded that PEPPI may be useful in measuring the impact of interventions designed to increase older patients’ personal sense of effectiveness in obtaining needed health care. For example, it was used in a study in the Netherlands, which showed that self-efficacy was significantly correlated with patients’ satisfaction after physician encounters in primary care (Zandbelt et al., Reference Zandbelt, Smets, Oort, Godfried and De Haes2004). It was also used in a study showing that in low-income patients with prostate cancer, low self-efficacy for interacting with physicians was best predicted by diminished overall satisfaction with care, low confidence in providers and worse symptom distress (Maliski et al., Reference Maliski, Kwan, Krupski, Fink, Orecklin and Litwin2004). Men with low self-efficacy fared worse over a range of psychosocial outcomes and both general and disease-specific health-related quality of life. It was also used to measure differences in self-efficacy between racial groups in a study looking at a public assistance programme for prostate cancer (Miller et al., Reference Miller, Gelberg, Kwan, Stepanian, Fink, Andersen and Litwin2008). This self-efficacy score was also used in a tailored education and coaching intervention to enhance care of cancer-related pain, as part of the Cancer Health Empowerment for Living without Pain study (Kravitz et al., Reference Kravitz, Tancredi, Street, Kalauokalani, Grennan, Wun, Slee, Evans Dean, Lewis, Saito and Franks2009).
There appears to be very few other scales focussing on measuring self-efficacy in doctor–patient interactions. We used the five-point PEPPI scale because it was relatively brief and focussed on the doctor–patient interaction.
Data analysis
Data from the HRA-O questionnaires were entered on a database designed for the study, with double data entry for purposes of quality control, and analysed in a two-stage process using SPSS 12 for Windows. In the first stage of the analysis, χ 2 tests were used to explore the associations between higher self-efficacy on the PEPPI scale and the characteristics listed in Table 2. Social isolation was measured according to the Lubben Social Network scale (Lubben, Reference Lubben1988; Lubben et al., Reference Lubben, Blozik, Gillmann, Iliffe, von Renteln-Kruse, Beck and Stuck2006), and physical activity by the Physical Activity Scale for the Elderly score (Washburn et al., Reference Washburn, Smith, Jette and Janney1993). Other factors included were history of falls (Kelsey et al., Reference Kelsey, Browner, Seeley, Nevitt and Cummings1992), assistance with more than one Lawton's Instrumental Activities of Daily Living (Lawton and Brody, Reference Lawton and Brody1969), self-reported functional change (Fried et al., Reference Fried, Bandeen-Roche, Chaves and Johnson2000), more service utilisation (more than six visits to the doctor in the last 12 months) and polypharmacy (on four or more repeat medications). We included questions on how recently patients had had blood pressure measurements, cholesterol checks and random blood glucose tests to evaluate uptake of preventive care.
In the second stage of the analysis, the variables with a significant association (other than uptake of preventive care activities and dietary factors) were entered in a single forward step into a binary logistic regression model.
Results
In all, 5982 patients aged 65 years and over were identified across the three practices, of which 515 were excluded based on the exclusion criteria. In 2000, 5467 older people were sent an invitation letter, a consent form and the questionnaire. In 2002, 2989 participants were sent the HRA-O questionnaire containing the PEPPI scale, and 81% returned them. Of these, 2320 (78%) completed all five PEPPI scale questions. Those who answered none or only some PEPPI questions were not significantly different from those who completed all five PEPPI questions in age or sex.
Responses to the PEPPI questions
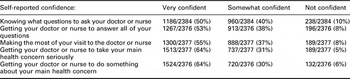
Responses to each of the PEPPI questions are shown in Table 1.
Table 1 Responses to each of the PEPPI questions
Analysis of PEPPI scores
The mean total PEPPI score was 20, with a median of 21 and a standard deviation of 5.383. The distribution of PEPPI scores was bimodal, peaking at 15 and 25. One in three (36%) of those who completed the PEPPI scale had scores of 15 or below, which for the purposes of analysis we categorised as ‘lower self-efficacy’. Scores of 16 or more were categorised as ‘higher self-efficacy’. There were 835 people in the lower self-efficacy category and 1485 in the higher self-efficacy category.
First stage analysis
Table 2 shows the associations between the chosen HRA-O domains and higher self-efficacy as measured by the PEPPI scale. Higher self-efficacy was significantly less likely among women, those with only basic education, and those living alone. Service utilisation (frequent doctor visits), polypharmacy and most lifestyle characteristics (smoking, hazardous alcohol consumption, dietary habits) were not significantly associated with higher or lower self-efficacy. However, those who reported having an unhealthy diet with low fruit and fibre content were less likely to have higher self-efficacy. Those reporting impaired functional ability, fear of falling and low physical activity levels were also less likely to have high self-efficacy scores. Multiple falls in the previous 12 months were unrelated to self-efficacy levels. Participants in this study were significantly less likely to have a higher self-efficacy in doctor–patient interactions if they had depressed mood, reported memory problems or were at risk of social isolation.
Table 2 Factors associated with higher self-efficacy: bivariate analysis n = 1485
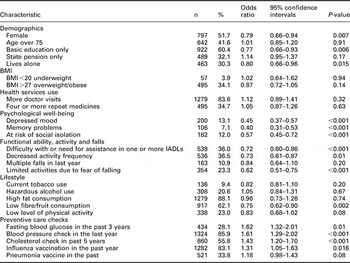
BMI = body mass index; IADL = instrumental activities of daily living.
Second stage analysis
The likelihood of having higher self-efficacy in doctor–patient interactions remained significantly negatively associated with memory problems, low mood, risk of social isolation and limitation of activities due to fear of falling, after adjustment for age, gender and years in education (see Table 3). Functional losses were no longer significantly associated with self-efficacy.
Table 3 Correlation of lower self-efficacy with selected factors significantly associated in bivariate analyses: results of multivariate logistic regression analysis
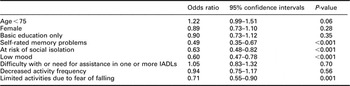
IADL = instrumental activities of daily living.
Those with higher self-efficacy were significantly more likely to have had recent measurements of BP, cholesterol and fasting blood glucose, and influenza immunisation.
Discussion
To the best of our knowledge, this is the first study of self-efficacy in doctor–patient interaction in older people in British general practice. Two-thirds of this sample of older people had PEPPI scores suggesting higher self-efficacy, and they were significantly more likely to have had recent measurements of blood pressure, cholesterol and fasting blood glucose, and influenza immunisation. A third had lower self-efficacy, and there were significant associations between having low self-efficacy and having poor self-rated memory, only basic education, limitation of activities due to fear of falling, being at risk of social isolation and having depressed mood.
Our hypothesis that lower self-efficacy would be associated with fewer years in education and lower uptake of preventive care was supported by the findings of the bivariate analyses, but not in the logistic regression analysis. The expected association of lower self-efficacy with lower income was not supported. The prediction that self-efficacy in doctor–patient interactions would be independent of other demographic and functional characteristics was supported by the findings from the logistic regression analysis. The relationship between depression and self-efficacy needs further exploration in longitudinal studies, to allow causality to be determined, for it is possible that low confidence is the product of depression, not a cause. The possibility that self-efficacy mediates between impairments or disability and depression also needs further investigation. The extent to which self-efficacy in doctor–patient interactions is modifiable needs to be evaluated, and this may require improved methods for measuring self-efficacy in primary care.
Limitations of the study
Owing to the cross-sectional nature of the data, it is not possible to determine causality in the relationships between self-efficacy and the factors associated with it. The sample was drawn from three general practices in suburban London, and subject to eligibility criteria and disability screening implemented for recruitment into a trial of health promotion, which may limit the generalisability of the results. The distribution of self-efficacy scores found in this sample may be different from that in the general population of older primary care patients, partly because we deliberately excluded disabled older people, people needing assistance with basic activities of daily living, and people with mental health problems and dementia, and partly because the participants were a self-selecting sub-group who returned lengthy questionnaires. We cannot comment on those who did not choose to participate in the questionnaire study. The results showed a bimodal distribution of results, which again cannot be explained, but may need further study to evaluate its significance. Finally, self-report of diagnoses and of preventive care uptake may be inaccurate.
Comparison with existing literature
There are no published studies with regard to self-efficacy in doctor–patient interactions in the older people. The association between depressed mood and low self-efficacy has been noted in other studies, although is not a dominant theme in the discussion of self-efficacy as a modifiable determinant of health. For example, in a study of adherence to antihypertensive medication in African Americans, depressive symptoms were associated with poor medication adherence and low self-efficacy (Schoenthaler et al., Reference Schoenthaler, Ogedegbe and Allegrante2007) but this relationship became non-significant when controlling for self-efficacy. The authors saw self-efficacy as having a mediating role between depression and medication adherence. In US studies, a similar mediating role has also been found between limited social support and depression (Holahan and Holahan, Reference Holahan and Holahan1987), and between pain intensity and disability (Arnstein et al., Reference Arnstein, Caudill, Mandle, Norris and Beasley1999).
Another way of thinking about self-efficacy is shown by a study of patients with heart failure in which patients were characterised as ‘experts’, ‘novices’ and ‘inconsistent’ in a recent self-care management study in the United States (Dickson et al., Reference Dickson, Deatrick and Riegel2008). ‘Experts’ had experience and skill in self-care, which novices lacked, and positive attitudes with self-efficacy that aligned with their behaviours. Most patients (71%) were classified as ‘inconsistent’, a self-care type associated with impaired cognition, poor physical functioning, negative attitudes and poor self-efficacy. Our findings are strikingly similar in the associations between lower self-efficacy and memory problems, low mood and fear of falling.
Implications for clinical practice and future research
Improving self-efficacy in any aspect of health is no panacea. The concept and much of the clinical practice based on fostering self-efficacy has been part of health care for twenty years, and (with some exceptions such as diabetes, arthritis and asthma management) have had limited impact on health behaviours. For example, in a recent Canadian study designed to increase self-efficacy in balance and mobility, both resistance training and agility training significantly improved balance confidence by a modest 6% from baseline after 13 weeks (Liu-Ambrose et al., Reference Liu-Ambrose, Khan, Eng, Lord and McKay2004). The change in balance confidence was only weakly correlated with improved general physical function and not significantly correlated with the changes in fall risk score, postural stability, gait speed or physical activity level. The authors also observed enhanced confidence in balance in people whose falls risk increased or physical abilities deteriorated. Our paper identifies characteristics that suggest that an older person will be less likely to have confidence in their interactions with doctors and their health, so that theoretically this subgroup of patients could benefit from interventions to improve their self-efficacy. However, even with approaches designed to enhance self-efficacy, changing behaviour through professional intervention remains difficult (Borsody et al., Reference Borsody, Courtney, Taylor and Jaraith1999).
Conclusion
A third of older people in this study had low self-efficacy in doctor–patient interactions, and they appeared to be a vulnerable group. The population prevalence of lower self-efficacy in doctor–patient interactions may be larger. Low mood and poor memory are both symptoms of depression, and limitation of activity because of the fear of falling has a psychological component independent of the experience of falling. In this population of older people, low self-efficacy in interactions with doctors (as measured by the PEPPI scale) may be a symptom of depression, or a characteristic of older people who also experience social isolation and depression. Understanding a person's confidence in doctor–patient interactions as measured by self-efficacy may be useful in clinical practice, but policies that depend on enhancing self-care and self-management need to consider the large number of older people with low self-efficacy in using medical services. Further studies looking at whether self-efficacy in doctor–patient interactions is modifiable and improvable may be useful.
Acknowledgements
Local research ethics committee approval was obtained from Brent Medical Ethics Committee (BEC745) and King's College Hospital Research Ethics Committee (Protocol 01-010). This study was funded by the European Commission project QLK6-CT-1999-02205 and the Federal Education Science Ministry, Berne, Switzerland BBW 990311.1. The authors have no conflict of interest to declare. The authors thank the practices and patients involved in the study.





