Spousal bereavement is a life-altering event that is associated with disruption in everyday life and changes in routine health behaviors (Stahl and Schulz, Reference Stahl and Schulz2014). Changes in routine health behaviors may place bereaved individuals at risk for mood disorders like major depressive disorder (MDD) because they disrupt the stability of the body’s circadian rhythm.
We performed a preliminary exploration of whether accelerometer-based rhythm measures differ between older spousally bereaved adults (M age = 70 years) and age- and sex-matched married controls (M age = 68 years); and whether any rhythm differences were associated with depression symptom severity in bereavement. From accelerometry recordings, we examined rest-activity rhythm (RAR) measures, which quantify different aspects of the 24-hour activity pattern including timing, regularity, and amplitude. Past research demonstrates that RAR measures correlate with depression symptoms and may also contribute to MDD (Smagula, Reference Smagula2016; Smagula et al., Reference Smagula, Krafty, Thayer, Buysse and Hall2018).
Using linear regression, we assessed the effect sizes of differences in RAR measures between the bereaved and non-bereaved sample (Figure 1). These models examined the effect of group (bereaved vs. non-bereaved) adjusted for age to ensure associations were not due to residual age differences. If RAR characteristics differed between the bereaved and non-bereaved samples, we then examined their associations with depression symptom severity (using the Hamilton [Reference Hamilton1960] Rating Scale for Depression) in bereaved individuals using Pearson correlations.
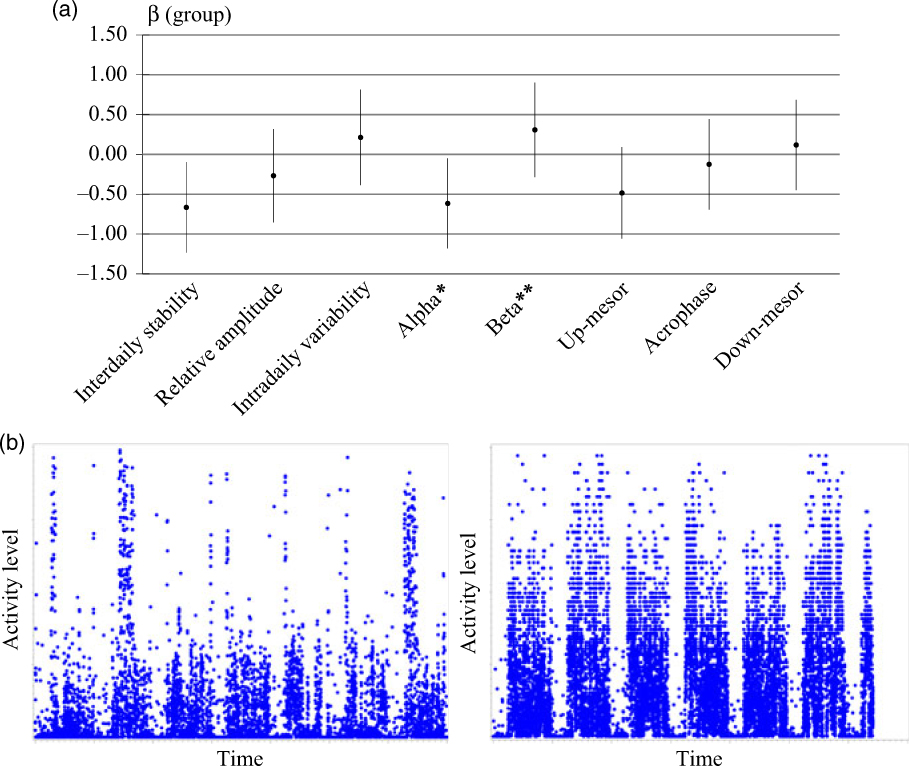
Figure 1. (a) Age-adjusted coefficients indicating group rest-activity (RAR) differences and (b) a week of recording from participants with low (left) and high (right) inter-daily stability. Note: age-adjusted coefficients (95% confidence intervals) shown with negative values indicating the RAR metric is lower in the bereaved compared to the non-bereaved sample.
We found that inter-daily stability of the RAR, an objective measure of the extent to which the activity patterns are stable across days, was lower in bereaved elders compared with married controls (β = −0.66, standard error [SE] = 0.28, p = 0.02). Bereaved elders commonly report fragmented sleep, irregular physical activity, and meal skipping; these behaviors likely contribute to a less stable circadian rhythm. Inter-daily stability was correlated with depression symptoms where bereaved elders with less stable circadian rhythms reported more depression symptom burden (r = −0.36, p = 0.03). In light of evidence that sub-syndromal symptoms predict progression to MDD (Cuijpers and Smit, Reference Cuijpers and Smit2004), these findings suggest that low inter-daily stability may contribute to the increased depression risk in bereaved elders.
We also found that bereaved elders “got going” earlier than married controls, resulting in a relatively longer period of activity compared with rest (β = −0.62, SE = 0.28, p = 0.03). Bereaved elders may have longer periods of activity compared to married controls because intrusive thoughts and trouble sleeping in the bed they once shared with their partner prompts them to get up instead of trying to return to sleep. Getting out of bed and starting the day may serve as a distraction from the circulating thoughts and emotions that are common following spousal bereavement. The relatively longer active periods we found in bereaved individuals indicates that future research is needed to address whether a shorter resting period (and shorter sleep) contributes to the burden of depression during bereavement.
Our findings provide preliminary evidence that inter-daily stability could serve as an objective target for decreasing depression symptoms in older spousally bereaved adults. Future longitudinal and intervention efforts are needed to investigate whether maintaining a stable behavioral pattern across days reduces depression in the wake of spousal bereavement.
Conflicts of interest
None.
Description of author’s roles
STS and SFS conceived and designed the study. SFS completed the statistical analysis. STS, SFS, and MHH contributed to writing the paper.
Acknowledgments
This work was supported in part by Grants from the National Institute of Mental Health (K01MH103467, K01MH112683, and P30MH90333), the National Heart, Lung, and Blood Institute (R01 HL104607), and the Clinical and Translational Science Institute (UL1 TR000005).



