To the Editor—Healthcare workers (HCWs) are encouraged to wear gloves by the WHO in the direct care of the patients during the COVID-19 pandemic. Medical gloves are made of different polymers, including latex, nitrile rubber, polyvinyl chloride, polyurethane, and neoprene. Nitrile and latex gloves are preferred during the COVID-19 pandemic due to better durability. Reference Kwon, Ko, Shin, Sung and Kim1 Latex gloves are flexible, fit well, are sensitive to touch, and provide moderate protection. Reference Chen, Shang, Yao, Liu and Liu2 Vinyl gloves provide moderate protection, are sensitive to touch, but are not as durable. Reference Chen, Shang, Yao, Liu and Liu2 However, nitrile gloves are chemical- and puncture-resistant and provide the highest level of protection and durability. Reference Chen, Shang, Yao, Liu and Liu2 Many adverse skin reactions, including irritant contact dermatitis, allergic contact dermatitis, and contact urticaria have been reported with the use of all types of gloves. Reference Alenius, Turjanmaa and Palosuo3
Latex gloves are frequently used among HCWs. Hypersensitivity to natural rubber latex (NRL) has been increasingly reported, with an incidence of 2.8% to 17% among HCWs. Reference Alenius, Turjanmaa and Palosuo3 HCWs are highly at risk of developing allergic reactions to NRL, especially operating room personnel, dental assistants, laboratory personnel, hospital housekeeping personnel, and ambulance attendants. Reference Taylor and Erkek4 Atopic background, history of hand dermatitis, allergy to certain foods, female gender, and multiple exposures are among the risk factors for developing hypersensitivity to NRL. Reference Alenius, Turjanmaa and Palosuo3 Hypersensitivity reaction to bananas, avocados, chestnuts, kiwis, and other fruits have been reported among these patients. Reference Bolognia, Schaffer and Cerroni5 Skin reactions include localized pruritus, burning, stinging, contact and generalized urticaria. The most frequently observed reaction is irritant contact dermatitis presenting as dry, crusted, fissuring patches. Reference Taylor and Erkek4 In suspected patients, a thorough history of allergic reactions to balloons, gloves, barium enema, and other latex devices should be taken. The gold standard in the diagnosis is skin-prick testing in patients with localized symptoms and latex-specific IgE antibody assessment in cases of systemic symptoms. Reference Bolognia, Schaffer and Cerroni5 However, the wear and/or use test and the patch test are the alternative diagnostic tests. Reference Taylor and Erkek4 The most effective approach for the management of latex allergy is personal and environmental avoidance by considering hypoallergic gloves. Reference Taylor and Erkek4
Recommendations for the prevention of allergic reactions to gloves are summarized in Fig. 1. Urticaria can be treated with antihistamines and the elimination of the antigen. H1,2 Blockers can be used before coming into contact with latex devices; however, latex avoidance is superior to this protocol. Reference Taylor and Erkek4
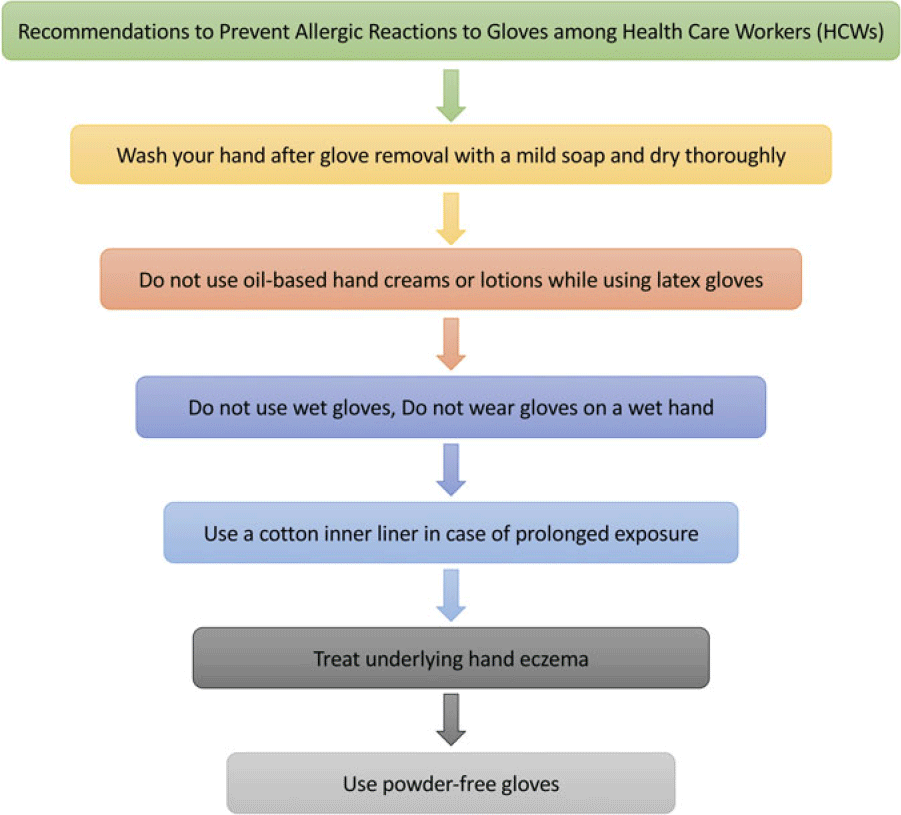
Fig. 1. Recommendations to prevent allergic reactions to gloves among healthcare workers.
Plastic gloves, considered as hypoallergenic polyvinylchloride (PVC) gloves, are also used among HCWs. Contact allergic reaction to PVC has also been reported as a result of allergy to many additives used in these gloves, including carba mix, mercaptobenzothiazole (MBT), thiuram mix, mixed dialkyl thioureas, and black rubber mix. Reference Bolognia, Schaffer and Cerroni5 Allergic contact dermatitis has been reported in numerous case reports. Lesions may also become generalized in some patients. A patch test can be used to confirm the diagnosis. Topical corticosteroids are considered as the best choice of treatment; however, patients should be advised to use other types of gloves, Reference Bolognia, Schaffer and Cerroni5 although allergic contact dermatitis may coexist with immediate hypersensitivity to Latex. Reference Bolognia, Schaffer and Cerroni5
Nitrile, neoprene, and polyurethane are also used in plastic gloves. Hand dermatitis has been reported with these types of materials. The patch test is recommended in suspicious cases. Application of topical and oral steroids can mitigate the symptoms but the benefits should be weighed against the risks of side effects. Reference Dooms‐Goossens, Bruze, Buysse, Fregert, Gruvberger and Stals6
Glove-related hand urticaria should also be considered as a differential diagnosis; it is caused by dermographism upon the application of the glove. Pain, burning, and pruritus in the affected area, and systemic symptoms such as fever are not present in glove-related hand urticaria. Further, nitrile gloves are more likely to cause this phenomenon because they are rigid and less flexible. Reference Hawkey and Abdul Ghaffar7
Some types of powder used in gloves have been associated with an increased risk of skin roughness due to altering glove pH. Reference Brehler, Voss and Muller8 Glove powder has been reported to cause allergic reactions, and hand eczema has been reported to decrease significantly after using powder-free gloves. Reference Edelstam, Arvanius and Karlsson9 Thus, the use of powder-free gloves is recommended in the current pandemic situation. HCWs are also encouraged to wear double gloves when handling COVID-19 patients’ airways, blood, urine, and other body fluids. The outer glove should be the first equipment to be removed. Reference Chen, Shang, Yao, Liu and Liu2
Acknowledgments
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.




