Significant outcomes
-
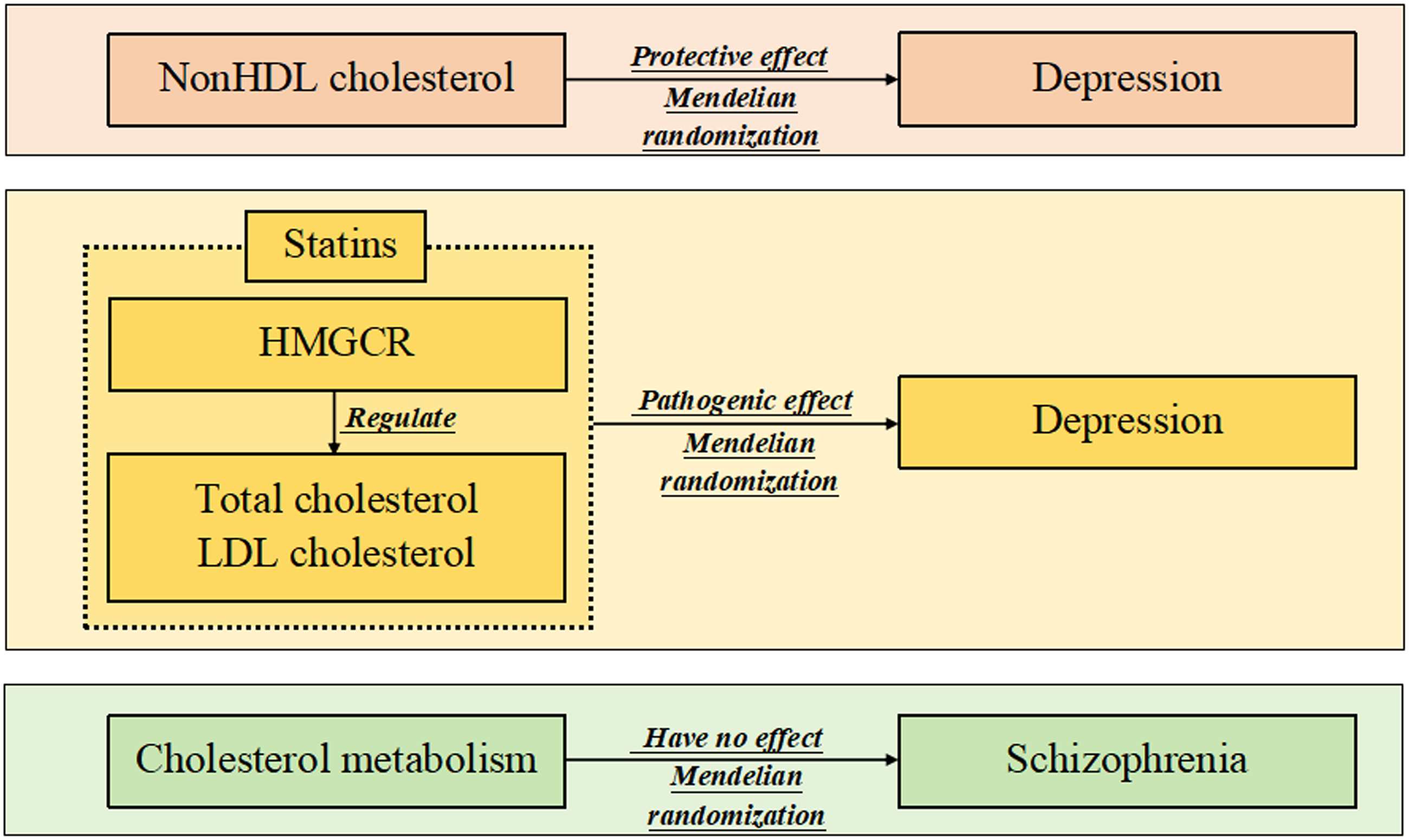
Mendelian randomisation is used to explore the relationship between cholesterol metabolism and psychological disorders for the first time.
-
NonHDL cholesterol genetically relieves depression, while statins may unexpectedly contribute to the disease.
-
These findings help to understand the pathogenesis of depression and identify new therapeutic targets for the disease.
Limitations
-
Depending on the purpose of the study, there are not many types of blood lipids and psychological disorders involved in this study.
-
The study adopts a commonly used drug-targeted Mendelian randomisation method to explore the association of the HMGCR gene with depression and schizophrenia, but due to data limitations, the study does not use another drug-targeted method called summary-data-based Mendelian randomisation.
Introduction
Mental and psychological disorders have become major health challenges in the human population. At present, depression is the most common psychological disorder worldwide, affecting 280 million people, while schizophrenia, another serious mental illness, affects approximately 24 million people (Ettman et al., Reference Ettman, Abdalla, Cohen, Sampson, Vivier and Galea2020; Mojtabai, Reference Mojtabai2021; Subramaniam et al., Reference Subramaniam, Abdin, Vaingankar, Sambasivam, Zhang, Shafie, Basu, Chan, Tan, Verma, Tang, Chua, Heng and Chong2021; Hu et al., Reference Hu, Zhao, Wu, Li, Luo, Yang and Yang2022). More importantly, these disorders significantly affect patients’ ability to work and quality of life and can lead to disability and even suicide in severe cases (Bai et al., Reference Bai, Liu, Jiang, Zhang, Rao, Cheung, Hall and Xiang2021; Jin, Reference Jin2022). Therefore, it is crucial to explore risk factors and potential therapies for depression and schizophrenia.
Although somewhat surprising, the available evidence does suggest that lipid metabolism (including cholesterol metabolism) is associated with these mental and psychological disorders. For example, two observational studies reported that adverse lipoprotein patterns were detected in patients with major depressive depression, and several diagnostic potential biomarkers comprising lipids can distinguish patients with this disease from healthy controls, revealing that lipidomics might be a potential tool for depression investigation (van Reedt Dortland et al., Reference van Reedt Dortland, Giltay, van Veen, van Pelt, Zitman and Penninx2010; Zhang et al., Reference Zhang, Guo, Li, Wang, Yang, Yang, Cui, Zhou, Chen, Yu, Peng and Tan2022). One Mendelian randomisation (MR) analysis confirmed a causal relationship between triglycerides and altered cholesterol levels and depression traits for the first time, although it had a relatively small sample size (So et al., Reference So, Chau, Cheng and Sham2021). In addition, one recent review concluded that increased serum lipids may be associated with the remission of schizophrenia symptoms during treatment, and another meta-analysis suggested that some schizophrenic patients with reduced lipids were more likely to develop suicidal tendencies (Kim et al., Reference Kim, Barr, Fredrikson, Honer and Procyshyn2019; Sankaranarayanan et al., Reference Sankaranarayanan, Pratt, Anoop, Smith, Espinoza, Ramachandran and Tirupati2021).
The effects of hydroxymethylglutaryl coenzyme A (HMG-CoA) reductase inhibitors (namely, statins), the most commonly used cholesterol-lowering drugs, on the risk of depression and schizophrenia have also been explored (Sirtori et al., Reference Sirtori, Manzoni and Lovati1991). Briefly, one population-based cohort study suggested that administration of the drug may have reduced the risk of depression, but a meta-analysis including 13 observational studies did not support this finding (Molero et al., Reference Molero, Cipriani, Larsson, Lichtenstein, D.’Onofrio and Fazel2020; Lee et al., Reference Lee, Peng, Lee, Wang, Lee, Chen and Shiang2021). Another meta-analysis clarified that adjunctive therapy with statins could improve schizophrenia symptoms, either negative or positive (Andrade, Reference Andrade2018; Shen et al., Reference Shen, Li, Yan, Zhou, Feng, Zhao and Xiao2018).
It is important to note that the above findings are mainly from observational studies, which are susceptible to confounding factors and causal inversions. Compared with this type of study, MR studies can apply genetic variants to replace exposures and outcomes of interest, enabling causal inference at the genetic level and providing more reliable results (Emdin et al., Reference Emdin, Khera and Kathiresan2017; Birney, Reference Birney2022).
Considering that cholesterol metabolism is one of the main components of lipid metabolism and that statins are the most commonly used cholesterol-lowering drugs, this study explored the effects of peripheral cholesterol traits and statin use on depression, schizophrenia and suicide attempts using traditional MR and drug-targeted MR methods.
Methods
Ethical requirements
This study was approved by the ethics committee of Tianjin Haihe Hospital. The summary data used in this study were obtained from publicly available databases, and the providers of these data were also approved by the local ethics committees.
Study design
This study was divided into traditional MR and drug-targeted MR sections.
In the former section, the study adopted three MR methods [i.e., random-effected inverse variance weighted (IVW), Mendelian randomisation pleiotropy residual sum and outlier (MR-PRESSO) and MR–Egger] to investigate the effects of four cholesterol traits [i.e., total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C) and nonHDL-C] on the risk of depression, schizophrenia and suicide attempts. Suicide attempts are the most serious consequence of mental and psychological disorders and were therefore included in the study (Bai et al., Reference Bai, Liu, Jiang, Zhang, Rao, Cheung, Hall and Xiang2021; Jin, Reference Jin2022). Instrumental variables predicting these cholesterol traits were extracted from corresponding genome-wide association studies (GWASs).
In the latter section, the study also adopted these three MR methods to examine the effects of two cholesterol traits (TC and LDL-C) mediated by the 3-hydroxy-3-methylglutaryl coenzyme A reductase (HMGCR) gene, which is the target gene for statins, on the three outcomes (Sirtori et al., Reference Sirtori, Manzoni and Lovati1991). TC and LDL-C are the main effectors of statins (Sirtori et al., Reference Sirtori, Manzoni and Lovati1991). When instrumental variables for these two cholesterol traits are also spatially related to the HMGCR gene on the chromosome, the use of statins can be predicted.
A series of sensitivity analyses were conducted on both the traditional and drug-target sections to assess the validity of the instrumental variables, determine heterogeneity and horizontal pleiotropy, and detect possible confounding factors.
An overview of this study is also provided in Table 1.
Table 1. Overview and process of the study

MR, Mendelian randomisation; SNP, Single nucleotide polymorphism; LD, Linkage disequilibrium; MAF, Minor allele frequency; IVW, Inverse variance weighted; MR-PRESSO, Mendelian randomisation pleiotropy RESidual sum and outlier.
Summary data
The summary depression data were obtained from the UK Biobank (UKB) and Psychiatric Genomics Consortium (PGC) (excluding 23andme) cohorts, which included 170,756 cases and 329,443 controls (Howard et al., Reference Howard, Adams, Clarke, Hafferty, Gibson, Shirali, Coleman, Hagenaars, Ward, Wigmore, Alloza, Shen, Barbu, Xu, Whalley, Marioni, Porteous, Davies, Deary, Hemani, Berger, Teismann, Rawal, Arolt, Baune, Dannlowski, Domschke, Tian, Hinds, Trzaskowski, Byrne, Ripke, Smith, Sullivan, Wray, Breen, Lewis and McIntosh2019). All cohort members were of European descent, and the dataset included both males and females. There were three types of depression phenotypes in this dataset, i.e., broad depression, major depressive disorder, and the international classification of disease (ICD)-coded major depressive disorder phenotype. The definitions of these phenotypes were determined by answering specific questions and reviewing ICD codes, the details of which are presented in Supplemental Table 1. The questions were ‘Have you ever seen a general practitioner for nerves, anxiety, tension or depression?’ and ‘Have you ever seen a psychiatrist for nerves, anxiety, tension or depression?’ Patients with other psychiatric disorders (such as bipolar disorder and schizophrenia) were excluded.
The data for schizophrenia were collected from a PGC two-stage GWAS using 52,017 cases and 75,889 controls (Trubetskoy et al., Reference Trubetskoy, Pardiñas, Qi, Panagiotaropoulou, Awasthi, Bigdeli, Bryois, Chen, Dennison, Hall, Lam, Watanabe, Frei, Ge, Harwood, Koopmans, Magnusson, Richards, Sidorenko, Wu, Zeng, Grove, Kim, Li, Voloudakis, Zhang, Adams, Agartz, Atkinson, Agerbo, Al Eissa, Albus, Alexander, Alizadeh, Alptekin, Als, Amin, Arolt, Arrojo, Athanasiu, Azevedo, Bacanu, Bass, Begemann, Belliveau, Bene, Benyamin, Bergen, Blasi, Bobes, Bonassi, Braun, Bressan, Bromet, Bruggeman, Buckley, Buckner, Bybjerg-Grauholm, Cahn, Cairns, Calkins, Carr, Castle, Catts, Chambert, Chan, Chaumette, Cheng, Cheung, Chong, Cohen, Consoli, Cordeiro, Costas, Curtis, Davidson, Davis, de Haan, Degenhardt, DeLisi, Demontis, Dickerson, Dikeos, Dinan, Djurovic, Duan, Ducci, Dudbridge, Eriksson, Fañanás, Faraone, Fiorentino, Forstner, Frank, Freimer, Fromer, Frustaci, Gadelha, Genovese, Gershon, Giannitelli, Giegling, Giusti-Rodríguez, Godard, Goldstein, González Peñas, González-Pinto, Gopal, Gratten, Green, Greenwood, Guillin, Gülöksüz, Gur, Gur, Gutiérrez, Hahn, Hakonarson, Haroutunian, Hartmann, Harvey, Hayward, Henskens, Herms, Hoffmann, Howrigan, Ikeda, Iyegbe, Joa, Julià, Kähler, Kam-Thong, Kamatani, Karachanak-Yankova, Kebir, Keller, Kelly, Khrunin, Kim, Klovins, Kondratiev, Konte, Kraft, Kubo, Kučinskas, Kučinskiene, Kusumawardhani, Kuzelova-Ptackova, Landi, Lazzeroni, Lee, Legge, Lehrer, Lencer, Lerer, Li, Lieberman, Light, Limborska, Liu, Lönnqvist, Loughland, Lubinski, Luykx, Lynham, Macek, Mackinnon, Magnusson, Maher, Maier, Malaspina, Mallet, Marder, Marsal, Martin, Martorell, Mattheisen, McCarley, McDonald, McGrath, Medeiros, Meier, Melegh, Melle, Mesholam-Gately, Metspalu, Michie, Milani, Milanova, Mitjans, Molden, Molina, Molto, Mondelli, Moreno, Morley, Muntané, Murphy, Myin-Germeys, Nenadić, Nestadt, Nikitina-Zake, Noto, Nuechterlein, O’Brien, O’Neill, Oh, Olincy, Ota, Pantelis, Papadimitriou, Parellada, Paunio, Pellegrino, Periyasamy, Perkins, Pfuhlmann, Pietiläinen, Pimm, Porteous, Powell, Quattrone, Quested, Radant, Rampino, Rapaport, Rautanen, Reichenberg, Roe, Roffman, Roth, Rothermundt, Rutten, Saker-Delye, Salomaa, Sanjuan, Santoro, Savitz, Schall, Scott, Seidman, Sharp, Shi, Siever, Sigurdsson, Sim, Skarabis, Slominsky, So, Sobell, Söderman, Stain, Steen, Steixner-Kumar, Stögmann, Stone, Straub, Streit, Strengman, Stroup, Subramaniam, Sugar, Suvisaari, Svrakic, Swerdlow, Szatkiewicz, Ta, Takahashi, Terao, Thibaut, Toncheva, Tooney, Torretta, Tosato, Tura, Turetsky, Üçok, Vaaler, van Amelsvoort, van Winkel, Veijola, Waddington, Walter, Waterreus, Webb, Weiser, Williams, Witt, Wormley, Wu, Xu, Yolken, Zai, Zhou, Zhu, Zimprich, Atbaşoğlu, Ayub, Benner, Bertolino, Black, Bray, Breen, Buccola, Byerley, Chen, Cloninger, Crespo-Facorro, Donohoe, Freedman, Galletly, Gandal, Gennarelli, Hougaard, Hwu, Jablensky, McCarroll, Moran, Mors, Mortensen, Müller-Myhsok, Neil, Nordentoft, Pato, Petryshen, Pirinen, Pulver, Schulze, Silverman, Smoller, Stahl, Tsuang, Vilella, Wang, Xu, Wenwen, Wildenauer, Agiananda, Amir, Antoni, Arsianti, Asmarahadi, Diatri, Djatmiko, Irmansyah, Khalimah, Kusumadewi, Kusumaningrum, Lukman, Nasrun, Safyuni, Prasetyawan, Semen, Siste, Tobing, Widiasih, Wiguna, Wulandari, Evalina, Hananto, Ismoyo, Marini, Henuhili, Reza, Yusnadewi, Akbarian, Ashley-Koch, van Bakel, Breen, Brown, Bryois, Carlyle, Charney, Coetzee, Crawford, Dracheva, Emani, Farnham, Fromer, Galeev, Gandal, Gerstein, Giase, Girdhar, Goes, Grennan, Gu, Guerra, Gursoy, Hoffman, Hyde, Jaffe, Jiang, Jiang, Kefi, Kim, Kitchen, Knowles, Lay, Lee, Li, Liu, Liu, Mattei, Navarro, Pan, Peters, Pinto, Pochareddy, Polioudakis, Purcaro, Purcell, Pratt, Reddy, Rhie, Roussos, Rozowsky, Sanders, Sestan, Sethi, Shi, Shieh, Swarup, Szekely, Wang, Warrell, Weissman, Weng, White, Wiseman, Witt, Won, Wood, Wu, Xu, Yao, Zandi, Bakker, Bender, Bramon, Collier, Crepo-Facorro, Hall, Iyegbe, Kahn, Lawrie, Lewis, Lin, Linszen, Mata, McIntosh, Murray, Ophoff, van Os, Powell, Rujescu, Walshe, Weisbrod, Andres-Alonso, Bagni, Bayés, Biederer, Brose, Brown, Chua, Coba, Cornelisse, de Jong, de Juan-Sanz, Dieterich, Feng, Goldschmidt, Gundelfinger, Hoogenraad, Huganir, Hyman, Imig, Jahn, Jung, Kaeser, Kim, Koopmans, Kreutz, Lipstein, MacGillavry, Malenka, McPherson, O’Connor, Pielot, Ryan, Sahasrabudhe, Sala, Sheng, Smalla, Smit, Südhof, Thomas, Toonen, van Weering, Verhage, Verpelli, Adolfsson, Arango, Baune, Belangero, Børglum, Braff, Bramon, Buxbaum, Campion, Cervilla, Cichon, Collier, Corvin, Curtis, Forti, Domenici, Ehrenreich, Escott-Price, Esko, Fanous, Gareeva, Gawlik, Gejman, Gill, Glatt, Golimbet, Hong, Hultman, Hyman, Iwata, Jönsson, Kahn, Kennedy, Khusnutdinova, Kirov, Knowles, Krebs, Laurent-Levinson, Lee, Lencz, Levinson, Li, Liu, Malhotra, Malhotra, McIntosh, McQuillin, Menezes, Morgan, Morris, Mowry, Murray, Nimgaonkar, Nöthen, Ophoff, Paciga, Palotie, Pato, Qin, Rietschel, Riley, Rivera, Rujescu, Saka, Sanders, Schwab, Serretti, Sham, Shi, St Clair, Stefánsson, Stefansson, Tsuang, van Os, Vawter, Weinberger, Werge, Wildenauer, Yu, Yue, Holmans, Pocklington, Roussos, Vassos, Verhage, Visscher, Yang, Posthuma, Andreassen, Kendler, Owen, Wray, Daly, Huang, Neale, Sullivan, Ripke, Walters, O’Donovan, van Amelsvoort, van Winkel, Gareeva, Sham, Shi, St Clair and van Os2022). They cohort members all from the European population, and the dataset included both sexes. Patients were diagnosed with schizophrenia based on their typical symptoms and treatment history. The data for suicide attempts were obtained from a Neale laboratory GWAS using the UKB population. The GWAS enrolled 2,658 cases and 2,275 controls, all of which were European individuals and included males and females. These data were downloaded directly from the IEU Open GWAS Project (https://gwas.mrcieu.ac.uk/), and the dataset ID was ukb-d-20483.
The summary data for obesity and coronary heart disease (CHD) were obtained from two FinnGen cohorts using 342,400 and 342,499 European individuals (including males and females) (Kurki et al., Reference Kurki, Karjalainen, Palta, Sipilä, Kristiansson, Donner, Reeve, Laivuori, Aavikko, Kaunisto, Loukola, Lahtela, Mattsson, Laiho, Della Briotta Parolo, Lehisto, Kanai, Mars, Rämö, Kiiskinen, Heyne, Veerapen, Rüeger, Lemmelä, Zhou, Ruotsalainen, Pärn, Hiekkalinna, Koskelainen, Paajanen, Llorens, Gracia-Tabuenca, Siirtola, Reis, Elnahas, Sun, Foley, Aalto-Setälä, Alasoo, Arvas, Auro, Biswas, Bizaki-Vallaskangas, Carpen, Chen, Dada, Ding, Ehm, Eklund, Färkkilä, Finucane, Ganna, Ghazal, Graham, Green, Hakanen, Hautalahti, Hedman, Hiltunen, Hinttala, Hovatta, Hu, Huertas-Vazquez, Huilaja, Hunkapiller, Jacob, Jensen, Joensuu, John, Julkunen, Jung, Junttila, Kaarniranta, Kähönen, Kajanne, Kallio, Kälviäinen, Kaprio, Kettunen, Kilpeläinen, Kilpi, Klinger, Kosma, Kuopio, Kurra, Laisk, Laukkanen, Lawless, Liu, Longerich, Mägi, Mäkelä, Mäkitie, Malarstig, Mannermaa, Maranville, Matakidou, Meretoja, Mozaffari, Niemi, Niemi, Niiranen, O´Donnell, Obeidat, Okafo, Ollila, Palomäki, Palotie, Partanen, Paul, Pelkonen, Pendergrass, Petrovski, Pitkäranta, Platt, Pulford, Punkka, Pussinen, Raghavan, Rahimov, Rajpal, Renaud, Riley-Gillis, Rodosthenous, Saarentaus, Salminen, Salminen, Salomaa, Schleutker, Serpi, Shen, Siegel, Silander, Siltanen, Soini, Soininen, Sul, Tachmazidou, Tasanen, Tienari, Toppila-Salmi, Tukiainen, Tuomi, Turunen, Ulirsch, Vaura, Virolainen, Waring, Waterworth, Yang, Nelis, Reigo, Metspalu, Milani, Esko, Fox, Havulinna, Perola, Ripatti, Jalanko, Laitinen, Mäkelä, Plenge, McCarthy, Runz, Daly and Palotie2023). These diseases were identified by consulting the International Classification of Disease (ICD)-10 codes in the medical records. The ICD-10 code for obesity was E66, and the ICD-10 codes for CHD were I20.0, I21 and I22. These data were used in the sensitivity analysis.
More information on these summary data is shown in Table 2.
Table 2. Characteristics of summary data in the study

CHD, Coronary heart disease; GLGC, Global Lipids Genetics Consortium; PGC, Psychiatric Genomics Consortium.
Instrumental variables
In the traditional MR section, a total of 286, 238, 335 and 209 instrumental variables [i.e., single nucleotide polymorphisms (SNPs)] were selected to separately predict TC, LDL-C, HDL-C and nonHDL-C from the corresponding GWASs according to the following standards: (1) The instrument variables must be highly correlated with the exposures (correlation P value <5 × 10−8). (2) The F statistic of the instrumental variable must be less than 10 to exclude weak instrumental variables. (3) Linkage disequilibrium (LD) clumping was conducted using an r 2 value of 0.001 and a window of 10,000 kb to ensure the independence of the instrumental variables. (4) The instrumental variables related to other common mental and psychological disorders were manually eliminated by consulting the ‘phenoscanner’ data platform.
In the drug-target MR section, 12 SNPs were separately selected to predict HMGCR-mediated TC and LDL-C according to the following standards: (1) The instrument variables were significantly correlated with the exposures (correlation P value <5 × 10−6). (2) Weak instrument variables were directly removed (F-statistic >10). (3) LD clumping was performed with an r 2 value of 0.30 and a window of 100 kb. (4) The instrumental variable must be within 100 kb of either side of the HMGCR gene on the chromosome. (5) The instrumental variables associated with other mental and psychological disorders were excluded according to the ‘phenoscanner’.
In these two sections, after completing the above steps, the instrumental variables related to the exposures were also extracted from the GWAS of the outcomes. Harmonisation was performed to adjust the orientation of the alleles.
The selection criteria for the instrumental variables are also shown in Table 1. The selected instrumental variables are listed in Supplemental Tables 2–7.
MR analysis
IVW, MR-PRESSO and MR–Egger were used to perform MR analysis (Emdin et al., Reference Emdin, Khera and Kathiresan2017; Birney, Reference Birney2022). Among them, IVW has the strongest causal inference ability and requires that all instrumental variables not be affected by horizontal pleiotropy; MR-PRESSO not only makes causal inferences but also detects outliers that significantly affect the results and further reports the corrected results; MR–Egger allows all instrumental variables to be pleiotropic, and the results are most conservative. All these methods reported odds ratios (ORs), 95% confidence intervals (95% CIs), and P values. In this study, a causal relationship could be established when the IVW result was statistically significant and the direction of the results from the other two methods coincided with the direction of the IVW result. A P value <0.05 indicated nominal statistical significance. After the Bonferroni correction, a P value <0.003 was considered to indicate statistical significance (for six exposures and three outcomes).
Sensitivity analysis
Several sensitivity analyses were performed on both MR sections (Wang et al., Reference Wang, Jiang, Zhang and Small2018; Zhang and Ghosh, Reference Zhang and Ghosh2021). First, the study conducted positive control analyses to test the validity of the instrumental variables. In these analyses, cholesterol traits or HMGCR-mediated cholesterol traits were used as the exposures, CHD was used as the outcome, and causal inference was made by IVW. Second, Cochran’s Q test was used to measure heterogeneity, and a P value less than 0.05 indicated heterogeneity. Third, the MR–Egger intercept test was adopted to determine horizontal pleiotropy, and a P value less than 0.05 indicated horizontal pleiotropy. Fourth, the study performed multivariate MR to identify confounding or mediating factors in the causal relationships, and these factors included obesity and CHD.
All MR and sensitivity analyses were performed using the TwoSampleMR package (version 0.5.7) in R software (version 4.3.0).
Results
Effects of cholesterol traits on depression, schizophrenia, and suicide attempts
According to the positive control analyses, IVW suggested that higher levels of TC, LDL-C and nonHDL-C and lower levels of HDL-C were associated with an increased risk of CHD (P = 3.457e-14, P = 6.397e-22, P = 1.396e-36, P = 8.918e-14). These results confirmed the validity of the instrumental variables (Supplemental Table 8).
As shown in Table 3, IVW revealed that higher levels of peripheral nonHDL-C were nominally associated with a decreased risk of depression (OR = 0.969, 95% CI = 0.941–0.998, P = 0.039). As shown in Supplemental Table 9, MR-PRESSO and MR–Egger supported the results from IVW (OR = 0.967, 95% CI = 0.941–0.994, P = 0.017; OR = 0.977, 95% CI = 0.933–1.022, P = 0.314). As shown in Table 3, the Cochran’s Q test revealed significant heterogeneity, but the random-effects IVW used in this analysis was tolerable and yielded reliable results (P = 1.017e-08). In addition, the MR–Egger intercept test did not reveal any horizontal pleiotropy (P = 0.651).
Table 3. MR estimates for cholesterol traits affecting the risk of depression, schizophrenia and suicide attempts

IVW, Inverse variance weighted; MR, Mendelian randomisation; TC, Total cholesterol; LDL-C, Low-density lipoprotein cholesterol; HDL-C, High-density lipoprotein cholesterol; NonHDL-C, Non high-density lipoprotein cholesterol; SNP, Single nucleotide polymorphism; OR, Odds ratio; 95%CI, 95% Confidence interval; CO, Cochran’s Q; MI, MR-Egger intercept.
* Number of SNPs predicted each exposure.
** These multivariate MR analyses adjusted for obesity.
Because obesity and hyperlipidaemia often coexist, multivariate MR was conducted to assess the effect of obesity. As shown in Table 3, peripheral nonHDL-C was no longer related to the risk of depression after adjusting for obesity (OR = 0.994, 95% CI = 0.966–1.023, P = 0.692). As shown in Supplemental Table 10, IVW was used to further explore the effect of obesity on depression and revealed that this factor had no significant effect on the risk of this disease (P = 0.578). Therefore, it is likely that obesity plays a mediating role between nonHDL-C and depression.
In addition, the peripheral levels of TC, LDL-C and HDL-C were not related to the risk of depression (Table 3). The peripheral levels of the four cholesterol traits were also not related to the risk of schizophrenia or suicide attempts (Table 3).
Effects of HMGCR-mediated cholesterol traits on depression
As shown in Supplemental Table 8, the positive control analyses (IVW) suggested that higher levels of HMGCR-mediated TC and LDL-C were associated with an increased risk of CHD (P = 3.100e-05, P = 4.299e-05). These results demonstrated that inhibiting HMGCR expression may reduce the risk of CHD. Therefore, these instrumental variables can effectively predict the use of statins.
As shown in Table 4, IVW and MR-PRESSO reported that higher levels of HMGCR-mediated TC were nominally associated with a decreased risk of depression (OR = 0.904, 95% CI = 0.835–0.979, P = 0.013; OR = 0.904, 95% CI = 0.840–0.973, P = 0.028). The direction of the MR–Egger result was the same as the direction of the above results (OR = 0.847, 95% CI = 0.546 ∼ 1.312, P = 0.481). The Cochran’s Q and MR–Egger intercept tests did not reveal any heterogeneity or horizontal pleiotropy (P = 0.551, P = 0.774).
Table 4. MR estimates for HMGCR-mediated cholesterol traits affecting the risk of depression

MR, Mendelian randomisation; HMGCR_TC, HMGCR-mediated total cholesterol; HMGCR_LDL, HMGCR-mediated low-density lipoprotein cholesterol; IVW, Inverse variance weighted; MR-PRESSO, Mendelian randomisation pleiotropy RESidual sum and outlier; SNP, Single nucleotide polymorphism; OR, Odds ratio; 95%CI, 95% Confidence interval; CO, Cochran’s Q; MI, MR-Egger intercept.
* Number of SNPs predicted each exposure.
** These multivariate MR analyses adjusted for coronary heart disease.
As shown in Table 4, the three MR methods explored the effect of HMGCR-mediated LDL-C on depression and reported some results similar to the relationship between HMGCR-mediated TC and disease (OR = 0.917, 95% CI = 0.854–0.985, P = 0.017; OR = 0.917, 95% CI = 0.864–0.974, P = 0.019; OR = 0.862, 95% CI = 0.575–1.293, P = 0.494). The sensitivity analyses also did not reveal any heterogeneity or horizontal pleiotropy (P = 0.707, P = 0.770).
As shown in Table 4, because CHD is the primary indication for statins, multivariate MR adjusted for this disease revealed that HMGCR-mediated TC and LDL-C no longer reduced the risk of depression (OR = 0.967, 95% CI = 0.928–1.006, P = 0.099; OR = 0.977, 95% CI = 0.947–1.009, P = 0.159). As shown in Supplemental Table 10, IVW further revealed that CHD did not affect the risk of depression (P = 0.979). Therefore, CHD is likely to play a mediating role between statin use and depression.
Effects of HMGCR-mediated cholesterol traits on schizophrenia
As shown in Table 5, IVW suggested that higher levels of HMGCR-mediated LDL-C were associated with an increased risk of schizophrenia (OR = 1.246, 95% CI = 1.022–1.519, P = 0.030), but MR–Egger reported the opposite result (OR = 0.672, 95% CI = 0.206–2.196, P = 0.530). IVW also revealed that HMGCR-mediated TC did not affect the risk of this disease (OR = 1.235, 95% CI = 0.961–1.587, P = 0.099).
Table 5. MR estimates for HMGCR-mediated cholesterol traits affecting the risk of schizophrenia

MR, Mendelian randomisation; HMGCR_TC, HMGCR-mediated total cholesterol; HMGCR_LDL, HMGCR-mediated low-density lipoprotein cholesterol; IVW, Inverse variance weighted; MR-PRESSO, Mendelian randomisation pleiotropy RESidual sum and outlier; SNP, Single nucleotide polymorphism; OR, Odds ratio; 95%CI, 95% Confidence interval; CO, Cochran’s Q; MI, MR-Egger intercept.
* Number of SNPs predicted each exposure.
** These multivariate MR analyses adjusted for coronary heart disease.
Effects of HMGCR-mediated cholesterol traits on suicide attempts
As shown in Table 6, the IVW and MR-PRESSO results suggested that higher levels of HMGCR-mediated TC were nominally associated with an increased risk of suicide attempts (OR = 1.187, 95% CI = 1.018–1.384, P = 0.028; OR = 1.187, 95% CI = 1.050–1.344, P = 0.020), and MR–Egger reported a similar result (OR = 1.271, 95% CI = 0.564–2.863, P = 0.575). In addition, the Cochran’s Q and MR–Egger intercept tests revealed no heterogeneity or horizontal pleiotropy (P = 0.785, P = 0.870).
Table 6. MR estimates for HMGCR-mediated cholesterol traits affecting the risk of suicide attempts

MR, Mendelian randomisation; HMGCR_TC, HMGCR-mediated total cholesterol; HMGCR_LDL, HMGCR-mediated low-density lipoprotein cholesterol; IVW, Inverse variance weighted; MR-PRESSO, Mendelian randomisation pleiotropy RESidual sum and outlier; SNP, Single nucleotide polymorphism; OR, Odds ratio; 95%CI, 95% Confidence interval; CO, Cochran’s Q; MI, MR-Egger intercept.
* Number of SNPs predicted each exposure.
** These multivariate MR analyses adjusted for coronary heart disease.
As shown in Table 6, multivariate MR revealed that HMGCR-mediated TC was not associated with the risk of suicide attempts after adjusting for CHD (OR = 1.042, 95% CI = 0.964–1.127, P = 0.301). As shown in Supplemental Table 10, IVW further revealed that CHD did not affect the risk of suicide attempts (P = 0.488). Therefore, CHD may also play an intermediary role in this potential relationship.
In addition, IVW did not reveal any relationship between HMGCR-mediated LDL-C and suicide attempts (OR = 1.122, 95% CI = 0.969–1.299, P = 0.123).
Discussion
Both depression and schizophrenia are common mental and psychological disorders worldwide. Their aetiologies are complex, and the risk of disease is influenced by many factors. Among these factors, cholesterol metabolism is one that is surprising but not negligible. These diseases are likely to be effectively controlled only if these factors, including cholesterol metabolism, are fully understood. Therefore, the present study used MR methods to explore the associations of peripheral cholesterol and cholesterol-lowering therapy with the risk of depression and schizophrenia. The findings obtained may help us to gain insight into the pathogenesis and risk factors for these diseases and help us to identify new therapeutic targets.
NonHDL-C refers to all lipoprotein cholesterol traits except HDL-C, mainly LDL-C and very low-density lipoprotein cholesterol (VLDL-C), of which LDL-C accounts for more than 70%. Furthermore, nonHDL-C has been shown to be a powerful predictor of atherosclerosis and CHD risk (Wang et al., Reference Wang, Jing, Wang, Zhang, Zhao, Li, Wang, Li, Liu, Wang and Wang2021). In the present study, we found that elevated peripheral levels of nonHDL-C were associated with a reduced risk of depression, while peripheral levels of LDL-C were not related to the risk of disease. Notably, the former correlation, although slight, did have nominal statistical significance; the strength of the latter correlation was similar to that of the previous correlation but failed to meet the criterion of nominal statistical significance. Therefore, we suspected that another major component of nonHDL-C (i.e., VLDL-C) might be the factor affecting the risk of depression. Unfortunately, the selected GWAS did not provide summary data on VLDL-C, and the present study cannot confirm this hypothesis with the existing data.
The present study also explored the potential effect of statin use on depression, but the results were surprising. Briefly, we found that each one-SD increase in HMGCR-mediated TC and LDL-C may reduce the risk of depression by 10% at the genetic level. These findings indicate that statins, which are HMGCR inhibitors, may unexpectedly increase the risk of this disease. Because the positive control analysis confirmed the validity of the instrumental variables for these HMGCR-mediated cholesterol traits, the above results were procedurally reasonable. Moreover, the results from the traditional MR section also appeared to be consistent with these results, which further added credibility to them, although these correlations were only nominally significant.
Multivariate analyses eliminated the associations of these cholesterol traits or HMGCR-mediated cholesterol traits with the risk of depression after removing confounding factors (i.e., obesity or CHD) in both the traditional and drug-targeted MR sections. Because further analyses confirmed that these two confounding factors did not affect the risk of depression, we believe that obesity and CHD may be potential mediators of the relationship between cholesterol metabolism and depression. The specific mechanism involved should be explored in future research.
The results for depression in the present study were not isolated. Several early observational studies reported that low peripheral cholesterol levels were associated with depression and that lower peripheral TC levels were the most important predictor of depression severity (Khalid et al., Reference Khalid, Lal, Trivedi, Dalal, Asthana, Srivastava and Akhtar1998). One recent review concluded that although the majority of published studies have suggested that statin use has a protective effect on depression, other studies have reported that these drugs have no effect or a negative effect on the disease (De Giorgi et al., Reference De Giorgi, Rizzo Pesci, Quinton, De Crescenzo, Cowen and Harmer2021). Therefore, this topic remains controversial and should be further explored.
There are two explanations for the above results: (1) The ‘obesity paradox’ is one controversial theory, but it is indeed supported by a number of studies (Koifman and Arow, Reference Koifman and Arow2022). The theory suggests that obesity has a potentially protective effect against several diseases. Obesity is closely related to cholesterol metabolism, so we suspected that the association between cholesterol metabolism and depression may support the obesity paradox. (2) Statins have a variety of biological effects. In addition to reducing cholesterol levels, these drugs may promote the occurrence of depression through other mechanisms. For example, statins may increase serum cortisol in humans, which is implicated in the development of depressive symptoms; the drugs may also increase brain-derived neurotrophic factor levels through multiple pathways, the latter being related to increased anxiety behaviours (Sahebkar et al., Reference Sahebkar, Rathouska, Simental-Mendía and Nachtigal2016; Okudan and Belviranli, Reference Okudan and Belviranli2020).
In addition, this study revealed that the HMGCR-mediated increase in TC increased the risk of suicide attempts by approximately 18% for every one-SD increase, indicating that statin use may reduce the risk of suicide. Thus, the effects of statins on depression and suicide attempts are conflicting. One possible explanation is that statins have the potential to increase the risk of depression but may not increase the severity of depression; alternatively, such drugs promote mild depression while reducing major depression. These two types of regulatory mechanisms, such as various physiological feedback mechanisms and the effects of angiotensin receptor inhibitors on renal function, are common in humans.
This study had the following limitations. First, due to a lack of data and avoidance of sample overlap, it was not possible to use the existing data to explore the association between VLDL and depression. Moreover, there are several concerns about using the new GWAS for VLDL analysis. For example, other GWASs that could be used had very small sample sizes, which may have led to unstable results; the use of completely different GWASs for VLDL analysis may have led to a lack of comparability between the results of the various components of this study. Second, in addition to HMGCR, many other genes, such as PCSK9 and NPC1L1, were involved in the regulation of cholesterol metabolism. However, the summary data for these genes were much less well developed than those for HMGCR, resulting in the inability to perform subsequent MR analyses. Therefore, these genes were not included in this study. Third, only one drug-target MR method was used in this study; due to the lack of data, another commonly used method, namely, summary-data-based MR, was not used. These limitations should be remedied in future studies.
In conclusion, this study provided some interesting, but less sufficient, evidence that nonHDL-C may have a protective effect on depression, and lowering cholesterol using statins might increase the risk of the disease. However, these findings do not provide a confirmed conclusion; therefore, more studies should be conducted to validate them and reveal the potential underlying mechanisms involved.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/neu.2024.26.
Data availability statement
Data was already available in the text and supplementary materials.
Acknowledgements
We want to acknowledge the participants and investigators of the FinnGen study.
Author contribution
Wang Feng and Chen Zheng conducted the study design. All authors performed the literature research, data acquisition/collation, data analysis and manuscript preparation.
Financial support
Not applicable.
Competing interests
There was no conflict of interest to declare.