Worldwide efforts to control the spread of coronavirus disease 2019 (COVID-19) are focused on the avoidance of close physical contact, reducing the possibility of transmission by respiratory droplets [Reference Taylor, Lindsay and Halcox1, Reference Chia2]. However, evidence from previous researches suggests the possibility of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission by fomites or environmental surfaces [Reference Taylor, Lindsay and Halcox1, Reference Cai3].
Previous work assessing the stability of SARS-CoV-2 on different surfaces has shown the ability to recover viable virus for up to seven days after it was applied to smooth surfaces made of plastic or metal, at room temperature [Reference Ong4, Reference Chin5]. High humidity and elevated temperatures significantly reduced the ability to recover viable virus from the surfaces.
Sanitation practices and constraints in the use of public recreational facilities were adopted by many countries. The world health organisation has issued interim guidance on the disinfection of environmental surfaces in the context of COVID-19 [6]. These guidelines provide information on effective measures for surface disinfection in health care settings as well as other public facilities such as schools and prison environments. However, these guidelines do not address whether measures for disinfection of outdoor facilities are needed.
In Israel, the initial regulatory response to the COVID-19 outbreak during March 2020 was to prohibit the use of many public utilities, including playgrounds. Playgrounds were not routinely disinfected. During the first wave of the pandemic, a lockdown was imposed and all outdoor activities (including individual sports activities) were prohibited for several weeks. The restrictions on playground activities have remained unchanged following the pandemic's first wave, only to be revoked on 6 August 2020, in the midst of a second disease wave, despite lack of evidence to support either decision.
We aimed to assess the presence of SARS-CoV-2 in environmental samples collected at public playgrounds and water fountains, in a country with high disease prevalence.
As a preliminary validation study, we initially obtained 13 samples from surfaces at patient rooms in the COVID-19 ward at Shamir Medical Center. Samples were taken from bed railings, door handles, sinks and light switches.
Environmental samples were collected from six cities in central Israel: Tel Aviv-Yaffo, Bnei Brak, Rehovot, Kfar Habad, Ramle and Nes Ziona from 8 August 2020 to 10 August 2020.
A convenience sample of playgrounds and water fountains from different quarters in each city was collected. We chose cities with a high overall prevalence of disease and sampled more locations in larger cities. Samples were collected from drinking fountains and high-touch recreational equipment at playgrounds. In playgrounds, swabs were obtained from the upper bar of ladders and from surfaces intended for crawling, mainly plastic tunnels connecting different parts of the playground structures and slides. At the water fountains, the same swab was used for the dispensing button and spigot. Sterile pre-moistened swabs were used to collect the samples, put in viral transfer media and transferred to the laboratory in a cooler. Data regarding sun exposure and temperature were collected at each sampling location. Viral detection was achieved by real-time reverse transcriptase–polymerase chain reaction, targeting four genes (Allplex SARS-CoV-2 Assay, Seegene, Korea), performed in the hospital's molecular laboratory that is approved by the Israeli Ministry of Health. Prevalence and population data were obtained from the Israeli national COVID-19 data repository and the Central Bureau of Statistics [7, 8]. Ethics committee approval was waived since human subjects were not involved in the study.
Of the 13 samples collected from surfaces at the COVID-19 ward, two tested positive (15%).
The prevalence of active COVID-19 cases in the areas sampled varied from 250 per 100 000 population in Tel Aviv-Yaffo to 1140 per 100 000 population in Kfar Habad (Table 1). As no population-based screening programmes have been carried out, and most SARS-Cov-2-positive children are asymptomatic carriers, the exact prevalence of COVID-19 among children is not known. However, in different studies in Israel, children constituted about 16–17% of all positive results. Forty-three samples were collected from equipment in 33 playgrounds (in large playgrounds, samples were taken from two separate areas) and 25 samples from water fountains. At the time of sampling, the temperature ranged from 29 to 34 °C in the shade with up to 60% humidity. Two of the 43 (4.6%) samples from playground equipment and one (4%) sample from a drinking fountain tested positive. All positive samples were collected from shaded areas while all samples collected from locations directly exposed to sunlight were found negative to SARS-CoV-2.
Table 1. COVID-19 prevalence and positive environmental samples across the studied cities and hospital ward
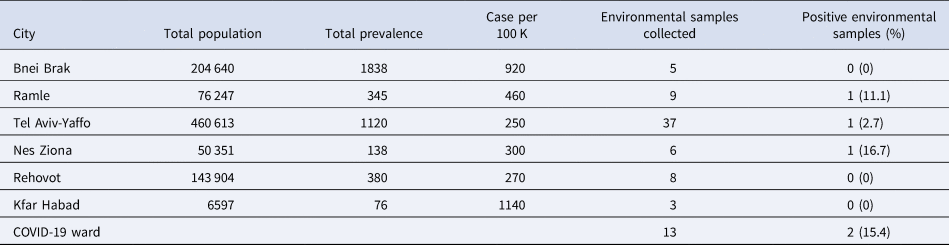
Disease prevalence on 10 August 2020. City population size was obtained from the 2019 survey of the Israeli Central Bureau of Statistics.
To the best of our knowledge, this is the first study showing that SARS-CoV-2 RNA can be detected on outdoor surfaces and water fountains in recreational communal areas.
Previous studies have demonstrated the presence of the virus on surfaces in experimental models and within hospitals [Reference Taylor, Lindsay and Halcox1, Reference Chia2, Reference Ong4, Reference Chin5] and, accordingly, two of the samples we collected in the COVID-19 ward were positive despite routine meticulous cleaning and disinfection.
Environmental samples were collected from six cities in Israel with a differing prevalence of the disease. We could not comment on the correlation between disease prevalence in the city and the number of positive results. This is due to the low number of positive results, in addition to the fact that many other factors might influence positivity, like the number of children using the playground or the water fountain.
Although our sampling was consistent in terms of the method of collection and the area of the playground tested, as we merely aimed to show a proof of concept (mainly that the virus can be detected on the equipment), the selection of location and the number of sites in each city were based on convenience.
It is worth noting that two of the positive samples were recovered from playground equipment. The role of young children in the spread of SARS-CoV-2 has been questioned, though recent data have shown that children are capable of transmitting the disease [Reference Luo9]. On the other hand, many children testing positive are asymptomatic carriers, and are thus likely to be socially active and use communal facilities. If, as these preliminary results suggest, environmental surfaces can play a role in the chain of transmission, children may be an important part of the chain.
Another interesting finding in our study is the fact that positive samples were all from shaded playground areas, with no positive samples from areas with direct sunlight exposure. These findings are in line with published data showing that the SARS-CoV-2 is sensitive to high temperatures and humidity with an inactivation time of only 5 min at 70 °C, reduced from several days at room temperature [Reference Chin5]. At the time of environmental sampling, all obtained from the same geographic and climatic area, Israel experienced a minor heatwave and the temperature was between 29 and 34 °C in the shade with 60% humidity. The temperature in areas with direct sun is extremely high and could therefore possibly preclude recovery of the virus.
We decided to sample water fountains in public areas since many people, especially children, drink directly from the nozzle and it was shown that the virus can survive in water for up to 4 days [Reference La Rosa10]. With one positive sample, of 25 obtained, it seems prudent to advice against direct contact between the mucosa of the lips and the nozzle.
Environmental disinfection in public areas has become routine practice in many countries. It has been suggested that this practice should be stopped [Reference Zhang and Yun11]. Our findings of SARS-CoV-2 RNA in public playgrounds and water fountains do not conclusively support either approach. Further research is needed in order to determine whether routine disinfection of playgrounds is warranted.
Our study has several limitations. First, it is unclear whether the recovery of viral RNA on surfaces in areas with a high prevalence of the disease also indicates the possibility of acquiring the virus via contact. Viral samples were not cultured, limiting our ability to examine the viability and possible infectivity. Second, the samples size was relatively small. However, a relatively low number of samples were collected from six different cities and three positive samples were observed.
The environmental contamination of playground equipment and water fountains with SARS-CoV-2 we were able to demonstrate in this study amplifies the need for strict adherence to environmental and personal hygiene in urban settings.
Further studies are required to confirm the results of this preliminary report.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0950268821000546.
Data
The data used to support the findings of this study are available from the authors upon request.
Acknowledgements
Supported by the Israeli Ministry of Health.
Author contributions
EK and IY conceptualised the study. IY, EK, GK, SP, AB-H, PB-L and HK collected and analysed the data. ER wrote the first draft of the manuscript. IY and EK revised the manuscript. All authors approved the final version.
Conflict of interest
None.




