In 2016, India was home to 250 million adolescents (UNICEF 2017), and in 2011, 19 % of Maharashtra’s population were adolescents(1). Adolescence is the period between 10 and 19 years of age(2) and is divided into early (10–14 years) and late adolescence (15–19 years)(Reference Patton, Sawyer and Santelli3).
The public health problems among adolescents in India include micronutrient deficiencies, stunting, underweight and overweight(Reference Christian and Smith4). Our previous work has shown that being born into an environment deficient in energy content and nutrients followed by later exposure to high-energy environments can be the least favourable combination in terms of non-communicable disease risk(Reference Bavdekar, Yajnik and Fall5). This phenomenon is increasingly likely in the context of the social, economic and nutrition transition putting the current generation at risk(Reference Popkin6,Reference Popkin, Adair and Ng7) . Between 2011 and 2017, the proportion of the population in rural areas has decreased from 70 to 66 %(8) due to migration from villages to cities and the urbanisation and expansion of villages to towns and small cities(Reference Cyril, Oldroyd and Renzaho9).
Adolescents worldwide consume too many refined grains, sugary foods and drinks and insufficient fruit, vegetables and whole grains(10).Over the last two decades in LMIC, the nutrition transition and reduced physical activity are contributing to the increased prevalence of overweight and obesity(Reference Popkin11,Reference Tzioumis and Adair12) .
Investments in adolescence benefit the individual’s current and future health, as well as that of their children(Reference Patton, Sawyer and Santelli3). Adolescence may be a critical period for later health and disease, and improving nutrition may increase human capital and reduce non-communicable disease risk over the lifecourse(Reference Viner, Ross and Hardy13,Reference Hanson and Gluckman14) .
Nutrition habits developed during adolescence are likely to track into adulthood(Reference Azevedo, Araujo and Cozzensa da15–Reference Craigie, Lake and Kelly17). Factors reported to influence adolescent’s food choices in high-income settings include age, gender, autonomy, taste, food security, family influences, parental control, peer and institutional influence(Reference Bassett, Chapman and Beagan18–Reference Story, Neumark-Sztainer and French20).
The Indian Government has initiated school health programmes including those aimed at empowering adolescent girls(21) such as Fe and folic acid supplementation. Despite these initiatives, adolescents remain a largely neglected population. Little is known about rural Indian adolescents’ attitudes to diet and physical activity(Reference Correa, Rajaraman and Swaminathan22), and we are not aware of any studies investigating the caregiver’s attitudes and beliefs. Our aim was to explore the drivers of adolescent food choice and physical activity patterns in a setting undergoing economic and social transition. We used focus group discussions (FGD) to obtain in-depth responses and understand social norms around this topic(Reference Krueger and Casey23).
Methods
Research setting, design and participants
The current study was part of an international collaboration, Transforming Adolescent Lives Through Nutrition (TALENT; for further details about the wider programme, see Barker et al., this issue). The setting was three villages 40–60 km from Pune city (Pabal, Dhamari and Kendur) selected to enable recruitment of participants from a range of socio-economic backgrounds. The villages are currently transitioning in terms of the expansion of city limits and economic growth.
A prospective cohort, the Pune Maternal Nutrition Study, was established in this setting in 1994 to examine associations between pregnancy diet and offspring outcomes(Reference Rao, Yajnik and Kanade24,Reference Yajnik, Fall and Coyaji25) . At this time, subsistence farming was common with little access to food markets. Most women were married and began childbearing by 18 years of age. Underweight and stunting were prevalent, and 31 % of women were severely chronically energy deficient with a BMI < 17 kg/m2(Reference Rao, Yajnik and Kanade24). Transport infrastructure was limited, and agriculture was largely rainfed.
Over the last 20 years, a dam system has improved farmland irrigation, generating capacity to grow cash crops, for example, sugarcane. The increased income has improved purchasing power, provided more permanent housing and ownership of vehicles and domestic appliances. There are more varied employment opportunities due to the emergence of small industries and improved road connectivity. Most villages now receive electricity, and literacy rates have increased. Housing varies from kuchha dwellings (made with temporary materials including mud and plastic sheeting) to concrete, pukka houses.
We recruited adolescents aged 10–12 and 15–17 years because we anticipated differences between early and late adolescence in terms of the influences on behaviour, the caregiver–adolescent relationship and the suggested solutions. Also, we expected that participants would feel more comfortable and talk more openly with others of a similar age.
Households known to include an adolescent of the target age were approached by TALENT project staff who were also residents of the study villages. Potential participants were given the opportunity to ask questions about the study before agreeing to take part. If adolescents and caregivers agreed to participate, written consent and assent were obtained from the caregivers and adolescents, respectively.
Thirty-eight adolescents and their caregivers (mothers) were recruited for the FGD from a wider pool of eighty-one adolescents. The wider pool was a convenience sample recruited to provide some context in terms of socio-demographic characteristics and anthropometric measurements.
Data collection
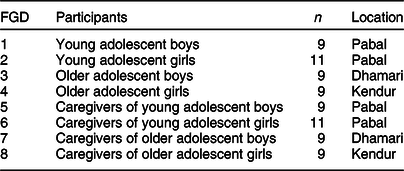
Eight FGD were conducted between May and August 2018: two with adolescents aged 10–12 years, two with those aged 15–17 years (boys and girls separately) and four with their mothers. Four were conducted at a primary health centre in Pabal village, two at a health centre in Dhamari and two at a gymnasium in Kendur. After obtaining written permission to record the discussion, participants were given numbered badges for anonymity. A digital audio recorder (Olympus VN-541PC) was used. FGD took 45–90 min. Those with adolescents were conducted by K.J.R. and with mothers were conducted by A.D./V.K. in Hindi and Marathi languages, and field notes were taken by P.K., R.S., P.S. and R.W. The facilitators were trained in qualitative research (Editorial issue) and had not met the participants previously.
A FGD guide was developed, to enable discussion of all levels of factors that might influence adolescent diet and physical activity levels (see conceptual map in Barker et al. in this issue for details). The guide was then tested and validated with pilot groups of adolescents and mothers. The guide included (i) current diet habits and food preferences, (ii) physical activity patterns, (iii) opportunities and challenges to having a healthy diet and being physically active, (iv) parental involvement in adolescent diets and (v) ideas about future interventions.
Among the wider pool of eighty-one adolescents, trained research staff administered socio-demographic questionnaires and measured height to the nearest 0·1 cm using a stadiometer (CMS Instruments Ltd) and weight to the nearest 0·1 kg using electronic scales (TANITA India Pvt. Ltd) (for further details about the wider pool data, see Fall et al. in this issue).
Data analysis
FGD recordings were transcribed in Hindi–Marathi and translated into English. Transcriptions were produced by K.J.R., P.K., V.K. and P.S., and translations were carried out by K.J.R., P.K., V.K. and R.W. A final check was carried out by K.J.R., and NVivo (version 12) software for qualitative analysis was used. A thematic approach was employed using Braun and Clarke’s step-by-step guide(Reference Braun and Clarke26). K.J.R. read the transcripts several times. Discussions about the emergent themes during a TALENT training workshop lead to the development of an initial coding framework. The emergent themes and codebook developed in the workshop informed the initial coding of the transcripts. As coding continued, the codebook was revisited and revised as necessary. The codes were checked by P.J., S.W. and M.B. The codebook was revised based on discussions with the research team to ensure that the codes reflected the data. The final codes formed the themes that the researchers felt accurately represented the messages from the data. Once the key themes were categorised, revisited and refined, the key findings were presented visually (Fig. 1). Figure 1 aims to conceptualise the relationships between themes. We adhered to the Consolidated Criteria for Reporting Qualitative Research(Reference Tong, Sainsbury and Craig27).
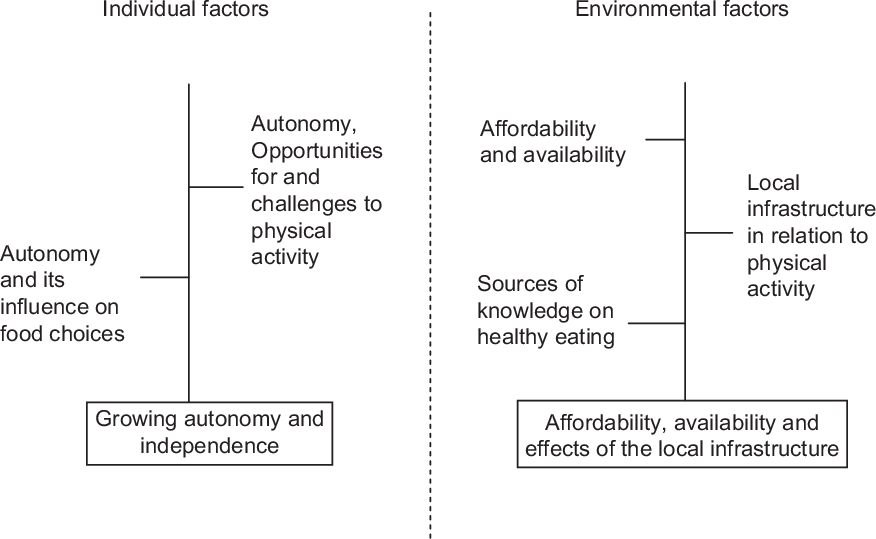
Fig. 1 Thematic map depicting individual and environmental factors associated with dietary and physical activity behaviour
Results
Participant characteristics
Anthropometric data relating to the larger pool of eighty-one participants are presented in Table 1. Mean height-for-age was below the WHO growth standards(28) for all adolescents, particularly for girls of both age groups who were on average approximately 1 sd below the mean. Approximately 10 % of the participants were stunted. BMI-for-age was below average for both boys and girls, with girls at 10–12 years and boys at 15–17 years being almost 1 sd below the mean.
Table 1 Adolescent anthropometry (n 81)*
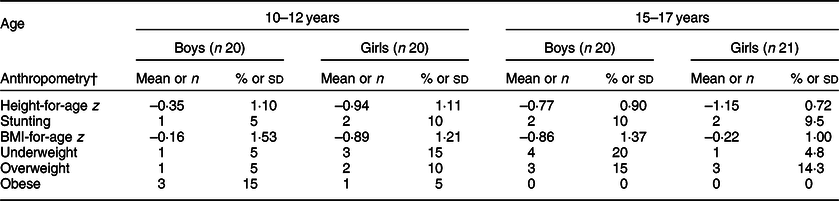
* Values are mean and sd for continuous variables and n and % for categorical variables.
† Height-for-age z, BMI-for-age z, stunting, underweight, overweight and obese are defined using WHO 2007(28).
Socio-demographic data relating to caregivers in Table 2 provide context for the study. Mothers of older adolescents had, on average, been schooled for 7 years and those of younger adolescents for 10 years. Most mothers were self-employed with approximately a quarter being unemployed. Table 3 presents the age category, gender, number and location of adolescents in each FGD.
Table 2 Socio-demographic characteristics of caregivers
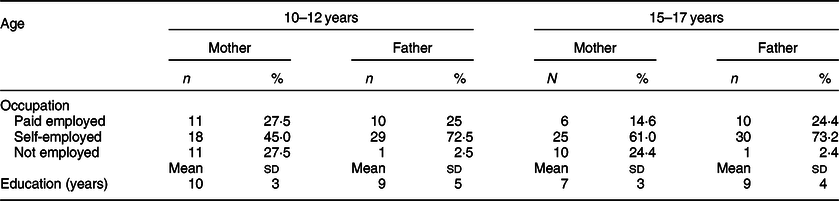
Table 3 Composition of each of the eight focus group discussions (FGD)
Themes emerging from the focus group discussions
Three major themes emerged from the data: (i) influence of growing autonomy and independence during adolescence, (ii) access, availability and effects of local infrastructure and (iii) preferences for interventions to improve diet and physical activity. We produced a thematic map to depict individual and environmental factors associated with themes 1 and 2 (Fig. 1).
Theme 1: The influence of growing autonomy and independence
Sub-theme 1.1: Autonomy and its influence on food choices
Adolescents reported consuming foods based on preference, appearance, taste, smell, habit and peer influence. A few reported choosing foods based on their health benefits. The choices of younger adolescents were driven by television advertisements and offers on food packets.
Respondent 1: ‘We choose food which is good, healthy, looks attractive’.
Respondent 2: ‘Food which we always eat - habit’. (FGD 3, older adolescent boys)
Respondent 1: ‘If something new is available then we eat that and do not eat the same food’.
Respondent 2: ‘TV advertisements…’
Respondent 3: ‘If there is something free with it - offers’.
Respondent 4: ‘If the packaging is simple only, then that food is not good….’
Respondent 5: ‘Friend brought it. He said it is good, then [I] ate the same the next day’. (FGD 1, young adolescent boys).
There was some indication that adolescent autonomy over food choices increases with age. For example, older adolescent boys chose to eat food made outside their homes.
‘[I] eat outside food more, [I] do not like homemade food’. (FGD 3, older adolescent boys)
‘During and after school they [girls] might eat something outside’. (FGD 8 caregivers of older adolescent girls)
‘Mostly boys eat outside, girls are shy’. (FGD 8 caregivers of older adolescent girls)
Older boys and girls described how decisions about the foods that were eaten at home were made together by parents and children.
‘[Mother asks] everyone, what should I prepare, this or that? Which vegetable should I make? What do you want to eat? Will you eat, if I prepare this will you eat? We are asked before meal is cooked’. (FGD 4, older adolescent girls)
‘Buy things which kids like’. (FGD 7 caregivers of older adolescent boys)
Most caregivers reported little conflict over food choices and tried to serve healthy foods to adolescents, while accommodating their preferences.
‘I make only what he will like. I mostly try [to ensure] that he eats everything. And I give him cucumber, etc in his school tiffin and I give him a fruit after he comes back. So other food items should also be included. I give him one litre water bottle for school and I make sure that he finishes it’. (FGD 5, mother of young adolescent boys)
‘He doesn’t go outside and eat. He asks his father to bring it for him. Generally children of this age don’t go out and eat, they go when the elders take them’. (FGD 5, caregivers of young adolescent boys)
However, some younger adolescents reported that their parents did not give them a choice and were reprimanded for eating unhealthy foods.
‘[Parents] ask [us] to eat given foods without any arguments’. (FGD 1, young adolescent boys)
Among younger adolescents and their caregivers, there were reports of parental disapproval of foods eaten outside the home and restriction on foods that were eaten.
‘Mother shouts if I eat outside food’. (FGD 2, young adolescent girls)
‘what we should do is, we should not let them go near the food items which shouldn’t be eaten (laughter) if we don’t let them go then how will they eat?’ (FGD 6, caregivers of young adolescent girls)
The younger adolescents reported that in most cases the menu for the household was decided by others.
‘We eat whatever [vegetable] is made or which is available at home’. (FGD 1, young adolescent boys)
There were differing reports from younger and older adolescents regarding lunch time habits. Younger girls said that they took home-prepared tiffins (lunch boxes) to school.
‘We carry tiffin from home and eat that at school’. (FGD 2, young adolescent girls)
Older adolescent girls talked about eating shop-bought snacks for lunch.
‘Eat Chakli, chips, kurkure, chocolate, biscuits…from the shop’. (FGD 4, older adolescent girls)
Street food was perceived to be particularly desirable, but more so by older than younger adolescents, and it was disapproved of by parents and caregivers.
‘My parents say that I should not eat street food items, I should eat homemade foods and cereals-pulses only’. (FGD 2, young adolescent girls)
Younger adolescents were more dependent on parents agreeing to bring street food home. Some wanted to eat homemade rather than street food.
‘Homemade food is fresh…. homemade food is tasty’. (FGD2, young adolescent girls)
Sub-theme 1.2: Autonomy, opportunities for, and challenges to, physical activity
Mothers reported resistance to helping with chores such as purchasing groceries in favour of watching television or playing on mobile phones. Sometimes, adolescents were given tasks to encourage physical activity.
‘He doesn’t do any work. He complains that I ask only him to do the work. [He] doesn’t listen even after telling’.
‘Children are mostly on the phone nowadays; there’s always somebody on the call. He takes games and keeps on playing. I think the old phones were better……’
‘Giving him small jobs like giving some message to someone, bringing something from the shop, then it makes him walk’. (FGD 5, mothers of young adolescent boys)
Adolescents reported that swimming, cycling, walking and running were their routine physical activities, while cricket, badminton and kabbadi Footnote * were among their favourite sports. However, there were negotiations between adolescents and their parents about opportunities for physical activity. Older adolescents reported resistance from parents and teachers to allowing them to go out and play before or during exams.
‘Parents do not allow to go for playing if there is work or exams, otherwise they do not stop’. (FGD 3, older adolescent boys)
Some older girls disliked physical activity in addition to household chores.
‘We do not like to do anything extra like this - playing etc’. (FGD 4, older adolescent girls)
A few girls said that they had stopped being active as they got older while some talked about activities they enjoyed that were no longer available.
‘[We] like dancing but no one teaches [it]. Before they used to but now have stopped’. (FGD 4, older adolescent girls)
Some girls described being actively supported by parents and caregivers to exercise more.
‘[My] parents bought me badminton’. (FGD 2, young adolescent girls)
‘If I am dancing in the evening, then mother tells me that you do this step. She also sometimes dances with me. I do get support’. (FGD 4, older adolescent girls)
Parents described how recently children spent a lot of time in sedentary activities such as games and TV.
‘Nowadays children remain engaged in games, TV. Children are addicted to such things. They should get some knowledge about this’. (FGD 5, caregivers of young adolescent boys)
Theme 2: Affordability, availability and effects of the local infrastructure
Sub-theme 2.1: Affordability and availability
Most adolescents said that there was enough food available in their households to fulfil their appetites. However, sometimes availability of fruits and sweets was limited.
Respondent 1: ‘We eat till [we] feel full’.
Respondent 2: ‘Sometimes the portions change, when everyone is very hungry’.
Respondent 3: ‘[We] eat as much as we want’. (FGD 2, young adolescent girls)
I get more [food]. [I] have younger brothers and sisters at home, so when something is brought into the house, then it is divided. (FGD 3, older adolescent boys)
Access to food was regular for most respondents with caregivers reporting that fresh vegetables and fruits were bought from the weekly market with a few reporting daily purchases. Non-farming households and those without kitchen gardens or fruit trees had no access to fruit.
‘[I buy groceries every] 15 days. The vegetables [are] home grown’. (FGD 5, mothers of younger adolescent boys)
‘[I buy]groceries once a month and vegetables once a week’. (FGD 6, mothers of young adolescent girls)
Adolescents said that what was eaten was a matter of availability.
‘[It is] decided based on the vegetable that is available in the house’. (FGD 1, young adolescent boys)
In some households, poverty was described as a barrier to the consumption of foods such as fruit.
‘Farmers do not get fruit because of poverty. So we eat what we grow in our fields - green leafy vegetables, etc’. (FGD 8, mothers of older adolescent girls)
Despite the fact that healthy foods were expensive, they were a priority in some households.
‘[We give] priority to nutrition. We pay and get nutritious food. I buy the food from which we get vitamins even if it is expensive’. (FGD 5, mothers of young adolescent boys)
Some adolescents talked about a school nutrition programme where pupils were served a mid-day meal of rice with spices and vegetables. Additionally, in some schools, older adolescents prepared food for other pupils.
‘There is a department where the students make their foods on their own at school with a teacher’s guidance, and sell it in school. It is like a canteen. This activity takes place three times a week, it happens on rotational basis for each standard’. (FGD 3, older adolescent boys)
Sub-theme 2.2: Local infrastructure in relation to physical activity
The villages had gyms which many older adolescent boys used. A few younger adolescents attended coaching for Karate and swimming. Mothers reported that some older girls found it difficult to spend time on physical activity due to the distances between home and school and the requirement to do chores.
‘Because school is far away, [my daughter] doesn’t participate in any sports activity’. (FGD 8, mothers of older adolescent girls)
‘Due to time constraint, no [physical] activity can be done [with the girls]. … We have to go to the fields’. (FGD 8, mothers of older adolescent girls)
Adolescents said that local schools had started operating full instead of half days on Saturdays and 2 h of this was dedicated to sports and yoga. Schools offered sports training for adolescents and opportunities to participate in competitions.
‘There is a Yoga session on every Saturday at school’. (FGD 1, young adolescent boys)
‘Teacher gives training every day and also gives time to play’. (FGD 3, older adolescent boys).
Sub-theme 2·3: Knowledge of healthy eating
All participants reported knowing about good health and nutrition. Their knowledge was derived from school teachers, parents and elders, social media and television advertisements. Older adolescents had greater exposure to social media and other digital tools, whereas younger adolescents had access to television and occasionally to parental mobile phones. These sources provided information about food adulteration and contamination issues.
‘It was shown in a Whatsapp video that Kurkure Footnote † has plastic [in it]’. (FGD 1, younger adolescent boys)
‘Ice gola Footnote ‡ has colours in it which may increase anxiety’. (FGD 1, younger adolescent boys)
‘Chinese food also has added colours which are bad. They can damage kidneys’. (FGD 1, young adolescent boys)
‘Vadapav Footnote § contaminated with the vectors from the feet of flies can go inside our stomach when we eat that Vadapav and spread diseases’. (FGD 1, younger adolescent boys)
Theme 3: Preferences for interventions
Adolescents suggested various school-based interventions including improving the food environment and providing better facilities for physical activity.
‘The distribution of biscuits at school must be stopped and almonds should be given instead…dry fruits should be given’. (FGD 1, young adolescent boys)
‘Vendors and food stalls serving unhealthy foods should be removed from the school premises’. (FGD 3, older adolescent boys)
‘Make a swimming tank [pool] in school’. (FGD 1, young adolescent boys)
‘[The] number of yoga sessions should be increased’. (FGD 1, young adolescent boys)
Caregivers talked about improved hygiene as a priority to enhance adolescent health and nutrition.
‘Bathroom facilities in school, and water facilities should be there’. (FGD 5, mothers of younger adolescent boys)
It was suggested that physical activity facilities be provided by the government
‘Villages are ignored by the government. A garden should be made here - swings, slides. A small swimming tank [pool] is required’. (FGD 5, mothers of young adolescent boys)
There was a focus on difficulties for older adolescent girls. Mothers suggested that the government offered targeted classes and facilities, distributed bicycles or provided better local transport to enable safe travel.
‘The village should have karate class because if it is nearby then parents would also agree to send us, since the school is too far’. (FGD 4, older adolescent girls)
‘They [government] should provide cycles for girls’. (FGD 8, mothers of older adolescent girls)
‘Bus facilities should be provided, as it gets late while going and returning [to and from school]’. (FGD 8, mothers of older adolescent girls)
Discussion
We explored eating behaviour and physical activity of adolescents living in transitioning villages of India. We spoke to both adolescents and their parents to compare their perceptions and understand how to support interventions in the context of cultural, social and economic transition.
As in other settings, older adolescents may experience more autonomy over their food choices and physical activity than younger adolescents and boys more so than girls(Reference Patton, Olsson and Skirbekk29). Parents and older adolescents described joint decision-making about food choices, whereas parents of younger adolescents described a more restrictive approach, particularly to the consumption of street foods. Increasing autonomy is a characteristic of adolescence involving a move to more independent thinking(Reference Sawyer, Afifi and Bearinger30), and eating and physical activity are opportunities to exercise some choice and control(Reference Bassett, Chapman and Beagan18,Reference Tiedje, Wieland and Meiers31,Reference Brown, Shaibu and Maruapula32) . There is evidence that increased autonomy can change family relationships while premature autonomy, that is, too much choice or responsibility too soon, is linked with poorer health outcomes(Reference Patton, Sawyer and Santelli3).
Effect of the economic, social and nutrition transition on adolescent diet
While rural to urban transition was not directly described by participants, abundant access to street foods and lack of infrastructure and facilities for physical activity were discussed. Rural populations in LMIC have been at the risk of food and nutrition insecurity due to lack of availability and access to affordable healthy foods and the time and means to prepare them(Reference Kehoe, Dhurde and Bhaise33–Reference Miller, Yusuf and Chow36). In our study, most foods were available throughout the year, and adolescents were able to access enough food as well as food they liked eating. The exception was fruit when out of season. No participants described having insufficient food or struggling to buy food, and some caregivers reported that providing high quality, nutritious food was a priority whatever the cost, possibly reflecting increasing prosperity(Reference Aijaz37). Many families living in transitioning settings have increased purchasing power as a result of changes in livelihoods from subsistence farming to cash crop farming and working in other industries. Some older adolescents had the option to purchase street, packaged and processed foods. As with previous research(Reference Misra, Singhal and Sivakumar38), we found that adolescents were attracted to street and packaged foods despite knowledge of the health implications. Adolescents were influenced by marketing practices. There is evidence that food companies are less likely to market healthy options in LMIC. A comparison of promotion activities between USA, Germany, Mexico, China, India and the Philippines found that three fast food and beverage companies promoted diet products and fresh dishes more frequently in the USA and Germany than in other countries. Also, McDonald’s in India has different marketing strategies for the poorer north with more advertising aimed at children than in the wealthier south(Reference Bragg, Eby and Arshonsky39).
Effect of the epidemiological transition on physical activity
Participants reported engaging in traditional activities such as household chores and farming activities as well as ‘modern’ sport and recreational activities. Gym facilities in these rural villages would have been largely unavailable until recently but several participants mentioned using them(Reference Aijaz37). Most LMIC have limited opportunities in terms of resources and infrastructure(Reference Van Royen, Verstraeten and Andrade40–Reference Tarun, Arora and Rawal42). As has been described before in India, parental aspirations and the burden of academic studies limited the time that adolescents were permitted to undertake sports and recreational activities(Reference Rajaraman, Correa and Punthakee43) despite evidence that physical activity may improve academic performance(Reference Alvarez-Bueno, Pesce and Cavero-Redondo44,Reference Marques, Santos and Hillman45) . Academic pressure may be another side effect of the transition increasing job opportunities, raising material expectations and earning potential. Adolescent girls have reported a lack of space and opportunity for physical activity but some have no interest in being active(Reference Satija, Khandpur and Satija46). This reduction in interest may be partly due to menarche onset(Reference Ravi, Shah and Edward47) but possibly also to spend more time in sedentary activities such as engaging with social media(Reference Shah, Chauhan and Gupta48). Mothers in our study talked about giving jobs to adolescents as a means of encouraging activity. Being male, having higher educational attainment and more interest in health and appearance have all been identified as predictors of adolescents’ participation in physical activity in South East Asia(Reference Chen, Tsai and Lin49). This information, in conjunction with our findings, may improve targeting of physical activity interventions. For example, interventions aimed at girls may need to be designed differently to those for boys. Overall, the epidemiological transition has been associated with a reduction in physical activity and increased overweight and obesity in LMIC(Reference Shetty50). The TALENT study villages may not yet be sufficiently transitioned for overweight to be observed but this may be a risk for the near future.
Public health implications
The longer-term aim of the TALENT consortium is to develop and test context-specific interventions to improve adolescent health in South Asia and sub-Saharan Africa. The current study was carried out to provide insight into adolescent diet and physical activity habits and how we might address them from the perspective of the beneficiaries of prospective interventions. Participants in our discussions identified factors influencing adolescents’ diets and physical activity habits operating at all levels: individual, familial and national. They had an appreciation of the interplay between factors such as food preferences and choices, family socio-economic status and infrastructure issues such as transport and the influence these exerted. Consequently, they understood that interventions to improve adolescent nutritional status would have to be wide ranging and take into account multiple factors. Our data indicate that nutrition knowledge is generally not a barrier to healthy eating but the increasing availability of processed and high salt, fat and sugar foods in villages, particularly around schools, may lead to unhealthy choices(Reference Naidoo, van Dam and Ng51,Reference Joseph, Nelliyanil and Rai52) . Interventions to reduce the availability of these foods would involve a wide group of stakeholders including schools, local government and food retailers. It would be important that consideration is given to alternative livelihood opportunities for vendors who sell these foods at present.
In terms of physical activity, improving walkability and road safety for cyclists may encourage more active transport to school and provide opportunities in the context of increasing pressure to spend time on academic study(Reference Villa-Gonzalez, Ruiz and Ward53). Addressing the trend towards sedentary activities including watching TV, using computers and phones is likely to be important to prevent a sedentary lifestyle tracking into adulthood(Reference Craigie, Lake and Kelly17). There has been little research conducted into provision of activity facilities in India(Reference Katapally, Goenka and Bhawra54), and it would be important to involve adolescents in the development of any interventions. Caregivers suggested that the government was responsible for providing facilities and that villages were often overlooked in this sort of planning. Larger scale surveys are required to confirm this and to map stakeholders who could be engaged in implementing interventions.
Strengths and limitations
This is the first study to generate qualitative data from rural Indian adolescents and their caregivers on drivers of dietary and physical activity behaviour. Adolescents were grouped by age ensuring perspectives from both early and later adolescence. The research team was trained as part of the TALENT collaboration in qualitative research by skilled researchers who supported data collection and analysis. FGD were conducted separately for adolescents and caregivers to encourage them to share views freely and to explore their perspectives in greater detail.
A limitation was that fathers were not included in FGD. Experience suggests that they are less involved in child’s diet and daily activities, so may have had less to contribute had they been involved. The majority of data coding was completed by K.J.R., thus limiting the assessment of inter-coder reliability. The training team and other collaborators in TALENT sought to ameliorate potential bias in data analysis by reviewing and confirming codes, their definitions and the interpretation. The training team was engaged in discussing and resolving any discrepancies in coding and adjusted code definitions as required.
Conclusions
The ongoing transition in these villages may be increasing accessibility to resources resulting in greater food security and some provision for leisure time physical activity. Adolescents reported that they were eating some unhealthy street food that they desired and understood the risks to health. Caregivers were involved in negotiating with their increasingly autonomous adolescents about access to food and physical activity, using a combination of enabling choice and authoritarianism.
The study could capture changing perspectives and expectations of the adolescents and caregivers over diet and physical activity due to current phase of transition and development. Both adolescents and caregivers believed that there were opportunities to improve food choices and increase physical activity and had ideas about how this might be achieved. The study gave us a picture of the prospects, desires and expectations of the adolescents and their caregivers are changing with transition regarding diet and physical activity. Thus, future intervention development will need to involve extensive engagement with caregivers and adolescents as key stakeholders. Their needs and priorities should form the basis for effective interventions that are aligned with the changing environments in these transitioning villages.
Acknowledgements
Acknowledgements: The authors would like to thank the adolescents and their parents for their time and interest in the study. The authors also thank Pallavi Yajnik and Rasika Ladkat for administrative support and Rucha Wagh, Priyanka Sawant, Rohan Shah, Anagha Deshmukh, Rahul Thigle, Ankush Bhalerao and Vishnu Solat (social workers) and Sujata, Sarla and Rajni (auxiliary nurse midwives) for contributing to the data collection. The authors also thank the TALENT collaboration and SNEHA India for their support. Financial support: The current study was funded by a Global Challenges Research Fund/Medical Research Council pump priming grant (grant no. MC_PC_MR/R018545/1). The funding agency was not involved in the study design, data analysis or writing of the current article. Conflict of interest: There are no conflicts of interest. Authorship: K.J.R. and S.H.K. wrote the manuscript which has been reviewed by all co-authors. K.J.R. and V.K. conducted FGD and P.K. collected data. K.J.R., V.K. and P.K. transcribed and translated the manuscripts independently. K.J.R. confirmed the accuracy of transcription and translation in English. K.J.R. developed the FGD guide with inputs from P.J., S.W. and M.B. K.J.R., V.K., P.K. and C.S.Y. assisted in the execution of the study; K.J.-R. analysed the data, with inputs on the analysis from S.W., P.J., S.H.K., C.H.D.F. and M.B. C.H.D.F. was the main investigator of the project, and C.S.Y. was the local principal investigator. All authors approved the final version of the manuscript. Ethics of human subject participation: The current study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the Institutional Ethics Committee of King Edward Memorial Hospital, Pune (ethics no. 1749). Written informed consent/assent was obtained from all participants. All the consents/assents were witnessed.







