Introduction
Chickenpox is generalised vesicular rash with a possible prodrome of fever, malaise, loss of appetite and headache. The causative agent of disease is varicella zoster virus (VZV), also known as human herpesvirus-3 (HHV-3) that belongs to family herpesviridae, subfamily alphaherpesvirinae and genus varicellovirus. VZV is DNA virus that infects only humans. After primary infection, VZV may reactivate, leading to herpes zoster (shingles). The risk of developing herpes zoster is increased with age, and among immunocompromised persons [Reference Grose1]. VZV transmission mainly occurs from direct contact, inhalation of aerosols from vesicular fluid of skin lesions of varicella or zoster, and possibly through infected respiratory secretions and its aerosols. The incubation period of VZV ranges from 10 to 21 days.
The epidemiology of chickenpox is less studied in tropical countries including India. Reports on chickenpox outbreaks in healthcare workers, hospital staff, unvaccinated villagers, schoolchildren and school staff have been published [Reference Balraj and John2–Reference Gupta, Gupta and Gupta11]. However, limited seroprevalence and surveillance studies are available from India.
A literature review documented that the VZV infection is common in adolescents and adults in a number of Asian countries including India. Age-related VZV seroprevalence pattern in these countries indicated that seroconversion in tropical countries occurs at a later age than in temperate countries [Reference Lee12]. Chickenpox vaccine is not available in the national immunisation schedule; however, the Indian Academy of Pediatrics recommended two doses of chickenpox vaccine at the age of 15 months and 4–6 years (http://www.iapindia.org). Presently, chickenpox vaccine is available as an optional vaccine but not in the Universal Immunisation Program of India.
Between 9th December 2016 and 12th February 2017 (42nd week of 2016 and 6th week of 2017), large numbers of chickenpox cases were observed in the tribal and industrial zone of Dadra and Nagar Haveli, India. To assess the characteristics and determinants of the disease, and implications of chickenpox cases in a crowded and congested place, an epidemiological investigation was undertaken.
Materials and methods
Outbreak setting
On the 49th week of 2016, the Silvassa block of Integrated Disease Surveillance Programme (IDSP) reported a rise in chickenpox cases from Rakholi and Surangi villages since the 42nd week of 2016. Subsequently, the IDSP deployed two rapid response teams for the investigation. An investigation was carried out for identifying the characteristics of the outbreak and associated risk factors along with possible control measures. Investigations were carried out up to 12th February 2017 (double the incubation period from the date of occurrence of the last case). There were no deaths observed during the active surveillance.
Rakholi and Surangi villages are located in the industrial zone situated in the Silvassa block of Dadra and Nagar Haveli and about 5.8 and 15.9 km respectively far from Silvassa city (a headquarter of health facility). These two villages are 11.5 km away and the villagers are occasionally visited each other during weekly bazaar/shopping. The total population of Rakholi is 9284 with 10.3% of the population between 0 and 5 years (62.3% males and 37.7% females), 12.3% between 6 and 10 years (36.8% males and 63.2% females) and 9.6% belonging to 11–15 years (58.5% males and 41.5% females) and 68.9% belonging to 16–60 years (63.6% males and 36.4% females). The overall population of Rakhloi village consists of 60.8% males (n = 5644) and 39.2% females (n = 3640).
Total population of Surangi village is 5891 with 11.8% of the population between 0 and 5 years (47.5% males and 52.5% females), 9.3% between 6 and 10 years (50% males and 50% females) and 9.4% belonging to 11–15 years (49.9% males and 50.1% females) and 67.2% belonging to 16–60 years (57.5% males and 42.5% females). The overall population of Surangi village consists of 55% males (n = 3241) and 45% females (n = 2650). Populations from both the villages were unimmunised for Chickenpox.
Case definition
An acute illness with diffuse (generalised) macular/papular/vesicular rash, AND Epidemiologic linkage to another probable or confirmed case, OR Laboratory confirmation by VZV-specific IgM antibodies detection or VZV DNA detection by PCR or isolation of chickenpox virus from a clinical specimen. The similar case definition was used for both children and adults (⩾15 years). The Medical Officer working at the Primary Health Centre (PHC) clinically diagnosed all the suspected cases. Clinical specimens (i.e. serum, blister/skin swab, urine and throat swabs) were collected from the cases and referred for the laboratory diagnosis.
Epidemiological investigations
On daily basis, suspected chickenpox cases were recorded during house-to-house visits, epidemiological information was collected using standard case investigation form and a line list of cases was maintained. Altogether, 80 and 69 clinically confirmed chickenpox cases were reported from the Rakholi and Surangi villages, respectively. The data were analysed by demographics, village and time from exposure to onset. The investigation team remained vigilant for 6 weeks after the last case was notified.
Laboratory investigations
Twenty-five serum samples were obtained from the suspected cases. Serum sample was not available from the 12-suspected cases but other alternative specimens (i.e. throat swabs, blister swabs and urine) were available for the laboratory testing. Overall, 21 specimens were collected from adult cases (⩾15 years) that consist of 13 males and eight females. Remaining 16 specimens were collected from the children that consist of six males and ten females. All these samples were subjected to VZV IgM and IgG antibody detection (NovaTec Immundiagnostica GmbH, Dietzenbach Germany) and results were interpreted according to the cut offs provided in the kit inserts.
Altogether, 17 specimens were processed for VZV DNA PCR (i.e. five serum samples, six blister swabs, three throat swabs and three urine specimens). The DNA was extracted from the vesicular swabs, throat swabs and serum sample using QIAmp® DNA Mini kit (Qiagen, Hilden, Germany) according to the manufacturer's instructions. The extracted DNA was eluted in 50 µl of elution buffer. The partial ORF-28 region of VZV was amplified using published primers [Reference Zhang13]. The PCR was performed in 50 µl reaction containing 5 µl of extracted DNA using EmeraldAmp® GT PCR MasterMix (TAKARA BIO INC, Japan). The reaction mixture consists of 25 µl of GT PCR MasterMix, 0.5 µl of each primer (concentration of 20 µM) and 19 µl of RNAase-free water. At first, the PCR mixture was heated at 94 °C for 3 min followed by 39 cycles at 94 °C for 30 s, 55 °C for 30 s and 72 °C for 45 s and a final extension at 72 °C for 3 min. The amplicons of 355 bp were visualised by gel electrophoresis in 2% agarose gel. In addition, PCR-positive clinical specimens were subjected to virus isolation using Vero and MRC-5 cells. The PCR products were sequenced using the same primers and the partial ORF-28 gene sequences were submitted to the GenBank under accession numbers (MF371116–MF371124).
Results
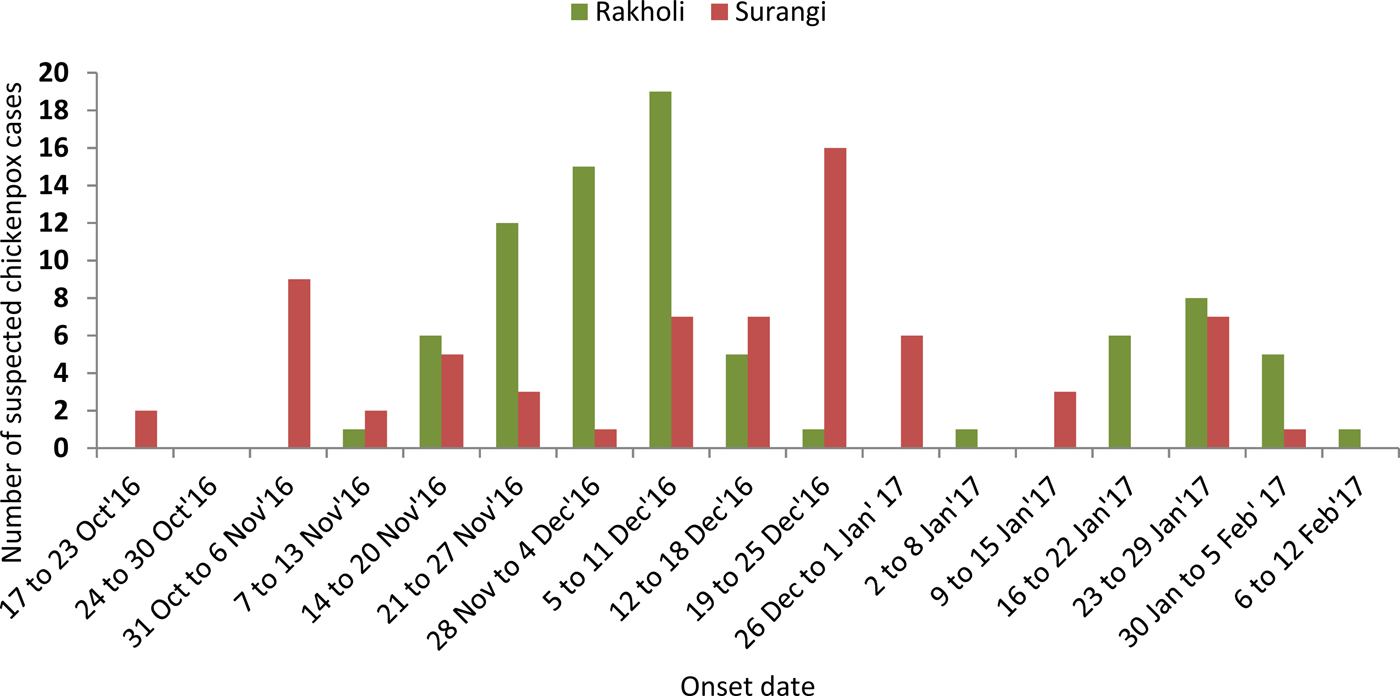
Between 9th December 2016 and 12th February 2017 (42nd week of 2016 and 6th week of 2017), 149 chickenpox cases were reported from Rakholi and Surangi villages with an attack rate of 4.5% and 19.2% (per 100 populations), respectively. An index case was a 25-year-old female that reported fever on 29 October 2016 and subsequently developed a skin rash after 2 days. Among the suspected cases, 96 were males (64.4%) and 53 were females (35.6%). The distribution of chickenpox cases is presented in Figure 1. This outbreak lasted for 3 months, without any major clinical complications.
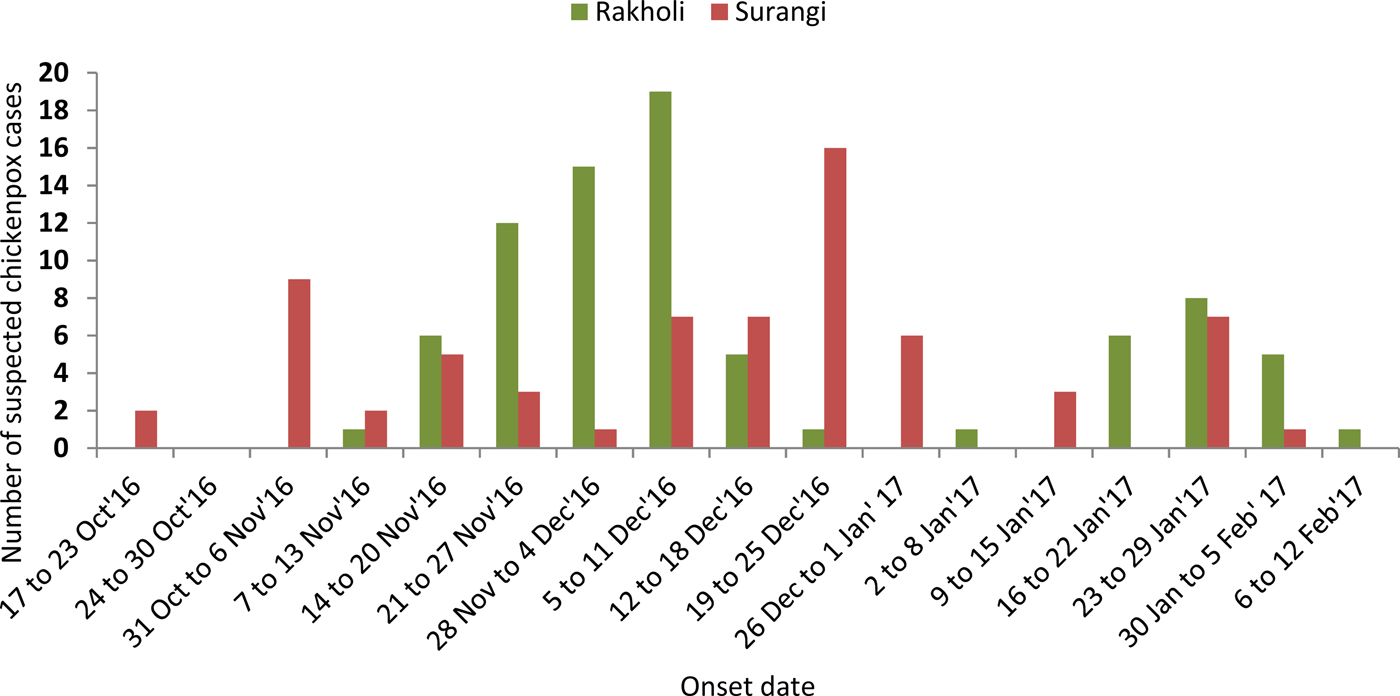
Fig. 1. The Epidemiological curve of the suspect cases of chickenpox reported in two Indian villages with high population density.
Although the overall age-range of the patients was wide, the majority of the cases were 21–25 years old (22.8%), followed by 21.5% in 0–5 years, 15.4% in 6–10 years, 2% in 11–15 years, 20.1% in 16–20 years, 13.4% in 26–30 years and the remaining 4.7% were >30 years old. This outbreak continued for 17 weeks yielding 149 clinical chickenpox cases. Precisely, the overall attack rate per 100 population in both villages were presented in Table 1.
Table 1. Suspected chickenpox cases and contacts from Rakholi and Surangi villages
a A sample had the equivocal result.
b Specimens were laboratory confirmed by IgM EIA or VZV DNA PCR.
The early symptoms in adolescents and adults are nausea (n = 16), loss of appetite (n = 124), aching muscles (n = 32) and headache (n = 48) followed by the characteristic rash (n = 149), malaise (n = 78) and a low-grade fever (n = 54) that signal the presence of the disease. All suspected cases recovered without any apparent complications. Typical symptoms of chickenpox were not reported in the close contacts.
Altogether, 22 suspected cases were laboratory confirmed (including one equivocal result) by VZV IgM EIA (NovaTec Immundiagnostica GmbH, Dietzenbach, Germany) and additional nine suspected cases were confirmed by VZV DNA PCR. Overall, 31 of 37 suspected cases were laboratory confirmed (Table 1). VZV DNA PCR was found positive in nine of 17 specimens collected from the suspected chickenpox cases. Altogether, six blister swabs, two urine specimens and one throat swab were positive with fever and vesicular rash onset ranging between 1 and 4 days, i.e. the interval between rash onset and specimen collection in the acute phase (Fig. 2).

Fig. 2. The VZV DNA PCR-positive specimens collected from the nine-chickenpox cases. DNA ladder (lanes 1 & 13); extraction control (lane 11); positive control (lane 12); blister swabs (lanes 2–4, 7, 9 & 10); urine specimens (lanes 5 & 8); Throat swab (lane 6).
Among 37 suspected cases with specimens collected, 21 (56.7%) were from adults (aged ⩾15 years) and 16 (43.2%) were from children; 90.5% of the 21 adult cases and 75% of 16 cases in children were laboratory confirmed. Fourteen of 18-suspected females and 16 of 19-suspected males were laboratory confirmed for chickenpox infection. All nine PCR-positive products were sequenced using both forward and reverse primers. A consensus sequence was analysed using BLAST resource available in the NCBI (www.ncbi.nlm.nih.gov). All sequences closely matched to (100% identical) the Human herpesvirus-3 isolate (Var/Cli/UK/Ves/2909/2013) from the UK that belongs to clade-1 viruses. The tissue culture fluids obtained after passaging (up to two passages) three blister swabs and a urine specimen showed the presence of VZV DNA by PCR; however, the distinct cytopathic effect was not observed in Vero and MRC-5 cells.
Discussion
For the first time, an outbreak of chickenpox has been confirmed by a combination of serological and molecular tools in the population residing in the tribal and industrial zone of Dadra and Nagar Haveli, India. Generally, the diagnosis of chickenpox is performed by the clinical presentations, so a number of specimens collected for the laboratory diagnosis are usually limited. Interestingly, a number of chickenpox cases were higher amongst the children compared with adults in the Rakholi village but were reverse in the Surangi village. This may be due to the fact that adult population may have an episode of chickenpox at childhood. In both villages, a number of male cases were higher than female cases despite varied attack rates per 100 populations. However, the attack rate was higher in males (22.1%) than females (12.6%) in the Surangi village whereas the attack rate was slightly higher in females (5.9%) than males (3.7%) in the Rakholi village (Supplementary Table S1). For the isolation of circulating chickenpox virus, a clinical specimen passaged on 24 h old monolayer of Vero and MRC-5 cells. However, a distinct cytopathic effect could not be evident in the Vero and MRC-5 cells but VZV DNA was detected in the cell suspension up to two passages.
The epidemiological and laboratory investigations suggest that outbreak spreads due to close and congested living places in the tribal and industrial zones of Dadra and Nagar Haveli (UT) areas. In an outbreak setting, rapid and more sensitive detection tools (such as VZV DNA PCR) would have added advantage for the timely isolation of cases that would be ultimately useful for minimising the number of cases. Previously, an application of VZV DNA PCR was showed to investigate a chickenpox outbreak from Chandigarh, India [Reference Singh10]. However, virus sequencing cum genotyping data were not available. In the present study, the partial sequencing of ORF-28 gene of VZV was performed and a circulation of clade-1 viruses was documented. Therefore, increased awareness amongst the clinicians, epidemiologists and healthcare staff working in the remote areas is crucial for the rapid diagnosis and ultimately for the isolation of chickenpox cases. Previously, chickenpox outbreak was reported in Velugam village situated nearby the Surangi village resulted in 75 cases in the month of January 2015. The distance between these two villages is 5.3 km (IDSP unpublished data).
In general, surveillance team had difficulties in the specimen collection mainly due to refusals by the patients. The migratory population and low literacy rate of the local tenant are likely reason for the poor sanitation and unhygienic conditions in the tribal belt/zone. This may be the contributing factors for clustering of the chickenpox cases. In addition, different culture and languages may be another barrier for undertaking the control measures in the field.
During investigations, the outpatient camp was organised in the affected areas and suspected cases were isolated to reduce the morbidity of the disease. In addition, symptomatic treatment has been provided to the clinical cases. Information about the mode of transmission of the disease has been circulated to the local residents and precautionary measures were suggested. Furthermore, intensified health awareness about the vaccine-preventable diseases and routine immunisation amongst the migratory population may be useful for the control of chickenpox. It was observed that very poor air ventilation and sanitation of affected tenants suffered more during the transmission period. The team visited a local school and Anganwadi (play school) situated in the tribal setting and interviewed managers and the workers of the affected industrial area. The team assessed complete campus for the hygiene, sanitation and home isolation.
In conclusion, this investigation provides detail information about the chickenpox outbreak in the tribal and industrial setting from India. Since chickenpox is vaccine-preventable disease, the morbidity and mortality associated with chickenpox may be reduced in the tribal population. Furthermore, study emphasises need to investigate more chickenpox outbreaks from the tribal and other population from India.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0950268818000201.
Acknowledgements
The authors would like to thank the Director, NIV Pune and State Program Officer IDSP, Union Territory of Dadra and Nagar Haveli for the permission to undertake this study and financial support provided from NIV intramural funds. Authors are grateful to the participants from Rakholi and Surangi villages and Medical staff from Primary Health Centers. Authors thank Dr K. Alagarasu (NIV, Pune) for the critical evaluation of the paper, especially for English language editing. There was no specific fund received for this work.
Conflict of interest
None.
Informed consent and ethical approvals
Informed consent has been taken from all study participants. The institutional Human Ethical Committee approved this project.