Introduction
The number of refugees worldwide has more than doubled over the past decade (UNHCR, 2022). An estimated 32% of refugees live with depression, and 31% with posttraumatic stress disorder (PTSD) (Patanè et al., Reference Patanè, Ghane, Karyotaki, Cuijpers, Schoonmade, Tarsitani and Sijbrandij2022). The prevalence of clinical depression and PTSD in displaced Syrians has been estimated to be 41% and 43%, respectively (Peconga and Høgh Thøgersen, Reference Peconga and Høgh Thøgersen2020). The availability of (suitable) mental health services for refugees remains, however, low (Satinsky et al., Reference Satinsky, Fuhr, Woodward, Sondorp and Roberts2019). The majority of refugees are hosted by low- and middle-income countries where health systems are already under-resourced (Cratsley et al., Reference Cratsley, Brooks and Mackey2021), whereas health systems of higher income countries are typically limited by waitlists, and a lack of professionals speaking other languages and limited interpretation services (Satinsky et al., Reference Satinsky, Fuhr, Woodward, Sondorp and Roberts2019). As a result, many refugees in need of services are untreated (Fuhr et al., Reference Fuhr, Acarturk, McGrath, Ilkkursun, Sondorp, Sijbrandij, Ventevogel, Cuijpers, McKee and Roberts2020).
To address the mental health treatment gap (i.e., the proportion of individuals with a mental health condition that is not being treated for it) worldwide, the World Health Organization (WHO) developed a series of potentially scalable psychological interventions that can be implemented by non-specialists (WHO, 2017). Problem Management Plus (PM+) is a concise, transdiagnostic intervention aimed at alleviating symptoms of common mental disorders (CMDs) in individuals affected by adversity such as armed conflict (WHO, 2018). It consists of five sessions that cover skills related to managing stress, problem solving, behavioural activation and accessing social support (Dawson et al., Reference Dawson, Bryant, Harper, Kuowei Tay, Rahman, Schafer and Van Ommeren2015). Research has demonstrated that PM+ delivered to individuals and groups in low-income settings has beneficial mental health effects 3 months after receipt of the intervention (Reference Bryant, Bawaneh, Awwad, Al-Hayek, Giardinelli, Whitney, Jordans, Cuijpers, Sijbrandij, Ventevogel, Dawson and Akhtar2022a; Bryant et al., Reference Bryant, Schafer, Dawson, Anjuri, Mulili, Ndogoni, Koyiet, Sijbrandij, Ulate, Harper Shehadeh, Hadzi-Pavlovic and van Ommeren2017; Jordans et al., Reference Jordans, Kohrt, Sangraula, Turner, Wang, Shrestha, Ghimire, Van’t Hof, Bryant, Dawson, Marahatta, Luitel and Van Ommeren2021; Rahman et al., Reference Rahman, Hamdani, Awan, Bryant, Dawson, Khan, Mukhtar-ul-haq Azeemi, Akhtar, Nazir, Chiumento, Sijbrandij, Wang, Farooq and Van Ommeren2016, Reference Rahman, Khan, Hamdani, Chiumento, Akhtar, Nazir, Nisar, Masood, Din, Khan, Bryant, Dawson, Sijbrandij, Wang and Van Ommeren2019; Schäfer et al., Reference Schäfer, Thomas, Lindner and Lieb2023). In high-income settings, non-specialist (or ‘task-shared’) interventions such as PM+ could be useful as a first step in a stepped-care model to scale up mental healthcare for refugees (Sijbrandij et al., Reference Sijbrandij, Acarturk, Bird, Bryant, Burchert, Carswell, de Jong, Dinesen, Dawson, El Chammay, van Ittersum, Jordans, Knaevelsrud, McDaid, Miller, Morina, Park, Roberts, van Son and Cuijpers2017). A recent study also demonstrated the effectiveness of individual PM+ for refugees over the same time period in a high-income setting (de Graaff et al., Reference de Graaff, Cuijpers, Twisk, Kieft, Hunaidy, Elsawy, Gorgis, Bouman, Lommen, Acarturk, Bryant, Burchert, Dawson, Fuhr, Hansen, Jordans, Knaevelsrud, McDaid, Morina and Sijbrandij2023).
Although the evidence-base for potentially scalable interventions such as PM+ is growing, we lack evidence on whether such brief interventions (for refugees) can also have mental health benefits over the long term. A meta-analysis of trials examining the effects of psychosocial interventions for refugees and asylum seekers demonstrated intervention effects for depression, anxiety and PTSD directly after the intervention and at follow-up (any assessment 1 month after the intervention or longer). However, only 8 out of 26 studies included follow-up assessments longer than 3 months after the intervention (Turrini et al., Reference Turrini, Purgato, Acarturk, Anttila, Au, Ballette, Bird, Carswell, Churchill, Cuijpers, Hall, Hansen, Kösters, Lantta, Nosè, Ostuzzi, Sijbrandij, Tedeschi, Valimaki and Barbui2019). The first study that investigated long-term effects of group PM+ showed that initial treatment gains at 3 months were not sustained at 12-month follow-up among refugees within a closed refugee camp in Jordan (Bryant et al., Reference Bryant, Bawaneh, Awwad, Al-Hayek, Giardinelli, Whitney, Jordans, Cuijpers, Sijbrandij, Ventevogel, Dawson and Akhtar2022b). Other research on PM+ thus far has been limited to the analysis of 3-month follow-up data (Reference Bryant, Bawaneh, Awwad, Al-Hayek, Giardinelli, Whitney, Jordans, Cuijpers, Sijbrandij, Ventevogel, Dawson and Akhtar2022a; Bryant et al., Reference Bryant, Schafer, Dawson, Anjuri, Mulili, Ndogoni, Koyiet, Sijbrandij, Ulate, Harper Shehadeh, Hadzi-Pavlovic and van Ommeren2017; de Graaff et al., Reference de Graaff, Cuijpers, Twisk, Kieft, Hunaidy, Elsawy, Gorgis, Bouman, Lommen, Acarturk, Bryant, Burchert, Dawson, Fuhr, Hansen, Jordans, Knaevelsrud, McDaid, Morina and Sijbrandij2023; Jordans et al., Reference Jordans, Kohrt, Sangraula, Turner, Wang, Shrestha, Ghimire, Van’t Hof, Bryant, Dawson, Marahatta, Luitel and Van Ommeren2021; Rahman et al., Reference Rahman, Hamdani, Awan, Bryant, Dawson, Khan, Mukhtar-ul-haq Azeemi, Akhtar, Nazir, Chiumento, Sijbrandij, Wang, Farooq and Van Ommeren2016, Reference Rahman, Khan, Hamdani, Chiumento, Akhtar, Nazir, Nisar, Masood, Din, Khan, Bryant, Dawson, Sijbrandij, Wang and Van Ommeren2019).
The randomised controlled trial (RCT) on individual PM+ for Syrian refugees in the Netherlands demonstrated that at 3-month follow-up, PM+ led to greater reductions in depression, anxiety, symptoms of PTSD and self-identified problems, but not functional impairment (de Graaff et al., Reference de Graaff, Cuijpers, Twisk, Kieft, Hunaidy, Elsawy, Gorgis, Bouman, Lommen, Acarturk, Bryant, Burchert, Dawson, Fuhr, Hansen, Jordans, Knaevelsrud, McDaid, Morina and Sijbrandij2023). The current study reports on the 12-month follow-up (i.e., 12 months after baseline) of this trial with the aim to investigate whether PM+ reduces psychological distress (depression/anxiety combined), depression, anxiety, PTSD symptoms, functional impairment and self-identified problems at the long-term.
Methods
Design
A two-arm, single-blind RCT was conducted in the Netherlands at the Vrije Universiteit Amsterdam (VU) in collaboration with i-Psy mental healthcare. This study was undertaken within an international research consortium investigating scalable psychological interventions among Syrian refugees in Europe and the Middle East (Sijbrandij et al., Reference Sijbrandij, Acarturk, Bird, Bryant, Burchert, Carswell, de Jong, Dinesen, Dawson, El Chammay, van Ittersum, Jordans, Knaevelsrud, McDaid, Miller, Morina, Park, Roberts, van Son and Cuijpers2017). The trial was approved by the Research Ethics Review Committee at VU Medical Center (NL61361.029.17) and prospectively registered in the Netherlands Trial Registry (#7552). The Consolidated Standards of Reporting Trials (CONSORT) guideline can be found in Supplement A (Schulz et al., Reference Schulz, Altman and Moher2010).
Procedures
Adult (≥18 years) Arabic-speaking Syrian refugees were recruited through community centres, non-governmental organisations, reception centres, language schools and social media. By ‘Syrian refugees’, we refer to individuals from Syria who requested asylum after the start of the war in 2011 regardless of current resident status. Oral and written informed consent were obtained from all participants before screening (with a required 1 week ‘reflection time’). Inclusion criteria were psychological distress and functional impairment determined by a score ≥16 on the 10-item Kessler Psychological Distress Scale (K10) (Kessler et al., Reference Kessler, Andrews, Colpe, Hiripi, Mroczek, Normand, Walters and Zaslavsky2002; Sulaiman-Hill and Thompson, Reference Sulaiman-Hill and Thompson2010) and a score ≥17 on the 12-item WHO Disability Assessment Schedule (WHODAS 2.0) (WHO, Reference Üstun, Kostansjek, Chatterji and Rehm2010) (cf. Bryant et al., Reference Bryant, Schafer, Dawson, Anjuri, Mulili, Ndogoni, Koyiet, Sijbrandij, Ulate, Harper Shehadeh, Hadzi-Pavlovic and van Ommeren2017; Rahman et al., Reference Rahman, Hamdani, Awan, Bryant, Dawson, Khan, Mukhtar-ul-haq Azeemi, Akhtar, Nazir, Chiumento, Sijbrandij, Wang, Farooq and Van Ommeren2016).
Exclusion criteria were acute medical conditions, imminent suicide risk (PM+ manual suicidality assessment), expressed acute needs/protection risks, indications of severe mental disorders (e.g., psychotic disorders), cognitive impairment (e.g., severe intellectual disability) as assessed by the PM+ manual observation checklist (World Health Organization, 2018) or current receipt of specialist mental healthcare. Participants meeting exclusion criteria were referred to the general practitioner/specialist services as required.
Participants were assessed at baseline, 1 week and 3 months after the intervention and 12 months after baseline (i.e., 10.5 months after the intervention). Assessments included Arabic-language questionnaires on demographics, clinical outcomes, daily functioning, stressful events and health service utilisation (de Graaff et al., Reference de Graaff, Cuijpers, Acarturk, Bryant, Burchert, Fuhr, Huizink, de Jong, Kieft, Knaevelsrud, McDaid, Morina, Park, Uppendahl, Ventevogel, Whitney, Wiedemann, Woodward and Sijbrandij2020a). Arabic-speaking assessors contacted participants for each assessment to share a personalized link to complete the online questionnaires using the questionnaire tool Survalyzer and to complete a phone-based interview on health service utilisation. Lower-literate participants were assisted by the audio-support function in Survalyzer or assistance from the assessor. Renumeration was 8.50 Euros for each follow-up assessment (totalling to 25.50 euros). Assessors were trained on questionnaire administration, general interview techniques, CMDs, psychological first aid and research ethics. Serious adverse events (SAEs) were recorded and monitored throughout the study.
Following baseline, participants were randomised on a 1:1 basis into PM+ in addition to care as usual (PM+/CAU) or CAU alone. An independent researcher not otherwise involved in the study generated a randomisation list with permuted block sizes of 4-6-8 in R (R Core Team, 2021), and a researcher not involved in the outcome assessments informed participants about the randomisation outcome using sealed opaque envelopes. Assessors completing outcome assessments were blinded to group allocation. Success of blinding was evaluated after each assessment (i.e., assessors indicated whether group allocation was revealed).
Conditions
Detailed information on the intervention arms have been reported elsewhere (Dawson et al., Reference Dawson, Bryant, Harper, Kuowei Tay, Rahman, Schafer and Van Ommeren2015; de Graaff et al., Reference de Graaff, Cuijpers, McDaid, Park, Woodward, Bryant, Fuhr, Kieft, Minkenberg and Sijbrandij2020b, Reference de Graaff, Cuijpers, Twisk, Kieft, Hunaidy, Elsawy, Gorgis, Bouman, Lommen, Acarturk, Bryant, Burchert, Dawson, Fuhr, Hansen, Jordans, Knaevelsrud, McDaid, Morina and Sijbrandij2023). In brief, individual PM+ is a five-session intervention rooted in cognitive behavioural therapy and problem solving therapy delivered consecutively on a weekly basis with each session lasting 90 minutes. In the first four sessions, participants learn strategies for relaxation (i.e., slow breathing exercise), problem management, behavioural activation and accessing social support. Session five focuses on relapse prevention. Helpers were Arabic-speaking Syrian refugees with no formal training in mental health. Helpers completed an 8-day training in PM+ (including training on CMDs, basic counselling skills, delivery of the strategies and self-care) and received ongoing, weekly group supervision by trained PM+ supervisors (psychologists from i-Psy mental healthcare, VU and University of Groningen) during the trial. Sessions were delivered in the community (e.g. community centres, language schools), at VU, i-Psy mental healthcare or reception centres for asylum seekers. Following the implementation of COVID-19 restrictive measures (first partial lockdown in March 2020), participants were given the option for in-person or video call sessions. CAU comprised any (mental) health service available to refugees in the Netherlands (e.g., accessible through a general practitioner).
Outcome measures
Psychological distress was measured by the Hopkins Symptom Checklist (HSCL-25). Items are scored on a 1–4 Likert scale with higher scores indicating worse symptomatology. For analysis, we used the mean of the items for the total scale and subscales. Probable depression and anxiety were defined by scores of 2.10 and 2.00 on the respective subscales (Mahfoud et al., Reference Mahfoud, Kobeissi, Peters, Araya, Ghantous and Khoury2013). Functional impairment was measured by the 12-item WHODAS 2.0 (World Health Organization, Reference Üstun, Kostansjek, Chatterji and Rehm2010). Items are scored on a 1–5 scale (total range, 12–60). PTSD symptoms were assessed by the 20-item PTSD Checklist for DSM-5 (PCL-5) (Ibrahim et al., Reference Ibrahim, Ertl, Catani, Ismail and Neuner2018). Items are scored on a 0–4 scale (total range, 0–80), with a score of 33 or higher as indicator of probable PTSD (Bovin et al., Reference Bovin, Marx, Weathers, Gallagher, Rodriguez, Schnurr and Keane2016). Self-identified problems were measured using the Psychological Outcomes Profiles (PSYCHLOPS) on a 0–5 scale (total range, 0–20) (Psychological Outcomes Profiles; PSYCHLOPS) (Ashworth et al., Reference Ashworth, Shepher, Christey, Matthews, Wright, Parmentier, Robinson and Godfrey2004). All outcome assessments were administered at each time point.
Other measures
Sociodemographic data included gender, age, living situation (i.e., living in a reception centre, independent housing in the community or other), education, marital status, work status, refugee status and time of displacement assessed through WHODAS 2.0. The number of potentially traumatic events was assessed with a dichotomously scored 27-item checklist (de Graaff et al., Reference de Graaff, Cuijpers, Acarturk, Bryant, Burchert, Fuhr, Huizink, de Jong, Kieft, Knaevelsrud, McDaid, Morina, Park, Uppendahl, Ventevogel, Whitney, Wiedemann, Woodward and Sijbrandij2020a). Post-migration stressors were assessed with the 17-item Post-Migration Living Difficulties (PMLD) checklist (Nickerson et al., Reference Nickerson, Bryant, Schnyder, Schick, Mueller and Morina2015). The total score was calculated by a count of all items with a score of at least 2 (moderately serious problem) (total score range, 0–17). Healthcare use was assessed using the Client Service Receipt Inventory (CSRI) (Chisholm et al., Reference Chisholm, Knapp, Knudsen, Amaddeo, Gaite and Van Wijngaarden2000) adapted for this study.
Statistical analysis
Power calculations for the trial were performed for the primary endpoint at 3-month follow-up. These were based on the results of the pilot RCT among Syrian refugees (de Graaff et al., Reference de Graaff, Cuijpers, McDaid, Park, Woodward, Bryant, Fuhr, Kieft, Minkenberg and Sijbrandij2020b). No power calculations were performed for the 12-month follow-up, but the analysis was pre-planned and reported in the study protocol (de Graaff et al., Reference de Graaff, Cuijpers, Acarturk, Bryant, Burchert, Fuhr, Huizink, de Jong, Kieft, Knaevelsrud, McDaid, Morina, Park, Uppendahl, Ventevogel, Whitney, Wiedemann, Woodward and Sijbrandij2020a).
To measure baseline differences between the two conditions (i.e., PM +/CAU vs CAU) as well as between the retained and lost to 12-month follow-up sample, t-tests were conducted for continuous variables and Chi-squared tests for categorical variables. Additionally, a t-test was performed to test for any differences in the number of participants who reported having accessed mental healthcare services at 12-month follow-up. We also calculated the total number of contacts participants had with any mental health service. Mental health services were defined as services provided by a psychiatrist, psychologist, psychiatric nurse, self-help group, consultation centre, psychiatric crisis service, psychiatric outpatient service, mental health ward and long-stay psychiatric ward.
We performed linear mixed models (LMMs) in R on the intention-to-treat sample to estimate treatment effect at 12-month follow-up. The model included three dummy variables for time (i.e., post-assessment, 3-month follow-up and 12-month follow-up), three interaction terms for condition*time and a random intercept on subject level. In this model, the intercept reflects the baseline value for both conditions, because we did not include the main effect of condition to adjust for baseline differences between conditions (Twisk et al., Reference Twisk, Rijnhart, Hoekstra, Schuster, ter Wee and Heymans2020). Regression coefficients of the interaction terms of condition with each follow-up time point are the effect estimates (i.e., mean difference between the two conditions). A separate model was estimated for the treatment effect at the whole follow-up period (i.e., the three follow-up time points on average).
We conducted LMMs for all outcomes, including psychological distress, depression, anxiety, functional impairment, symptoms of PTSD and self-identified problems. We conducted the same analyses with relevant covariates measured at baseline (i.e., gender, age, education, work status, number of potentially traumatic events, post-migration stressors and probable depression, anxiety and PTSD) to estimate covariate-adjusted models. These variables were also investigated as potential moderators (i.e., added in interaction with condition at 12-month follow-up) to the LMM of the HSCL-25 total score. Cohen’s d was calculated by the difference in least square means between conditions divided by the raw (i.e., as measured) pooled standard deviation (SD) at that assessment. A positive value for Cohen’s d indicates a beneficial effect for the PM+/CAU group in comparison to the CAU group.
Sensitivity analyses were performed including only participants retained at 12-month follow-up (completers) and including only participants of the PM+/CAU group who completed at least four sessions (per protocol) (de Graaff et al., Reference de Graaff, Cuijpers, McDaid, Park, Woodward, Bryant, Fuhr, Kieft, Minkenberg and Sijbrandij2020b).
Across all analyses, two-tailed tests were reported where p < 0.05 indicated statistical significance.
Results
Participants
Participants were enrolled between March 2019 and December 2021 with the final 12-month assessments conducted in December 2022. There were 758 individuals who expressed interest in the project, of whom 236 signed informed consent and were screened. Of those, 206 met the inclusion criteria and completed baseline. Participants were randomised into PM+/CAU (n = 103) or CAU (n = 103). At inclusion, the sample was on average 36.5 years old (range, 18–69, SD = 11.7) and the majority (61.7%) were men (see Table 1).
Table 1. Baseline characteristics

PTSD = posttraumatic stress disorder.
a n = 200.
b Based on HSCL-25 depression subscale cut-off ≥2.10.
c Based on HSCL-25 anxiety subscale cut-off ≥2.00.
d Based on PCL-5 ≥33.
We re-assessed 169 participants (82%) at 12-month follow-up, with 22 participants in PM+/CAU and 15 participants in CAU lost to follow-up (see flowchart in Figure 1). Of those, 20 (9.7%) refused to participate and 17 (8.3%) could not be reached. The loss to follow-up sample did not differ from the retained sample in terms of baseline characteristics (see Supplement B). At 12-month follow-up, blinding was successful in the assessment of 152 (89.9%) participants.

Figure 1. CONSORT flowchart.
At 12-month follow-up, participants had on average spent 56 months (SD = 22.8, range, 11–109 months) in the Netherlands. The most frequently reported post-migration stressors were worries about family back home (65.7%), unable to return home in case of emergency (52.7%) and difficulties learning the Dutch language (50.9%) (see Table 2). The full sample reported an average of 5.1 (SD = 3.7) post-migration stressors at 12-month follow-up, which was significantly lower compared to the average number of 7.0 (SD = 3.6) post-migration stressors reported at baseline (estimate for main effect of time −1.63; 95% CI −2.208 to −1.042; p < 0.0001). There was no significant interaction between time and condition for the number of post-migration stressors reported at 12-month follow-up (mean difference −0.21; 95% CI −1.016 to 0.597; p = 0.61). The resident status of participants had also changed over the course of the trial. At baseline, 55/194 participants (28.3%) reported having a permanent resident permit or Dutch citizenship, 12 months later this was reported by 81/168 participants (48.2%).
Table 2. Post-migration stressors and healthcare use reported at 12-month follow-up
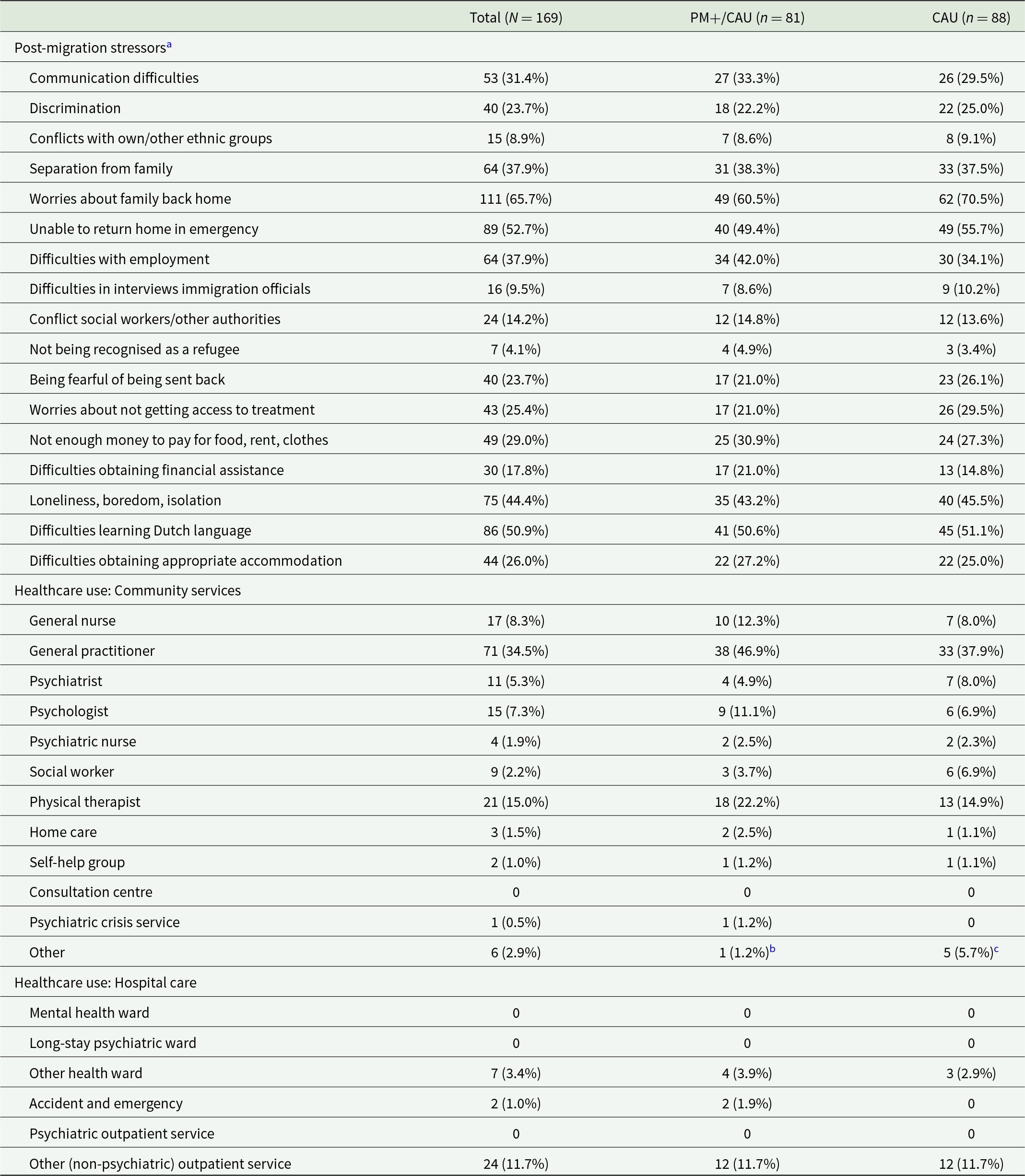
Percentages represent valid percentages (i.e., based on number of retained participants).
a Three participants in the CAU group did not complete the questionnaire.
b Unclear n = 1.
c Dentist n = 3; public health centre n = 1; dietician n = 1.
Table 2 provides an overview of the different types of (mental) healthcare services that participants accessed in the three months preceding the 12-month follow-up. There was no statistically significant difference between the two groups in terms of the number of participants who accessed mental health services (t = −0.251, p = 0.8). In the PM+/CAU group, 11 participants (10.7%) had accessed mental health services with an average of 9.6 contacts (SD = 9.9; range, 1–30), while in the CAU group, 13 participants (12.6%) had accessed mental health services with an average of 5.9 contacts (SD = 4.8; range, 1–18).
Among participants in the PM+/CAU group, 85 (82.5%) completed all five sessions, two (1.9%) stopped after four sessions, three (2.9%) after three sessions, six (5.8%) after two sessions, six (5.8%) after one session and one (1.0%) did not complete any session. Due to COVID-19 restrictions, 64 (62.8%) participants completed the sessions in person, 25 (24.5%) online only (i.e., video calls) and 13 (12.7%) completed both in person and online (i.e., hybrid).
Intervention effects
The LMM analysis (see Table 3) showed that the intervention effect on the HSCL-25 total score (depression and anxiety combined) found at the primary endpoint at 3-month follow-up was sustained. At 12-month follow-up, the PM+/CAU group had a significantly larger reduction on the HSCL-25 total score compared with CAU (mean difference −0.17; 95% CI −0.310 to −0.027; p = 0.01; Cohen’s d = 0.28). The average scores for each condition on all outcomes are visualized in Figure 2.

Figure 2. Group scores of primary and secondary outcomes across all time points. (a) HSCL-25 total, (b) HSCL depression, (c) HSCL anxiety, (d) PCL-5 PTSD symptoms, (e) WHODAS 2.0 functional impairment and (f) PSYCHLOPS self-identified problems.
Table 3. Summary statistics and results from the mixed-model analyses

LS mean = Least Squares mean; PM+/CAU = Problem Management Plus in addition to care as usual; CAU = care as usual alone.
a This is the overall effect of condition on average over the two follow-up assessments
b Effect sizes were calculated using the difference in least square means between conditions divided by the raw pooled SD at that assessment. A positive value indicates a beneficial effect for the PM +/CAU group in comparison to the CAU group.
c Covariates included in these models are gender, age, education, marital status, work status and probable depression, anxiety and PTSD assessed at baseline, and trauma exposure and post-migration living difficulties assessed at baseline and 12-month follow-up.
We found a significantly larger reduction on HSCL anxiety in favour of the PM+/CAU group (−0.20; 95% CI −0.344 to −0.047; p = 0.01; d = 0.31), indicating that the intervention effect on anxiety at the primary endpoint was sustained over time. We did not find a significant difference between conditions on HSCL depression (−0.15; 95% CI −0.310 to 0.001; p = 0.05; d = 0.23). PM +/CAU also did not outperform CAU at 12-month follow-up on the PCL-5 (−0.80; 95% CI −4.504 to 2.913; p = 0.67; d = 0.05), WHODAS 2.0 (−0.42; 95% CI −2.414 to 1.565; p = 0.67; d = 0.05) and PSYCHLOPS (−0.39; 95% CI −1.606 to 0.836; p = 0.53; d = 0.09). This means that the short-term intervention effects on PTSD and self-identified problems at 3-month follow-up were no longer observed 12 months after baseline.
Covariate-adjusted models showed that the intervention effects at 12-month follow-up on HSCL-25 total and HSCL anxiety became less strong and were no longer significant (−0.13; 95% CI −0.255 to 0.005; p = 0.06; d = 0.21 and −0.14; 95% CI −0.277 to 0.000; p = 0.05; d = 0.22). The models for the other outcomes were consistent with the primary LMMs (Table 3).
Exploratory moderation analyses of the HSCL-25 total score showed a significant moderation of baseline depression (p = 0.007), with a stronger treatment effect for participants scoring above cut-off on the depression subscale at baseline (−0.25; 95% CI −0.395 to −0.096; p = 0.001; d = 0.53), than for participants scoring below cut-off on the depression subscale at baseline (0.01; 95% CI −0.446 to −0.071; p = 0.8; d = −0.05). Similarly, baseline anxiety (p < 0.0001) and PTSD (p = 0.0006) were significant moderators of the treatment effect on HSCL-25 total score, with a stronger effect for participants scoring above cut-off on anxiety (−0.30; 95% CI −0.456 to −0.140; p = 0.0002; d = 0.62) and PTSD (−0.33; 95% CI −0.495 to −0.169; p < 0.0001; d = 0.69), than participants scoring below cut-off on anxiety (0.08; 95% CI −0.079 to 0.248; p = 0.3; d = −0.22) and PTSD (0.02; 95% CI −0.176 to 0.143; p = 0.8; d = 0.04). We also found a negative effect modification with the number of potentially traumatic events at baseline (p = 0.004) and the number of post-migration stressors at baseline (p = 0.02), indicating that the effect of the intervention at 12-month follow-up became stronger with a higher number of potentially traumatic events and a higher number of post-migration stressors reported at baseline. Lastly, there was a significant moderation with gender (p = 0.03), with a stronger treatment effect for men (−0.23; 95% CI −0.385 to −0.081; p = 0.003; d = 0.38) than for women (−0.01; 95% CI −0.217 to 0.191; p = 0.9; d = 0.02). Participant characteristics such as age, educational level, marital status and work status did not moderate treatment effects (all p ≥ 0.05).
Sensitivity analyses of participants retained at 12-month follow-up and the per protocol sample showed that results were consistent with the primary LMMs (Supplements C and D). An exploratory subgroup analysis of the different PM+ delivery formats showed that participants who took in-person sessions (n = 64) had significantly lower HSCL-25 total scores relative to CAU at 12-month follow-up (−0.23; 95% CI −0.388 to −0.062; p = 0.007, d = 0.38), while participants who took video/hybrid PM+ sessions (n = 38) did not (−0.09; 95% CI −0.272 to 0.099; p = 0.36, d = 0.15) (Supplement E).
Four SAEs unlikely related to study procedures were reported (two in each group).
Discussion
Against the backdrop of the rising number of forcibly displaced people worldwide, there is an urgent need to scale up psychological interventions for refugees and other displaced people. Although evidence supporting the short-term effectiveness of scalable interventions such as PM+ is growing (Bryant et al., Reference Bryant, Schafer, Dawson, Anjuri, Mulili, Ndogoni, Koyiet, Sijbrandij, Ulate, Harper Shehadeh, Hadzi-Pavlovic and van Ommeren2017; de Graaff et al., Reference de Graaff, Cuijpers, Twisk, Kieft, Hunaidy, Elsawy, Gorgis, Bouman, Lommen, Acarturk, Bryant, Burchert, Dawson, Fuhr, Hansen, Jordans, Knaevelsrud, McDaid, Morina and Sijbrandij2023; Rahman et al., Reference Rahman, Hamdani, Awan, Bryant, Dawson, Khan, Mukhtar-ul-haq Azeemi, Akhtar, Nazir, Chiumento, Sijbrandij, Wang, Farooq and Van Ommeren2016), little is known about their long-term effectiveness (Bryant et al., Reference Bryant, Bawaneh, Awwad, Al-Hayek, Giardinelli, Whitney, Jordans, Cuijpers, Sijbrandij, Ventevogel, Dawson and Akhtar2022b). In the current study, we investigated whether PM+/CAU had beneficial effects on psychological distress, anxiety, depression, PTSD symptoms, functional impairment and self-identified problems at 1-year follow-up compared to CAU only in Syrian refugees living in the Netherlands.
A key finding was that PM+ had small but significant effects on the reduction of psychological distress and anxiety at 12-month follow-up. This is an important finding for scale-up given that PM+ was delivered by non-specialists in only five sessions. To date, there is limited evidence for the effectiveness of task-shared interventions (Karyotaki et al., Reference Karyotaki, Araya, Kessler, Waqas, Bhana, Rahman, Matsuzaka, Miguel, Lund, Garman, Nakimuli-Mpungu, Petersen, Naslund, Schneider, Sikander, Jordans, Abas, Slade, Walters and Patel2022; Singla et al., Reference Singla, Kohrt, Murray, Anand, Chorpita and Patel2017) and of psychological interventions examined among refugees and asylum seekers (Thompson et al., Reference Thompson, Vidgen and Roberts2018; Turrini et al., Reference Turrini, Tedeschi, Cuijpers, Del Giovane, Kip, Morina, Nosè, Ostuzzi, Purgato, Ricciardi, Sijbrandij, Tol and Barbui2021) beyond immediate post-assessment or 3-month follow-up. Although the gains on psychological distress were significant at 12 months, they were not as strong as what was found at 3-month follow-up (i.e., a reduction from d = 0. 41 at 3 months to d = 0.28 at 12 months) (de Graaff et al., Reference de Graaff, Cuijpers, Twisk, Kieft, Hunaidy, Elsawy, Gorgis, Bouman, Lommen, Acarturk, Bryant, Burchert, Dawson, Fuhr, Hansen, Jordans, Knaevelsrud, McDaid, Morina and Sijbrandij2023), and became less strong and no longer significant when adjusted for covariates.
There was no statistically significant difference in depression scores at 12-month follow-up. That means that the initial treatment gains directly after the intervention and 3 months later (de Graaff et al., Reference de Graaff, Cuijpers, Twisk, Kieft, Hunaidy, Elsawy, Gorgis, Bouman, Lommen, Acarturk, Bryant, Burchert, Dawson, Fuhr, Hansen, Jordans, Knaevelsrud, McDaid, Morina and Sijbrandij2023) were not sustained. However, it must be noted that this study was not powered for the 12-month follow-up and depression scores at 12 months were in favour of the PM+/CAU group. Moderation analysis showed that the reduction in psychological distress (i.e., depression and anxiety combined) was significant for men but not for women. It is unclear why women have no long-term benefits of PM+. Social factors may play a role or women’s vulnerability for a higher symptom burden over time (Musliner et al., Reference Musliner, Munk-Olsen, Eaton and Zandi2016). Additional support after PM+ such as booster sessions may help to sustain initial treatment effects, especially given the evidence for the long-term efficacy of problem-solving therapy on depression (Cuijpers et al., Reference Cuijpers, Quero, Noma, Ciharova, Miguel, Karyotaki, Cipriani, Cristea and Furukawa2021). PM+ may also be considered as a first step in a stepped-care model, whereby individuals who do not benefit from this brief intervention can be referred to specialist care (Sijbrandij et al., Reference Sijbrandij, Acarturk, Bird, Bryant, Burchert, Carswell, de Jong, Dinesen, Dawson, El Chammay, van Ittersum, Jordans, Knaevelsrud, McDaid, Miller, Morina, Park, Roberts, van Son and Cuijpers2017).
Contrary to our expectations, we did not observe a sustained intervention effect on symptoms of PTSD at 12 months. Participants who received PM+ reported a drop in PTSD symptoms immediately after the intervention and remained far below baseline level over time, while participants in CAU showed a gradual decrease in PTSD symptoms from baseline to 12-month follow-up. So, although we did not observe an intervention effect at 12 months, it appeared that participants receiving PM+ had a quicker decrease in PTSD symptoms compared with participants who did not receive PM+. However, although PTSD symptoms at 12-month follow-up remained far below baseline levels, the average symptom level was still considerable. Meta-analytic evidence examining psychosocial interventions among refugees and asylum seekers shows that trauma-focused psychological interventions are best supported for the reduction of PTSD symptoms (Nosè et al., Reference Nosè, Ballette, Bighelli, Turrini, Purgato, Tol, Priebe and Barbui2017; Turrini et al., Reference Turrini, Purgato, Acarturk, Anttila, Au, Ballette, Bird, Carswell, Churchill, Cuijpers, Hall, Hansen, Kösters, Lantta, Nosè, Ostuzzi, Sijbrandij, Tedeschi, Valimaki and Barbui2019). Complementing PM+ with a trauma-focused module may potentially enhance effectiveness for individuals with serious PTSD symptoms (Alozkan Sever et al., Reference Alozkan Sever, Cuijpers, Mittendorfer-Rutz, Bryant, Dawson, Holmes, Mooren, Norredam and Sijbrandij2021).
Similar to our findings at 1-week and 3-month follow-up, PM+ did not lead to reduced functional impairment at 12 months. ‘Functional impairment’ may be too generic as it also captures impairment due to medical conditions or social restrictions (e.g., during COVID-19 restrictive measures). The often challenging social context of refugees may have had a larger impact on their psychosocial functioning than the psychological intervention, especially over a 12-month period. A meta-analysis of psychosocial interventions for refugees and asylum seekers also demonstrated no treatment effects on functioning outcomes (Turrini et al., Reference Turrini, Purgato, Acarturk, Anttila, Au, Ballette, Bird, Carswell, Churchill, Cuijpers, Hall, Hansen, Kösters, Lantta, Nosè, Ostuzzi, Sijbrandij, Tedeschi, Valimaki and Barbui2019). We also found that the short-term benefits of PM+ in terms of reductions on self-identified problems (de Graaff et al., Reference de Graaff, Cuijpers, Twisk, Kieft, Hunaidy, Elsawy, Gorgis, Bouman, Lommen, Acarturk, Bryant, Burchert, Dawson, Fuhr, Hansen, Jordans, Knaevelsrud, McDaid, Morina and Sijbrandij2023) were not retained. The effects of PM+ may be enhanced through integrated approaches, for example, if combined with social services that target social determinants of health including employment opportunities, housing and social support and better tap into the self-identified problems that often relate to practical issues.
Contrary to our expectation and to earlier findings where a higher number of post-migration stressors at baseline was associated with a smaller treatment effect at 3-month follow-up (Bryant et al., Reference Bryant, Bawaneh, Awwad, Al-Hayek, Giardinelli, Whitney, Jordans, Cuijpers, Sijbrandij, Ventevogel, Dawson and Akhtar2022a; de Graaff et al., Reference de Graaff, Cuijpers, Twisk, Kieft, Hunaidy, Elsawy, Gorgis, Bouman, Lommen, Acarturk, Bryant, Burchert, Dawson, Fuhr, Hansen, Jordans, Knaevelsrud, McDaid, Morina and Sijbrandij2023), higher numbers of potentially traumatic events and post-migration stressors at baseline were associated with larger treatment effects on psychological distress at 12 months. This may be explained by the association of potentially traumatic events and post-migration stressors with worse baseline symptom severity, which also modified the intervention effect at 12-month follow-up (i.e., participants scoring above clinical cut-offs had larger intervention effects).
Lastly, we found that participants who received in-person PM+ sessions had lower psychological distress compared to the control group, whereas participants who received video/hybrid PM+ sessions did not. These sub-group analyses on the delivery format of PM+ were in line with what was found for the short-term (de Graaff et al., Reference de Graaff, Cuijpers, Twisk, Kieft, Hunaidy, Elsawy, Gorgis, Bouman, Lommen, Acarturk, Bryant, Burchert, Dawson, Fuhr, Hansen, Jordans, Knaevelsrud, McDaid, Morina and Sijbrandij2023). It must be noted that there was likely selection bias in the delivery format of PM+ because participants could choose (after an initial period in which no in-person sessions took place due to stricter COVID-19 measures) the format they preferred. Participants who took video/hybrid PM+ sessions had lower baseline scores compared to those who took in-person sessions, and it might be that participants with lower distress preferred the more easily accessible delivery format of video calls.
Strengths included high retention at 12-month follow-up (i.e., 82%) and the high representation of men in the sample which is rare in refugee studies. A limitation of this study was that mental healthcare utilisation was only reported for the preceding three months and did not cover the whole trial period. We thus do not know whether participants (in either group) accessed more specialist care for part of the study period. Another limitation is that the number of asylum seekers in this study was low (8% vs 85% of participants having a resident permit or citizenship), which prevented investigating whether resident status affected the effectiveness of PM+. Lastly, this study was not powered for a 12-month follow-up and no corrections for multiple testing were carried out, so conclusions about statistical significance should be interpreted with care.
An important implication of this study is that transdiagnostic and brief interventions like PM+ can be effectively delivered by non-specialists to refugees in high-income settings where PM+ could be considered a first step of stepped-care. Psychological therapies such as (trauma-focused) cognitive behavioural therapy focusing on a single disorder (e.g. PTSD) and delivered by specialists have better effect sizes (e.g., Weber et al., Reference Weber, Schumacher, Hannig, Barth, Lotzin, Schäfer, Ehring and Kleim2021), but refugees in high-income countries may not access these services due to a lack of interpreters and long wait lists. We thus argue that, from a public health perspective, small intervention effects of non-specialist delivered interventions are crucial, especially as part of stepped-care and collaborative care models. In the past decade there has been a steep increase in the number of displaced people worldwide, including in European countries. There is an urgent need to scale up psychological interventions to meet the likely demand for mental health by refugees and other displaced populations. Booster sessions may be considered to enhance intervention effects over the long term, and implementation research is needed to evaluate the uptake of PM+ when integrated into healthcare systems.
Conclusion
The benefits of PM+ delivered by non-specialist peer-providers to Syrian refugees on psychological distress and anxiety are sustained up to 1-year follow-up. To prolong benefits gained with PM+ on other mental health and psychosocial outcomes such as depression, PTSD symptoms and self-identified problems, stepping up to specialist support within a stepped-care model or the addition of targeted modules may be required. Considering the potential of PM+ for the long-term, scalable psychological interventions should be made available to underserved populations such as refugees.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796024000519
Availability of data and materials
Data are available on reasonable request. The Vrije Universiteit Amsterdam (VU) will keep a central data repository of all data collected in the STRENGTHS project. The data will be available on reasonable request to the STRENGTHS consortium. Data access might not be granted to third parties when this would interfere with relevant data protection and legislation in the countries participating in this project and any applicable European Union legislation regarding data protection. The PM+ training manual and intervention manual are available through the consortium. Interested researchers can contact Prof. Dr. Marit Sijbrandij at [email protected] to initiate the process.
Acknowledgments
The authors would like to acknowledge the contributions of the STRENGTHS research assistants and helpers.
Financial support
This project has received funding from the European Union’s Horizon 2020 Research and Innovation Programme Societal Challenges under grant agreement No. 733337. The opinions expressed in this paper are those of the authors and do not necessarily represent the decisions, policies, nor views of the organizations they serve or of the funder. The European Community is not liable for any use that may be made of the information contained therein.
Competing interests
The authors declare that there is no conflict of interest regarding the publication of this article.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.







