Diogenes syndrome – named after the Greek philosopher and cynic – is a neurobehavioural syndrome characterised by severe domestic squalor, pathological hoarding and lack of insight into the condition,Reference Assal1 the latter preventing the majority of patients from seeking medical help. First cases of elderly patients with self-neglect and extreme lack of hygiene were published by Dupré in 1925Reference Dupré2 and Stevens in 1963Reference Stevens3 and then more precisely described as a syndrome in 1966 by Macmillan & Shaw,Reference Macmillan and Shaw4 who called this condition ‘senile breakdown’. Halliday et al in 2000 proposed domestic squalor, evidence of self-neglect, living alone, tendency to hoard and lack of concern for surroundings as the five defining features of the syndrome and they also developed the Environmental Cleanliness and Clutter Scale to assess squalor and hoarding.Reference Halliday, Banerjee, Philpot and Macdonald5 However, even in their study only 22% of individuals met all items on the scale and diagnostic criteria still lack consensus.Reference Halliday, Banerjee, Philpot and Macdonald5
The majority of cases occur in older adults (average age of 79 years) who live alone, although rare cases have been described in siblings and married couples.Reference Halliday, Snowdon and Simpson6 The current incidence of the full syndrome is not well-known: a retrospective observational French study found 1.6 cases per 10 000 inhabitants; 25% of patients had the complete syndrome and 75% had the partial syndrome.Reference Monfort, Hugonot-Diener, Devouche, Wong and Péan7 Cipriani et al estimate an approximate annual incidence of 0.05% in people over the age of 60.Reference Cipriani, Lucetti, Vedovello and Nuti8 In all probability, our society will be faced with more cases in the future owing to increased life expectancy and a consequent higher number of elderly individuals living alone.
Despite being an uncommon condition, diagnosis is paramount since Diogenes syndrome has been associated with increased morbidity and a 46% 5-year mortality rate,Reference Clark, Mankikar and Gray9 with death commonly due to physical illnesses subsequent to self-neglect. Moreover, Diogenes syndrome poses ethical questions and legal challenges, such as finding a balance between autonomy and beneficence.Reference Freckelton10
Although the syndrome may occur as a single entity – so-called primary Diogenes syndrome – it is usually secondary to an underlying neuropsychiatric condition. Overall, Diogenes syndrome tends to be associated with psychosis, alcohol-induced disorder, affective disorder or obsessive–compulsive disorder (OCD) in younger individuals, whereas it is frequently associated with dementia in the elderly: clinical hoarding behaviour, often associated with self-neglect, and Diogenes syndrome are described in 23%Reference Hwang, Tsai, Yang, Liu and Lirng11 and 15%Reference Radebaugh, Hooper and Gruenberg12 respectively of older individuals with dementia. The unique combination of behavioural symptoms of behavioural variant frontotemporal dementia (bvFTD) may predispose to a high likelihood of developing Diogenes syndrome, which in fact occurs in up to 36% of people with bvFTD.Reference Lebert13 We describe here a case of bvFTD presenting with Diogenes syndrome and subsequent follow-up of the patient.
Ethics statement
Informed written consent approved by the local Institutional Review Board was obtained from the patient, in accordance with specific national laws and the ethics standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Case report
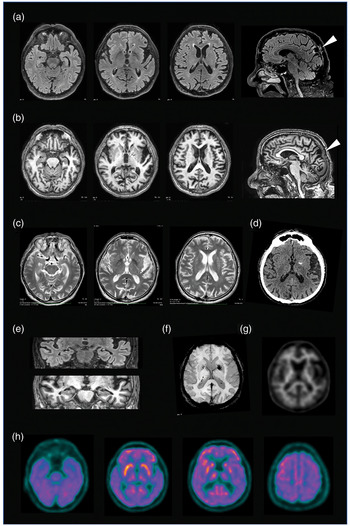
A 77-year-old dextral man was referred to the emergency department of our hospital by the police because he was found on the landing outside his flat, unkempt and dishevelled in personal appearance, after reportedly having lived there for 10 days. When questioned about this behaviour, he claimed that he was waiting for his next-door neighbour, who held a spare set of his flat keys, since he had accidentally locked his set in his garage. However, while he believed her to be on holiday, she had actually been living in a retirement home for 2 years. His medical history was significant only for a craniotomy, performed 16 years before, for the excision of a left parietal meningioma, with no residual neurological deficits, and hypertension, for which he did not take any drugs. He admittedly consumed more than a litre of wine per day but denied smoking. His psychiatric history was unremarkable, but in recent years he had begun packing his flat with ‘art pieces’. An electrocardiogram performed in the emergency department revealed the presence of atrial fibrillation, and a chest radiography showed a right lower lobe consolidation, which were treated with oral medication because he refused any infusion therapy. He was initially admitted to the geriatric department and then moved to the psychiatric unit because of repeated instances of wandering and a quarrel with another homeless in-patient. When contacted, the patient's building manager reported behavioural changes over the past few years, and a recent history of pathological hoarding was confirmed by his general practitioner. A mental state examination revealed confabulation, along with a more structured delusion about being married to a counterterrorism spy, daughter of a 19th-century marshal, with whom he would communicate only non-verbally in order for her not to be discovered. Neuropsychological evaluation outlined an impairment in selective attention and letter verbal fluency retrieval, in the context of an overall preserved mental functioning, with a score of 26/30 on the Mini-Mental State Examination (MMSE); a subsequent more thorough testing for language excluded semantic impairment (Table 1). Brain magnetic resonance imaging (MRI) showed a mild temporo-insular atrophy on both sides and calcifications in the left lenticular nucleus; fluorodeoxyglucose positron emission tomography (FDG-PET) revealed mild hypometabolism in the left superior temporal gyrus; amyloid PET did not reveal areas of increased radiotracer binding, ruling out an underlying amyloid brain deposition (Fig. 1). The search for expansion in the Chromosome 9 open reading frame 72 (C9orf72) gene gave negative results, and no mutations were detected through next generation sequencing (NGS) analysis.Reference Ghezzi, Carandini, Arighi, Fenoglio, Arcaro and De Riz14 According to Rascovsky criteria,Reference Rascovsky, Hodges, Knopman, Mendez, Kramer and Neuhaus15 a diagnosis of bvFTD was made. In view of agitation and delusions, the patient was initially prescribed clotiapine, then shifted to zuclopenthixol and eventually to haloperidol, with only partial response. After the hospital admission, the patient was admitted to a care home.

Fig. 1 Brain scans showing mild temporo-insular atrophy on both sides, calcifications in the left lenticular nucleus and the location of the previously removed meningioma (arrowhead).
(a) Fluid attenuated inversion recovery (FLAIR) and (b) T1-weighted axial and sagittal (rightmost images) scans. (c) T2-weighted axial scans. (d) Computed tomography axial scan. (e) Coronal FLAIR section of temporal lobes (above) and coronal T1 scans of temporal lobes (below). (f) Susceptibility weighted imaging (SWI) scan. (g) Amyloid positron emission tomography (PET) scan, negative for amyloid deposition. (h) fluorodeoxyglucose PET scans showing left superior temporal hypometabolism.
Table 1 Neuropsychological evaluation scores

Discussion
The exact pathogenesis and neuroanatomical basis of the full Diogenes syndrome are only hypothetical. In fact, no definite triggers to the condition have been identified and it is not clear whether solitude is a risk factor or a consequence of decision-making. Also, while hoarding is a major feature of Diogenes syndrome, there is no agreement on how to consider it in respect to other manifestations of the full syndrome (namely, squalor), to possibly related obsessive–compulsive behaviours and to other nosological entities such as OCD. The DSM-5 considers hoarding disorder and OCD to be distinct clinically, neuroanatomically and therapeutically. Collecting in OCD is associated with anxiety and fear and often driven by obsessions or preoccupations, whereas hoarding disorder is characterised by distress on discarding possessions, leading to clutter. Results from voxel-based morphometry studies have detected significant structural differences both in people with OCD compared with controlsReference Piras, Piras, Chiapponi, Girardi, Caltagirone and Spalletta16,Reference Subirà, Cano, de Wit, Alonso, Cardoner and Hoexter17 and in people with hoarding disorder relative to those with OCD and to controls.Reference Yamada, Nakao, Ikari, Kuwano, Murayama and Tomiyama18 Also, Hough et al found significantly greater dorsolateral prefrontal cortex activation during executive tasks in individuals with hoarding disorder compared with those with OCD.Reference Hough, Luks, Lai, Vigil, Guillory and Nongpiur19
In contrast to hoarding disorder, acquired hoarding has been described both as a consequence of vascular lesions in the medial prefrontal or bilateral orbitofrontal cortexReference Figee, Wielaard, Mazaheri and Denys20 and in the context of dementia.Reference Perry, Whitwell, Boeve, Pankratz, Knopman and Petersen21 Despite not being specific to any dementia subtype, hoarding appears to be much more common in bvFTD and semantic variant primary progressive aphasia (svPPA) – subtypes of FTD – occurring both in isolation and in the presence of additional obsessive–compulsive behaviours.Reference Mitchell, Tavares, Palaniyappan and Finger22
Various explanations have been offered to account for the new onset of compulsive collecting in individuals with dementia.
Frontal lobe deficits are common in all the FTD subtypes and could clearly contribute to increased clutter due to a combination of disturbances. Finney et al reviewed five cases of Diogenes syndrome in individuals with bvFTD who exhibited hoarding accompanied by decline in self-care, other obsessive–compulsive behaviours and prominent executive dysfunctions.Reference Finney and Mendez23 All these patients had bilateral or right predominant frontotemporal atrophy and hypometabolism, suggesting that compulsive collecting in these patients may be part of the environmental dependency syndrome in frontal disease, with specific involvement of a right fronto-limbic-striatal system.
On the other hand, results from a quantitative MRI volumetric analysis of 47 individuals with FTD showed hoarding and obsessive–compulsive behaviours to be partially dissociable clinically and neuroanatomically, though highlighting an important role of the temporal lobes, particularly the left, in both disturbances.Reference Mitchell, Tavares, Palaniyappan and Finger22 The study found that new or increased hoarding behaviour in people with FTD were more frequently associated with svPPA and predicted by left temporal atrophy. Left lateral temporal lobe grey matter loss also correlated with severity of obsessive–compulsive behaviours in a study conducted by Perry et al on 11 people with bvFTD.Reference Perry, Whitwell, Boeve, Pankratz, Knopman and Petersen21 A plausible explanation for this finding is that deterioration of semantic organisation and storage secondary to degeneration of left temporal lobe structures, particularly in svPPA, may impair categorisation of objects, causing each to be considered unique and therefore non-discardable. Interestingly, in line with these newer data, our patient showed mild left superior temporal gyrus hypometabolism on the FDG-PET scan, much more limited in respect to the extensive frontotemporal hypometabolism in Finney et al's seriesReference Finney and Mendez23 and usually observed in bvFTD.Reference Cerami, Dodich, Lettieri, Iannaccone, Magnani and Marcone24 However, to the best of our knowledge no previous studies specifically aimed at comparing patterns of cerebral glucose metabolism in individuals with FTD with and without hoarding are available to support our finding.
In conclusion, even if the development of the full Diogenes syndrome may require a more extensive and predominantly right-sided impairment of frontotemporal lobe connectivity and function, as seen in bvFTD, the occurrence of hoarding as an isolated finding in people with dementia, particularly in svPPA, along with newer literature suggests a pivotal role of left temporal lobe pathology in compulsive collecting, which our case seems to confirm.
Therapeutic management of Diogenes syndrome includes non-pharmacological and pharmacological approaches. Overall, both have proven difficult, since most patients deny their condition, avoid medical attention and exhibit poor therapeutic adherence.
Behavioural therapy-based skills seem beneficial.Reference Waserman, Hategan and Bourgeois25 However, owing to the absence of randomised controlled trials, there are no guidelines on pharmacological interventions and no approved drugs, so that pharmacological interventions frequently depend on associated symptoms when present.
Many drugs have been tried in different studies, including selective serotonin reuptake inhibitors (SSRIs), first- and second-generation antipsychotics and anti-epileptics, with mixed results. Given the well acknowledged role of serotonin and dopamine in impulse control disorders and the approved use of SSRIs in the treatment of OCD, a therapeutic trial with molecules from one of these classes may be justified.
In fact, Finney et al reported some effect of high-dose sertraline in reducing collecting behaviours in two of their patients.Reference Finney and Mendez23 Other authors found benefit on hoarding from other SSRIsReference Saxena, Brody, Maidment and Baxter26 and a combination of valproic acid and quetiapine in treating patients with bvFTD and secondary Diogenes syndrome.Reference Gálvez-Andres, Blasco-Fontecilla, González-Parra, Molina, Padín and Rodriguez27 Lithium significantly improved one patient with long-standing Diogenes syndrome, although probably secondary to bipolar disorder,Reference Fond, Jollant and Abbar28 and risperidone reduced hoarding in an individual with Diogenes syndrome, but caused significant motor side-effects.Reference Herrán and Vázquez-Barquero29 Although not specifically tried for hoarding, trazodone has proven beneficial for behavioural symptoms in FTD.Reference Lebert, Stekke, Hasenbroekx and Pasquier30
Our patient needed typical antipsychotics to manage agitation but quitting hoarding was mainly due to hospital admission and no specific treatment was tried. Admitting patients to hospital or moving them to another location is sometimes mandatory, but out-patient treatment through community care should be privileged if there is little risk to the patient or neighbours. Management should be conducted sensitively lest patients return to previous living conditions even more reluctant to receive medical aid.
Implications
This case, while illustrating the importance of suspecting Diogenes syndrome in elderly patients presenting with squalor and hoarding, especially in the context of dementia, supports recent evidence about the importance of the left temporal lobe in compulsive collecting pathogenesis. A deeper understanding of this condition, facilitating a timelier diagnosis, may lead to more effective pharmacological and non-pharmacological interventions, which in turn may reduce acute and chronic physical illness and improve social health outcomes.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Data availability
The study data are available on reasonable request.
Author contributions
L.S. made substantial contributions to the acquisition of data and drafted the manuscript; ER., S.P., A.F., G.S., C.M., C.C., G.G.F., T.C., A.M.P., D.G.G., E.A.S., M.C. and P.B. made substantial contributions to the acquisition of data and revised the work; F.T. and G.M. made substantial contributions to the acquisition and interpretation of data and revised the work; A.A. made substantial contributions to the acquisition of data and drafted and revised the manuscript. All authors gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Declaration of interest
None.





eLetters
No eLetters have been published for this article.