Introduction
Children are among the most vulnerable populations inadvertently affected by explosions both related and unrelated to terrorism. For the last two decades, the primary battlespace of war and civil conflict continues to be crowded cities and urban environments. Thus, children are killed and injured either intentionally or collaterally by explosive weapons. This has been evident in modern-day conflicts in Iraq, Reference Hicks, Dardagan, Guerrero Serdán, Bagnall, Sloboda and Spagat1 Afghanistan, Reference Bilukha and Brennan2 Syria, Reference Guha-Sapir, Rodriguez-Llanes and Hicks3 and Gaza. Reference Smith4 Parallel to the threat of terrorism and counter-terrorism warfare, accidental explosions are another potential means causing pediatric civilian casualties. This was most recently seen in the 2020 explosion in Beirut, Lebanon where over 200 people were killed (including six children) and tens of thousands more were injured (including over 1,000 children) by ammonium nitrate incorrectly stored adjacent to a fireworks factory. 5 On a smaller scale, injuries secondary to accidental fireworks explosions also have the potential to produce significant blast injury in the pediatric population. Reference Demirbag, Cetinkursun, Surer and Ozturk6–Reference Ratto, Johnson, Condra and Knapp8 Natural gas explosions and accidental detonation of old warfare ordnance are additional causes of pediatric blast injuries outside of armed conflict. Given that there have been, on average, 3,400 bombings per year since 2000 Reference Miller, LaFree and Dugan9 and over 15,000 fireworks-related injuries in the United States in the year 2020 alone, Reference Marier, Smith and Lee10 it is clear that the medical enterprise must be well-prepared to successfully triage and resuscitate pediatric patients who have experienced devastating blast injuries. To date, no studies have directly analyzed environmental risk factors for pediatric mortality in blast trauma or differences in pediatric injury patterns based on if explosions were related or unrelated to terrorism. Such data would be useful to design subsequent training for emergency medical personnel and to prepare medical organizational disaster response plans. Therefore, the objective of this study was to analyze risk factors for pediatric mortality and injury profiles in the setting of explosions related and unrelated to terrorism.
Methods
Literature Search
The systematic review was carried out under Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) guidelines (Supplementary Material, Table S1; available online only) and was designed to answer the following Population, Intervention, Comparison, Outcome (PICO)-centered question: Is there a difference in mortality and blast injury patterns (outcome) between pediatric patients (population of interest) affected by explosions related to terrorism (exposure) and pediatric patients affected by explosions unrelated to terrorism (comparison)? PubMed (National Center for Biotechnology Information, National Institutes of Health; Bethesda, Maryland USA) was used as the primary search engine, and the following search terms were utilized: “child”[MeSH Terms] OR “child”[All Fields] OR “children”[All Fields] OR “child s”[All Fields] OR “children s”[All Fields] OR “childrens”[All Fields] OR “childs”[All Fields]) AND (“blast injuries”[MeSH Terms]) OR (“blast”[All Fields] AND “injuries”[All Fields]) OR “blast injuries”[All Fields] OR (“blast”[All Fields] AND “injury”[All Fields]) OR “blast injury”[All Fields]. All articles were subject to a screening protocol where two independent reviewers screened the full text against pre-set inclusion and exclusion criteria. To be considered for inclusion, the text had to have been written in the English language and published after the year 2000. The text also had to have provided an injury profile, defined as a list of injuries sustained from an explosion stratified by Abbreviated Injury Scale (AIS) body region. The AIS is an anatomically based scoring system that describes injury by body region; it is the basis for the Injury Severity Score (ISS) utilized to assess overall severity in the patient with systemic polytrauma. The AIS codes are stratified anatomical areas and include the head, face, and neck (AIS Regions 1-3), thorax (AIS Region 4), abdomen (AIS Region 5), and upper and lower extremities (AIS Regions 7-8). In addition, articles must have reported the injury profiles of pediatric patients where “pediatric” was defined in this study as any patient less than age 18. If articles reported both adult and pediatric injury profiles, articles were included only if pediatric patients had an injury profile separate from the adult population. Exclusion criteria included basic science research, quality improvement studies, studies not including pediatric patients, studies describing injuries focused on one part of the body (for example, a study solely describing blast-related ophthalmologic injury), case studies, and any study not published in a peer-reviewed journal. Studies with missing data were excluded post hoc. Finally, the references of articles meeting the present inclusion criteria were screened for additional relevant articles not captured by the initial data extraction. The systematic review protocol was carried out by two authors (MT, RP) with any discrepancies decided on by a third author (JR).
Data Quality Analysis
All studies were appraised for scientific rigor using an 11-point modified Mixed Method Appraisal Tool (MMAT) Reference Hong, Fàbregues and Bartlett11 with discreet scores given of -1, 0, and +1 where articles fully meeting a given listed quality metric are graded at +1, articles where not meeting the quality metric cannot be ruled out are graded at 0, and articles definitively not meeting the quality metric are graded at -1. The quality metric grades were then summated for each article and are reported in Supplementary Material, Table S2 (available online only). Questions on the MMAT utilized in this work were those pertaining to quantitative non-comparative descriptive studies. Each question on the MMAT was formulated and adapted to relate to metrics relevant to this study. Data quality analysis was performed by two researchers (MT, RP).
Data Extraction and Analysis
Injury pattern data were extracted from each study and stratified into AIS-defined body regions. Other data extracted included the type of study, years analyzed, geographic location of the explosion(s), mean casualty age, biological sex distribution, mortality rate, total number of patients studied, ISS, and if the explosion was deemed to be related or unrelated to terrorism. The definition of terrorism utilized here was derived from the United States Code of Federal Regulations (28 C.F.R. § 0.85). An explosion was defined as being related to terrorism if the act occurred with the intent of producing immediate casualties and the assailants had the political and/or social objective of instilling communal fear. If an event did not meet this criterion, it was deemed to be unrelated to terrorism. 12
All statistical analysis was performed in the GraphPad Prism statistical software package (version 09; GraphPad Software; San Diego, California USA). Data sets were initially examined for normality using four independent normality tests: the Anderson-Darling test, Reference Anderson and Darling13 D’Agostino-Pearson test, Reference D’Agostino14,Reference Pearson15 Shapiro-Wilk test, Reference Shapiro and Wilk16 and Kolmogorov-Smirnov test. Reference Smirnov17 In addition, QQ plots of each of the four injury pattern data sets were analyzed. Continuous data sets that passed all four quantitative tests for normality in addition to qualitative QQ plot analysis were analyzed for statistical significance using Welch’s t test of unequal variance. Reference Welch18 Welch’s t test was selected over student’s t test as it provides better control of Type I errors when homoscedasticity (the assumption that data variance is homogenous) is violated, while performing as well as the student’s t test when homoscedasticity is maintained. Reference Zimmerman19–Reference Delacre, Lakens and Leys22 Aggregated data were reported as mean values with data spread described as standard deviation (SD). Discreet data were collated into contingency tables to ascertain bivariate odds ratios (OR) with variables being represented as a hypergeometric probability function of explosions related versus unrelated to terrorism. An exact test approach was chosen over the chi-squared approximation as the latter relies on the assumption that the central limit theorem is met, while the former does not and was thus posited by the authors to be of higher reliability. Reference Ramsey and Ramsey23 Fisher’s exact test was selected over Barnard’s exact test given the equivalent power generation of both tests at high sample numbers coupled with the more conservative determination of significance associated with Fisher’s exact test. Reference Kim24–Reference Mehta and Senchaudhuri26 This results in a deliberately higher sensitivity in establishing statistical significance with Fisher’s test as compared to Barnard’s test. The 95% odds ratio confidence intervals (CI) were calculated using the Woolf-Logit models. Statistical significance was conferred if P < .05.
Results
Systematic Review
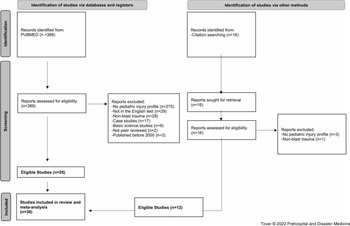
A total of 389 articles were extracted from PubMed using the search criteria previously described. Twenty-six studies from the initial data extraction were found to meet inclusion criteria. Twelve additional studies that met inclusion criteria were identified by searching the citations from the original articles (Figure 1). Thus, a total of 38 studies were included in the systematic review and meta-analysis, as shown in Table 1. 27–Reference Marenco, Lammers, Do, Morte, Horton and Eckert64 The most common causes for article exclusion were no pediatric injury profiles included (n = 275; 75.9%); articles not written in English (n = 29; 8.0%); articles did not describe blast injuries (n = 28; 7.7%); articles identified as case studies (n = 17; 4.7%); articles identified as basic science studies (n = 9; 2.49%); non-peer-reviewed studies (n = 2; 0.55%); and articles describing events not in the specified date range (n = 3; 0.83%; Figure 1).

Figure 1. A 2020 PRISMA Flow Diagram of the Systematic Review Process Performed to Select Articles for Inclusion into Study.
Abbreviation: PRISMA, Preferred Reporting Items for Systematic Reviews and Meta Analyses.
Table 1. Summary of Studies Investigating Pediatric Blast Trauma

Data Quality
Quality assessment was performed utilizing an 11-point MMAT grading tool due to its ability to successfully evaluate quantitative non-comparative studies. Overall, the mean score attained was 8.81 (SD = 2.4) out of a possible 11.0 points (Supplementary Material, Table S2; available online only). The lowest score attained by this grading scheme was a two (n = 1), while the highest score attained was an eleven (n = 16). No studies attained a score of three and two studies attained a score of four. Overall, this suggested that the majority of the studies included in this work were of high quality and were thus feasible to extract and collate data from.
Study Characteristics
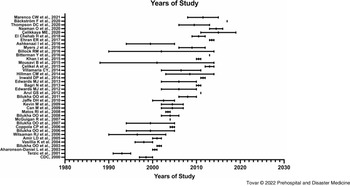
The majority of the articles (n = 33/38; 84.8%) from which data were extracted were retrospective cohort in design, followed by database search (n = 3/38; 7.9%), cross-sectional (n = 2/38; 5.3%), and prospective observational studies (n = 1/38; 2.6%). Most studies (n = 34/38; 89.4%) described explosions occurring outside the continental United States (OCONUS) and the minority (n = 5/38; 13.1%) described explosions that occurred within the continental United States (CONUS). Of studies that described OCONUS events (n = 34), 18/34 (52.9%) were related to the Global War on Terror (GWOT) campaign and 16/34 (47.0%) were unrelated to the GWOT campaign. Of 18 studies describing non-terrorism events, 6/18 (33.3%) were related to firework explosions and 7/18 (38.9%) were related to land mine explosions left over from prior conflicts. The remaining 5/18 studies (27.8%) described explosions produced by state-sponsored entities (eg, the Syrian Arab Republic utilizing ordnance that results in civilian casualties in the on-going Syrian civil war). Reference Sherlock65 The study pool described conflicts and accidents ranging from the years 1988-2017 (Figure 2).

Figure 2. Years of Conflict Covered by Each Representative Study Included in the Meta-Analysis.
Patient Demographics
The 38 articles from which data were extracted collectively described 128,424 pediatric patients affected by blast injuries, sustaining a total of 222,638 unique recorded injuries (19,879 injuries related to terrorism and 202,759 injuries unrelated to terrorism). Of this study population, 9,962 patients were affected by explosions related to terrorism and 118,462 patients were affected by explosions unrelated to terrorism. All data analyzed passed all metrics for normal data distribution. The demographic data (Table 2) illustrated that the average age of blast victims affected by bombings related to terrorism was lower than blast victims affected by non-terrorism explosions (10.28 years-old, SD = 2.7 versus 12.07 years-old, SD = 1.87, respectively). The biological sex distribution was also different between terrorism victims versus accidental explosion victims (68.96% male, SD = 17.58 versus 79.15% male, SD = 8.02, respectively). The overall mortality rate of explosions related to terrorism was 15.4% (SD = 19.3%) compared to 5.2% (SD = 7.1%) of explosions unrelated to terrorism.
Table 2. Demographics of Victims of Explosions Related-To and Unrelated-To Terrorism

Note: Compared using Student’s t-test with Welch’s correction for unequal variance with P < .05 considered statistically significant.
Abbreviation: ISS, Injury Severity Score.
Risk Factors for Pediatric Mortality
Bivariate odds ratio analyses of situational factors surrounding the setting of the explosion showed several harmful and protective factors associated with pediatric mortality (Figure 3). The odds of mortality were significantly higher in the setting explosions related to terrorism compared to those unrelated to terrorism (OR = 32.73; 95% CI, 28.8-37.2; P < .0001). Weapons-grade explosives (WGEs), including improved explosive devices (IEDs), land mines, unexploded ordinance, and conventional munitions, detonated in GWOT conflicts were also associated with increased odds of pediatric mortality compared to WGEs detonated in non-GWOT conflicts (OR = 1.28; 95% CI, 1.04-1.44; P = .0130). Being treated at a North Atlantic Treaty Organization (NATO; Brussels, Belgium)-affiliated combat support hospital in the GWOT was associated with decreased pediatric mortality in the setting of terror-related explosions (OR = 0.48; 95% CI, 0.37-0.62; P < .0001). With respect to explosions unrelated to terrorism, the odds of mortality were substantially lower if the explosive agent was a commercial firework compared to accidental detonation of landmines and unexploded ordnance (OR = 3.20×10-5; 95% CI, 2.00×10-6-5.16×10-4; P < .0001). Victims of explosions unrelated to terrorism also had decreased odds of mortality if the incident occurred within CONUS compared to OCONUS (OR = 2.40×10-5; 95% CI, 1.51×10-6-3.87×10-4; P < .0001).

Figure 3. Bivariate Odds Ratio Analysis Revealed Several Protective and Harmful Factors Related to Pediatric Mortality.
Note: Overall, explosions related to terrorism (T) were highly associated with pediatric mortality compared to explosions unrelated to terrorism (NT). However, being resuscitated at a forward-deployed CTRS was a protective factor against pediatric mortality compared to those who were not resuscitated at a CTRS. Use of WGEs in conflicts related to the GWOT associated with increased odds of mortality when compared to use of WGEs in conflicts not associated with the GWOT. Finally, for NT explosions, protective factors included if the event took place in the CONUS and if a commercial firework was the explosive.Abbreviations: CTRS, combat trauma resuscitation service; WGE, weapons-grade explosive; GWOT, Global War on Terror; CONUS, Continental United States.
Pediatric Injury Profiles and Injury Severity
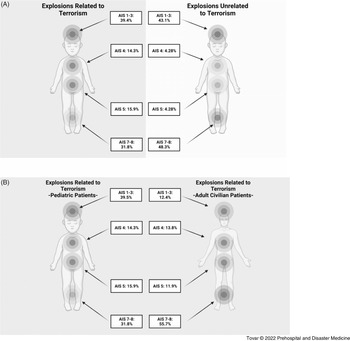
There were differences in the injury profile between those affected by terror-related blast trauma versus those affected by non-terror-related explosions (Figure 4A). When stratified by injury region, there was a similar incidence of head, face, and neck trauma (AIS 1-3) between terrorism and non-terrorism explosions (39.5% versus 43.1%, respectively). However, there was an increase in the incidence of thoracic injury (AIS 4; 14.3% versus 4.28%) and abdominal injury (AIS 5; 15.9% versus 4.3%) in explosions related to terrorism compared to explosions unrelated to terrorism. Finally, the incidence of extremity injury (AIS 7-8) was increased in explosions unrelated to terrorism compared to explosions related to terrorism (48.3% versus 31.8%, respectively). It was also noted that the pediatric blast injury profile was unique compared to the adult civilian blast injury profile (Figure 4B) with a higher incidence of injury to AIS 1-3 but a lower incidence of injury to AIS 7-8 in the pediatric population compared to adults. Reference Tovar, Bell and Neal66 Only one non-terror-related trauma article reported victim ISS, and thus the ability to compare this reported score to terror-related blast victims was unachievable. The average ISS among terror-related blast victims was 16.0 (SD = 6.30). Within explosions related to terrorism, there was a statistically significant increase in the ISS of those mortally wounded versus those non-mortally wounded (44.5, SD = 22.1 versus 16.5, SD = 5.47; P = .006).

Figure 4. (A) Pooled Summary of Pediatric Injury Profiles in Explosions Related to Terrorism and Unrelated to Terrorism; and (B) Pooled Summary of Pediatric Injury Profile Compared to Adult Civilian Injury Profile in Blasts Related to Terrorism.
Abbreviation: AIS, Abbreviated Injury Scale.
Discussion
Understanding Differences in Pediatric Injury Profile between Explosions Related to Terrorism versus Unrelated to Terrorism
This study presents the first meta-analytical study of environmental risk factors of pediatric mortality in the setting of explosions related and unrelated to terrorism. Fundamental differences were noted in the injury patterns of victims affected by explosions related to terrorism compared to those affected by explosions unrelated to terrorism. Victims affected by explosions related to terrorism had a higher incidence of thoracoabdominal trauma, a lower incidence of extremity trauma, and a similar incidence of craniocerebral trauma compared to victims affected by explosions unrelated to terrorism. These findings are likely explained by the observation that most articles that described non-terror explosions involved a patient either accidentally stepping on old, unexploded ordnance or holding an explosive in their hand, thus inducing a higher level of extremity injury than explosions related to terrorism. The higher incidence of thoracoabdominal trauma in explosions related to terrorism likely stems from the use of higher quantities of high-grade explosives in bombings compared to what is present in unexploded ordnance or low-grade firework explosives. 67–69
Furthermore, it was found that the use of WGEs in GWOT conflicts were associated with increased mortality compared to both WGEs not used in GWOT conflicts and non-WGE devices (eg, fireworks). A practical example of this delineation is that IEDs constructed and detonated by a terrorist cell are more likely to increase mortality compared to anti-personnel mines left over from a conflict accidentally triggered to detonate. This is likely related to the fact that the amounts of explosive used in unexploded ordnance is much smaller than that used in modern-day terrorism bombings. Unexploded ordnance typically contain between 1-30kg of explosive materials while modern-day IEDs have been reported to have between 9kg to >4,000kg of explosive maternal. Reference Miller, LaFree and Dugan9,Reference Fiederlein70 Explosions related to terrorism also typically use high-grade explosives such as nitroglycerin, Reference Gutierrez de Ceballos, Fuentes, Diaz, Sanchez, Llorente and Sanz71 plasticized cyclonite, 72,73 peroxide-based explosives, Reference Chukwu-Lobelu, Appukuttan, Edwards and Patel74 and ammonium nitrate 75 where the velocity of the blast pressure front is many times greater than the velocity produced by explosives in commercial-grade fireworks (approximating 4500m/s versus less than 1000m/s, respectively). Reference Akhavan76,Reference Bellamy and Zajtchuk77 Furthermore, terrorist groups have been reported to utilize a combination of directional amplifiers to further increase the velocity of the blast pressure wave and metal foreign bodies designed to maximize penetrating trauma, further improving control of the pressure wave and the lethality of the explosive, respectively. Reference Bellamy and Zajtchuk77,Reference Wolf, Bebarta, Bonnett, Pons and Cantrill78 This directional concentration of the blast pressure wave from explosives used in GWOT conflicts further increases the potential to cause devastating injury and mortality compared to other WGEs and commercial explosives.
A lower odds of pediatric victim mortality in casualties treated at NATO-affiliated hospitals was also discovered at forward-deployed combat resuscitation services compared to non-NATO affiliated civilian hospitals. This is potentially due to superior trauma resuscitation practices of forward-deployed NATO combat resuscitation services, as trauma casualties sustained during the GWOT revolutionized the science of traumatology. During the GWOT, a major revision in resuscitative practices resulted in a decrease in the mortality rate of injuries sustained in combat. Reference Maughon79,Reference Eastridge, Mabry and Seguin80 Examples of such practices include the wide-spread adoption of tourniquet use to stop exsanguinating hemorrhage, increased use of walking blood banks, use of tranexamic acid to promote hemostasis, and aggressive forward damage control resuscitation. Reference Schrager, Branson and Johannigman81 These resuscitative guidelines likely contributed to the lower mortality rate of pediatric patients in patients resuscitated at NATO combat resuscitation hospitals compared to those not treated at these facilities. However, to date, there is no unified combat trauma treatment protocol to guide medical personnel in the treatment of pediatric trauma sustained in the setting of armed conflict as there is in the adult population. 82 Further research in this space is required to further minimize death and morbidity in the pediatric population.
Although the annual incidence of injury from fireworks contributes to the largest explosion-related injury mechanism in the United States, the incidence of pediatric fatality is extremely low. Reference Marier, Smith and Lee10 A federal government report not captured by the systematic review protocol recorded only one pediatric fatality associated with a fireworks explosion in 2020, which saw upwards of 15,600 fireworks-related injuries across the country. Reference Marier, Smith and Lee10 The low observed mortality rate likely stems from the fact that firework explosives in the United States are regulated by both state and federal statutes (Regulation 27 CFR Part 555 promulgated by the Bureau of Alcohol, Firearms, and Tobacco [ATF; Washington, DC USA]) that are designed to keep firework-related mortality low. Nevertheless, isolated case studies of firework factory explosions that caused severe morbidity and mortality in all ages (including children) have been reported in the literature but were either not captured or excluded by this systematic review protocol. Reference Baldino, Stassi, Mondello, Bottari, Vanin and Ventura Spagnolo83–Reference Chen, Wang, Wang and Li85
Differences in Pediatric versus Adult Injury Profile in the Setting of Explosions Related to Terrorism
The injury patterns of pediatric blast victims is significantly different from a cohort of adult blast trauma patients previously studied in a similar manner. Reference Tovar, Bell and Neal66 The incidence of craniocerebral trauma in the pediatric population (n = 7,860 injuries to AIS 1-3 out of 19,879 total injuries, incidence = 39.5%) was approximately 30% higher than their civilian adult counterparts (1,845 injuries to AIS 1-3 out of 14,676 total injuries, incidence = 12.5%) in the setting of trauma sustained from a terrorism bombing. Also, the incidence of extremity trauma was reduced by upwards of 36% in pediatric patients (6,336 injuries to AIS 7-8 out of 19,926 total injuries, incidence = 31.8%) when compared to civilian adults (9,924 injuries to AIS 7-8 out of 14,676 total injuries, incidence = 67.6%) in the setting of trauma sustained from a terrorism bombing. Reference Tovar, Bell and Neal66 These differences in injury patterns are suspected to be largely associated with body surface area of a given pediatric patient compared to their adult counterpart as the volume and surface area ratio of the craniocerebral structures to the rest of the body is significantly larger in the pediatric patients compared to adults. Reference Figaji86 In addition, the presence of open cranial fontanelles in infants and toddlers also have the potential to contribute to an increased incidence of traumatic intracranial pathology, as has been shown in biomechanical modeling studies. Reference Margulies and Thibault87,Reference Li, Park and Liu88
Unique Utility of Injury Profile Data: Advantages of Designing Data-Driven Interventions to Mitigate Disaster Morbidity and Mortality
It was posited that injury profile meta-analyses such as the one prepared here have the potential to influence emergency medical provider education—both prehospital and in-hospital. For example, emergency medical response agencies can use the finding of increased head trauma in pediatric patients compared to adults to focus on screening for head trauma in the field and transporting patients to pediatric trauma centers with neurosurgical capabilities. Alternatively, if providers live in an area prone to terrorist attacks (ie, in war zones, areas of violent civil conflict, or highly targeted cities like Washington, DC [USA], New York City [New York USA], or London, United Kingdom), there is a need to be prepared for complex craniocerebral and thoracoabdominal trauma in the pediatric population.
These injury profile data can also be successfully leveraged when designing disaster response packages utilizing the “all-hazards approach” philosophy. When designing response packages, the all-hazards approach philosophy dictates that emergency preparedness be focused on ensuring capacities and capabilities critical to respond to a wide variety of disasters. Leveraging these data could potentially involve assigning more fiscal and personnel resources dedicated to addressing pediatric head and chest trauma. Examples of such resource allocation strategies include increasing the availability of staff capable of performing emergent cranial decompressions and ensuring robust access to pediatric thoracotomy surgical trays during times of heightened terrorism threats. Organizations utilizing a data-driven approach for the organization of emergency medical response protocol can optimize their life-saving efficacy while minimizing over-spending and resource wasting with the accumulation of unnecessary supplies.
Limitations
A number of studies (15/39; 38.4%) extracted data from hospital records, not standardized trauma databases, potentially introducing a degree of data heterogeneity since retrospective chart reviews are not as uniform as trauma database inputs. In addition, many papers were excluded from the study solely due to the fact that pediatric patient injury profiles were not separated from adult patients. Moreover, markers of pediatric morbidity, such as ISS, were inconsistently reported and thus were not able to be compared across cohorts of blasts related versus unrelated to terrorism. Due to the nature of disaster epidemiology papers reporting a large number of patients, it was difficult to ascertain the severity of a given patient’s injuries. As a result, any given “head injury” code might have been a simple scalp laceration requiring routine wound care, or it could have been a devastating injury requiring surgical intervention. As it was not reported in the study details, the authors were not able to provide further detail or compare injury severity, particularly with respect to craniocerebral injury.
Conclusion
The first epidemiological study that describes mortality risk factors and the blast injury profile of pediatric victims is reported in this work. Moreover, novel differences in the blast injury pattern of patients exposed to explosions related to terrorism versus explosions unrelated to terrorism were reported as well. Pediatric victims of explosions related to terrorism had a higher incidence of thoracoabdominal trauma and a lower incidence of extremity trauma when compared to victims of explosions unrelated to terrorism. Emergency response agencies should use these data to optimize disaster education and disaster response packages with the goal of further reducing pediatric morbidity and mortality in the setting of acts of terrorism.
Conflicts of interest/disclaimer
The views expressed in this submitted article are that of the authors and do not represent the official position of the institutions from which the authors are affiliated with. MAT is a commissioned officer in the United States Navy at the time of this manuscript submission. The views expressed in this paper are those of the author and do not reflect the official policy of the Department of the Navy, Department of Defense, or US Government. The authors declare no conflicts of interest.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1049023X22000747