Changes in clinical practice during the coronavirus disease 2019 (COVID-19) pandemic, including the potential increased use of broad-spectrum antibiotics, may have exacerbated the burden of Clostridioides difficile infection (CDI). Reference Abelenda-Alonso, Padullés and Rombauts1 Single-center studies have reported increased, Reference Lewandowski, Rosołowski and Kaniewska2 decreased, Reference Ponce-Alonso, Sáez De La Fuente and Rincón-Carlavilla3,Reference Hazel, Skally and Glynn4 or unchanged CDI rates. Reference Luo, Grinspan and Fu5,Reference Yadlapati, Jarrett, Lo, Sweet and Judge6 Furthermore, the impact of the COVID-19 pandemic on rates of CDI in Canada has not yet been described. Using national surveillance data, we compared CDI rates, patient characteristics, and clinical outcomes before and during the COVID-19 pandemic in Canada.
Methods
Data collection and participating hospitals
Using standardized case definitions, we included patients with CDI identified from hospitals participating in the Canadian Nosocomial Infection Surveillance Program (CNISP) between January 1, 2015, and June 30, 2021. Healthcare-associated (HA) and community-associated (CA) CDI rates were classified as previously described. 7 Beginning January 2021, COVID-19 diagnosis status was collected for all CDI patients.
Statistical analysis
We calculated HA-CDI rates per 10,000 patient days and CA-CDI rates per 1,000 patient admissions. We used interrupted time series (ITS) analysis to assess changes in CDI rates between the prepandemic period (62 monthly periods from January 1, 2015, to February 29, 2020) and the COVID-19 pandemic period (16 periods from March 1, 2020 to June 30, 2021) by modeling monthly CDI rates, accounting for time trends and seasonality. Models were fitted using a generalized linear mixed model with Poisson distribution and log-link function with first-order autocorrelation. The outcome was monthly CDI counts. Models included an offset term (ie, the natural log of either patient days or patient admissions). Changes over time for HA- and CA-CDI rates by month were displayed graphically. Predictor variables were pandemic status (pre pandemic = 0 and pandemic = 1), West (British Columbia, Alberta, Saskatchewan and Manitoba, Central; Ontario and Quebec) or East (Nova Scotia, New Brunswick, Prince Edward Island, Newfoundland and Labrador, and Nunavut) region, month and time (78 monthly periods from January 2015 to June 2021). Results were reported as incidence rate ratios (IRRs) comparing prepandemic and COVID-19 pandemic periods with 95% confidence intervals (CIs).
The χ2 test was used for categorical variables and the Student t test or Wilcoxon rank-sum test was used for continuous variables to compare characteristics and clinical outcomes among CDI patients by COVID-19 status and pandemic period. All statistical analyses were conducted using SAS version 9.4 software (SAS Institute, Cary, NC) with a significance level of 0.05.
Results
We summarized CDI rates from 71 hospitals (38 adult hospitals, 24 mixed hospitals, and 9 pediatric standalone hospitals) between January 1, 2015, and June 30, 2021. All 71 hospitals participated in HA-CDI surveillance, and 60 (85%) participated in CA-CDI surveillance. Crude HA-CDI rates per 10,000 patient days increased by 4.5%, but this increase was not significant (P = .0896). Crude CA-CDI rates per 1,000 patient admissions increased significantly by 21.8% from the prepandemic period (January 1, 2019, to February 29, 2020) to the pandemic period (March 1, 2020, to June 30, 2021) (Supplementary Table 1).
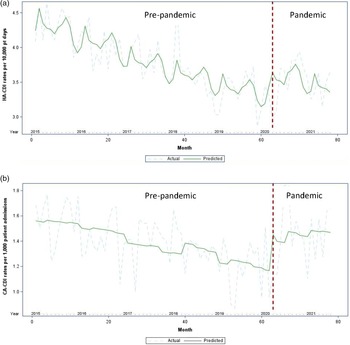
Figure 1 displays the results of the ITS analyses of HA-CDI and CA-CDI rates across the entire surveillance period (January 1, 2015, to June 30, 2021). Before the COVID-19 pandemic, both HA-CDI and CA-CDI rates decreased over time. We modeled the monthly CDI rates and adjusting for region and month; the results indicated that pandemic status was a significant predictor for both the HA-CDI model (P = .0007) and the CA-CDI model (P < .0001). We detected a statistically significant rate increase of 11% of HA-CDI (IRR, 1.11; 95% CI, 1.04–1.18) and 25% of CA-CDI (IRR, 1.25; 95% CI, 1.14–1.37) during the pandemic period.

Fig. 1. Monthly HA-CDI and CA-CDI rates between January 2015 and June 2021. (a) Actual and predicted HA-CDI rates per 10,000 patient days. (b) Actual and predicted CA-CDI rates per 1,000 patient admissions. Note. Red dotted line represents the declaration of the pandemic. Quarterly denominators were used to estimate monthly denominators, proportional to the number of days in each month.
We did not detect significant differences in age, sex, temperature, leukocyte counts, albumin levels or severe outcomes (death, admission to the ICU or colectomy) between the prepandemic cohort (n = 23,315, January 1, 2015, to February 29, 2020) and the pandemic cohort (n = 6,214) (data not shown).
Among 1,576 CDI patients identified in 2021, data regarding COVID-19 status were reported for 1,244 (89%). Of those, 64 (5%) were coinfected with Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2). A significantly higher proportion of CDI patients with COVID-19 had HA-CDI (78%) compared to those without COVID-19 (66%; P = .0366). Both groups were similar in age, sex, and severe outcomes (Supplementary Table 2). Time to CDI positive test from admission, measured in days, was longer for COVID-19 patients (10.5 days) than non–COVID-19 patients (4.0 days; P = .0004).
Discussion
This study is the first Canadian multicenter research to assess the impact of COVID-19 on CDI. We have described CDI rate trends, patient characteristics, and clinical outcomes before and during the COVID-19 pandemic for 71 hospitals across Canada.
Our previous surveillance data showed a steady decline in CDI rates before the pandemic. 7,Reference Du, Choi and Silva8 However, during the pandemic, we observed an increase in HA- and CA-CDI rates, whereas other jurisdictions reported varying changes in healthcare-associated infections. Reference Weiner-Lastinger, Abner and Edwards9 CDI and COVID-19 coinfection was uncommon (5%); however, COVID-19 patients were more likely to be associated with HA-CDI acquisition than non–COVID-19 patients. The increased HA-CDI rates in COVID-19 patients could be attributable to increased use of broad-spectrum antibiotics for clinical management of COVID-19. 7,Reference Langford, So and Raybardhan10 Changes in IPAC practices due to pandemic-related surge pressures may have also contributed to the observed increase. Additionally, COVID-19 disproportionately affected the elderly population in Canada during the early phases of the pandemic. Reference Flint, Bingham and Iaboni11,Reference Hsu, Lane and Sinha12 The elderly are at higher risk of respiratory infections leading to empiric antibiotic treatment, resulting in increased risk for acquiring CDI. Reference van Heijl, Schweitzer, Zhang, van der Linden, van Werkhoven and Postma13 Furthermore, COVID-19 outbreaks in Canadian long-term care facilities (LTCFs) resulted in a surge of residents being admitted to hospitals at the beginning of the pandemic. Reference Mitchell, Choi, Pelude, Rudnick, Thampi and Taylor14 LTCF residents are at higher risk of acquiring CDI, further contributing to increased HA-CDI rates.
Our results are similar to those of previous studies showing a slight increase in HA-CDI rates during the pandemic Reference Luo, Grinspan and Fu5,Reference Yadlapati, Jarrett, Lo, Sweet and Judge6 ; however, neither prior study demonstrated statistical significance or controlled for time. Although our unadjusted rates were not significantly different when comparing prepandemic and pandemic periods, the ITS analysis showed a significant HA-CDI rate increase of 11% after adjusting for region and month.
Other studies have reported decreases in CDI rates during the COVID-19 pandemic. Single-center studies by Ponce-Alonso et al Reference Ponce-Alonso, Sáez De La Fuente and Rincón-Carlavilla3 and Hazel et al Reference Hazel, Skally and Glynn4 reported significant reductions in CDI rates, citing enhanced infection control measures as a probable contributor with factors such as antimicrobial consumption remaining constant.
CA-CDI rates increased significantly from the prepandemic to pandemic periods. The increased CA-CDI rates among CNISP hospitals may be attributable to reduced accessibility and/or avoidance of healthcare facilities during the pandemic. Those seeking medical care were often assessed through virtual visits or emergency departments, which are suboptimal settings for determining antibiotic appropriateness, resulting in excessive or broad-spectrum antibiotic usage. Additionally, it has been reported that COVID-19 can affect the normal intestinal flora similar to treatment with antibiotics, causing a predisposition to CDI acquisition. Reference Leonardi, Gao and Lin15
Our findings show an increase in CDI rates during the COVID-19 pandemic. Considering the significant strain that COVID-19 has placed on the Canadian healthcare system, these data further our understanding of CDI epidemiology and assist in our ability to manage current and future pandemics.
Our study had several limitations. Data analysis was limited to 16 months of the pandemic; hence, longer-term impacts could not be assessed. Comparisons of prepandemic and pandemic rates are preliminary and should be interpreted with caution. Infection control policies and pandemic restrictions were dynamic throughout the pandemic period and may have impacted on monthly rates differentially. Additionally, our study did not assess changes in screening practices, antibiotic usage, or associations between CDI rates and COVID-19 rates across Canada or within the participating hospital sites. Such studies would have been beneficial to furthering our understanding of the impact of COVID-19 on CDI rates. Future studies should aim to elucidate factors that may have influenced changes in CDI rates during the pandemic.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2022.210
Acknowledgments
We gratefully acknowledge the contribution of the physicians, epidemiologists, infection control practitioners, and laboratory staff at each participating hospital. We thank the staff at Public Health Agency of Canada in the Centre for Communicable Diseases and Infection Control, Ottawa, Ontario: Cecilia McClellan, Joelle Cayen, and Jessica Bartoszko. We also thank Sean Ahmed of the the National Microbiology Laboratory, Winnipeg, Manitoba. CNISP is a collaborative effort between sentinel hospitals across Canada, the Public Health Agency of Canada’s Centre for Communicable Diseases and Infection Control (CCDIC), the National Microbiology Laboratory (NML), and the Association of Medical Microbiology (AMMI) Canada.
Financial support
This work was supported by the Public Health Agency of Canada.
Conflict of Interest
Y.L. has received research grants from Becton Dickinson and Merck, unrelated to this work. S.S.H. received research funding from Finch Therapeutics Group for participating as a site principal investigator for a clinical trial. All authors report no conflicts of interest relevant to this article.