Obesity is a highly prevalent health problem. In Germany, 9·6 % of boys (11–17 years old) and 10·3 % of girls are obese( Reference Brettschneider, Schaffrath Rosario and Kuhnert 1 ), with an incidence rate of 2·7 % in school-aged children( Reference von Kries, Beyerlein and Müller 2 ). There is substantial forward tracking of obesity into adulthood( Reference Llewellyn, Simmonds and Owen 3 ) and a positive relationship exists between childhood BMI and adult mortality( Reference Park, Falconer and Viner 4 ). The disease burden is tremendous and is expressed in manifold ways. Considerable evidence supports the association between childhood obesity and both medical (high blood pressure, diabetes type 2) and psychological problems like depression, eating disorders and low quality of life( Reference Finkelstein, Graham and Malhotra 5 , Reference Sanders, Han and Baker 6 ). Additionally, childhood obesity is related to higher lifetime excess costs in adulthood( Reference Sonntag, Ali and Lehnert 7 ). Therefore, its successful and efficient treatment and its continuous improvement are essential topics.
Standard weight-loss treatments focus on modifying lifestyle factors like nutrition and physical activity. Besides initial positive effects on weight loss, their long-term success is limited( Reference Altman and Wilfley 8 ). Therefore, novel treatments are needed to increase their effectiveness, and focusing on the cognitive mechanisms underlying eating behaviour is one such compelling new approach. According to dual process models( Reference Strack and Deutsch 9 ), our behaviour is regulated via two processes or systems: the reflective and the impulsive system. Eating behaviours are largely considered to be automatic, involuntary behaviours triggered by internal (e.g. negative emotions) and external cues (e.g. availability of food). The strength of these ‘obesogenic’ eating patterns differs between normal- and overweight persons. For example, there is convincing evidence for enhanced reactivity to food stimuli in overweight compared with normal-weight individuals( Reference Hendrikse, Cachia and Kothe 10 , Reference Werthmann, Jansen and Roefs 11 ). Thus, modifying these altered cognitive processes constitutes a promising approach in the design of novel intervention strategies because cognitive biases with respect to attention, associations and reactions could explain the gap between knowledge about healthy lifestyles and their implementation( Reference Jansen, Houben and Roefs 12 , Reference Turton, Bruidegom and Cardi 13 ).
One strategy in cognitive bias modification is the approach–avoidance training (AAT)( Reference Kakoschke, Kemps and Tiggemann 14 ). AAT aims to modify automatic action tendencies by training participants to avoid tempting stimuli and approach alternative stimuli, typically by pushing and pulling a joystick. It has been shown that AAT successfully reduced relapse rates in alcohol-dependent patients( Reference Eberl, Wiers and Pawelczack 15 , Reference Wiers, Eberl and Rinck 16 ). In contrast, four recently published papers examining the effects of food-specific AAT in student samples yielded inconsistent results: three studies reported group differences with respect to approach–action tendencies after the training( Reference Dickson, Kavanagh and MacLeod 17 – Reference Schumacher, Kemps and Tiggemann 19 ), whereas one found no group differences( Reference Becker, Jostmann and Wiers 20 ). Furthermore, while Schumacher et al.( Reference Schumacher, Kemps and Tiggemann 19 ) observed an effect on food consumption, Dickson et al.( Reference Dickson, Kavanagh and MacLeod 17 ) failed to find such an effect. Moreover, a recent uncontrolled study( Reference Brockmeyer, Hahn and Reetz 21 ) examined the effects of multisession AAT in a group of adults showing increased signs of eating pathology. A large significant reduction in approach–avoidance bias was reported and eating pathology scores dropped significantly between pre-treatment and the one-month follow-up. In conclusion, the training of approach–avoidance tendencies may be a promising method for bias modification( Reference Wiers, Rinck and Kordts 22 ), but previous results are less consistent compared with the alcohol domain( Reference Kakoschke, Kemps and Tiggemann 14 ). This could be for different reasons: research in the eating domain did not focus on clinical samples, which show a stronger approach bias, but mainly on non-clinical samples (students within the normal weight range). In addition, compared with the eating domain more studies in the alcohol domain applied a multiple session design, which presumably resulted in a greater reduction of approach bias. Besides this, even though alcohol consumption and food intake share common features( Reference Volkow, Wang and Tomasi 23 ), total abstinence of alcohol is the primary treatment goal. On the other hand, the establishment of healthy eating does not simply mean that snack foods should always be avoided. Moreover, there is no sharp distinction between ‘healthy’ and ‘unhealthy’ foods.
Besides approach–avoidance tendencies, automatic affective associations connected with a stimulus are a central component of the impulsive system( Reference Strack and Deutsch 9 ). A modification of automatic tendencies should therefore be accompanied by changes in affective associations. Since approach and association tendencies are both responses of the impulsive system( Reference Strack and Deutsch 9 ), it is assumed that modifying approach tendencies will be accompanied by a change in the evaluation tendencies of the respective stimuli. Studies that revealed positive training effects for an AAT on alcohol approach bias reported such a generalization to implicit associations as measured with the implicit association test (IAT)( Reference Wiers, Eberl and Rinck 16 , Reference Wiers, Rinck and Kordts 22 ). In a similar manner, positive associations with unhealthy or high-energy foods were reported( Reference Becker, Jostmann and Wiers 20 ). To the best of our knowledge, only one study has investigated the effects of a food-specific AAT on implicit food associations, finding no effect( Reference Maas, Keijsers and Rinck 18 ).
To summarize, there is preliminary evidence for the efficacy of an AAT in modifying approach bias towards (unhealthy) foods. Overall, there appears to be a lack of studies in overweight samples, especially in children and adolescents. Previous studies were conducted with adult samples (mainly students), and it is not clear whether children and adolescents can be trained with the same paradigms. In addition, trainings targeting approach–avoidance tendencies hardly ever employed explicit training instructions, which make the participants aware of the training goal. Instead, usually implicit training instructions, concealing the training goal, were used. There is some evidence that explicit and implicit training instructions yield similar treatment effects( Reference Wiers, Eberl and Rinck 16 ). However, it is an open question whether this applies to children and adolescents as well. Furthermore, there are no data on how many sessions are needed to cause a training effect. Recent studies often used single-session trainings and focused predominantly on one food item (chocolate), whereas multisession trainings with a wide range of stimuli are considered to be a necessary component of successful trainings( Reference Wiers, Gladwin and Hofmann 24 ). Prior to applying a randomized control group design, it is fundamental to test the feasibility of the training approach and the practicability of the implicit instructions. Therefore, the effects of an AAT were examined here in a group of overweight children and adolescents within a pilot study with a pre–post design. We expected that, at the end of the training, children and adolescents would show a training effect in their approach–avoidance tendencies. In addition, the potential generalization of the training to implicit associations with snacks was assessed. In an exploratory manner, we also looked to determine how many sessions were necessary to obtain a training effect. To evaluate the influence of the instruction mode, the children and adolescents were allocated to either an implicit or an explicit version of the AAT. In accordance with Wiers et al.( Reference Wiers, Eberl and Rinck 16 ), we hypothesized that both training conditions would modify approach tendencies and implicit associations.
Materials and methods
Participants
Recruitment took place at two paediatric inpatient rehabilitation clinics. Comparable to other studies in the alcohol domain, the setting implemented the AAT in combination with treatment as usual: all patients participated in a lifestyle weight-loss intervention encompassing theoretical and practical lessons on physical activity and nutrition as well as a cognitive-behavioural group training. Children and adolescents aged between 8 and 16 years, overweight or obese (BMI>90th percentile), not suffering from secondary obesity (obesity caused by a medical condition such as endocrine disorder or genetic syndrome) and not receiving physician-ordered pharmacological therapy for attention-deficit hyperactivity disorder were eligible for participation. All participants received written, standardized information, participation was voluntary and they could withdraw approval at any time without disadvantages for their treatment. Written informed consent was obtained from the children and their parents. The study was approved by the local ethics committee.
Sample characteristics
Altogether, fifty-nine (thirty-three female) overweight or obese children and adolescents with a mean age of 13·23 (sd 1·93) years took part in the study. Before intervention, their mean BMI standard deviation score (BMI-SDS) reached 2·52 (sd 0·52), and 10·2 % were classified as overweight and 89·8 % as obese. Based on the date of arrival, a cluster randomization was conducted: thirty participants were allocated to the explicit training condition, twenty-nine to the implicit training condition. There were no differences between the training groups in terms of gender (χ 2=1·36, P=0·24), age (t(57)=0·37, P=0·72), BMI-SDS (t(57)=1·29, P=0·20) or weight status (χ 2=0·82, P=0·37).
Procedure
All participants were trained individually in six sessions over two weeks as a supplemental treatment offer by the clinics. The first four sessions were attended on a daily basis, followed by the remaining two sessions after a break of two or three days. Training sessions were implemented consistently, either after breakfast or after lunch. The training schedule was implemented for theoretical (distributed learning) and organizational reasons (no therapies on weekends). Every session contained the AAT, including training and test trials (approximately 15 min). This training phase was framed by a short assessment of current hunger, appetite and mood, prior to and following the AAT. Additionally, each person completed the IAT in the first session (before the training) and the last session (after the training), these sessions lasting approximately 25–30 min.
Measures
Anthropometric data
The weight and height of each child were measured with a calibrated digital scale and a wall-mounted stadiometer. On that basis, the BMI-SDS was calculated( Reference Kromeyer-Hauschild, Wabitsch and Kunze 25 ). The BMI-SDS indicates the difference of the individual’s BMI compared with the average BMI of other children and adolescents of the same gender and age. According to national guidelines, overweight was defined as a BMI above the 90th percentile, obese as scores above the 97th percentile.
Approach–avoidance training
We decided to include vegetables instead of other sweet or savoury foods (such as fruits) to apply clearly distinct categories: fruits can also be considered as healthy in general, but consuming no more than two fruit portions daily is part of the education lessons for the participants of our study and we therefore did not want to confuse the children by training them to approach fruit snacks. Furthermore, vegetables in particular are even less frequently consumed than fruits, so there is a special need for promoting the consumption of vegetables( Reference Borrmann and Mensink 26 ). For the AAT, we used twenty photographs of high-energy snacks (e.g. chocolate, muffins, popcorn, pretzel sticks, crackers) and twenty pictures of vegetables (e.g. tomatoes, cucumber, pepper, carrots, beetroot). We tested the familiarity and frequency of consumption, the categorization as ‘healthy’ or ‘unhealthy’, and the participants’ willingness to taste that food item in a pilot study (conducted among 159 primary-school children). More than 98 % of the food items were correctly categorized as ‘healthy’ or ‘unhealthy’. Snack items were preferred and consumed slightly more often than vegetables. In the final picture set, only food items that were known and correctly named by at least 95 % of the children were included. Food items were presented on either a circular or square plate. All items were matched according to their colour.
During the AAT, participants were instructed to either pull the pictures presented closer to them or push them away using the joystick. When the participants pulled the joystick towards them, the size of the picture on the screen increased, imitating an approach reaction. When the joystick was pushed away, the size decreased, imitating an avoidance reaction.
The AAT consisted of five phases: (i) a practice phase; (ii) a pre-assessment phase (sixty pictures of snacks, vegetables and empty plates); (iii) the actual training phase (120 pictures of snacks and vegetables); (iv) a post-assessment phase (forty pictures of snacks and vegetables); and (v) the booster training phase (forty pictures of snacks and vegetables), which terminated the training session. Two different training conditions (implicit and explicit) were implemented. In both conditions, the participants were trained to pull the vegetables towards them and push the snack foods away, but the instructions differed. In the implicit condition, they were instructed to react to the shape of the plate (push square plates and pull circular plates). It was not mentioned during the training phases that the square plates were always filled with snacks and the circular ones with vegetables. In the explicit condition, children and adolescents were asked to react to the type of food (push snacks and pull vegetables). During the test blocks, all children and adolescents followed the implicit instructions. Participants’ response latencies were recorded, and the lowest 1 % and the highest 1 % of the reaction times, as well as trials registering incorrect movements, were excluded( Reference Baird, Rinck and Rosenfield 27 ). Based on participants’ mean response latencies, compatibility scores were calculated as the difference between the mean scores of ‘approach–snack’ and ‘avoid–vegetable’ stimulus–response combinations (pull snacks and push vegetables) minus ‘avoid–snack’ and ‘approach–vegetable’ ones (push snacks and pull vegetables)( Reference Becker, Jostmann and Wiers 20 , Reference Wiers, Rinck and Kordts 22 ). In addition, compatibility scores for snack stimuli and vegetable stimuli were calculated separately. For all scores, positive values indicate an effect corresponding to the intended training effect (more quickly pushing snacks and pulling vegetables).
Implicit association test
To measure implicit associations with snacks, participants completed a modified version of the single category picture IAT given by Karpinski and Steinman( Reference Karpinski and Steinman 28 ) before and after the training. Stimuli consisted of seven pictures of high-energy snacks (drops, lollipops, gummy bears, pastries, ice cream, pretzels, nuts, crisps)( Reference Blechert, Meule and Busch 29 ) and of seven positively (merry, great, fantastic, happiness, nice, peace, friend) and negatively (hate, disgusting, mean, pain, sad, misfortune, embarrassing) valenced words. To ensure that younger children with insufficient reading abilities could complete the test, verbal stimuli were provided via loudspeaker. The visual and auditory stimuli had to be sorted into one target category (snacks) and two attribute categories (good v. bad). We administered an IAT with four blocks: a practice block (twenty-four trials) followed by a congruent test block (seventy-two trials) and a practice block followed by an incongruent test block. In test blocks, the target category (snacks) was combined with either one of the attribute categories (good or bad) on one side (left or right) of the screen and the categorization responses were mapped to the same key. Based on the expected association, the block that required the same response for snacks and positive words was labelled the congruent block, while the block that required the same response for snacks and negative words was labelled the incongruent block. These blocks were presented in counterbalanced order.
To assess the strength of the implicit association, a difference score was calculated by subtracting the mean reaction time in the congruent block from the mean reaction time in the incongruent block. A positive score indicates a positive association with snacks and a negative score a negative association. The lowest 1 % and the highest 1 % of the reaction times and error trials were excluded( Reference Karpinski and Steinman 28 ).
Mood, hunger and appetite
To measure hunger (‘How hungry are you right now?’), appetite (‘How much do you feel like eating snacks/vegetables right now?’) and mood (‘How do you feel right now?’) as potential confounding factors, participants rated their current state on 5-point Likert scales ranging from ‘not at all’/‘very bad’ (=1) to ‘very much’/‘very good’ (=5) prior to and following the AAT in every single session.
Acceptance
To measure the acceptance of the AAT, participants rated their general liking of the training (‘How much did you like the computer game?’) after the last session on a 5-point Likert scale ranging from ‘not at all’ (=1) to ‘very much’ (=5).
Analyses
Our primary outcome measure was the change in action tendencies (measured with the AAT) over time. In the first step, we analysed data for potential confounding influences (age, gender, hunger, appetite, mood). Since no significant associations with our outcome measures were found, no covariates were included. To analyse the general effectiveness of the training, we examined the AAT compatibility scores of the six sessions using a mixed-factor ANOVA with the between-subjects factor being training condition (implicit v. explicit instructions) and the within-subjects factor being time (with baseline and the six post-assessment points). In addition, we analysed the change across all sessions with a repeated-measure ANOVA including only the very first and the very last assessment. In addition to the overall compatibility scores, separate analyses were conducted for snacks and vegetables. As a measure of the magnitude of the treatment effects, the partial η 2 values are reported. According to Cohen( Reference Cohen 30 ), partial η 2 values of about 0·01 can be classified as small, about 0·06 as medium, and values of 0·14 or greater as large effects. The course of the compatibility scores over the training sessions was analysed in an exploratory manner to determine the number of sessions necessary to create a training effect. In addition, each session was also analysed separately to test learning effects, comparing the compatibility scores at the beginning and at the end of a session. In general, conducting multiple tests yields the problem of cumulated α errors and usually requires an adjustment. According to Victor et al.( Reference Victor, Elsäßer and Hommel 31 ), this is not recommended for exploratory procedures, therefore we decided not to adjust for multiple testing.
To evaluate changes in the IAT difference scores, another mixed-factor ANOVA with the between-subjects factor being training condition (implicit v. explicit instructions) and the within-subjects factor being time (before and after training) was performed. Acceptance of the AAT and its association with the training effect were analysed on a descriptive and correlational basis. All analyses were performed using the statistical software package IBM SPSS Statistics version 23. Significance was set at P<0·05 in all analyses.
Results
Descriptive data
Table 1 displays the performance data of the children and adolescents in the AAT and IAT at the beginning of the training. There were no significant differences between the training conditions.
Table 1 Descriptive data at pre-test among fifty-nine overweight/obese children and adolescents aged 8–16 years (twenty-six boys), recruited in inpatient rehabilitation clinics in Germany (January–December 2014)

AAT, approach–avoidance training; IAT, implicit association test.
Approach–avoidance training
Pre–post comparisons
The mixed-factor ANOVA (see Table 2 for details) including seven assessment points revealed a medium-sized, significant main effect of time on the compatibility scores. Neither the training group factor nor the interaction of time and training condition reached significance. Analysing the overall effect of the training including only the first and last assessment points revealed a large effect of time (see Fig. 1), with no significant effects for either training condition or time × training condition.
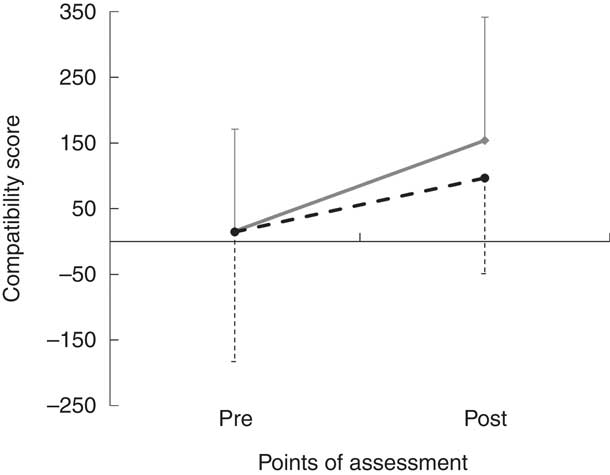
Fig. 1 Compatibility scores before (pre) and after (post) approach–avoidance training using implicit(![]() )and explicit (
)and explicit (![]() ) approaches among fifty-nine overweight/obese children and adolescents aged 8–16 years (twenty-six boys), recruited in inpatient rehabilitation clinics in Germany (January–December 2014). Values are means, with their standard deviations represented by vertical bars (for clarity, standard deviations are displayed in only one direction for each condition)
) approaches among fifty-nine overweight/obese children and adolescents aged 8–16 years (twenty-six boys), recruited in inpatient rehabilitation clinics in Germany (January–December 2014). Values are means, with their standard deviations represented by vertical bars (for clarity, standard deviations are displayed in only one direction for each condition)
Table 2 Pre–post comparisons of AAT compatibility scores by mixed-factor ANOVA among fifty-nine overweight/obese children and adolescents aged 8–16 years (twenty-six boys), recruited in inpatient rehabilitation clinics in Germany (January–December 2014)

AAT, approach–avoidance training.
Separate analyses for the snack and vegetable compatibility scores confirmed the picture of the analyses reported above. With respect to the snack compatibility effect, we observed a significant main effect of time when including seven assessment points, as well as when including only the first and last assessments. The effect of the training condition was not significant in either one of the two analyses. A significant interaction effect was observed only when just two time points were included v. seven assessments. With respect to the vegetables compatibility effect, the main effect of time was significant when including all seven assessment points, but not with only two assessment points. There was neither a significant main effect of the training condition nor a significant time × training condition interaction in either analysis.
Exploratory analyses of the training course
On an exploratory level, we analysed the course of the overall compatibility scores over time through pairwise comparisons. Since we did not find a consistent influence of the training condition, this factor was no longer included in the analyses. In a first step, we examined the difference between the pre-test score of the first session (initial baseline) and the post-training values of each session. At the end of each session, the compatibility score was significantly higher than at baseline (see Table 3).
Table 3 Mean compatibility scores over the AAT sessions and significance of changes among fifty-nine overweight/obese children and adolescents aged 8–16 years (twenty-six boys), recruited in inpatient rehabilitation clinics in Germany (January–December 2014)

AAT, approach–avoidance training.
* Change of scores within session from pre- to post-assessment.
† Change of baseline (pre-score of session 1) compared with the post-score of the particular session.
In addition, the changes within each session were investigated. Significant increases in the compatibility scores were observed only for the first two sessions (see Table 3), with large effect sizes (session 1: F(1, 54)=18·11, P<0·001, η 2=0·25; session 2: F(1, 54)=9·98, P=0·003, η 2=0·16).
Implicit association test
Contrary to our assumptions, our sample showed negative associations with snacks at pre-test (mean −26·4 (sd 87·5); t(56)=−2·28, P=0·026). We observed neither a significant change over time (F(1, 54)=0·14, P=0·712), nor significant effects of the training condition (F(1, 54)=0·08, P=0·773) or the interaction (F(1, 54)=0·04, P=0·837). Correlational analyses revealed a negative correlation between the post-training compatibility scores and the post-training IAT scores (r=−0·29, P=0·03), indicating that more positive associations with snacks in the IAT went along with a stronger approach to snacks in the AAT. No significant correlations were found with age or with BMI-SDS (see Table 4).
Table 4 Correlations of IAT difference scores with age and BMI-SDS among fifty-nine overweight/obese children and adolescents aged 8–16 years (twenty-six boys), recruited in inpatient rehabilitation clinics in Germany (January–December 2014)

IAT, implicit association test; BMI-SDS, BMI standard deviation score.
Additional analyses
In addition, we observed no significant correlations of compatibility scores (pre, post, change) with age or BMI-SDS (see Table 5). The mean liking score of the training was 2·46 (sd 1·04), indicating an acceptance of the AAT in the middle range. There were no significant differences between boys and girls (t(57)=−0·57, P=0·6), but between training conditions (t(57)=2·14, P=0·037), with higher acceptance of the explicit condition (mean 2·73 (sd 0·98)) than of the implicit condition (mean 2·17 (sd 1·04)). We found no correlation of the acceptance scores with age (r=−0·2, P=0·127). There was a significant correlation between the acceptance scores and the change in the compatibility scores, i.e. higher acceptance was associated with a more pronounced rise in the compatibility score (see Table 5).
Table 5 Correlations of age, BMI-SDS and acceptance with AAT compatibility scores among fifty-nine overweight/obese children and adolescents aged 8–16 years (twenty-six boys), recruited in inpatient rehabilitation clinics in Germany (January–December 2014)

BMI-SDS, BMI standard deviation score; AAT, approach–avoidance training; Δ compatibility scores, post-compatibility score – pre-compatibility score.
Discussion
The primary aim of our study was to explore the trainability of action tendencies towards vegetables and snack foods by means of an AAT in overweight children and adolescents. Our second aim was to explore whether the changes in action tendencies were accompanied by changes in implicit associations. At an exploratory level, we addressed differences between implicit and explicit instructions and the number of sessions needed to elicit a significant training effect. To the best of our knowledge, the present study is the first to examine a food-specific AAT in a group of overweight children and adolescents.
As hypothesized, the children and adolescents successfully learned to alter their automatic tendencies. In addition, our results show that the AAT training was well accepted, with slightly higher acceptance scores for the explicit instruction. This might be due to the fact that this version offers a more varied game, since instruction formats have to change between training and testing phases. We did not find an influence of gender or age, suggesting that the training programme is applicable regardless of age or gender.
There is already evidence for a successful implementation of an AAT in this age group, focusing on anxiety in pre-adolescent children( Reference Huijding, Field and Houwer 32 ) and adolescent smokers( Reference Kong, Larsen and Cavallo 33 ). In line with these studies, our results underscore that automatic approach tendencies are trainable in children and adolescents, too. Up to now, current studies in the context of nutrition behaviour have solely focused on normal-weight adults, mainly students, and the pattern of results was inconsistent. In line with reports from four other studies( Reference Dickson, Kavanagh and MacLeod 17 – Reference Schumacher, Kemps and Tiggemann 19 , Reference Brockmeyer, Hahn and Reetz 21 ), we found a significant change in automatic approach–avoidance tendencies, with effect sizes in the medium-to-large range, whereas Becker et al.( Reference Becker, Jostmann and Wiers 20 ) failed to find such a training effect in three experimental studies. Despite the fact that all of the studies mentioned above examined the effects of a food-specific AAT, they differ in many respects (such as training condition or stimulus material), aggravating the comparison. Due to the lack of a control group, one might overestimate the results; however, two other recent controlled studies( Reference Maas, Keijsers and Rinck 18 , Reference Becker, Jostmann and Wiers 20 ) reported similar results. One relevant factor explaining the controversial findings might be the stimulus materials or comparisons included. Our separate analyses for snacks and vegetables revealed significant changes in action tendencies for both stimuli, but less so for vegetables: effect sizes were lower than for snacks, and the analyses for vegetables were significant only when including all six post-intervention scores. This indicates that the training may be more effective for increasing avoidance of snacks, while effects on the approach of vegetable stimuli are less convincing. This is in line with studies showing trainability for the avoidance of unhealthy choices (mainly chocolate), but not for the approach of healthy choices( Reference Eberl, Wiers and Pawelczack 15 , Reference Wiers, Eberl and Rinck 16 , Reference Becker, Jostmann and Wiers 20 , Reference Wiers, Rinck and Kordts 22 ). Our results extend previous research with respect to the stimulus material, by applying a snack food v. vegetables paradigm. Regarding the trainability of approach reactions, only Maas et al.( Reference Maas, Keijsers and Rinck 18 ) were able to observe such an effect (with e.g. a bell pepper, cucumber and apple as low-energy food stimuli and chocolate, French fries and hamburgers as high-energy food stimuli). In addition, moderating or mediating influences might play a role. Some authors( Reference Eberl, Wiers and Pawelczack 15 ) argue that the stimulus materials must be salient in order to elicit training effects. This is in line with our data with respect to the acceptance of the presented stimulus materials. Vegetables are less well liked than snack foods and that could be an explanation for their lack of trainability. In general, it should be noted that our results apply to the comparison of snack foods and vegetables and are therefore not fully comparable with previous results. We did not observe significant training effects on implicit associations. The evidence on the effect to implicit associations is indeed quite inconsistent: positive associations were mainly reported in the context of alcohol drinking( Reference Wiers, Eberl and Rinck 16 , Reference Wiers, Rinck and Kordts 22 ), whereas for food-related stimuli, mainly non-significant effects were reported( Reference Maas, Keijsers and Rinck 18 , Reference Becker, Jostmann and Wiers 20 ). One possible explanation for this might be that the category of ‘snacks’ is fuzzier than the category of ‘alcoholic beverages’, the latter of which can be classified more easily.
Snack items are popular among children and adolescents and are consumed quite often( Reference Mensink, Kleiser and Richter 34 ). Thus, one would expect that particularly overweight children and adolescents would exhibit a strong preference for snack items( Reference Lanfer, Knof and Barba 35 ). However, we observed unexpected negative associations with snacks at the beginning of the training. Analogously, some studies reported greater choices of healthy foods in youngsters( Reference Craeynest, Crombez and Haerens 36 ) and implicit negative associations with snacks in obese adults( Reference Roefs and Jansen 37 ). In accordance with Maas et al.( Reference Maas, Keijsers and Rinck 18 ), one might speculate that the clinical setting of our study goes along with a strong weight-loss control motivation of the obese children and adolescents, and this might serve as a buffer against the temptations of snack foods. From a statistical point of view, the already negative associations with snack foods might have prevented us from inducing even more pronounced negative associations. Future studies with larger sample sizes should analyse data on the basis of the initial implicit associations.
Despite the general lack of a generalization effect, we observed a negative correlation of the AAT compatibility score with the IAT score, indicating that the tendency to avoid snacks and to approach vegetables was associated with more pronounced negative associations with snacks. Because this relationship existed only after, but not before the training, an influence of the AAT may be present, which should be studied further in future studies.
In line with other studies( Reference Wiers, Eberl and Rinck 16 ), our results do not indicate differences between the two instruction formats: implicit v. explicit. Only when we included just the pre- and post-training data there was a significant time × instruction interaction for snacks. When examining the whole course of the training with seven assessments, the interaction effect was no longer significant. These preliminary data suggest that there may be no difference in treatment efficacy. Due to the fact that an implicit training version is more closely related to the basic idea of AAT, which is to modify automatic, implicit approach tendencies, it might be more adequate to apply the implicit training instruction. Regarding the number of sessions needed to elicit a reliable training effect, our data suggest that two sessions might be sufficient: after two, we observed a consolidation of the effect. This result contradicts that reported by Eberl et al.( Reference Eberl, Wiers and Pawelczack 38 ), who detected the strongest effects after six sessions. Therefore, the number of sessions necessary should be further explored in future studies. It must be considered that two sessions might be sufficient to show an effect of the training, but this is not automatically connected with a clinical effect (e.g. weight loss or changes in eating behaviour). Since we did not systematically vary the number of training sessions and only assessed the learning effect from session to session, it is premature to draw any conclusions with respect to the number of training sessions needed to elicit a ‘clinically meaningful’ training effect. Moreover, our results only pertain to a training effect in the AAT itself. Due to the exploratory nature of our multiple testing format, the risk of false positive conclusions can arise, and therefore our data should be interpreted with caution. Six sessions presenting the same content might become boring and decrease the recipients’ interest over time. We cannot rule out the fact that a loss of interest in the training programme might influence the subsequent learning curve. In general, a gamification of the AAT for children is suggested( Reference Boendermaker, Prins and Wiers 39 ) to increase their motivation and acceptance. To ensure their motivation, continuous feedback on the points already earned combined with reinforcement strategies (e.g. smileys) might be helpful tools in this context. Taken together, our results provide preliminary evidence that food-related approach–avoidance tendencies can be successfully modified. Further research is needed to examine not only the feasibility of AAT but also its efficacy in clinical and non-clinical settings.
Strengths and limitations
On the one hand, several limitations of the current study should be pointed out. First, we did not include a placebo training control group. This means that we cannot conclude definitively that our observed changes over time are caused by our training programme. Second, our pilot study contained only pre- and post-assessments. We have no further information about the stability of the observed changes later on. Third, our sample is quite small and allocation to the two instruction modes was based on the participants’ arrival in the clinic. In addition, we have no data on whether the training was associated with a change in the nutritional behaviour of the children and adolescents, or on their explicit liking of the food items. Since we compared snack foods with vegetables, we cannot draw any conclusion about the effects of a snack v. fruit comparison, for example. Future research on that topic is warranted.
On the other hand, the strengths of our study should be mentioned, too. First, we conducted a multisession training programme, recently recommended( Reference Eberl, Wiers and Pawelczack 38 ) as a necessary ingredient of a successful training. Second, we considered different instruction conditions, and we included a variety of snack and vegetable items, increasing the external validity of our approach. Third, we included children and adolescents who were already overweight from two clinical settings, increasing the generalizability of our results to the relevant clinical target group of interest. Fourth, anthropometric data were objectively assessed, avoiding the problem of invalid self-report data in this sensitive field( Reference Connor Gorber, Tremblay and Moher 40 ). Finally, by including multiple outcome measures, we can add to the current knowledge on the generalizability of training effects.
Conclusion
In summary, our results showed that AAT is applicable in overweight children and adolescents. Not only is it accepted by the participants, but it is also associated with the expected positive effects. We did not find notable differences between an implicit and an explicit training condition, suggesting that even children can profit from the implicit version of the AAT. Further studies including longer follow-up assessments and control groups are needed.
Acknowledgements
Acknowledgements: Special thanks are extended to the participating rehabilitation clinics, Spessartklinik Bad Orb and AHG Klinik Beelitz-Heilstätten, and the children and adolescents who volunteered for this trial. Thanks also to K. Lieck for programming the computer tasks. Financial support: This work was supported by the German statutory pension insurance scheme under Grant 8011-106-31/31.113. The funding organization played no role in designing and conducting the study, the data collection, its analysis and interpretation. Conflict of interest: None. Authorship: P.W. designed the study; M.R. developed the AAT and supported the data analysis; M.G. and P.W. were responsible for the statistical analysis; M.M. conducted the trainings. All authors took an active part in writing the paper. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the Ethics Committee of the University of Potsdam, Germany. Written informed consent was obtained from all patients and their parents.









