Introduction
In Japan, people who have stolen account for approximately 50% of criminal offenders; therefore, it is vital that recidivism prevention measures for people who have stolen are improved (Research and Training Institute of the Ministry of Justice, 2014). However, the rehabilitation of people who have stolen is insufficiently developed compared with drug offenders who have similar recidivism rates (Research and Training Institute of the Ministry of Justice, 2009). It is difficult to systematize preventive measures for people who steal due to various reasons (Research and Training Institute of the Ministry of Justice, 2014). One factor is that some people who steal have kleptomania, a mental illness (Takemura, Reference Takemura2016).
According to the Diagnostic and Statistical Manual of Mental Disorders (5th edn; DSM-5), with kleptomania, the purpose is to engage in the act of stealing itself (rather than a desire to acquire the objects stolen), and the stealing behaviour is maintained by a release of tension or pleasure. Although the goal of shoplifting is personal gain, it has been found that approximately 4–24% of those arrested for shoplifting have kleptomania (American Psychiatric Association, 2013). A previous study that compared 37 persons with kleptomania and 35 shoplifters indicated that those with kleptomania reported a significantly higher number of prior stealing behaviours than shoplifters (Sarasalo et al., Reference Sarasalo, Bergman and Toth1997). In addition, it has been highlighted that some shoplifters are unable to resist their impulses to steal (McElroy et al., Reference McElroy, Hudson, Pope and Keck1991), and it is often assumed that kleptomania and shoplifting exist on a continuum.
Although kleptomania was positioned as being on the obsessive-compulsive spectrum in the 1990s, it is now increasingly considered an addiction due to its similarity to substance use disorder and its response to opioid antagonists (naltrexone), which are effective in treating addiction (Grant, Reference Grant2006). Furthermore, pharmacotherapy and psychological support for other psychiatric disorders have been used for kleptomania.
Regarding medication, there have been inconsistent findings on the effectiveness of treating kleptomania with selective serotonin reuptake inhibitors, which are used to treat obsessive-compulsive disorder (Grant, Reference Grant2006). Recently, it has been suggested that naltrexone, which is thought to reduce cravings for addictive behaviours, is also effective in improving kleptomania symptoms. Furthermore, it has been reported that kleptomania symptoms were reduced more in the group of 11 patients who received naltrexone than in the group of 12 patients who received a placebo (Grant et al., Reference Grant, Kim and Odlaug2009). In addition, behavioural therapy such as aversion therapy is considered to be effective for kleptomania (Keutzer, Reference Keutzer1972). Furthermore, cognitive behavioural therapy (CBT), which has also proved effective for addiction, is utilized to treat kleptomania (Christianini et al., Reference Christianini, Conti, Hearst, Cordás, de Abreu and Tavares2015; Kohn and Antonuccio, Reference Kohn and Antonuccio2002).
CBT aims to reduce problematic behaviours by adjusting antecedent–behaviour–consequence contingency and establishing operation of problematic behaviours, controlling the environment, and acquiring more adoptive alternative behaviours (Shimada and Nomura, Reference Shimada and Nomura2008). Furthermore, CBT has been shown to be effective in the treatment of addiction (Korn and Shaffer, Reference Korn and Shaffer2004; Magill and Ray, Reference Magill and Ray2009). In contrast, a review for substance use disorders suggested that the strength of automatic responses, which are related to higher rates of relapse or drop-out, can interfere with the effectiveness of CBT (Stevens et al., Reference Stevens, Verdejo-García, Goudriaan, Roeyers, Dom and Vanderplasschen2014). It has been indicated that emotional arousal reduces self-awareness and increases addictive behaviour as an automatic response (Goldstein et al., Reference Goldstein, Craig, Bechara, Garavan, Childress, Paulus and Volkow2009). In particular, as negative affect has been suggested to influence relapse, the usefulness of interventions to improve the tolerance to negative affect has been highlighted (Hsu et al., Reference Hsu, Collins and Marlatt2013). Furthermore, it has also been suggested that mindfulness can improve awareness and acceptance of psychological and physical reactions to negative affect and enable people to consciously observe how emotions are aroused and transitioned, rather than engaging in addictive behaviour as an automatic habitual response (Witkiewitz et al., Reference Witkiewitz, Bowen, Harrop, Douglas, Enkema and Sedgwick2014a). In fact, it has been reported that the latter is more effective in the treatment of addiction when the cognitive behavioural approach of relapse prevention is implemented alone or when mindfulness is added to relapse prevention (Witkiewitz et al., Reference Witkiewitz, Warner, Sully, Barricks, Stauffer, Thompson and Luoma2014b).
Regarding kleptomania, the amnesia of stealing behaviour and stronger impulsivity than other addictions have been observed (Baylé et al., Reference Baylé, Caci, Millet, Richa and Olié2003; Grant, Reference Grant2004), and it is assumed that many patients steal as an automatic response. In addition, the fact that stealing is a criminal offence has resulted in a strong social and occupational dysfunction, in addition to a strong sense of guilt and shame after stealing (Grant and Odlaug, Reference Grant and Odlaug2008). In fact, an interview study of 22 patients with kleptomania revealed that stress/anxiety was the most prevalent trigger for stealing behaviour in approximately half of the patients, followed by loneliness/depression (Grant and Kim, Reference Grant and Kim2002), suggesting the influence of negative affect. Thus, it is assumed that CBT together with mindfulness may be effective for treating kleptomania.
In areas of Japanese forensics and criminology, group-based CBT is the mainstream practice due to its advantageous cost and time savings (Nomura et al., Reference Nomura, Shimada and Kamimura2020). Furthermore, the prevalence of kleptomania is low, ranging from 0.3 to 0.6% (American Psychiatric Association, 2013), and it has been shown that it is common for patients who perceive stealing as a moral issue to reject the diagnosis of kleptomania, partly because stealing is generally regarded as a crime (Christianini et al., Reference Christianini, Conti, Hearst, Cordás, de Abreu and Tavares2015). In addition, it has been reported that approximately 80% of patients with kleptomania who were instructed to continue treatment discontinued within 3 months (Takemura, Reference Takemura2013). Therefore, it is assumed that the rolling-group format is useful. This is an open-ended format that allows participants to join a treatment programme at any time and where each participant works through the sessions at their own pace. Therefore, the rolling format has advantages in terms of flexibility of participation, group cohesiveness, gradual intervention, and individualization (Ware and Bright, Reference Ware and Bright2008). In fact, it has been shown to be effective in reducing drop-outs in a sex offender programme (Howard et al., Reference Howard, de Almeida Neto and Galouzis2019).
Many previous studies have focused on the reduction of stealing behaviour or impulse to steal as outcome variables (e.g. Christianini et al., Reference Christianini, Conti, Hearst, Cordás, de Abreu and Tavares2015). However, it has been highlighted that those patients with kleptomania generally experience strong social and occupational dysfunction and poor quality of life (QOL) (Grant and Odlaug, Reference Grant and Odlaug2008). In addition, a study involving gambling addiction showed that patients who relapse experience higher psychological distress following CBT and have lower QOL at follow-up (Sander and Peters, Reference Sander and Peters2009). Therefore, it is assumed that QOL and psychological stress responses are useful indicators for predicting the relapse of stealing behaviour.
This study aimed to examine the effectiveness of cognitive behavioural group therapy (CBGT) combined with mindfulness on kleptomania symptoms and QOL.
Method
Participants
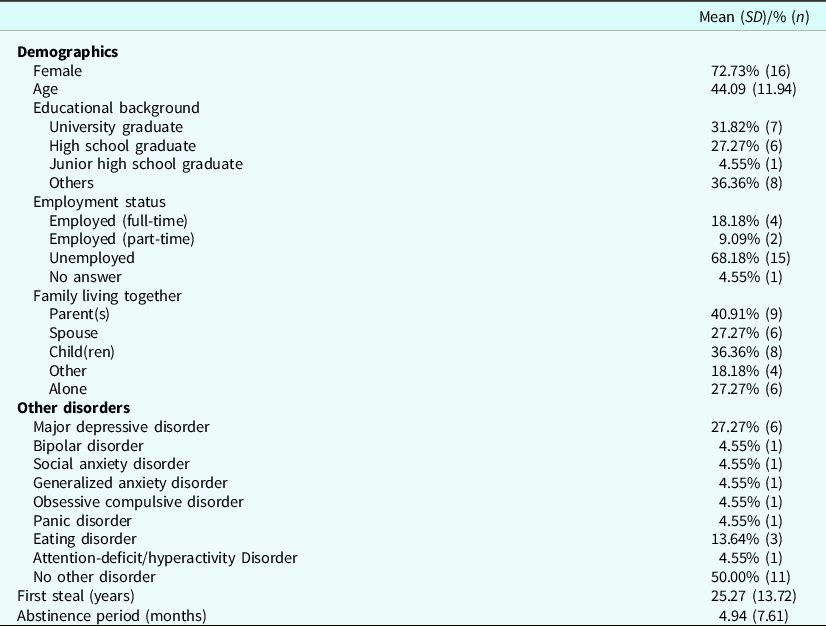
A total of 37 patients aged 20 years or older, who had been diagnosed with kleptomania by qualified medical doctors, and had participated in a CBGT combined with mindfulness treatment programme (between September 2016 and August 2021), were included in this study. Those who were judged by doctors of the psychiatric hospital to be incompatible with the group format or who were judged to have difficulty participating in the study were excluded. In Japan, participation in psychotherapy is directed by the doctor’s judgement. Of the 37 participants who provided informed consent to participate in the study, six discontinued during the programme, two had missing values, two failed to respond to initial questionnaires, and five failed to respond to questionnaires at the end. Therefore, only 22 participants (six men), with a mean age of 44.09 years (SD = 11.94), completed all 12 sessions of the programme and responded to questionnaires at the beginning and end of the programme. Of the 15 patients who were excluded, three were interrupted due to arrest or imprisonment for recurrent stealing behaviour. The demographic information collected included sex, age, education level, occupation, whether the patient was living with their family, co-morbid disorders, and stealing experience. Participants’ demographic data are summarized in Table 1. Regarding co-morbidities, those with personality disorders were not included in our study.
Table 1. Demographic of participants
Measures
Outcome variables
Kleptomania symptoms
The Kleptomania Symptom Assessment Scale (K-SAS) is an 11-item self-report scale designed to measure the symptoms of kleptomania (Asami et al., Reference Asami, Nomura, Shimada, Ohishi and Ohishi2020). A 5-point scale was calculated; thus, the total score of the scale ranges from 0 to 44, where 8–20 is regarded as mild, 21–30 as moderate, and 31–44 as severe kleptomania. Each item assesses the average symptom based on activities during the previous week. In fact, regarding CBGT for kleptomania, lower K-SAS scores have been reported for 10 participants in the maintenance treatment (>20 sessions) than eight in the initial treatment (≤20 sessions) (Christianini et al., Reference Christianini, Conti, Hearst, Cordás, de Abreu and Tavares2015).
QOL
The General Health Questionnaire-28 (GHQ-28) is a valid instrument for the assessment of mental health (Nakagawa and Daibo, Reference Nakagawa and Daibo1985). It consists of 28 items that assess four factors: ‘somatic symptoms’, ‘anxiety and insomnia’, ‘social dysfunction’ and ‘severe depression’. In addition, a 4-point rating scale was calculated in accordance with the standard method (2-point). Thus, total scores ranged from 0 to 28, with higher scores reflecting more severe mental health symptoms. A total cut-off point of 6 has been identified as distinguishing between healthy functioning and neurosis. For ‘somatic symptoms’ and ‘anxiety and insomnia’, a cut-off point of 4, and for ‘social dysfunction’ and ‘severe depression’, a cut-off point of 3 have been identified as distinctions between mild and moderate symptoms.
Psychological stress response
The Stress Response Scale-18 (SRS-18) is a valid instrument used to assess psychological stress responses that occurred over the preceding 2 or 3 days (Suzuki et al., Reference Suzuki, Shimada, Miura, Katayanagi, Umano and Sakano1997). It is an 18-item self-report measure that assesses three factors, ‘depression-anxiety’, ‘irritability-anger’ and ‘helplessness’. A 4-point rating scale was used; thus, the total score ranged from 0 to 54, with higher scores reflecting greater severity of stress responses.
Process variables
Reward perception
The Environmental Reward Observation Scale (EROS) is a valid instrument for assessing environmental rewards for life in general (Kunisato et al., Reference Kunisato, Takagaki, Okajima, Nakajima, Ishikawa, Kanai and Yamawaki2011). It is a 1-factor, 10-item self-report measure. A 4-point rating scale was used; thus, the total score ranged from 10 to 40, with a lower score reflecting poorer levels of environmental reward.
Distress tolerance
The Distress Tolerance Scale (DTS) is a valid instrument for assessing the tolerance for unpleasant emotional states (Oe, Reference Oe2010). It is a 15-item self-report measure. A 5-point rating scale was used; thus, the total score ranged from 15 to 75, with higher scores reflecting lower levels of tolerance for unpleasant emotions.
Intervention
The content of the programme consisted of CBT based on functional analysis and mindfulness (Table 2). It was developed based on a mindfulness and goal setting-focused CBT programme used for the treatment of drug offenders in Japan (Nomura et al., Reference Nomura, Abe and Shimada2016). This programme consisted of 12 sessions that occurred weekly, each lasting for 90 minutes.
Table 2. Content of the programme
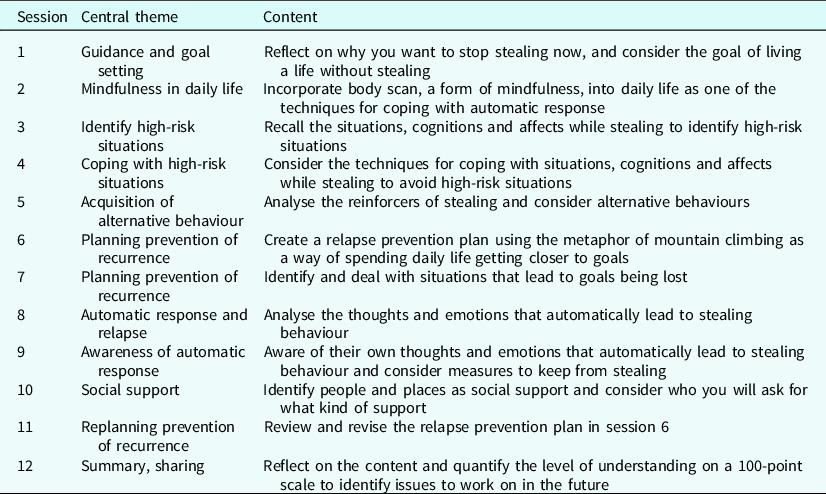
Functional analysis is a basic intervention to identify and control the antecedents of stealing behaviour, identify the reinforcers of the behaviour, and acquire alternative behaviours. With kleptomania, the assumption is that stealing behaviour is most likely triggered as an automatic response to stealing-related stimuli. Therefore, mindfulness is used as an intervention to improve the awareness of emotional arousal and control stealing behaviour whenever triggered by it.
In session 2, as a mindfulness intervention, participants received psychoeducation on the body scan technique (Bowen et al., Reference Bowen, Chawla and Marlatt2011), which allows a person to increase their awareness of their bodily experiences in the present moment. The subjects practised the technique by following the leader’s instruction. Furthermore, subjects were encouraged to practise the body scan daily whenever possible. In addition to promoting understanding through the observation of practice during the programme and the self-reporting of post-experience impressions and insights, we assigned homework to be performed at a set time each day. In session 8, participants analysed stealing behaviour as an automatic response to emotional arousal, and in session 9, we practised the body scan again in the programme and confirmed mastery through self-reports of awareness and acceptance of the automatic response in stealing behaviour. We did not obtain data on the implementation of the body scan homework.
Treatment was delivered in a psychiatric hospital. Each session involved approximately four to eight participants. This programme was conducted by a group leader and subleader, who were psychologists specializing in CBT, and the hospital staff (psychologists, psychiatric social workers, and nurses). The programme was operated in a rolling format so that participants could join the programme at any time, and each participant proceeded sequentially through sessions 1 to 12. Therefore, each session was simultaneously treated in one programme.
Procedure
Participants who had been referred to the CBGT programme by a doctor and were 20 years or older were asked to answer a questionnaire at the time of their initial participation and at the conclusion of the programme. In addition, subjects were provided with a written and verbal description of the study as part of the informed consent procedure to participate in the study, along with a pamphlet. Participation in the study was voluntary, and the protection of personal information was emphasized.
Statistical analyses
Data analysis was conducted using SPSS Statistics 28 and AMOS 28. First, we calculated the differences in the change of each variable between the beginning and end of the programme by employing a t-test. Furthermore, Pearson’s correlation coefficient was used to determine the correlations between the changes in each variable from the start to the end of the programme. In addition, an analysis of covariance structure was used to examine the influence of the process variables on the outcome variables.
Results
In terms of kleptomania symptoms at the time of participation in the programme, the overall mean score for the K-SAS was 18.77 (SD = 9.01; n = 22; 5/22 severe, 2/22 moderate, 14/22 mild, and 1/22 zero). The overall mean score for the GHQ-28 was 14.68 (SD = 7.84), and 19/22 participants scored 6 or more (cut-off). For the subscales of GHQ-28, nine participants were considered moderate for ‘somatic symptoms’, 16 were moderate for ‘anxiety and insomnia’, 13 were moderate for ‘social dysfunction’ and 15 were moderate for ‘severe depression’. The mean score of the SRS-18 was 28.32 (SD = 13.37), which corresponds to ‘rather high’ in the normative data given by Suzuki et al. (Reference Suzuki, Shimada, Miura, Katayanagi, Umano and Sakano1997).
Moreover, Cronbach’s alpha for each variable was .86 for K-SAS, .93 for GHQ-28, .94 for SRS-18, .83 for EROS, and .88 for DTS. These indicated that each scale has good internal consistency.
Changes in outcomes and process variables
The changes in each variable between the beginning and end of the programme were analysed using a t-test. Regarding the outcome variables, results showed that the K-SAS decreased (t 21 = 4.31, p < .01), as did the GHQ-28 (t 21 = 2.21, p < .05) and the SRS-18 (t 21 = 2.92, p < .01) (Table 3). For the process variables, DTS decreased (t 21 = 4.64, p < .01), and EROS highlighted an increasing trend (t 21 = −2.02, p < .10).
Table 3. Comparison of variables between pre- and post-programme

K-SAS, Kleptomania Symptom Assessment Scale; GHQ-28, General Health Questionnaire-28; SRS-18, Stress Response Scale-18; DTS, Distress Tolerance Scale; EROS, Environmental Reward Observation Scale. **p<.01, *p<.05, †p<.10.
Moreover, four participants had a relapse of stealing behaviour while participating in the programme, 15 performed no stealing, and three made no response. Those who relapsed had fewer years of education (t 17 = 1.88, p < .10), and higher K-SAS scores both at the beginning (t 17 = −5.28, p < .01) and the end of the programme (t 17 = −4.24, p < .01), than those with no relapse.
Influence of process variables on outcome variables
An analysis of the correlations between the changes in each variable from the beginning to the end of the programme showed that K-SAS was not correlated with GHQ-28 and SRS-18, while GHQ-28 and SRS-18 were strongly positively correlated (r = .85, p < .01; Table 4). Regarding the process variables, no correlation was found between EROS and DTS. For the association between process and outcome variables, EROS indicated a moderate negative correlation with GHQ-28 (r = −.62, p <.01), and a strong negative correlation with SRS-18 (r = −.70, p < .01). The DTS showed a moderate positive correlation with the GHQ-28 (r = .44, p < .05) and the SRS-18 (r = .53, p < .05), and a moderate positive correlation trend with the K-SAS (r = .40, p < .10).
Table 4. Correlation of the amount of change in each variable

K-SAS, Kleptomania Symptom Assessment Scale; GHQ-28, General Health Questionnaire-28; SRS-18, Stress Response Scale-18; DTS, Distress Tolerance Scale; EROS, Environmental Reward Observation Scale. **p<.01, *p<.05, †p<.10.
Furthermore, an analysis of covariance structure was conducted to examine the influence of the process variables on the outcome variables and to explore the interaction model of the outcome variables. Results showed that an improvement in DTS resulted in an improvement of K-SAS. In addition, it was highlighted that EROS and DTS affected the improvement of SRS-18 and GHQ-28 (RMR=2.25, GFI=.98, AGFI=.93, CFI=1.00, RMSA=.00, AIC=21.33 (Fig. 1).

Figure 1. Model in which a change in process variables affects a change in outcome variables.
DTS, Distress Tolerance Scale; EROS, Environmental Reward Observation Scale; K-SAS, Kleptomania Symptom Assessment Scale; SRS-18, Stress Response Scale-18; GHQ-28, General Health Questionnaire28.
**p<.01, *p<.05.
Discussion
This study examined the effects of a programme consisting of CBGT and mindfulness on kleptomania. The results suggest that this programme may improve the symptoms, QOL and psychological stress responses of people with kleptomania. Therefore, the programme may be expected to be a useful intervention for kleptomania.
Furthermore, it was suggested that the programme contributed to improved reward perception in the living environment and to increased tolerance of unpleasant emotions as a process variable leading to recovery. Although the sample size was small, the result of the covariance structure analysis revealed the recovery process, as the improvement in tolerating unpleasant emotions affected the improvement of kleptomania symptoms, and the improvement in reward perception and tolerance of unpleasant emotions led to an improvement in both psychological stress responses and QOL.
As for the effect of the improvement in unpleasant emotional tolerance on the improvement of kleptomania symptoms, the results suggest that there was an increase in monitoring and control of the emotional arousal that triggered stealing behaviour. In terms of the influence of unpleasant emotional tolerance on the psychological stress response and QOL, the results suggest that the programme contributed to the development of the monitoring and control of emotional arousal that triggered problematic behaviour other than stealing behaviour. Regarding this, 50% of the participants had psychiatric disorders co-morbid with kleptomania, such as depression or eating disorders, and there were several comments about problematic behaviours other than stealing, such as over-eating, compulsive behaviour, and excessive shopping during the programme. This result aligns with previous research indicating a link between patients with kleptomania and other co-morbid psychiatric disorders (Sarasalo et al., Reference Sarasalo, Bergman and Toth1996).
With reference to the influence of reward perception on psychological stress response and QOL, the results suggest that the programme contributed to the expansive development of other behaviours, which are not necessarily an alternative to stealing behaviour, and an increase in positively reinforced behaviour in general life. It has been highlighted that people with kleptomania are increasingly likely to lose families and jobs and to encounter legal problems due to the illegality of stealing (Grant and Odlaug, Reference Grant and Odlaug2008). Therefore, people with kleptomania are often forced to rebuild their lives, and this is one of the reasons for an increase in the repertoire of new behaviours being encouraged.
Hence, it is assumed that an improvement in the monitoring and control of emotional arousal that triggers various problematic behaviours, including stealing, and an expansion of other behaviours to get closer to reinforcers in general life affected the improvement of kleptomania symptoms and QOL.
Furthermore, no interaction between kleptomania symptoms and psychological stress responses or QOL was found. Given that kleptomania has been reported to be a state in which it is very difficult to identify the reinforcer that maintains stealing behaviour due to the very high repetition of the behavior (Asami et al., Reference Asami, Nomura, Shimada, Ohishi and Ohishi2021; Sarasalo et al., Reference Sarasalo, Bergman and Toth1997), it is assumed that there is less interaction between stress and stealing behaviour and that in kleptomania, stealing behaviour is not only maintained by negative reinforcement.
Moreover, participants who had relapses during their participation in the programme were less educated and displayed more severe kleptomania symptoms than those who did not. This suggests that a lower level of education is associated with less cognitive control over stealing behaviour. Therefore, it may be useful for those who have less cognitive control over stealing behaviour to focus on environmental interventions such as environmental control and behavioural approaches.
This study has some limitations. First, although the CBGT programme showed several effects on kleptomania symptoms and QOL, it lacked a comparison with a control group; therefore, it is difficult to suggest that the results were sufficiently demonstrated. In addition, although a rolling format was used to prevent drop-out, 40% of the participants were excluded from the analysis due to drop-out or non-response to the questionnaire, and consequently the sample size was small. Therefore, the generalization of the effects of the programme in this study is limited. Consequently, the effectiveness of the programme should be further examined by increasing the number of participants, comparing the results with those of the control group, and examining the follow-up period after the completion of the programme. Moreover, to prevent drop-out and non-response, it would be useful to provide reward incentives for research participation.
Next, co-morbidity was not an exclusion criterion in this study, and 50% of the participants had co-morbid psychiatric disorders. Considering that the study included hospital patients, and that the number of co-morbidities was consistent with the findings of previous studies, the study has high ecological validity in terms of examining the effects of the programme in actual clinical situations. However, it is possible that the CBGT programme affected not only the kleptomania symptoms but also the co-morbidity symptoms. Therefore, it remains a possibility that improvement of co-morbidity symptoms may affect improvement of kleptomania symptoms. It is a limitation of the study in terms of typical effects on kleptomania symptoms. Although the participants of this study were individuals who had been undiagnosed with a personality disorder by doctor, a limitation of this study is that structured interviews about personality disorders were not conducted.
Furthermore, the K-SAS, a questionnaire discussing kleptomania symptoms in the last week, was administered at the beginning and end of the programme to measure changes in kleptomania symptoms after 12 sessions of CBGT combined with mindfulness. However, it is unclear how the kleptomania symptoms changed during the programme, and it is possible that unexpected changes occurred during the final week of the programme. Therefore, it is necessary to examine which variables change during the intervention and how they facilitate improvement in kleptomania symptoms.
Conclusion
This study aimed to examine the effectiveness of CBGT combined with mindfulness in the treatment of kleptomania. Although there is a limitation in the generalization of the results because only 59.46% of the participants were analysed due to drop-outs, the results suggested that kleptomania symptoms and QOL were improved. Furthermore, the recovery process revealed that an improvement in distress tolerance resulted in an improvement in kleptomania symptoms and that an improvement in reward perception and distress tolerance resulted in an improvement in the stress response and QOL. Therefore, CBGT combined with mindfulness may be an effective intervention for the treatment of kleptomania.
Key practice points
-
(1) This study examined the effectiveness of CBGT combined with mindfulness for treating kleptomania.
-
(2) A total of 22 participants with kleptomania completed the 12-session programme and completed a questionnaire at the time of their initial participation and at the end of the programme.
-
(3) CBT plus mindfulness techniques have been shown to be effective with kleptomania.
-
(4) The CBGT plus mindfulness programme improved QOL of people with kleptomania.
-
(5) The recovery process revealed that the improvement of distress tolerance affected the improvement of kleptomania symptoms.
Data availability statement
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
None.
Author contributions
Yuka Asami: Conceptualization (lead), Data curation (lead), Formal analysis (lead), Funding acquisition (lead), Investigation (lead), Methodology (lead), Project administration (lead), Resources (lead), Writing – original draft (lead), Writing – review & editing (lead); Kazutaka Nomura: Conceptualization (equal), Data curation (equal), Investigation (equal), Methodology (equal), Project administration (equal); Hironori Shimada: Conceptualization (equal), Investigation (equal), Methodology (equal), Project administration (equal); Keiko Nakagawa: Investigation (equal); Mayuka Sugano: Investigation (equal); Azusa Koshiba: Investigation (equal); Yasufumi Ohishi: Project administration (equal); Hiroyo Ohishi: Project administration (equal); Masayuki Ohishi: Project administration (equal).
Financial support
We gratefully acknowledge funding from JSPS KAKENHI (grant number JP21J14483).
Conflicts of interest
We have no conflicts of interest to disclose.
Ethical standards
This study was approved by the Ethics Review Committee on Research with Human Subjects of Waseda University (No. 2016–137) and was conducted in accordance with international ethics guidelines, including the Declaration of Helsinki.








Comments
No Comments have been published for this article.