Background
Autism is a lifelong neurodevelopmental condition consisting of difficulties in social communication, adapting to unexpected change, heightened sensory sensitivity and restricted interests.1 There are many barriers to obtaining an autism diagnosis, such as knowledge of autism, availability of diagnostic services and funding.Reference Lai and Baron-Cohen2 A population study in the UK screened the adult population, including individuals with previously unknown or undiagnosed autism, to establish the true prevalence of autism, and found that approximately 1.1% of UK general population adults meet criteria for an autism diagnosis.Reference Brugha, Spiers, Bankart, Cooper, McManus and Scott3 Those with elevated autistic traits can experience similar difficulties to autistic people, such as sensory hypersensitivity, and social communication and sensorimotor difficulties.Reference Hannant, Cassidy, Tavassoli and Mann4 Many adults who are high in autistic traits, and in particular women, are likely to go undiagnosed, even though they might meet criteria for an autism diagnosis owing to lack of appropriate services, validated diagnostic tools and a tendency to camouflage their autistic behaviours and characteristics to ‘fit in’ in social situations.Reference Lai and Baron-Cohen2 Previous research has confirmed an increased vulnerability to mental health problems in both autistic people and those with elevated autistic traits.Reference Cassidy, White, Maddox and Mazefsky5,Reference Griffiths, Allison, Kenny, Holt, Smith and Baron-Cohen6
Autistic people are at significantly higher risk of suicidal thoughts and behaviours compared with non-autistic people.Reference Cassidy, White, Maddox and Mazefsky5–Reference Pelton, Crawford, Robertson, Rodgers, Baron-Cohen and Cassidy8 Lifetime prevalence of suicidal ideation in autistic adults ranges between 19.7% and 66%, and suicide attempts between 1.8% and 36%,Reference Cassidy, White, Maddox and Mazefsky5 the highest prevalence estimates being in late-diagnosed adults.Reference Cassidy, Bradley, Robinson, Allison, McHugh and Baron-Cohen7 Self-reported autistic traits in those without autism diagnoses are also associated with increased risk of suicidal thoughts and behaviours.Reference Cassidy, White, Maddox and Mazefsky5,Reference Pelton, Crawford, Robertson, Rodgers, Baron-Cohen and Cassidy8
Research has found that autism and autistic traits are over-represented in groups at risk for suicide. A high proportion of patients with depression (11%)Reference Takara and Kondo9 and women with borderline personality disorder (15%)Reference Rydén, Rydén and Hetta10 meet diagnostic criteria for co-occurring autism. Suicide attempts were found to be highest in people with a co-occurring diagnosis, across both groups. A total of 45% of women with elevated autistic traits in the region of clinical concern for possible autism reported making a suicide plan, and 16% had attempted suicide.Reference South, Beck, Lundwall, Christensen, Cutrer and Gabrielsen11 A study found that 40.6% of those who attempted suicide scored above the cut-off for clinical concern for possible autism on the Autism Spectrum Quotient,Reference Baron-Cohen, Wheelwright, Skinner, Martin and Clubley12 even after removing those with a self-reported diagnosis or suspected autism from the analysis.Reference Richards, Kenny, Griffiths, Allison, Mosse and Holt13
Studies have shown significantly increased risk of dying by suicide in autistic people compared with the general population.Reference Hirvikoski, Mittendorfer-Rutz, Boman, Larsson, Lichtenstein and Bölte14,Reference Kirby, Bakian, Zhang, Bilder, Keeshin and Coon15 As discussed above, many autistic people remain undiagnosed, with increased risk of attempting suicide. However, no studies have yet explored potentially undiagnosed autism or attempted to quantify autistic traits in those who have died by suicide.
Autism and autistic traits are beginning to be considered for inclusion in contemporary suicide theories.Reference Cassidy, White, Maddox and Mazefsky5 For example, cognitive inflexibility may reduce ability to solve problems in stressful or challenging circumstances, and therefore impair the ability to see a way out, increasing the risk of experiencing entrapment, with suicide being perceived as the only possible escape route.Reference Cassidy, White, Maddox and Mazefsky5,Reference O'Connor and Kirtley16 Autistic people and those with elevated autistic traits report camouflaging their autistic behaviours in an attempt to ‘fit in’ in social sitations,Reference Hull, Mandy, Lai, Baron-Cohen, Allison and Smith17 leading to feelings of not being accepted for one's true self in society (termed ‘thwarted belongingness’), increasing their risk of suicidality.Reference Cassidy, Gould, Townsend, Pelton, Robertson and Rodgers18,Reference Mitchell, Sheppard and Cassidy19 Autistic people's increased vulnerability to adverse life events, such as bullying, abuse, exploitation, social exclusion and poverty, also increases their risk of suicidality.Reference Griffiths, Allison, Kenny, Holt, Smith and Baron-Cohen6 Autistic people (diagnosed and undiagnosed), are also more likely to experience perseverative suicidal thoughts, and impulsively attempt suicide without a plan during a crisis when means for self-harm were present, which could particularly increase their risk of death by suicide.Reference Cassidy, Bradley, Cogger-Ward, Shaw, Bowen and Glod20,Reference Cassidy, Bradley, Cogger-Ward and Rodgers21
Aims
Previous general population studies have used psychological autopsy methods to gather evidence of diagnoses, characteristics and risk markers in those who died by suicide. Information is gathered from a variety of sources, such as coroners’ inquest records, medical records and interviews with next of kin.Reference Conner, Beautrais, Brent, Conwell, Phillips and Schneider22,Reference Hawton, Appleby, Platt, Foster, Cooper and Malmberg23 The psychological autopsy method can be used to systematically gather evidence in support of previously unidentified diagnoses (such as autism), personality traits (such as autistic traits), and unique characteristics and risk markers for suicide in different groups (such as those with and without evidence of autism). This approach can therefore identify unique suicide prevention targets in different groups.Reference Conner, Beautrais, Brent, Conwell, Phillips and Schneider22 The current study is particularly novel as it utilises a large analysis of coroners’ inquest records, followed by psychological autopsy interviews with a subsample of next of kin of those who died. Through these two stages, we address the following research questions.
(a) What is the prevalence of autism and evidence for autistic traits in those who died by suicide in England?
(b) What are the characteristics and risk markers for suicide in those who died by suicide who had evidence of autism and/or elevated autistic traits compared with those who died by suicide who had no evidence of autism?
We predicted that autism, and elevated autistic traits (indicating possible undiagnosed autism), would be significantly over-represented in those who died by suicide compared with the prevalence expected in the general alive population.
Method
Design
Recruitment to the two stages of the study is shown in Fig. 1. In stage 1, coroners’ inquest records covering dates of death between 1 January 2014 and 31 December 2017 were requested from two regions of England.
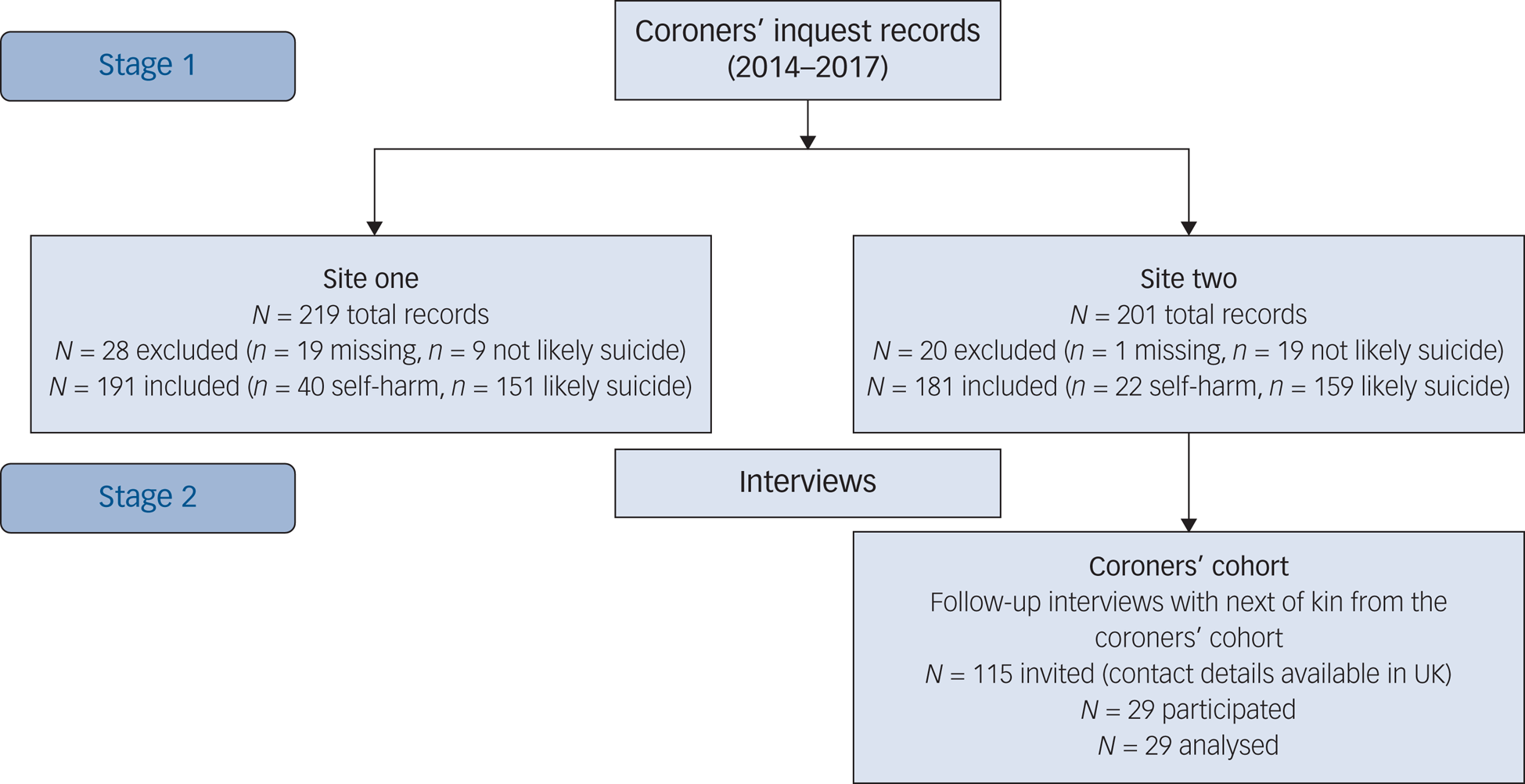
Fig. 1 Recruitment to stage 1 and stage 2 of the study.
Data were obtained from the Office of National Statistics 2011 census (https://www.ons.gov.uk/census/2011census) and 2016–2018 Public Health England Suicide Prevention Profile (https://www.gov.uk/government/statistics/suicide-prevention-profile-updates) for each site. Site 1: 77.4% employed, 97.5% White (2011 census), prevalence of suicide 8.4 per 100 000 (2016–2018); site 2: 81% employed, 90.3% White (2011 census), rate of suicide 8.8–12.2 (across different parts of the region) per 100 000 (2016–2018). In the rest of the UK: 75% employed, 85.4% White (2011 census), rate of suicide 9.6 per 100 000 (2016–2018).
We independently identified records where the person likely died by suicide and analysed these records for: (a) evidence of autism; and (b) characteristics of those who died. The data entry for stage 1 took place between October 2015 and July 2019. Data entry was undertaken by S.C., L.B., A.R., S.A.-Y. and G.R. In stage 2, interviews were conducted with next of kin recruited through the coroners’ offices included in stage 1 to gather evidence of autism for those who died.
The interviews for stage 2 took place between June 2018 and March 2019. Interviews were undertaken by S.C., A.R., S.A.-Y.and H.C.-W.
Ethical approval
Ethical approval was granted by the relevant local ethics committee at Coventry University (stage 1: P42264; stage 2: P60970). Our ethical approval stipulates that the sites included in this study are not published to protect the anonymity of those who died and their families.
Stage 1: analysis of coroners’ inquest records
Evidence of suicide
Coroners’ inquests covering dates of death between 1 January 2014 and 31 December 2017 returning a conclusion of suicide, narrative, open or other suspected suicide (for example drug and alcohol related, accident/misadventure) were requested from coroners’ offices in two regions of England.
In 2019, the standard of proof for a suicide conclusion in all coroners’ inquests changed from a criminal standard (beyond reasonable doubt) to a civil standard (balance of probabilities).Reference Appleby, Turnbull, Kapur, Gunnell and Hawton24 The coroners’ inquests analysed in the current study therefore used the criminal standard of proof to determine a conclusion of suicide. This criminal standard of proof in coroners’ inquests can underestimate the true rate of suicide,Reference Rockett, Kapusta and Coben25 and conclusions for people who likely died by suicide also vary considerably among coroners.Reference Palmer, Bennewith, Simkin, Cooper, Hawton and Kapur26 Hence, we independently reviewed all coroners’ inquests to determine whether the person likely died by suicide, as recommended by best practice guidelines for psychological autopsy studies.Reference Hawton, Appleby, Platt, Foster, Cooper and Malmberg23
Cause of death was coded as:
(a) self-harm, using the ICD-1027 definition of intentional self-harm where intent to end life is undetermined; or
(b) suicide, where there was evidence of intentional self-harm with intent to end life, such as leaving a note or message, communication of suicidal intent to others, previous suicide attempts, or the method and/or circumstances of the suicide that suggested suicidal intent (i.e. that the person who died could have reasonably have predicted that the method of self-harm would have likely resulted in their death).
A total of 372 coroners’ inquest records were included in the analysis (Fig. 1). Of these 98 (26.3%) were independently reviewed for evidence of self-harm/suicide by two members of the research team who were also responsible for inputting the data from the coroners’ records (S.C., L.B., G.R., A.R., S.A.-Y.). Of the 98 selected for independent review, 32 (32.7%) of the sample had evidence of possible autism, 58 (59.2%) had a suicide conclusion returned by the coroner and 40 (40.8%) had another conclusion returned where the intent was unclear (such as open, alcohol/drug related, misadventure).
There was agreement between the two raters for 86 (87.8%) of the records selected for independent review. Disagreements were resolved with discussion to reach consensus. Of the 372 records included in the analysis, the coroners’ returned a conclusion of suicide for 243 individuals (65.3%), and the research team agreed with the coroners’ conclusion of suicide in 100% of these records. Of the remaining 129 records where the coroners’ returned a conclusion indicating likely suicide (for example open, drug/alcohol related, misadventure), the research team coded 67 (51.9%) as death by likely suicide, and 62 (48.1%) as death by self-harm.
Out of the 372 records, the research team classified 62 (16.7%) as death by self-harm, and 310 (83.3%) as death by suicide (Table 1).
Table 1 Evidence of autism in cases of likely suicide and self-harm identified from the coroners’ inquest records

a. Evidence of autism, sum of ‘possible diagnosis’ + ‘strong evidence’ + ‘definite diagnosis’.
b. Denotes percentage calculated by row.
c. Denotes percentages calculated by column.
Evidence of autism
We devised a checklist to systematically gather evidence of autism from the coroners’ inquest records based on the main symptom domains in DSM-51 (see Appendix). A total of 95 (25.5%) of the coroners’ inquest records were independently rated for evidence of autism by two members of the research team who were also responsible for inputting the data from the coroners’ records (S.C., L.B., G.R., A.R., S.A.-Y.). All records identifying evidence of autism (possible/strong/definite) were checked by a second rater, alongside a random sample of records with no evidence of autism. There was agreement for 81 (85.3%) of records. Disagreements were resolved with discussion to reach consensus.
Risk markers
A data spreadsheet was developed, informed by previous research, to capture qualitative data pertaining to a broad range of characteristics of those who died (Table 2).Reference Conner, Beautrais, Brent, Conwell, Phillips and Schneider22,Reference Hawton, Appleby, Platt, Foster, Cooper and Malmberg23 Content analysis was conducted on these qualitative data to capture the full range of characteristics of each person who died. This method was used as it is more open to discovering new characteristics in the underexplored area of suicide in autism, rather than relying on a pre-existing theoretical framework. S.C. conducted the initial content analysis. A second researcher (H.C.-W.) independently conducted a content analysis on 80 (21.5%) of the coroners’ records to ensure that the extracted codes captured the full range of data. Two additional codes were identified by H.C.-W., which S.C. added to the full data-set. To ensure a sufficient sample size in analyses, these codes were collapsed into broader categories (see Table 2 for details of all codes included in the broader categories).
Table 2 Characteristics of those who died identified from the coroners’ inquest records
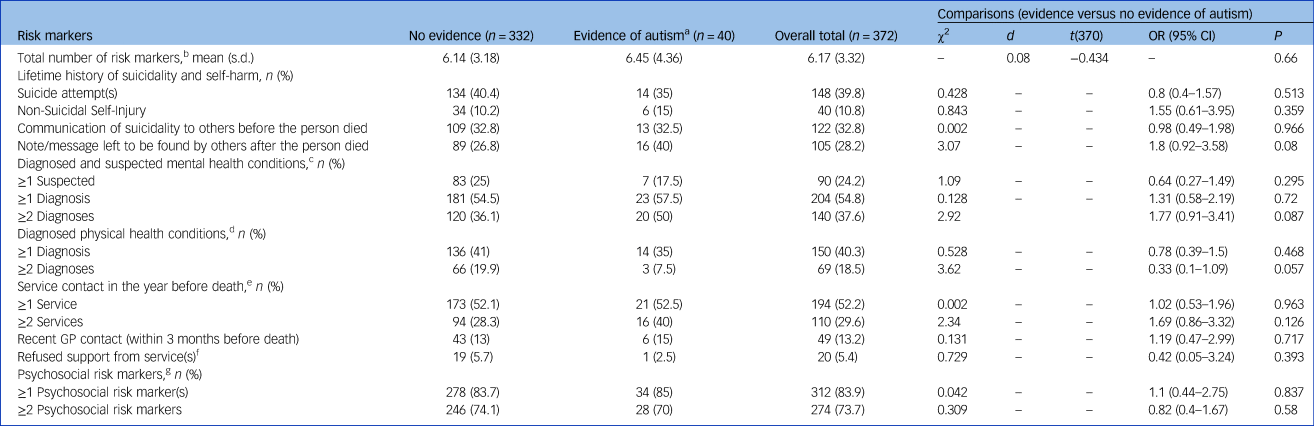
a. Evidence of autism: sum of ‘possible diagnosis’ + ‘strong evidence’ + ‘definite diagnosis’.
b. Risk markers: sum of suicidality and self-harming behaviours, diagnosed mental and physical health conditions, and psychosocial risk markers.
c. Diagnosed and suspected mental health conditions: depression, anxiety, personality disorder, bipolar disorder, psychosis, obsessive–compulsive disorder, post-traumatic stress disorder, social anxiety, eating disorder, attention deficit hyperactivity disorder, Tourette's syndrome.
d. Diagnosed physical health conditions, migraines, hypothyroidism, unexplained pain, drug/alcohol dependency, liver disease, anaemia, asthma, gout, hepatitis, heart condition, high blood pressure, stress, insomnia, skin condition, cancer, chronic obstructive pulmonary disease, diabetes, chronic back pain, kidney disease/failure, arthritis, irritable bowel syndrome, degenerative neurological condition, brain injury, epilepsy, stroke, eye problem, ear problem, genetic disorder, multiple sclerosis
e. Service contact in the year before death: occupational therapist, charity, social worker, home resolution team, oncologist, pain management, general practitioner (family doctor), community psychiatric nurse, hospital, drug/alcohol team, crisis team, Improving Access to Psychological Therapies team. Awaiting referral to a service, Awaiting treatment from a service, Awaiting assessment by a service/health practitioner.
f. Refused support from service(s): the person who died refused to engage with the service they were referred to.
g. Psychosocial risk markers: socially isolated, isolated from family, alcohol/drug abuse, gambling addiction, bereavement, trauma/abuse, unstable family life; exposure to others’ suicidal behaviour, lived alone, homeless, legal problems, not in employment or education, aggression/agitation, stress, deteriorating/poor general health, chronic pain, retired, financial problems, religious, carer for another person.
Analysis
Chi-square analyses compared: (a) the number of individuals with confirmed autism; and (b) total evidence of autism (possible, strong and definite) identified in the coroners’ inquest records, to the prevalence of autism expected in the general population. We used the most recent prevalence estimate of autism identified in the UK adult population (1.1%); this estimate included undiagnosed or unknown cases of individuals with autism, which is therefore similar to the approach taken for the current study.Reference Brugha, Spiers, Bankart, Cooper, McManus and Scott3
The frequency of mental and physical health problems, service contact and psychosocial risk markers recorded for those who died with any evidence of autism (possible, strong and definite) was compared with that of those who died with no evidence of autism. Odds ratios (ORs) were calculated as an estimate of effect size. To correct for multiple comparisons in the analysis, a Bonferroni-corrected alpha level of P < 0.0036 was used. Chi-square analyses were only performed on variables with expected cell counts of at least five, and Fisher's exact tests were used for cell counts between 4 and 4.9.
Stage 2: interviews with next of kin
Participants
Next of kin of those who died were invited to take part through the coroners’ office of site 2 for all inquests included in stage 1 (Fig. 1). Through the coroners’ office, out of the 181 records included in the stage 1 analysis, we were able to invite next of kin of 115 people who died, who were in the UK and for whom contact details were available.
To explore whether the characteristics of those who died were different depending on whether we were able to invite their next of kin to take part in stage 2 or not, we compared age, gender and evidence of autism between these two groups. There were no significant differences in gender (χ2 = 0.21, P = 0.65; OR = 1.19, 95% CI .56–2.51), or evidence of autism (χ2 = 0.94, P = 0.33; OR = 1.69, 95% CI 0.58–4.93). However, the people who died whose next of kin were invited to participate in stage 2 were significantly older at the time of their death (mean age 49.24 years, s.d. = 19.05) than the people who died whose next of kin we were not able to invite to take part in stage 2 (mean age 42.68, s.d. = 15.34) (t = 2.53(160), P = 0.018). In total, 29 (25%) next of kin took part in the interviews (mean age 57.86 years, s.d. = 13.62, 11 male, 18 female).
Measures
Evidence of autism
The checklist for evidence of autism developed for the analysis of the coroners’ inquest records in stage 1 was adapted for the stage 2 interviews (see Appendix).
Psychological autopsy interview
Signs of possible autism in the psychological autopsy interview were required in at least two areas (using the same criteria as in the analysis of coroners’ inquest records; Appendix). The interviewers (S.C., H.C.-W., S.A.-Y., A.R.) were all involved in data entry in stage 1 of the study. However, H.C.-W., S.A.-Y.and A.R. did not read the coroners inquests before the interviews. S.C. did participate in data entry of some coroners’ inquests prior to the interviews, with a gap of at least 6 months between reading the records and conducting the interviews. Two interviewers were present at each interview. Both interviewers discussed evidence for autism directly after the interview was completed. Agreement was required by both interviewers to code evidence of autism, otherwise a code of ‘no evidence’ was returned.
Social Responsiveness Scale
The Social Responsiveness Scale - second edition (SRS-2) is a 65-item proxy report rating scale of autistic traits.Reference Constantino and Gruber28 Each item is scored on a scale from 0 (never true) to 3 (always true), with higher scores indicating a greater number and severity of autistic traits. Scores at or above 60 suggest autistic traits in the range of clinical concern for possible autism.Reference Constantino and Gruber28 The SRS-2 wording was adapted to enable next of kin to report on the behaviour of the person within the 6-month period before they died.
Autism Diagnostic Interview
The Autism Diagnostic Interview – revised (ADI-R) is a widely used and validated tool for diagnosis of autism in children and adults.Reference Rutter, LeCouteur and Lord29 The ADI-R is a semi-structured interview with an informant who reports on the early developmental history and/or current behaviour of the person being assessed.Reference Rutter, LeCouteur and Lord29 The ADI-R was modified to enable next of kin to report on the early developmental history and/or more recent behaviour present within the 6-months prior to the person's death. ADI-R interviews were conducted by trained interviewers (S.C., S.A.-Y., A.R.), with 18% of the ADI-R interviews independently scored by two interviewers. Agreement was above the required 80% (83–93%).
Procedure
The coroners’ cohort comprised next of kin of those who died, each of whom received a postal invitation through the coroners’ office of site 2. Participants were invited to take part in an interview study aiming to understand why people take their own lives, to help prevent future deaths. Participants were informed that the study was exploring a range of characteristics of the person who died, including their demographics and medical information, social skills and early development. In order to minimise bias, the invitations to the coroners’ cohort did not mention autism or autistic traits.
Interviews took place either in participants’ homes, or on university premises, according to their preference. Prior to the interview, all participants discussed their invitation with a member of the research team either by phone or by email, to ensure they had appropriate support during and after the interview. Participants all completed the first interview, which included the psychological autopsy interview and SRS-2. If the person who died showed evidence of autism in the analysis of the coroners’ records, psychological autopsy interview or SRS-2, the next of kin were invited to complete the ADI-R in a follow-up interview.
Analysis
Point biserial correlations were calculated between the SRS-2 total scores, evidence of autism from the coroners’ inquest records, evidence of autism from the psychological autopsy interviews, and whether the person who died met the threshold for autism on the ADI-R. Chi-square analyses were used to compare the occurrence of total evidence of autism (possible/strong/definite) to the prevalence of autism expected in the general alive population.
Results
Stage 1: coroners’ inquest records
Descriptive statistics
Table 1 shows evidence of autism in those who died by self-harm or likely suicide from analysis of the coroners’ inquest records. There was no significant difference in total evidence of autism (possible/strong/definite) between those who likely died by suicide (11.9%) or by self-harm without clear evidence of intent (4.8%) (χ2 = 2.71, P = 0.1; OR = 2.67, 95% CI 0.79–8.94). There were no significant gender differences in the rate of death by self-harm (85.5% male) or likely suicide (78.4% male) (χ2 = 1.6, P = 0.21; OR = 1.62, 95% CI 0.76–3.46), or in those with (85% male) or without (78.9% male) any evidence of autism (χ2 = 0.813, P = 0.37; OR = 0.66, 95% CI 0.27–1.64).
A three-way ANOVA showed no significant differences in age according to gender (F(1, 363) = 1.2, P = 0.274, ηp 2 = 0.003), evidence of autism (F(1, 363) = 0.886, P = 0.347, ηp 2 = 0.002) or cause of death (F(1, 363) = 0.335, P = 0.56, ηp 2 = 0.001), and no significant interactions between the variables (all P > 0.33, ηp 2 < 0.003). Therefore, in subsequent analyses data were combined across cause of death (self-harm/suicide), gender (male/female) and age.
Evidence of autism
Chi-square analysis showed that the proportion of individuals with total evidence of autism (possible/strong/definite; 10.8%) was significantly higher in those who died by self-harm or suicide than the 1.1% prevalence expected in the UK general alive population (1.1% including people with previously unknown (i.e. undiagnosed) cases of autism)Reference Brugha, Spiers, Bankart, Cooper, McManus and Scott3 (χ2 = 31.31, P < 0.001; OR = 11.08, 95% CI 3.92–31.31). In contrast, the proportion of individuals who died with a diagnosis of autism recorded (0.5%) was not significantly different to the expected prevalence of autism in the UK general alive population (1.1%) (χ2 = 0.672, P = 0.41; OR = 0.5, 95% CI 0.9–2.73).
Risk markers
Table 2 shows results of the content analysis, comparing the characteristics and risk markers stratified by evidence of autism. There were no significant differences between those with evidence of autism (possible/strong/definite) and those without evidence of autism in regard to suicide method (χ2 = 10.32, P = 0.24; ϕ = 0.17). There were no significant differences in the rate of suicidality and self-harming behaviour, mental or physical health conditions or service contact, or psychosocial risk markers between the two groups.
Stage 2: interviews with next of kin
Evidence of autism
In total 5 (17.2%) of the follow-up sample had possible/strong evidence of autism identified from the coroners’ records in stage 1 of the study (but none had a definite diagnosis of autism recorded). The psychological autopsy interview/SRS-2 identified evidence of ‘possible autism’ in an additional 7 (24.1%), giving a total of 12 (41.4%) individuals. However, ‘strong evidence of autism’ was not confirmed, as none of the 12 met the threshold for autism on the ADI-R.
Chi-square analysis showed that the number of individuals with possible autism in the coroners’ cohort (n = 12, 41.4%) was significantly higher than expected in the general alive population (1.1%) (χ2 = 12, P < 0.001; OR = 19.76, 95% CI 2.36–165.84).
Reliability
SRS-2 scores were not significantly correlated with evidence of autism from the psychological autopsy interview using point biserial correlation (n = 29; r pb = 0.259, P = 0.176), or with evidence of autism identified from the coroners’ inquest records using spearman's correlation (n = 29; r s = 0.06, P = 0.754).
Discussion
Main findings
As far as we know, this is the first study to examine evidence of autism and autistic traits in those who died by suicide in England. Through analysis of 372 coroners’ inquest records in two regions of England, there was evidence of autism and elevated autistic traits in 10.7% of those who died by suicide – 11 times higher than prevalence of autism in the UK general population similarly including previously unknown diagnoses of autism (1.1%).Reference Brugha, Spiers, Bankart, Cooper, McManus and Scott3 Given that coroners’ records do not systematically gather evidence of autism and autistic traits, this is likely an underestimate of the true rate.
Consistent with this, subsequent interviews with a subsample of the next of kin of those who died showed evidence of elevated autistic traits indicating possible autism in 41.4% of the sample. However, none of the follow-up sample showed strong evidence of undiagnosed autism using a validated diagnostic instrument (ADI-R). This high rate (41.4%) of possible autism identified in the current study is consistent with previous research in which 40.6% of those who attempted suicide (without autism or suspected autism diagnosis) scored above the cut-off for clinical concern for possible autism on the Autism Spectrum Quotient; when including people with autism and those with suspected autism, 53.9% scored above the cut-off.Reference Richards, Kenny, Griffiths, Allison, Mosse and Holt13 Results suggest that autistic traits in the range of clinical concern for possible autism (regardless of confirmed diagnosis) are also significantly over-represented in those who die by suicide.
Analysis of the coroners’ records showed a similarly high number of risk markers in those who died with evidence of autism compared with those who died without evidence of autism. There was also a broadly similar pattern of risk markers between these groups across both stages of the study. Therefore, the current research emphasises common collective concerns for the prevention of suicide, regardless of evidence of autism. Suicide method did not significantly differ between the groups, contrary to previous research suggesting that people with autism may use more lethal forms of attempting suicide.Reference Kato, Mikami, Akama, Yamada, Maehara and Kimoto30
The most commonly shared characteristics of those who died included previous self-harm and/or suicide attempt, at least one diagnosed or undiagnosed physical or mental health problem, poor current engagement with services and psychosocial risk markers (for example financial difficulties, recent unemployment, bullying and abuse, bereavement, relationship breakdown, living alone and/or recent changes to living situation, exposure to others’ suicidal behaviour and social isolation).
Those who died did not typically experience one risk marker in isolation, but a number of different risk markers (on average n = 6 identified from the coroners’ records). This is consistent with previous suicide research and theory showing that the accumulation of background risk factors (personal and historical events) in the context of current stressors increases risk of attempting suicide.Reference O'Connor and Kirtley16 There was limited evidence of different or unique risk markers for suicide in those with evidence of autism or elevated autistic traits.
Strengths and limitations
The current study has a number of strengths and limitations. Limitations include the relatively small subsample of next of kin and those with evidence of autism identified in the study. A large number of comparisons were carried out, and, although a conservative alpha level was used in the study, many comparisons were underpowered. Although all proxy report measures used here demonstrate evidence of validity, undiagnosed conditions cannot be confirmed, as it was not possible to assess the person who died directly. The team who conducted the interviews with next of kin were also involved with data entry from the coroners’ records, which could have led to some bias. However, this was minimised by three interviewers only inputting data from the coroners’ records after the interviews, and one interviewer having a gap of at least 6 months between inputting data from the coroners’ records and conducting the interviews.
Although analysis of the coroners’ records covered two regions of England, next of kin were only invited from one of the coroner's offices covering one region of England, limiting the generalisability of results. The characteristics of those who died included in stage 2 interviews with their next of kin, also tended to be slightly older than those who died where we were not able to contact next of kin to participate in the second stage of the study. A majority of next of kin who took part in the interviews were female, which could also limit the generalisability of the results from the follow-up interviews.
Reliability analysis showed that scores on a validated autism screening tool (SRS-2) did not significantly correlate with evidence of autism identified from the coroners’ records. Strong evidence of possible undiagnosed autism identified from the coroners’ records was also not confirmed using a validated autism diagnostic tool (ADI-R). The interviews with next of kin identified evidence of autism or elevated autistic traits in an additional seven people who died. This suggests that gathering evidence of autism from the coroners’ records alone is not valid, and it is important to interview next of kin to identify further evidence of autism and autistic traits.
Strengths of the study include that a range of sources of evidence for autism and autistic traits were systematically gathered, including validated autism screening (SRS-2) and an autism diagnostic tool (ADI-R). Interrater reliability was used extensively to ensure high validity and consistency of data classification and coding.
Implications
There are clear implications for suicide prevention. First, as elevated autistic traits and possible undiagnosed autism are over-represented in those who attempt and die by suicide, it is crucial for clinicians to screen for autistic traits and possible undiagnosed autism in patients presenting with suicidal thoughts and behaviours, and to offer appropriate tailored support.Reference Camm-Crosbie, Bradley, Shaw, Baron-Cohen and Cassidy31 A quick (10-item) and validated screening instrument for autistic traits is the Autism Spectrum Quotient-10,Reference Allison, Auyeung and Baron-Cohen32 although the full Autism Spectrum Quotient does not take much longer to complete (50 items) and would provide more detail.Reference Baron-Cohen, Wheelwright, Skinner, Martin and Clubley12 Scoring above cut-off on either version should support a referral for an autism assessment.
Second, although 32% of the sample communicated their suicidal thoughts to another person before they died, some families reported how the death of their loved one ‘came out of the blue’ with no obvious warning signs. This suggests that some people do not present with clear warning signs or risk markers for suicide, but nevertheless may be at significant risk of suicide. It is therefore important to ask whether a person is feeling suicidal, and to believe the person if they disclose feeling suicidal.Reference Cassidy, Goodwin, Robertson and Rodgers33 Clinicians should also regularly check up on patients, as risk can change dramatically in a short period of time.
Third, given that the current study suggests that evidence of autism is typically not included in coroners’ inquests in England, it is crucial for coroners to begin to systematically gather evidence of autism and autistic traits in inquests. This will enable more accurate nationwide estimates of autism and autistic traits in those who die by suicide in the UK to be determined, and may facilitate identification of potentially unique suicide prevention targets identified in this group. This could be achieved by asking general practitioners to confirm whether the person who died had an autism diagnosis or suspected autism, and/or by asking next of kin to complete a brief checklist to identify autistic traits in the person who died.
Finally, in terms of suicide prevention programmes, it is important that these are tailored to autistic people. The top autism community priority for suicide prevention is removing barriers to support and treatment,Reference Cassidy, Goodwin, Robertson and Rodgers33 given that autistic people report being excluded from services, and receiving inappropriate support and treatment for mental health problems and suicidality.Reference Camm-Crosbie, Bradley, Shaw, Baron-Cohen and Cassidy31,Reference Cassidy, Goodwin, Robertson and Rodgers33 Our results also suggest that suicide prevention programmes need to tackle wider societal issues, such as social exclusion and isolation, poverty, unemployment, trauma and abuse.Reference Griffiths, Allison, Kenny, Holt, Smith and Baron-Cohen6,Reference Pelton, Crawford, Robertson, Rodgers, Baron-Cohen and Cassidy8,Reference Mitchell, Sheppard and Cassidy19 All of these are significantly more common experiences among autistic people compared with non-autistic people, and increase their risk of attempting suicide.Reference Cassidy, White, Maddox and Mazefsky5
Suicide prevention programmes could also help the person understand how an exclusive focus on one's own point of view might lead a person to make incorrect assumptions about other people's thoughts and feelings (for example believing incorrectly that ‘no one cares about me, the world would be better off without me, and my death would not affect anyone else’), leading them to consider suicide. Programmes could also explain and demonstrate that with the right support (peer support, support from social care services, and supported employment and befriending schemes), quality of life can be improved and social isolation can be reduced.
In conclusion, our results suggest that autism and autistic traits are over-represented in those who died by suicide in England; 41.4% of those who died had evidence of elevated autistic traits. This is consistent with a growing body of research showing that autistic people, and those with elevated autistic traits, are at increased risk of contemplating, attempting and dying by suicide.Reference Cassidy, White, Maddox and Mazefsky5 It is imperative for clinical services to address barriers to treatment and support that are experienced by autistic people, and to develop programmes with and for autistic people to reduce their high risk of suicide.Reference Cassidy, Goodwin, Robertson and Rodgers33
Data availability
The data that support the findings of this study are available from the corresponding author (S.C.), on reasonable request. The data are not publicly available owing to their containing information that could compromise the privacy of research participants.
Acknowledgements
We sincerely thank the families and friends of those who died who took part in this study to help us to understand and prevent suicide, and all the staff in the coroners’ offices who supported this research project. We are also extremely grateful to those with lived experience and expertise who provided feedback on the interview schedules and participant recruitment materials for the current study. We additionally thank Professor Clare Wood, Professor Erica Bowen, Susan Goodlad, Dr Rebecca Shaw, Dr Rosie Holt and Dr Sarah Griffiths, for valuable discussions, and Claire Pillinger, Dr Penelope Hannant, Kathy Cook, Gurkaran Dhanda, Becky Cooke and Sam Waldron for their assistance with data entry in stage 1 of the study.
Author's contributions
S.C., S.B.-C. and C.A. conceived of the study. All authors contributed to the study design. S.C., G.R., L.B., H.C.-W., S.A.-Y., A.R. all contributed to data collection. S.C. and H.C.-W. contributed to data analysis. All authors contributed to data interpretation. S.C. wrote the first draft of the manuscript. All authors provided critical feedback on the draft manuscript, and read and approved the manuscript before submission for publication.
Funding
This research was supported by Autistica [grant number: 7247], the Economic and Social Research Council Future Research Leaders grant [grant number: ES/N000501/2], Coventry University, and the University of Nottingham (received by S.C.). S.B.C. received funding from the Wellcome Trust 214322\Z\18\Z. For the purpose of Open Access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission. In addition, S.B.-C. received funding from Innovative Medicines Initiative 2 Joint Undertaking (JU) under grant agreement No 777394. The JU receives support from the European Union's Horizon 2020 research and innovation programme and EFPIA and AUTISM SPEAKS, Autistica, SFARI. S.B.-C. also received funding from the Autism Research Trust, SFARI, the Templeton World Charitable Fund, SFARI and the NIHR Cambridge Biomedical Research Centre. The research was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care East of England at Cambridgeshire and Peterborough NHS Foundation Trust. The views expressed are those of the author(s) and not necessarily those of the NHS, NIHR or Department of Health and Social Care. The funding sources were not involved in any aspect of the study design, recruitment, data collection, analysis, interpretation of results, writing of the manuscript, or the decision to submit for publication. The corresponding author has full access to all data used in the study and had final responsibility for the decision to submit for publication.
Declaration of interest
The authors disclose no conflicts of interest.
Appendix
Checklist for gathering evidence of autism from the coroners’ inquest records/psychological autopsy interview, and stage 2 interviews






eLetters
No eLetters have been published for this article.