Introduction
Cystic echinococcosis (CE) is a cosmopolitan often under-reported neglected disease of economic and public health significance (McManus et al., Reference McManus, Zhang, Li and Bartley2003; Nakao et al., Reference Nakao, McManus, Schantz, Craig and Ito2007; Battelli, Reference Battelli2009; Da Silva, Reference Da Silva2010). Although humans are affected as accidental hosts, CE affects both wild and domestic animals. It is caused by the metacestodes of parasitic tapeworms belonging to the family Taeniidae and genus Echinococcus (Spickler, Reference Spickler2020). Extensive research has shown transmission to livestock (intermediate hosts) and humans (accidental hosts) is through the consumption of Echinococcus spp. eggs, from fecal matter of infected, unrestricted, freely roaming and in most cases un-wormed domestic and wild canids (definitive hosts), present in contaminated pastures, water, vegetables and fresh fruits (Torgerson and Budke, Reference Torgerson and Budke2003; Eckert and Deplazes, Reference Eckert and Deplazes2004). Canids harbour mature adult worms in their intestines, producing eggs that, once ingested by the intermediate hosts, hatch into larvae, enter the circulation and slowly develop into fluid-filled structures lodged as cysts in various host organs, mainly in lungs and liver, thus compromising their functions (Eckert and Deplazes, Reference Eckert and Deplazes2004).
Hydatidosis is mainly caused by Echinococcus granulosus sensu lato complex comprising the following strains: E. granulosus sensu stricto (G1, G2 and G3), Echinococcus canadensis incorporating G6-camel strain, pig strain (G7), G9 up to G8 and G10 (the cervid strains), Echinococcus equinus (G4), Echinococcus ortleppi (G5) and Echinococcus felidis – the lion strain (Hüttner et al., Reference Hüttner, Nakao, Wassermann, Siefert, Boomker, Dinkel, Sako, Mackenstedt, Romig and Ito2008; Alvarez Rojas et al., Reference Alvarez Rojas, Romig and Lightowlers2014; Romig et al., Reference Romig, Ebi and Wassermann2015; Shariatzadeh et al., Reference Shariatzadeh, Spotin, Gholami, Fallah, Hazratian, Mahami-Oskouei, Montazeri, Moslemzadeh and Shahbazi2015; Thompson, Reference Thompson2017).
CE causes considerable losses of productivity in livestock measured in terms of weight loss, lowered meat quality and birth rates, coupled with economic losses as a consequence of organ condemnations during post-mortem (PM) meat inspections (Craig et al., Reference Craig, Budke, Schantz, Li, Qiu, Yang and Zeyhle2007; Cardona and Carmena, Reference Cardona and Carmena2013). Studies in ruminants in Iran revealed total liver and lung condemnations of 36.08 and 48.04% respectively, estimated at US$ 459 659.6 (Ahmadi and Meshkehkar, Reference Ahmadi and Meshkehkar2011); and in Turkey, US$ 89.2 million (72.2–107.9) (Sariözkan and Yalçin, Reference Sariözkan and Yalçin2009); in Australia, ranged from AU$ 36 683 in 2016 to AU$ 163 006 in 2014 in beef cattle (Wilson et al., Reference Wilson, Jenkins, Victoria, Tamsin and Budke2020); in Ethiopia, in bovines: 410 755.90 Ethiopian Birr (ETB; 30 202.64 US$; 1 US$ = 13.60 ETB) (Bekele and Butako, Reference Bekele and Butako2011); 25 608 ETB (Kebede et al., Reference Kebede, Hagos, Girma and Lobago2009b) and 1 691 266 200 ETB (101 203 734 US$) (Fromsa and Jobre, Reference Fromsa and Jobre2012). In recent years, there has been an increasing interest in CE research worldwide.
Echinococcus granulosus is known to occur in over 100 countries globally (Otero-Abad and Torgerson, Reference Otero-Abad and Torgerson2013; Deplazes et al., Reference Deplazes, Rinaldi, Alvarez Rojas, Torgerson, Harandi, Romig, Antolova, Schurer, Lahmar, Cringoli, Magambo, Thompson and Jenkins2017); a high prevalence was recorded in the Mediterranean countries (Bosco et al., Reference Bosco, Alves, Cociancic, Amadesi, Pepe, Morgoglione, Maurelli, Ferrer-Miranda, Santoro, Ramos, Rinaldi and Cringoli2021), Pakistan (Khan et al., Reference Khan, Naz, Ahmed, Simsek, Afzal, Haider, Ahmad, Farrakh, Weiping and Yayi2018), Turkey (Sariözkan and Yalçin, Reference Sariözkan and Yalçin2009), Saudi Arabia (Almalki et al., Reference Almalki, Al-Quarishy and Abdel-Baki2017), Australia (Lightowlers et al., Reference Lightowlers, Gasser, Hemphill, Romig, Tamarozzi, Deplazes, Torgerson, Garcia and Kern2021), China (Nakao et al., Reference Nakao, Li, Han, Ma, Xiao, Qiu, Wang, Yanagida, Mamuti, Wen, Moro, Giraudoux, Craig and Ito2010; Fu et al., Reference Fu M H, Wang, Han, Guan, Bergquist and Wua2021) and South America (Larrieu et al., Reference Larrieu, Costa, Cantoni, Alvarez, Cavagion, Labanchi, Bigatti, Araya, Herrero, Alvarez, Mancini and Cabrera2001).
In Africa, it has been found to be highly prevalent among domestic and wild animals (Ohiolei et al., Reference Ohiolei, Li, Ebhodaghe, Yan, Isaac, Bo, Fu and Jia2020). So far, limited studies in Uganda have revealed a CE prevalence of 1.84% in humans (Othieno et al., Reference Othieno2016); 12.2 and 66.4% in dogs (Inangolet et al., Reference Inangolet, Biffa, Opuda-Asibo, Oloya and Skjerve2010; Oba et al., Reference Oba, Ejobi, Omadang, Chamai, Okwi, Othieno, Inangolet and Ocaido2016), identification of E. granulosus sensu stricto G1 sheep strain and E. canadensis G6/7 camel strain in livestock in Karamoja (Chamai et al., Reference Chamai, Omadang, Erume, Ocaido, Oba, Othieno, Bonaventure and Kitibwa2016). Also E. felidis was found in lions and warthogs (Hüttner et al., Reference Hüttner, Nakao, Wassermann, Siefert, Boomker, Dinkel, Sako, Mackenstedt, Romig and Ito2008). Hence in Uganda, at least 4 strains of E. granulosus sensu lato complex do occur. Also, earlier studies had been conducted on peoples’ attitudes and practices towards CE persistence in livestock among pastoral and agro-pastoral areas in Uganda (Oba et al., Reference Oba, Ejobi, Omadang, Chamai, Okwi, Othieno, Inangolet and Ocaido2016; Omadang et al., Reference Omadang, Chamai, Othieno, Okwi, Inangolet, Ejobi, Oba and Ocaido2018). Furthermore, such studies had been conducted in Kenya (Njoroge et al., Reference Njoroge, Mbithi, Gathuma, Wachira, Gathura, Magambo and Zeyhle2002; Addy et al., Reference Addy, Alakonya, Wamae, Magambo, Mbae, Mulinge, Zeyhle, Wassermann, Kern and Romig2012; Kagendo et al., Reference Kagendo, Magambo, Agola, Njenga, Zeyhle, Mulinge, Gitonga, Mbae, Muchiri, Wassermann, Kern and Romig2014; Mbaya et al., Reference Mbaya, Magambo, Njenga, Zeyhle, Mbae, Mulinge, Wassermann, Kern and Romig2014; Odongo et al., Reference Odongo, Tiampati, Mulinge, Mbae, Bishop, Zeyhle, Magambo, Wasserman, Kern and Romig2018; Nungari et al., Reference Nungari, Mbae, Gikunju, Mulinge, Kaburu, Zeyhle and Magambo2019), Ethiopia (Sissay et al., Reference Sissay, Uggla and Waller2008; Kebede et al., Reference Kebede, Gebre-Egziabher, Tilahun and Wossene2011; Terefe et al., Reference Terefe, Kebede, Beyene and Wondimu2012; Kumsa and Mohammedzein, Reference Kumsa and Mohammedzein2014; Tigre et al., Reference Tigre, Deresa, Haile, Gabriël, Victor, Pelt, Devleesschauwer, Vercruysse and Dorny2016; Serda and Jago, Reference Serda and Jago2017), Sudan (Omer et al., Reference Omer, Dinkel, Romig, Mackenstedt, Elnahas, Aradaib, Ahmedd, Elmalik and Adam2010) and Tanzania (Ernest et al., Reference Ernest, Nonga, Kassuku and Kazwala2009; Miran et al., Reference Miran, Kasuku and Swai2017).
However, much less is known about prevalence of CE in livestock in Uganda. To address this gap, this study was undertaken to establish the prevalence of CE among slaughtered livestock in pastoral and agro-pastoral areas in Uganda. These studies are important in informing policy about the urgency needed to control CE among these rural livestock-keeping communities in Uganda.
Materials and methods
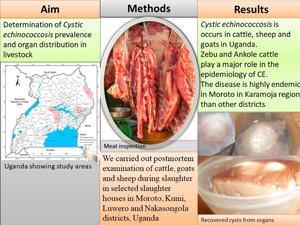
The study was carried out from March 2019 to February 2020 in selected designated slaughter abattoirs in the districts of Moroto in Karamoja region, Kumi in Teso region and Luwero and Nakasongola in Buganda region, Uganda (see Fig. 1). Moroto district was selected to represent pastoral areas (keeping livestock) in Karamoja region, Kumi to represent agro-pastoral (practice of both livestock keeping and crop agriculture) areas in eastern Uganda and Luwero and Nakasongola districts to represent agro-pastoral areas in central Uganda

Figure 1. Map of Uganda showing study areas.
A stratified random sampling procedure was used during this study. A total of 14 937 livestock were inspected. Details are shown in Table 1.
Table 1. Number of livestock examined in different districts

PM examination was undertaken on slaughtered cattle, sheep and goats. Most livestock brought for slaughter were local indigenous breeds from the neighbouring local livestock markets. Animals for PM inspection were randomly selected before entry to the slaughter facility. Selected animals were marked with paint for easy traceability. For each selected animal, information on species, breed, sex and origin/market purchased from, date and age were recorded. The animals were grouped based on teeth eruption (Torell et al., Reference Torell, Bruce and Kvasnicka2003; Eubanks, Reference Eubanks2012; Whiting et al., Reference Whiting, Brown, Browne, Hadley and Knowles2013) as ‘young’ when aged below 3 years and as ‘adults’ when aged above 3 years.
During PM inspection, each organ was visually assessed, palpated and incised to detect embedded hydatid cysts (Soulsby, Reference Soulsby1982). Recovered cysts were collected in air-tight labelled containers. The nature of the examinations performed would also detect other tapeworm parasites and these would also be recorded. For each positive organ, all recovered cysts were counted. Cyst diameters were measured to determine their sizes: ‘small’ when measuring below 4 cm, ‘medium’ measuring 4–8 cm and ‘large’ measuring beyond 8 cm, as described by Kebede et al. (Reference Kebede, Mitiku and Tilahun2009a). Recovered cysts were further characterized to determine their fertility and sterility status using standard protocols developed by Soulsby (Reference Soulsby1982). The cyst wall was carefully separated from host tissues, incised with a sterile scalpel blade and the contents were poured into a clean Petri dish and examined under a microscope under ×40 magnification. The presence of protoscolices seen as white dots on the germinal epithelium were categorized as ‘fertile’ while those without as ‘infertile’. Cyst infertility was further classified as ‘sterile’ when having turbid contents, as ‘calcified’ when it was gritty when cut and as ‘degenerated’ when it had pus.
The nature of the examination performed would also detect other tapeworm parasites notably Cysticercus tenuicollis cysts and these would also be recorded. This is because Taenia hydatigena, a tapeworm responsible for C. tenuicollis infection in sheep and goats shares a strong association with Cysticercus and Echinococcus in terms of the definitive hosts (dog) and intermediate hosts (herbivores) and therefore have the same risk factors and infection levels (Eckert et al., Reference Eckert, Gemmell and Matyas1984; Murell, Reference Murell2005).
Data analysis
Data were entered into an MS Excel 16.0 spreadsheet. Statistical analysis was performed using R Statistical software program (R Core Team, 2022). Chi-squared tests and odds ratios (ORs) at 95% confidence interval (CI) were used to examine differences in CE prevalence by livestock species, age, sex, districts and organs affected. Values of P < 0.05 were considered statistically significant.
Results
The overall prevalence of CE in livestock by sex and age showed that infection in males (6.2%) was higher than those in females (2.3%), and ‘older’ animals >3 years were also more infected (8.2%) than ‘young’ animals (0.3%) as shown in Table 2. The prevalence of CE among livestock species by district is shown in Table 3. A very highly significant CE prevalence of 29.1% was found in goats in Moroto (χ 2 = 4473.7, P < 0.001) than in Kumi (0.6%), Luwero (0.6%) and Nakasongola (0.2%); similar trends were also observed in sheep (28%) in Moroto district (χ 2 = 981.4, P < 0.001), Kumi district (2.1%) and none (0%) in both Luwero and Nakasongola districts; and in zebu cattle (31.3%; χ 2 = 631.3, P < 0.001) in Moroto, Kumi (1.8%) and Luwero districts (1.6%) and none in Nakasongola district. CE prevalence was significantly higher (P < 0.05, χ 2 = 4.04) in Ankole cattle (2.8%) in Nakasongola district than in Luwero (1.8%) and none (0%) in both Kumi and Moroto districts. No exotic cattle examined only in Luwero district was found with CE cysts. No sheep were slaughtered in Luwero and Nakasongola districts. Similarly, no Ankole cattle were slaughtered in Moroto and Kumi districts.
Table 2. Overall prevalence in all regions by sex and age

Table 3. Percentage CE prevalence with 95% CIs among livestock species by district

Regarding percentages of CE prevalence by organ infected among livestock species per district, in Moroto, the lungs of 27.7% of goat, 24% of sheep and 20.3% of zebu cattle had cysts significantly higher than that of goats (0.6%), sheep (2.1%) and zebu cattle (0.8%) in Kumi; in Luwero district, lungs of 0.9% of zebu cattle, 1.1% of Ankole cattle and 0.5% of goats and, in Nakasongola district, 1.6% of lungs of Ankole cattle and 0.2% of goats. Cyst infection in the livers was not reported in goats, sheep and zebu cattle in Nakasongola district. In Moroto district, the livers of zebu cattle (12.8%), sheep (5.3%) and goats (3.6%) were more infected than those of the same animals in Kumi and Luwero districts, and none in goats, sheep and zebu cattle in Nakasongola district and in sheep in Luwero district. Ankole cattle had almost similar prevalence in lungs in Luwero (1.1%) and Nakasongola (1.6%) compared to 0.8 and 1.6% in the liver respectively, and no cysts were recovered from Ankole cattle in Kumi and Moroto districts as shown in Table 4.
Table 4. Percentage organ CE prevalence (number positive in brackets) by species across all districts

Lung prevalence in goats was 100% in Nakasongola district, 88.9% in Kumi, 88.3% in Moroto and 70.6% in Luwero; in sheep was 100% in Kumi and 81.6% in Moroto; in zebu cattle was 50% in Luwero, 44.1% in Kumi and 61.1% in Moroto; only in Nakasongola 55.2% of the lungs of Ankole cattle were affected.
In the liver: in zebu cattle, 55.9% in Kumi and 38.7% in Moroto were infected, 39.7% and 50% in Ankole cattle in Luwero and Nakasongola districts were affected; and in goats, 29.4% in Luwero, 11.4% in Moroto and 11.1% in Kumi districts were affected. Details are shown in Table 5. Among cyst sizes, small cysts (72.1%) formed the bulk of infection in the lungs than in the liver (53.3%); mixed organ infections had more medium-sized infection (44.4%) than the liver (23.3%) and lungs (18.6%); the large cysts formed in the liver (23.3%) and (9.2%) in the lungs, as shown in Table 6. The number of cysts recovered per CE-infected organ is shown in Table 7. The lungs harboured the highest number of single and multiple cysts (890) compared to the liver (296). The mean cyst counts was 1.4 ± 0.03 per CE-infected liver, 1.4 ± 0.9 per infected lung, 3.2 ± 0.23 per mixed lung and liver infection and 5 per mixed lung, liver and spleen infection.
Table 5. Percentage composition of certain organs being CE-infected compared to other CE-infected organs per livestock species per district

Table 6. Percentage of organs of livestock examined with small-, medium- and large-sized cysts

Table 7. Percentage number of cysts recovered per CE-infected organ recovered

Percentage composition of status of CE cysts recovered from different organs per livestock species examined is shown in Table 8. Ankole cattle (33.4%), zebu cattle (6.4%) and sheep (1.7%) had fertile cysts in the liver while only goats had fertile cysts in the lungs (4.5%).
Table 8. Percentage composition of status of CE cysts recovered from different organs per livestock examined

Moreover, we were not interested in other parasites in this study, the proximity and similarity of this tapeworm (C. tenuicollis) cysts made them obvious as present within the protocol/procedure followed for examination. The prevalence of C. tenuicollis cysts therefore was found to be high in both goats and sheep. Details are as shown in Table 9.
Table 9. Percentage prevalence (number positive in brackets) of Cysiticercus tenuicollis in goats and sheep per district

Discussion
The communities in the study areas were pastoralists in Moroto district in Karamoja region; agro-pastoralists in Kumi district in Teso region and Luwero and Nakasongola districts in Buganda region. The overall CE prevalence among livestock examined was found to be 21.9% in sheep, 15.2% in zebu cattle, 5.5% in goats and 2.1% in Ankole cattle. Moroto district was found to have higher prevalence of CE than other districts; cattle had CE prevalence of 31.3%, sheep 28% and goats 29.1%. This could be attributed to differences in life styles affecting the level of dog–livestock interactions, sources and level of water availability. This may be because livestock keepers in Moroto were practicing transhumance thus seasonally move during periods of severe water shortages (dry season) to areas with water and pasture. This led to high concentration of livestock with the accompanying dog population, kept for security purposes, increasing the potential of transmission of CE between livestock, humans and dogs. In such a situation, dogs’ fecal matter easily contaminates water sources with E. granulosus eggs. However in agro-pastoral areas (practicing both crop and livestock farming) in Teso, livestock farmers lived a sedentary life style – access to clean water was relatively better, water sources were often bore holes and protected wells where dog access was limited or completely denied. In agro-pastoral areas in Nakasongola and Luwero farmers’ practiced agro-pastoralism – sources of water were open unprotected pools, dams, springs, lakes, rivers and swamps. These water sources were being shared among humans, livestock and dogs. In these areas, there is loose association of dogs with livestock keepers because dogs are mostly owned by communities for hunting (Oba et al., Reference Oba, Ejobi, Omadang, Chamai, Okwi, Othieno, Inangolet and Ocaido2016).
CE prevalence found in cattle in Moroto was similar to that reported in Maasailand in Kenya (25.5%) by Addy et al. (Reference Addy, Alakonya, Wamae, Magambo, Mbae, Mulinge, Zeyhle, Wassermann, Kern and Romig2012) and in Ethiopia (28%) by Debas and Ibrahim (Reference Debas and Ibrahim2013). CE prevalence found was lower than that reported in Ethiopia by Serda and Jago (Reference Serda and Jago2017) and Mandefro et al. (Reference Mandefro, Tilahun, Bayu and Zeryehun2019) of 52.5 and 54%, respectively, in Adama municipal abattoir, south-eastern Ethiopia, 34.5% in Bahir Dar, North West Ethiopia (Kebede et al., Reference Kebede, Mitiku and Tilahun2009a), 40.5% in Addis Ababa Abattoirs Enterprises (Terefe et al., Reference Terefe, Kebede, Beyene and Wondimu2012), 46.8% central Oromia, Ethiopia (Getaw et al., Reference Getaw, Beyenea, Ayanab, Megersa and Abunnac2010) and 48.7% in Arusha, Tanzania (Ernest et al., Reference Ernest, Nonga, Kassuku and Kazwala2009). CE found in Moroto was higher than that reported in Kajiado, Kenya: of 14.3% (Nungari et al., Reference Nungari, Mbae, Gikunju, Mulinge, Kaburu, Zeyhle and Magambo2019) and 5.3% in Migori county (Kere et al., Reference Kere, Erume, Banda and Kagira2019); in Ethiopia: of 21% in Addis Ababa Abattoir Enterprises (Kumsa, Reference Kumsa2019), in Gessa (17%) and Wolaita Sodo (16.85%), southern Ethiopia (Bekele and Butako, Reference Bekele and Butako2011; Mesfin et al., Reference Mesfin, Dawa, Yirgalem, Denano and Fesseha2022) and 15.2% in north-western Ethiopia (Kebede et al., Reference Kebede, Gebre-Egziabher, Tilahun and Wossene2011). Despite being in the same ecological zones of ‘horn of Africa’, these differences in prevalence could have been due to variances in environmental conditions, livestock population densities, livestock migrations and grazing systems (Njoroge et al., Reference Njoroge, Mbithi, Gathuma, Wachira, Gathura, Magambo and Zeyhle2002; Serda and Jago, Reference Serda and Jago2017), diverse cultures and E. granulosus strains (McManus, Reference McManus2006) and awareness (Omadang et al., Reference Omadang, Chamai, Othieno, Okwi, Inangolet, Ejobi, Oba and Ocaido2018) in these areas.
CE prevalence of 28% in sheep found in Moroto was similar to 29.5% in sheep reported among sheep slaughtered in restaurants in south-western Oromo (Kumsa and Mohammedzein, Reference Kumsa and Mohammedzein2014) and 29.3% in central Oromia, Ethiopia (Getaw et al., Reference Getaw, Beyenea, Ayanab, Megersa and Abunnac2010). CE prevalence of sheep in Moroto was much lower than that reported earlier in CE hyperendemic zones in southern Italy of 62.9% (Bosco et al., Reference Bosco, Alves, Cociancic, Amadesi, Pepe, Morgoglione, Maurelli, Ferrer-Miranda, Santoro, Ramos, Rinaldi and Cringoli2021) and in eastern Ethiopia of 68% (Sissay et al., Reference Sissay, Uggla and Waller2008). Lower CE prevalence rates of sheep had also been reported in Kenya of 14.9% by Nungari et al. (Reference Nungari, Mbae, Gikunju, Mulinge, Kaburu, Zeyhle and Magambo2019) in Kajiado, 16% by Odongo et al. (Reference Odongo, Tiampati, Mulinge, Mbae, Bishop, Zeyhle, Magambo, Wasserman, Kern and Romig2018) in Narok county and 0.1% by Kere et al. (Reference Kere, Erume, Banda and Kagira2019) in Migori county; and 17.1% in Ethiopia (Tadesse et al., Reference Tadesse, Birhanu, Sultan, Ayele and Ejeta2014).
CE prevalence of 29.1% found in goats was similar to that reported in CE hyperendemic zones in southern Italy of 28% (Bosco et al., Reference Bosco, Alves, Cociancic, Amadesi, Pepe, Morgoglione, Maurelli, Ferrer-Miranda, Santoro, Ramos, Rinaldi and Cringoli2021), 24.8% in south-western Oromo, Ethiopia (Kumsa and Mohammedzein, Reference Kumsa and Mohammedzein2014) and 22.2% in Ngorongoro, Tanzania (Miran et al., Reference Miran, Kasuku and Swai2017). Much higher CE prevalence of 65% in goats had been reported (Sissay et al., Reference Sissay, Uggla and Waller2008) in south-eastern Ethiopia and 63.8% in Tanzania (Ernest et al., Reference Ernest, Nonga, Kassuku and Kazwala2009). However, lower goat CE prevalence rates had also been reported in Kenya of 16% (Odongo et al., Reference Odongo, Tiampati, Mulinge, Mbae, Bishop, Zeyhle, Magambo, Wasserman, Kern and Romig2018) and 14.8% (Nungari et al., Reference Nungari, Mbae, Gikunju, Mulinge, Kaburu, Zeyhle and Magambo2019).
An earlier study (Othieno et al., Reference Othieno2016) also showed high prevalence of CE in humans using ultrasound screening. The risk factors were found to be, owning of a large number of livestock, large dog populations found in livestock grazing and watering areas, home livestock slaughters and feeding of dogs with cystic offals (Oba et al., Reference Oba, Ejobi, Omadang, Chamai, Okwi, Othieno, Inangolet and Ocaido2016; Othieno et al., Reference Othieno, Okwi, Mupere, Zeyhle, Oba, Chamai, Omadang, Inangolet, Siefert, Ejobi and Ocaido2017; Omadang et al., Reference Omadang, Chamai, Othieno, Okwi, Inangolet, Ejobi, Oba and Ocaido2018). Overall, these were promoted by limited awareness within the community of the epidemiology of CE (Omadang et al., Reference Omadang, Chamai, Othieno, Okwi, Inangolet, Ejobi, Oba and Ocaido2018; Othieno et al., Reference Othieno, Ocaido, Mupere, Omadang, Oba and Okwi2018). The observation shows that CE is endemic and a public health hazard in the study areas and the potential could be transmission to humans.
Almost all (96.7%) of livestock slaughtered were old animals beyond 3 years. This is because most livestock communities keep indigenous zebu and Ankole cattle which achieve slaughter weight at 3 and more years and hence longer exposure to E. granulosus eggs over time. Older animals above 3 years were more affected than younger ones. This was in agreement with the study by Terefe et al. (Reference Terefe, Kebede, Beyene and Wondimu2012) in Ethiopia. There was very highly significant difference in CE prevalence between sexes, with males being highly infected. Although the specific reason for this is not clear, it could be postulated that males are heavier than females hence more male cattle appear in abattoirs for slaughter and hence more preferred for purchase by the cattle traders (butchers) than females. The higher prevalence of CE in older livestock >3 years could be due to cumulative exposure of older animals to CE infection over time. This was in agreement with suggestions by Torgerson et al. (Reference Torgerson, Williams and Abo-Shehada1998); Larrieu et al. (Reference Larrieu, Costa, Cantoni, Alvarez, Cavagion, Labanchi, Bigatti, Araya, Herrero, Alvarez, Mancini and Cabrera2001) and Kebede et al. (Reference Kebede, Mitiku and Tilahun2009a). Lung was the most affected organ in all livestock species: sheep, goats and cattle (Tables 4 and 5). This was in agreement with what was observed in Kenya (Kere et al., Reference Kere, Erume, Banda and Kagira2019), in Ethiopia (Getaw et al., Reference Getaw, Beyenea, Ayanab, Megersa and Abunnac2010; (Negash et al., Reference Negash, Beyenea and Kumsa2013) and in China (Meng et al., Reference Meng, Guanglei, Jun, Xinquan, Tianli, Xuemei, Jinsheng, Huisheng, Kuojun and Chuangfu2014). In contrary, liver was the most affected organ in humans in the study area using ultrasound screening (Othieno et al., Reference Othieno2016). Furthermore, liver was the most livestock affected. This was found to be true in Kenya (Addy et al., Reference Addy, Alakonya, Wamae, Magambo, Mbae, Mulinge, Zeyhle, Wassermann, Kern and Romig2012; Odongo et al., Reference Odongo, Tiampati, Mulinge, Mbae, Bishop, Zeyhle, Magambo, Wasserman, Kern and Romig2018; Nungari et al., Reference Nungari, Mbae, Gikunju, Mulinge, Kaburu, Zeyhle and Magambo2019).
The lungs and livers were the most CE-infected. This is because they are the first organs rich in capillaries to be met by migrating Echinococcus oncospheres hence easily accessing the portal vein via the hepatic and pulmonary blood vessel system prior to any other peripheral organ. Also, the high infection rates in the lungs were probably due to their softer consistency thereby allowing easier development of the cysts with advancement in age (Himonas et al., Reference Himonas, Frydas and Antoniadol-Sotiriadou1987). However, a majority of lung CE cysts were small sized. Liver and mixed organ infections had medium and large cysts. Similarly, the more the multi-organ infected the more the number of cysts recovered per organ (Table 7). For lung and liver 1.4 cysts were recovered per organ, 3.2 cysts were recovered per mixed lung and liver infection and 5 cysts per mixed lung, liver and spleen infection. This could mean the CE infection causing CE multi-organ infection was more aggressive due to different genotypes of infecting E. granulosus strains, host immunity, site, size of the cysts and geographical location, host, site, size and type of cyst may have different rates of fertility (Ibrahim, Reference Ibrahim2010). A study by Chamai et al. (Reference Chamai, Omadang, Erume, Ocaido, Oba, Othieno, Bonaventure and Kitibwa2016) in Moroto found majorly E. granulosus sensu stricto – sheep (G3) strain and E. canadensis (G6/7) strains in slaughtered livestock and could partly explain this scenario. No fertile cysts were recovered from liver cysts of sheep, zebu cattle and goats. Most CE cysts recovered in the lungs and liver of goats, sheep and zebu cattle were calcified. This may suggest that goats, sheep and zebu cattle are slaughtered when they are older and by then most developed cysts had calcified. Ankole cattle had 33.9 and 4% fertile cysts in the liver and lungs respectively; sheep 1.7% and zebu cattle 6.4% had fertile cysts only in the liver, while goats had 4.5% fertile cysts in the lungs only. Fertile cysts pose greater risk for CE transmission when fed to dogs. This showed that sheep, goats and zebu cattle may potentially play a less significant role as intermediate hosts of CE in their localities as compared to Ankole cattle. Cysticercus tenuicollis is a tapeworm which has the same lifecycle as Echinococcus worms, sharing the same canids, especially dogs, as their final hosts, and herbivores as their intermediate hosts (Murell, Reference Murell2005). Almost all sheep and goats which had CE infection also had C. tenuicollis infection in their mesenteries. There was high prevalence of C. tenuicollis in all districts of this study. This was because dogs had access to pastures that were being grazed by goats and sheep and hence can contaminate pastures with their fecal matter. The overall prevalence of 35.4 and 23.3% observed in goats and sheep respectively in this study was comparable to what has been observed among goats and sheep in Pairaba, Brazil of 39% in goats and 17.4% in sheep (de Morais et al., Reference de Morais, Vilela, Feitosa, dos Santos, Gouveia, Athayde and de Azevêdo2017) and in Ceara of 26.2% in goats and 35% in sheep (Soares et al., Reference Soares, Maquelotti, Grisi and Serra-Freire2012) and in Uttar Pradesh, India of 27.3% in goats and 37.2% in sheep (Pathak and Gaur, Reference Pathak and Gaur1982); in Soroti, Uganda of 42.5% in sheep and 33.3% in goats (Nyero et al., Reference Nyero, Zirintunda, Omadang and Ekou2014) and in Nile Delta, Egypt of 21% in sheep (Abbas et al., Reference Abbas, El-Alfy, Janecek- Erfurth and Strubep2021). More high prevalence rates have been observed among goats (53%) and sheep (79%) in eastern Ethiopia (Sissay et al., Reference Sissay, Uggla and Waller2008). Much lower prevalence had been observed in north India of 4.8% in goats and 2.2% in sheep (Singh et al., Reference Singh, Sharma, Gill and Sharma2015), northeast Tunisia of 8.9% in goats and 2.2% in sheep (Khaled et al., Reference Khaled, Teber, Bouaicha, Amairia, Rekik and Gharbi2020) and northwest Iran of 8.9% in goats and 2.8% in sheep (Mirzaei and Rezaei, Reference Mirzaei and Rezaei2015). Cysticercus tenuicollis though not zoonotic does not cause serious health effects in goats and sheep but have been found to lower their productivity (Soares et al., Reference Soares, Maquelotti, Grisi and Serra-Freire2012; de Morais et al., Reference de Morais, Vilela, Feitosa, dos Santos, Gouveia, Athayde and de Azevêdo2017; Abbas et al., Reference Abbas, El-Alfy, Janecek- Erfurth and Strubep2021). Therefore dogs should be dewormed to get rid of adult cestode worms which shed their eggs in dogs’ feces thereby contaminating pasture grazed by livestock.
In the present study, it has been observed that CE is endemic in pastoral and agro-pastoral areas in Uganda; higher prevalence was reported in sheep, goats and zebu cattle in Moroto compared to Kumi, Luwero and Nakasongola districts. Overall, the lungs were more affected than the liver. Higher cyst fertility rates in the liver of Ankole cattle, zebu cattle and sheep and lungs of goats suggest Ankole and zebu cattle, sheep and goats play an important role in the epidemiology of CE zoonosis and offer a great potential risk of transmission to humans.
Cysticercus tenuicollis, a similar type of tapeworm to Echinococcus spp. causing CE, was more prevalent in goats in all the study areas while sheep prevalence was observed only in Moroto and Kumi districts. This prevalence (C. tenuicollis and E. granulosus cysts) in food animals raises the possibility of dog infection from condemned infected organs, hence food and water contamination by abundant stray dogs’ infected fecal matter. This is responsible for disease transmission onto livestock and humans and therefore posing a serious public health risk. There is therefore an urgent need to create public health awareness among the communities about the need for proper and safe infected organ disposal, hence the epidemiology of both C. tenuicollis and E. granulosus in dogs, livestock and humans. Similar prevalence studies should also be undertaken in other areas of Uganda, and furthermore, assessment of financial losses due to CE, risk factor determination and CE molecular characterization in all livestock, dogs and humans. This will inform the relevant stakeholders in the animal and health sectors to enhance control strategies in livestock and the communities keeping them.
Data availability
Data supporting results are provided within the article.
Acknowledgements
The authors thank Dr Eberhard Zeyle and Mulinge Erastus from Kenya Medical Research Institute (KEMRI) for the technical guidance. The authors appreciate the support received from the district authorities and the respective technical/veterinary staff, traders and butchers of Moroto, Kumi, Bukedea, Luwero and Nakasongola districts, for participating in this study.
Author's contribution
L. O., M. O. and F. E. conceived and designed the study. L. O., M. C. and P. O. carried out the field work. L. O., M. C. and J. E. performed laboratory analysis. L. O. and P. O. performed statistical analyses and all the authors wrote and revised the article.
Financial support
This research was funded by the Higher Education, Science and Technology (HEST) project, Busitema University, Uganda.
Competing interests
None.
Ethical standards
Approval for the study was obtained from the Institutional Review Board (IRB) of the School of Veterinary Medicine and Animal Resources (SVAR) research ethics committee (REC)-SVAR IACUC/IRB-Ref SVAR_IACUC/40/2020, Makerere University and from Uganda National Council of Science and Technology (UNCST)-Ref A87ES. Approval for the study in each district was obtained from the respective District Veterinary Offices and written consent from livestock owners and butchers was obtained before enrolment into the study.