CLINICIAN'S CAPSULE
What is known about the topic?
Aeromedical evacuation is risky, resource intensive, and is done by a variety of crew compositions.
What did this study ask?
What impact do advanced provider presence and crew composition have on outcomes for adult trauma patients evacuated by air?
What did this study find?
Findings showed a trend towards improved survival and other outcomes for adult trauma patients treated by aeromedical evacuation crews led by advanced providers.
Why does this study matter to clinicians?
Better outcomes could be achieved by determining how advanced providers contribute to reduced mortality and other metrics in aeromedical evacuation.
INTRODUCTION
Mortality from trauma represents 10% of global deaths. Injuries kill over five million people annually and account for 12% of the global burden of disease.1,Reference Krug, Dhalberg, Mercy, Zwi and Lozano2,Reference Murray and Lopez3 In the military setting, severe injury mechanisms lead to distinctive early lethality patterns and more deaths occurring shortly after wounding.Reference Eastridge, Mabry and Seguin4 Prehospital care improvements have led to increased survival, but the greatest potential for improved outcomes still lies in lowering preventable deaths.Reference Cutting and Agha5,Reference Eastridge, Holcomb and Shackelford6 It is thought that implementing a military rotary-wing Forward Aeromedical Evacuation during the Korean and Vietnam conflicts provided a 2% absolute mortality reduction in hospitalized soldiers, compared with World War II.Reference Galvagno, Sikorski and Hirshon7 In subsequent years, civilian Helicopter Emergency Medical Services (HEMS) became widespread in the developed world.Reference Butler, Anwar and Willett8
Together, military Rotary Wing and Vertical/Short Take Off and Landing Forward Aeromedical Evacuation and HEMS deliver Primary Aeromedical Retrieval. In this paper, Primary Aeromedical Retrieval is defined as retrieving patients from point of injury and transferring them to a medical treatment facility by Rotary Wing or Vertical/Short Take Off and Landing airframes with medical providers on board. Forward Aeromedical Evacuation refers to military Primary Aeromedical Retrieval, and HEMS refers to civilian Primary Aeromedical Retrieval.
In trauma, Primary Aeromedical Retrieval is thought to improve patient outcomes through rapid transfer to trauma centres and by providing advanced prehospital interventions.Reference Dreyfuss, Faktor and Charnilas9 Many studies show that Primary Aeromedical Retrieval is associated with improvements in morality and other outcomes. However, other studies showed no such benefit.Reference Butler, Anwar and Willet10
HEMS is expensive to implement and maintain. One medium helicopter's annual operating costs can reach 1.3 M USD.Reference Collett11 HEMS is inherently risky for crew members, particularly when responding at night or in marginal weather. Forward Aeromedical Evacuation missions are even costlier and riskier. Military rotary-wing aircraft are more expensive to acquire and operate than their related civilian airframes. Forward Aeromedical Evacuation crews are exposed to enemy action at the point of injury. It is therefore important to clearly determine the benefits of Primary Aeromedical Retrieval and to elucidate from where these benefits are derived.
The benefit of rapid retrieval is more pronounced the farther that the trauma centre is from the scene. Yet studies show that early advanced clinical interventions have a greater positive impact on mortality than retrieval time.Reference Moylan, Fitzpatrick and Beyer12 If clinical procedures during Primary Aeromedical Retrieval have an impact on mortality, does it matter what kind of medical professionals provide them? There are studies that compared physician HEMS to paramedic Ground EMS, with divergent conclusions. But the confounding factors when comparing HEMS and Ground EMS treatment groups are extensive and obviously included the mode of transportation.Reference Garner13 In Europe, where physicians are common, a survival benefit due to physician-led crews was identified.Reference Baker, Neill, Se, Haddon and Long14 Other narrative reviews without a systematic approach reported conflicting results.Reference Sikka and Margolis15 We therefore conducted a descriptive systematic review comparing different crew composition in Primary Aeromedical Retrieval, in military and civilian settings, addressing different clinical outcomes in the trauma population.
MATERIALS AND METHODS
This systematic review is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Reference Moher, Liberati, Tetzlaff and Altman16
Studies
The search included prospective and retrospective cohort studies (with or without a control group), case control studies, and randomized controlled trials that addressed clinical outcomes for different air ambulance crew configurations. Case reports and case series were excluded. Studies were included if they reported at least one outcome of interest.
Participants
We included studies with a population of adult trauma patients transported by air, directly from the scene of the accident to the receiving trauma centre. Providers studied included medical doctors, nurses, and/or paramedics of different backgrounds and levels of expertise.
Interventions and controls
The intervention was the Primary Aeromedical Retrieval crew composition, defined as any difference in provider type (medical doctors, nursing, and paramedics of different levels of training, subspecialties, or expertise). Controls were any comparison between crew configuration, that is, physician compared with paramedic, nurse, and so forth.
Outcome measures
The primary outcome of interest was mortality. Secondary outcomes included, but were not limited to, hemodynamic status, length of stay, disposition, mean response time, scene time, delivery time, clinical interventions, and procedures. We searched for any time-based data on response time, scene time, and time to the emergency department (ED) or operating room. We looked for information about on scene and flight clinical interventions performed, such as rapid sequence induction, endotracheal intubation, mechanical ventilation, oxygen treatment, fluid resuscitation with crystalloids or blood products, thoracic decompression by needle or tube thoracostomies, and analgesia. Finally, we documented patient disposition (discharge home, rehabilitation, direct discharge from ED, and patients transferred to another facility) and length of stay (Intensive Care Unit days, hospital days).
Search methods
We searched Medline (from 1946 to January 1, 2020), Embase (1947 to January 1, 2020), Cochrane Controlled Trials Register (from inception to January 1, 2020), ClinicalTrials.gov (http://www.clinicaltrials.gov), and Google Scholar (first 200 hits). The search was not restricted by date, language, or publication status. Search terms were defined a priori and by reviewing the MeSH terms of articles identified in preliminary literature searches. The search strategy was based on the Medline initial search strategy and was modified as necessary for the other databases. A search strategy combining MeSH headings and the keywords “air ambulance/aeromedical evacuation/air evacuation/aeromedical transport/air patient transport” AND “team or group/unit or squad/crew” was used after a decision with an experienced librarian.
Data abstraction
Two review authors (CL, JPRC) not blinded to authors, journal or institutions, examined all study abstracts and full texts independently, which were identified by the search. Titles and abstracts of every record retrieved were screened to determine which of the studies should undergo a full-text review. Full texts of the studies with questionable eligibility or considered eligible were retrieved in this phase for evaluation. The reference lists of the retrieved articles were also searched for additional citations. Any disagreements were resolved by consensus or with another review author (LTDL). Only published data were included. Study authors were not contacted for obtaining or clarifying further information. At the data extraction period, data were also collected independently by two review authors (CL and JPRC).
Risk of bias assessment
Risk of bias was assessed by two review authors (LTDL and CL) for each included study. Disagreements were resolved through discussion and consensus with a third author (HT). Each included study was classified as observational cohort or case-control, and the risk of bias was assessed according to each type of study design. The Newcastle–Ottawa Scale was used to assess risk of bias in cohort studies and case-control studies.Reference Wells, Shea and O'Connell17 This tool defines patient groups as comparable in either the design or analysis when the effect of the exposure is adjusted for confounders. The Newcastle–Ottawa Scale assesses risk of bias in the domains of selection of exposed and non-exposed cohorts, comparability of cohorts, assessment of outcomes, and adequacy of follow-up. The Newcastle–Ottawa Scale scores 1 to 9. We considered studies with a score of < 3 with high risk of bias, 4–6 moderate, and > 7 low risk.
Analyses
Studies were analysed separately according to their design (retrospective or prospective cohorts and case-control studies). Clinical and methodological heterogeneity across the studies were assessed by examining the details of the subjects, the baseline data, the interventions, and the outcomes to determine whether or not the studies were sufficiently similar. Large heterogeneity and the absence of common outcome measures reported precluded meta-analyses. Therefore, all studies were analysed qualitatively with a descriptive systematic approach.
RESULTS
Included studies (Figure 1)
As indicated in Figure 1, the electronic search identified 3,778 potentially relevant citations. After removing duplicates, the abstracts for 1,668 potentially relevant studies were screened and 89 studies were selected for full-text review. From these, 16 studies met the inclusion criteria.Reference Baxt and Moody18–Reference Jung, Huh and Lee33 There was excellent agreement between the reviewers for study inclusion (Cohen`s Kappa, 0.87).Reference Cohen34
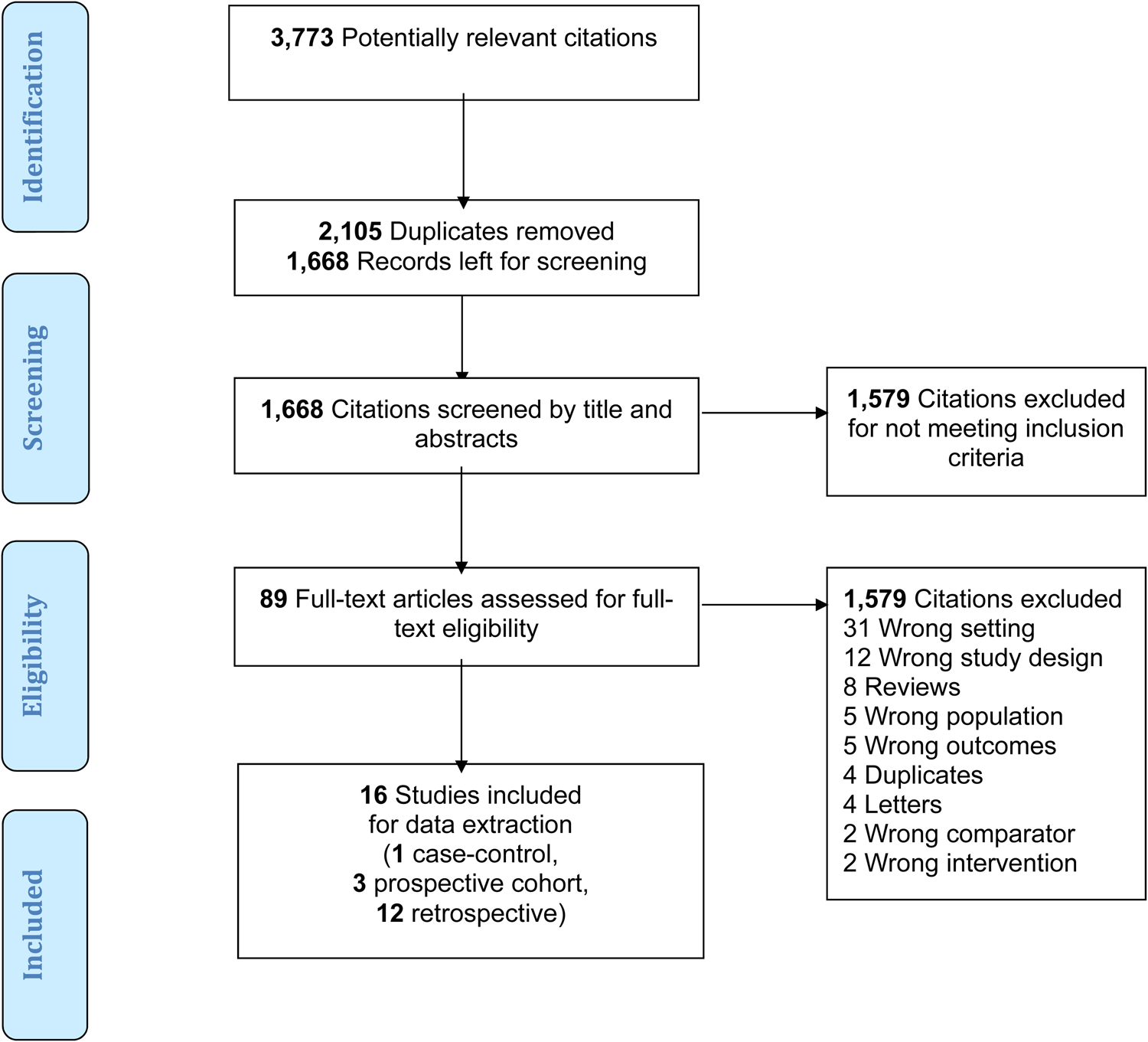
Figure 1. Flow chart of the screening process.
Interventions performed across the studies (Table 1)
Most studies evaluated the performance of crews that included a physician versus a non-physician crew.Reference Baxt and Moody18–Reference Burney, Hubert, Passini and Maio23,Reference Cameron, Pereira, Mulcahy and Seymour27–Reference Klemenc-Ketis, Tomazin and Kersnik29,Reference Apodaca, Olson and Bailey31–Reference Jung, Huh and Lee33 In two of these studies, the physician provider was a postgraduate resident physician.Reference Hamman, Cue and Miller19,Reference Housel, Pearson, Rhee and Yamada22 In another study, four different HEMS configurations were compared, each with a different physician-led crew composition, helicopter, and base location.Reference Klemenc-Ketis, Tomazin and Kersnik29 Another study compared multiple crew configurations (dual flight nurse or flight nurse plus paramedic, or emergency medicine (EM) resident or EM physician) with ground crews.Reference Abbott, Brauer, Hutton and Rosen24 Two observational studies did not address the presence of a physician as a crew member: WirtzReference Housel, Pearson, Rhee and Yamada22 examined the performance of a flight nurse + flight paramedic crew versus a dual flight nurse team. MabryReference Mabry, Apodaca and Penrod30 compared the outcomes between a critical care flight paramedic + basic paramedic crew against a lone basic paramedic crew.
Table 1. Summary of included study findings
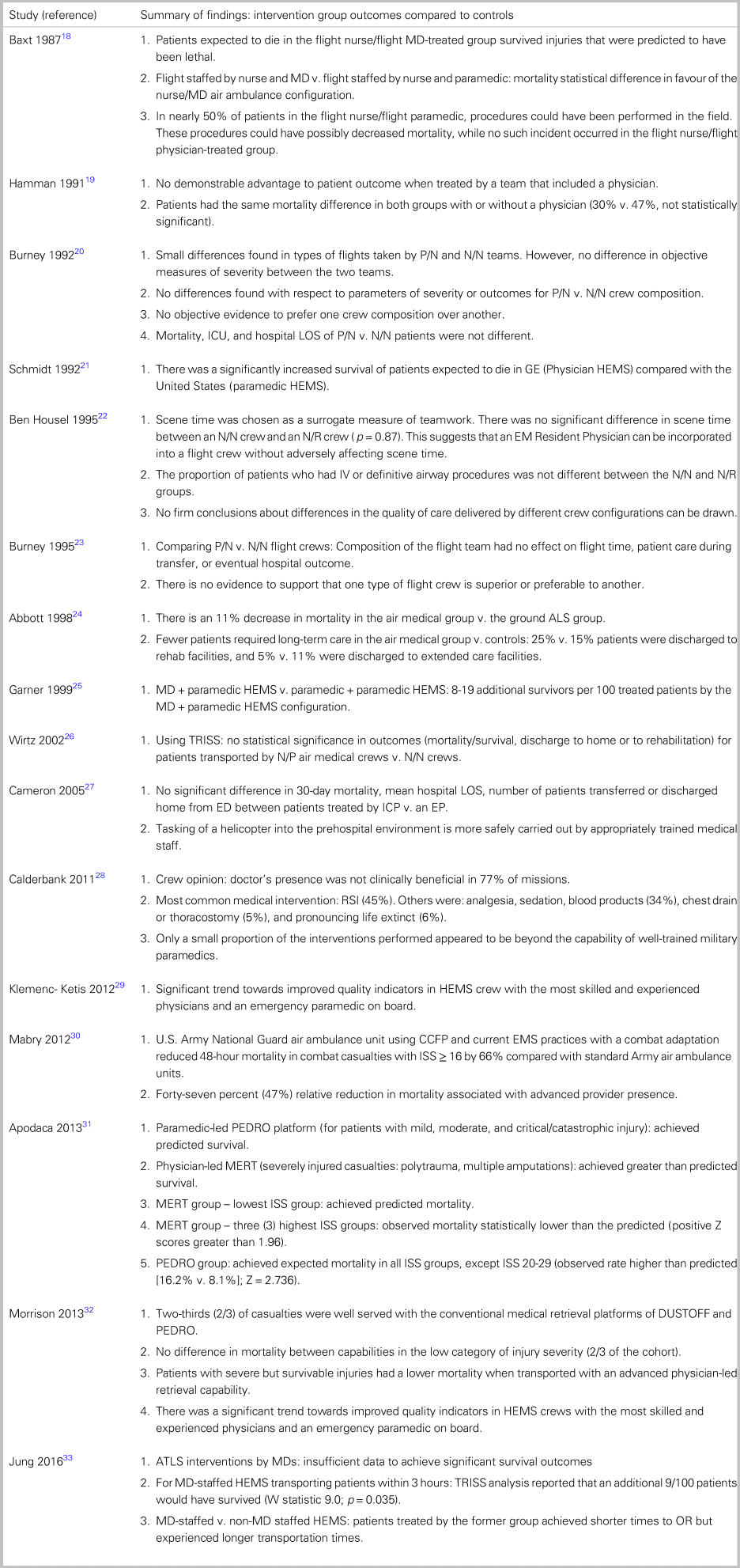
Notes: CCFP = Critical Care Flight Paramedic; DUSTOFF = U.S. Forward Aeromedical Evacuation helicopter platform with two basic paramedics; ED = emergency department; EM = emergency medicine; EMS = emergency medical services; EP = emergency physician; GE = German; HEMS = Helicopter Emergency Medical Services; HTT = helicopter trauma team; ICP = intensive care paramedic; ISS = Injury Severity Score; LOS = length of stay; MD = medical doctor; MERT = Medical Emergency Response Team – Physician-led UK Forward Aeromedical Evacuation helicopter platform; N/N = Nurse/Nurse; N/P = Nurse/Physician; N/R = Nurse/Resident; PEDRO = U.S. Forward Aeromedical Evacuation helicopter platform with two advanced care paramedics; RSI = rapid sequence induction; TRISS = Trauma Injury Severity Score.
Clinical characteristics (see Table 1)
There were 3 prospective cohort studiesReference Baxt and Moody18, Reference Burney, Hubert, Passini and Maio23, Reference Calderbank, Woolley and Mercer28 (n = 2,172), 12 retrospective cohort studiesReference Hamman, Cue and Miller19–Reference Housel, Pearson, Rhee and Yamada22, Reference Garner, Rashford, Lee and Bartolacci25–Reference Cameron, Pereira, Mulcahy and Seymour27, Reference Klemenc-Ketis, Tomazin and Kersnik29–Reference Jung, Huh and Lee33 (n = 8,491), and 1 case-control studyReference Abbott, Brauer, Hutton and Rosen24 (n = 1,286). In all studies, patients were transported to a trauma centre. Four studiesReference Schmidt, Frame and Nerlich21, Reference Housel, Pearson, Rhee and Yamada22, Reference Garner, Rashford, Lee and Bartolacci25, Reference Klemenc-Ketis, Tomazin and Kersnik29 transported patients to more than one trauma centre. Four studiesReference Calderbank, Woolley and Mercer28, Reference Mabry, Apodaca and Penrod30-Reference Morrison, Oh and DuBose32 were conducted in a military setting (the Afghanistan conflict), and 12 studiesReference Baxt and Moody18-Reference Cameron, Pereira, Mulcahy and Seymour27, Reference Klemenc-Ketis, Tomazin and Kersnik29, Reference Jung, Huh and Lee33 were conducted in civilian settings. Eight studies were conducted in the United States,Reference Baxt and Moody18-Reference Abbott, Brauer, Hutton and Rosen24, Reference Wirtz, Cayten, Kohrs, Atwater and Larsen26 two in Australia,Reference Garner, Rashford, Lee and Bartolacci25, Reference Cameron, Pereira, Mulcahy and Seymour27 one in Slovenia,Reference Klemenc-Ketis, Tomazin and Kersnik29 and one in South Korea.Reference Jung, Huh and Lee33 One study compared two international settings: a trauma surgeon/paramedic crew in Hannover, Germany, with a flight nurse/paramedic crew in Knoxville, Tennessee.Reference Schmidt, Frame and Nerlich21 The mean age ± SD of patients across all included studies was 35.6 ± 9.3, and their mean ± SD Injury Severity Score (ISS) was 18.0 ± 8.16. Most patients were male (73%).
Risk of bias (Table 2)
Observational cohort studies
Only one studyReference Mabry, Apodaca and Penrod30 scored a 9 in the Newcastle–Ottawa Scale and demonstrated a low risk of bias. All other studiesReference Baxt and Moody18-Reference Burney, Hubert, Passini and Maio23, Reference Garner, Rashford, Lee and Bartolacci25–Reference Klemenc-Ketis, Tomazin and Kersnik29, Reference Apodaca, Olson and Bailey31-Reference Jung, Huh and Lee33 scored a 6 to 8, demonstrating an overall moderate risk of bias. Most studies had no comparable controls, as they did not report adjustment for confounders in either the design or analysis.
Table 2. Included studies – risk of bias (The Ottawa-Newcastle toolReference Wells, Shea and O'Connell17)
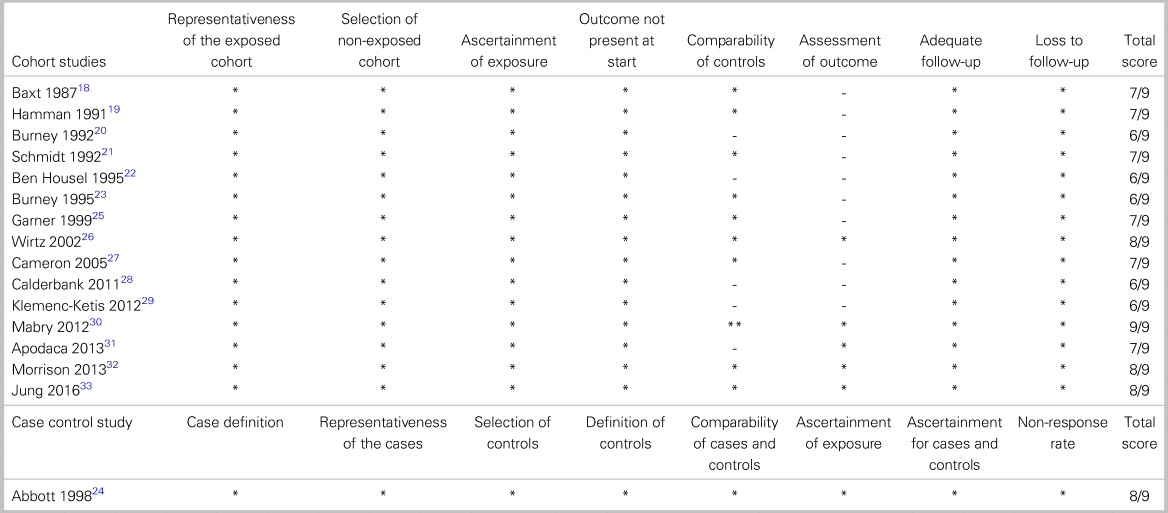
*High quality choices are indicated by a star. Comparability has a maximum of two stars. All other categories have a maximum of one.
Case-control study
The case-control study had a score of 8 in the Newcastle–Ottawa Scale.Reference Abbott, Brauer, Hutton and Rosen24
Outcomes measured across the studies (Table 3)
Primary outcome
Mortality was the most common outcome measured across the studies. In most studies, there was a mortality benefit associated with the presence of more advanced providers. In six studies, there was a significant mortality benefit in physician-led crews compared with non-physician-led crews.Reference Baxt and Moody18,Reference Schmidt, Frame and Nerlich21,Reference Abbott, Brauer, Hutton and Rosen24,Reference Garner, Rashford, Lee and Bartolacci25,Reference Apodaca, Olson and Bailey31,Reference Morrison, Oh and DuBose32 BaxtReference Baxt and Moody18 found that, in the physician-led group, 11 patients died, out of n = 316, where 16.9 were predicted to die (Z statistic = 2.284, p < 0.05). The study also identified a 35% reduction in mortality compared with the non-physician-led crews (Z statistic = 2.076, p < 0.05). SchmidtReference Schmidt, Frame and Nerlich21 found 9 unexpected survivors in the physician HEMS group (Z statistic = 2.459, W statistic = 1.35) compared with only 6 unexpected survivors in the United States, non-physician-led crews (Z statistic = 1.049). AbbottReference Abbott, Brauer, Hutton and Rosen24 found an 11% mortality reduction in the air transported group (OR = 1.75, p < 0.01, 95% CI 1.21-2.53), which persisted after adjustment for age (OR = 1.57, 95% CI: 1.06-2.27). GarnerReference Garner, Rashford, Lee and Bartolacci25 found a significant mortality benefit in the physician-treated group (Z = 2.72, p < 0.01 and W = 0.48, 95% CI: 3.84-15.12) but not in the paramedic-treated group (Z = -1.16, p = 0.25). The adjusted W statistic in comparing the physician versus paramedic group was 13.44 (95% CI: 7.8-19.08), suggesting an additional 13 survivors per 100 patients treated by the physician group.
Table 3. Included study characteristics
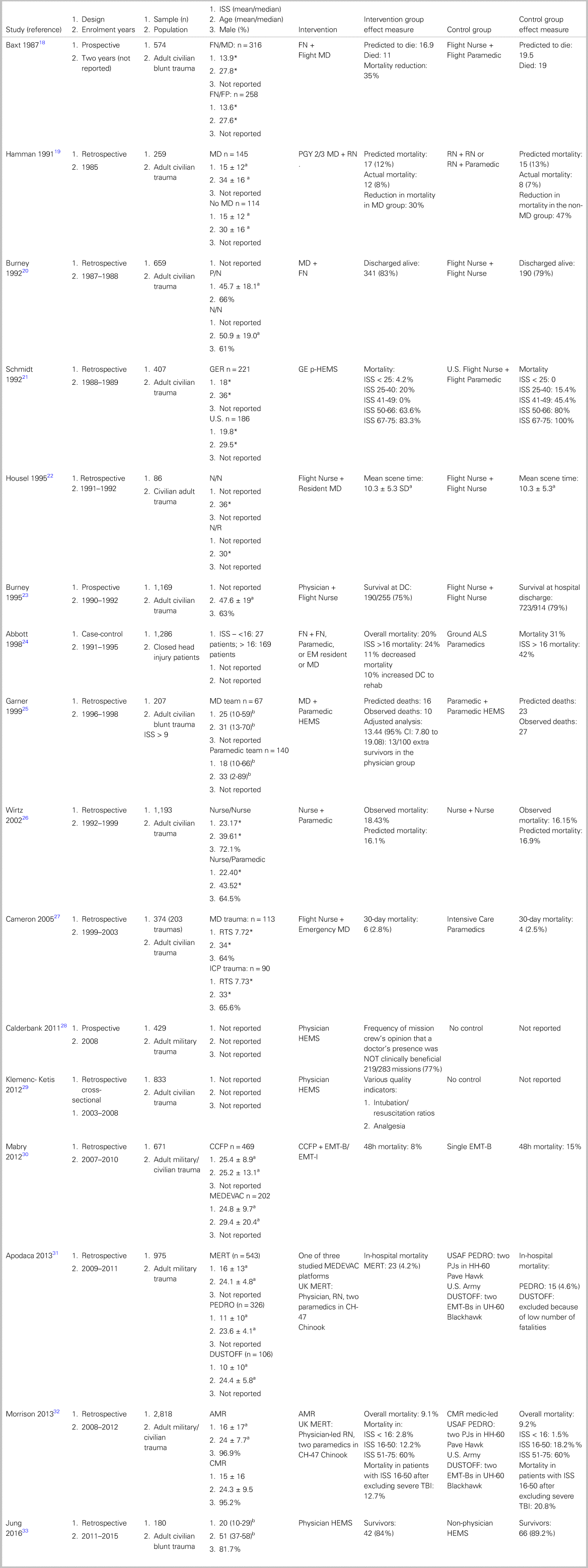
Notes: a Mean, b Median, *Standard deviation not reported.
Three studies conducted in the military setting revealed that the survival benefit was most pronounced in patients with more severe, but survivable injuries.Reference Mabry, Apodaca and Penrod30–Reference Morrison, Oh and DuBose32 MabryReference Mabry, Apodaca and Penrod30 found a significant mortality reduction of 66% in patients with ISS > 15 treated by an advanced care paramedic-led crew compared with a basic paramedic crew. The mortality rate in U.S./North Atlantic Treaty Organization military, Afghan military settings, and Afghan civilian settings treated by Critical Care Flight Paramedic crews were 15%, 4%, and 5%, respectively, compared with respective mortality rates of 12%, 18%, and 16% for patients treated by basic paramedic crews. The 48-hour mortality of patients treated by advanced providers was 8% versus 15% in the group treated by basic paramedics (OR 0.24, 95% CI: 0.14-0.88). ApodacaReference Apodaca, Olson and Bailey31 found a significant reduction of in-hospital mortality in patients with ISS of 20–29 treated by the physician-led UK Medical Emergency Retrieval Team (MERT–UK Forward Aeromedical Evacuation with advanced medical providers) compared with patients treated by two other non-physician-led forward Aeromedical Evacuation capabilities (4.8% v. 16.2%, p < 0.021). Furthermore, the Medical Emergency Retrieval Team–treated groups achieved lower mortality than predicted by the Trauma Injury Severity Score in all ISS > 9 patient groups, whereas the paramedic-led U.S. Army group was found to have a higher than predicted mortality in the ISS 20–29 group.Reference Apodaca, Olson and Bailey31 MorrisonReference Morrison, Oh and DuBose32 found a mortality reduction in patients with ISS 16–50 (after excluding severe traumatic brain injury [TBI]) in patients treated by the physician-led UK Medical Emergency Retrieval Team compared with patients treated by two other Forward Aeromedical Evacuation platforms with no physicians (12.2% v. 18.2%, p = 0.035).
In four studies,Reference Hamman, Cue and Miller19,Reference Burney, Passini, Hubert and Maio20,Reference Burney, Hubert, Passini and Maio23,Reference Cameron, Pereira, Mulcahy and Seymour27 there was no significant mortality difference associated with the presence of more advanced health care providers. HammanReference Hamman, Cue and Miller19 found similar mortality and similar causes of death when directly comparing flight teams with and without a physician (Z statistic 2.03 v. 3.11 for physician and non-physician groups). BurneyReference Burney, Passini, Hubert and Maio20 found no difference in mortality between patients treated by physician plus nurse and nurse plus nurse teams (year one: 76% v. 78%, p = 0.06, year two: 70% v. 80%, p = 0.06). In addition, WirtzReference Schmidt, Frame and Nerlich21 found no significant difference in mortality outcomes between patients transported by a flight nurse plus paramedic crew versus a dual flight nurse crew (p = 0.14).
For secondary outcomes, see Supplemental Material.
DISCUSSION
Main findings
This review summarizes the evidence for how crew composition in Primary Aeromedical Retrieval impacts clinical outcomes in adult trauma patients. Overall, there was a trend to improved mortality with crews comprising, or led by, providers with advanced training and/or more experience. Where population segments were broken down by ISS, this mortality benefit was most pronounced in patients with severe but survivable injuries, and in patients with severe TBI. With respect to secondary outcomes, most studies reported no significant differences in quality of patient care indicators, such as on-scene time, ratios of appropriate clinical interventions, hypotension, length of hospital and Intensive Care Unit stay, and discharge disposition.
In a review of mortality during recent military settings, 87.3% of battlefield deaths occurred prehospital, of which 35.2% died instantaneously due to physical dismemberment, catastrophic brain injury, and destructive cardiothoracic great vessel injuries.Reference Eastridge, Holcomb and Shackelford6 The remainder died within minutes to hours before reaching a trauma centre. Most patients (75.7%) had non-survivable injuries (severe TBI, great vessel injury, high spinal cord injury, and abdomino-pelvic destructive injuries). The remaining 24.3% had potentially survivable injuries, of which 8.0% were airway compromise and 90.9% were hemorrhagic (67.3% truncal, 19.2% junctional, and 13.5% extremity). It is hard to extrapolate from military to civilian settings. However, we can say that this analysis points to a set of “most potentially survivable injuries.” Bearing in mind this (military) injury and mortality pattern, and examining studies showing a pronounced survival trend in severely injured patients treated by (military) Forward Aeromedical Evacuation crews containing advanced providers, one can posit that 1) there is a subset of key prehospital interventions that have the greatest influence on overall mortality,Reference Cutting and Agha5 and 2) there is a subset of providers prepared to a) assess the requirement for, and b) implement the aforementioned interventions better than the remainder.
The evidence suggests that advanced providers in Primary Aeromedical Retrieval may be more decisive and/or competent in performing these interventions. However, our inquiry suffers from a lack of detailed content and high-quality evidence, which precludes robust conclusions about which prehospital interventions are responsible for improving clinical outcomes and which providers are best prepared to administer them. In fact, the current data registries may simply not have sufficiently granular, high-quality data. We also noted that the current evidence does not report on other aspects that advanced providers may offer: leadership, clinical judgement and decision-making, reassurance, leading after action reviews, and coordinating quality improvement.Reference Calderbank, Woolley and Mercer28
Strengths and weaknesses of this review and future research
To our knowledge, this is the first systematic review to examine the influence of crew composition on clinical outcomes in adult trauma. This study is limited by the observational nature of the data, so confounding is highly probable. Also, most observational data are represented by small retrospective studies with high clinical and methodological heterogeneity. The interventions and controls varied substantially across all studies. Moreover, the various different endpoints were addressed inconsistently and without adjusted analyses for covariates. Finally, no common effect measures could be pooled for quantitative analysis due to the data's heterogeneity.
Primary Aeromedical Retrieval's high costs, high risks, combined with high military trauma prehospital mortality with its great proportion of survivable injuries underscore a need for well-designed studies. Randomized controlled studies that are planned in detail from the design and research question phase should be conducted. Interventions and controls should be better standardized. Meaningful clinical endpoints should be addressed, such as mortality and other important outcome measures in patients with brain injury, compromised airway and ventilator status, and hemorrhagic injuries. Data points should detail the type of intervention performed, by which provider, and to what effect. Some examples of important interventions are intravenous and intraosseous access, chest decompression, time between injury and transfusion of blood products and tranexamic acid administration, junctional and extremity tourniquet application, use of vasoactive drugs, and hypothermia prevention.
CONCLUSION
In trauma, the data on the outcomes of different crew composition in Primary Aeromedical Retrieval demonstrated that a trend towards decreased mortality was associated with the presence of advanced providers. However, these results should be interpreted with caution because the evidence is constrained by small sample sizes, observational studies, non-random treatment group allocation, and a high likelihood of confounding factors. Ultimately, an appropriately powered randomized trial that captures sufficient details on injury patterns, crew configurations, interventions and procedures performed, and meaningful clinical outcomes will be required to determine the most appropriate Primary Aeromedical Retrieval crew composition.
Supplemental material
The supplemental material for this article can be found at https://doi.org/10.1017/cem.2020.404.
Acknowledgements
The authors gratefully acknowledge Henry Lam, Librarian, Sunnybrook Health Sciences Centre, and Captain Sean Wilson, MD, Flight Surgeon CANSOFCOM CFB Trenton, for assistance with the literature search and proofreading, respectively.
Competing interests
None declared.






