Alcohol dependence (AD) is a component of alcohol use disorder (AUD) involving tolerance, withdrawal, and continued use despite problems (National Institute on Alcohol Abuse and Alcoholism, 2016). Young adults are at greater risk for AUD than any other age group (Grant et al., Reference Grant, Goldstein, Saha, Chou, Jung, Zhang, Pickering, Ruan, Smith, Huang and Hasin2015), and being diagnosed with AD by young adulthood has lasting effects on physical and mental health in late life (Haber et al., Reference Haber, Harris-Olenak, Burroughs and Jacob2016). Therefore, characterizing adolescent predictors of later AD is critical to identify relevant targets for preventive intervention efforts and to mitigate long-term consequences of AD symptoms.
Prior work has identified a series of adolescent factors related to young adult alcohol problems, including conduct disorder (CD) symptoms, aggression, higher levels of alcohol consumption, and depressive symptoms (Edwards et al., Reference Edwards, Gardner, Hickman and Kendler2016; Huurre et al., Reference Huurre, Lintonen, Kaprio, Pelkonen, Marttunen and Aro2010; Merline et al., Reference Merline, Jager and Schulenberg2008). However, the vast majority of studies examining adolescent predictors of AD are conducted on samples of unrelated individuals, and between-family differences remain an unaddressed potential confound. As a result, associations may reflect a causal effect of the adolescent factor on later AD, shared genetic liability, overlapping environmental influences, or a combination of these possibilities. Evaluating confounding by familial factors is, therefore, important for understanding pathways to AD and for developing effective intervention efforts. For example, there is evidence that overlapping genetic influences contribute to the correlation between CD symptoms and substance use (Verweij et al., Reference Verweij, Creemers, Korhonen, Latvala, Dick, Rose, Huizink and Kaprio2016), and socioeconomic status (SES) is related to both adolescent conduct problems (Piotrowska et al., Reference Piotrowska, Stride, Croft and Rowe2015) and rates of substance use disorders (Galea et al., Reference Galea, Nandi and Vlahov2004). If the prospective association between CD and AD is substantially reduced when controlling for shared familial influences, this suggests that intervention efforts aiming to reduce conduct problems in adolescence are not likely to reduce risk for later alcohol problems. On the other hand, if the magnitude of the association between CD symptoms and AD after accounting for between-family differences is largely the same as in the population, this would highlight conduct problems as a relevant target for preventive intervention.
Co-twin comparisons offer a complementary tool to other standard methods, such as statistical covariates, to address potential confounding by between-family factors. By evaluating whether differences between co-twins in risk or protective factors predict differences in AD symptoms, this type of design controls for all measured and unmeasured genetic and environmental influences that twin siblings share. In prior analyses of self-report alcohol measures from a population-based sample of Finnish twins (n = 3,402), we applied the co-twin comparison design to evaluate adolescent predictors of young adult alcohol use and intoxication frequency (Stephenson et al., Reference Stephenson, Barr, Ksinan, Aliev, Latvala, Viken, Rose, Kaprio, Dick and Salvatore2020). Though many risk and protective factors were related to a composite of these alcohol use behaviors in individual-level analyses, only adolescent academic achievement, substance use, and alcohol expectancies remained substantially and significantly associated with alcohol misuse in co-twin comparisons, suggesting that these predictors were robust to family-level confounds.
In the current study, we build on these prior analyses (Stephenson et al., Reference Stephenson, Barr, Ksinan, Aliev, Latvala, Viken, Rose, Kaprio, Dick and Salvatore2020) to examine the adolescent predictors of clinically significant alcohol problems, which were assessed in an intensively studied subsample of our Finnish twins in young adulthood (N = 1286 individuals from 581 complete pairs; Rose et al., Reference Rose, Salvatore, Aaltonen, Barr, Bogl, Byers, Heikkilä, Korhonen, Latvala, Palviainen, Ranjit, Whipp, Pulkkinen, Dick and Kaprio2019). Delineating the adolescent predictors of clinically significant alcohol problems is important in light of findings that alcohol use and AD clinical criteria are related but distinct phenotypes: only 1 in 10 USA adults who engage in binge drinking meet diagnostic criteria for AD (Esser et al., Reference Esser, Hedden, Kanny, Brewer, Gfroerer and Naimi2014). Twin data indicate only partially overlapping genetic influences (Dick et al., Reference Dick, Meyers, Rose, Kaprio and Kendler2011), a finding supported by genome-wide association studies on alcohol consumption and AUD (Liu et al., Reference Liu, Jiang, Wedow, Li, Brazel, Chen, Datta, Davila-Velderrain, McGuire, Tian, Zhan, Choquet, Docherty, Faul, Foerster, Fritsche, Gabrielsen, Gordon, Haessler and Vrieze2019; Walters et al., Reference Walters, Polimanti, Johnson, McClintick, Adams, Adkins, Aliev, Bacanu, Batzler, Bertelsen, Biernacka, Bigdeli, Chen, Clarke, Chou, Degenhardt, Docherty, Edwards, Fontanillas and Agrawal2018). Moreover, different patterns of adolescent predictors have emerged for heavy drinking and AD in studies conducted with samples of unrelated individuals (Merline et al., Reference Merline, Jager and Schulenberg2008), highlighting the need to elucidate pathways to AD using the co-twin comparison design. The expanded assessment protocol for the intensively studied group of FinnTwin12 participants also permitted us to examine a set of key neuropsychological and clinical psychiatric correlates of AD, which were uniquely assessed in this subsample.
To this end, we investigated a series of adolescent domains previously shown to predict young adult alcohol problems or AD, including academic achievement (Kendler et al., Reference Kendler, Ohlsson, Sundquist and Sundquist2017), substance use (Huurre et al., Reference Huurre, Lintonen, Kaprio, Pelkonen, Marttunen and Aro2010; Merline et al., Reference Merline, Jager and Schulenberg2008), externalizing problems (Edwards et al., Reference Edwards, Gardner, Hickman and Kendler2016; Merline et al., Reference Merline, Jager and Schulenberg2008), internalizing problems (Marmorstein, Reference Marmorstein2009), executive functioning (Latvala et al., Reference Latvala, Castaneda, Perälä, Saarni, Aalto-Setälä, Lönnqvist, Kaprio, Suvisaari and Tuulio-Henriksson2009; Mahmood et al., Reference Mahmood, Goldenberg, Thayer, Migliorini, Simmons and Tapert2013), peer environment (Guo et al., Reference Guo, Hawkins, Hill and Abbott2001; Huurre et al., Reference Huurre, Lintonen, Kaprio, Pelkonen, Marttunen and Aro2010), physical health (Wong et al., Reference Wong, Roberson and Dyson2015), and parent–child relationship characteristics (Donaldson et al., Reference Donaldson, Handren and Crano2016). First, we estimated the association of each adolescent domain with AD symptoms using an individual-level Poisson mixed-effects model. We then conducted co-twin comparisons to evaluate whether the magnitude of each association was attenuated after accounting for genetic and environmental influences shared by co-twins. Our preregistered hypotheses (https://osf.io/3vrn5/register/565fb3678c5e4a66b5582f67) were informed by prior work characterizing the genetic and environmental architecture of each adolescent factor and, when available, associations of each adolescent factor with alcohol misuse or problems. We expected that associations of academic achievement (Benner et al., Reference Benner, Kretsch, Harden and Crosnoe2014), externalizing problems (Edwards & Kendler, Reference Edwards and Kendler2012), physical health (Korhonen et al., Reference Korhonen, Kujala, Rose and Kaprio2009; Silventoinen et al., Reference Silventoinen, Posthuma, Lahelma, Rose and Kaprio2007), and parent–child relationship characteristics (Latendresse et al., Reference Latendresse, Rose, Viken, Pulkkinen, Kaprio and Dick2010; Savage et al., Reference Savage, Rose, Pulkkinen, Silventoinen, Korhonen, Kaprio, Gillespie and Dick2018) with AD symptoms would be significantly attenuated within the co-twin comparison design, whereas relations of alcohol expectancies (Samek et al., Reference Samek, Keyes, Iacono and McGue2013) and stressful life events (Boardman et al., Reference Boardman, Alexander and Stallings2011) with later AD would be similar across individual-level and co-twin comparison analyses. We did not forward specific hypotheses for early adolescent substance use (Do et al., Reference Do, Prom-Wormley, Eaves, Silberg, Miles and Maes2015; Irons et al., Reference Irons, Iacono and McGue2015), internalizing problems (Ehringer et al., Reference Ehringer, Rhee, Young, Corley and Hewitt2006; Savage et al., Reference Savage, Kaprio, Korhonen, Pulkkinen, Rose, Verhulst and Dick2016), executive functioning (Friedman et al., Reference Friedman, Miyake, Altamirano, Corley, Young, Rhea and Hewitt2016; Latvala et al., Reference Latvala, Tuulio-Henriksson, Dick, Vuoksimaa, Viken, Suvisaari, Kaprio and Rose2011), and features of the peer environment (Edwards et al., Reference Edwards, Maesr, Prescott and Kendler2015; Savage et al., Reference Savage, Rose, Pulkkinen, Silventoinen, Korhonen, Kaprio, Gillespie and Dick2018) due to mixed evidence from prior research.
Materials and Methods
Sample
Participants included 1035 families from FinnTwin12 (Rose et al., Reference Rose, Salvatore, Aaltonen, Barr, Bogl, Byers, Heikkilä, Korhonen, Latvala, Palviainen, Ranjit, Whipp, Pulkkinen, Dick and Kaprio2019), a longitudinal, population-based study of Finnish twins who were selected for intensive study partially on the basis of parental alcohol use (28% chosen based on parental scores on the Malmo-Modified Michigan Alcoholism Screening Test; Kristenson & Trell, Reference Kristenson and Trell1982). Adolescent predictors were from interview and questionnaire assessments at ages 12 (n = 2,070 respondents) and 14 (n = 1,852 interviews). In young adulthood (average age = 22 years, range = 20−26 years), participants completed a semistructured psychiatric assessment interview. We limited analyses to 1286 individuals (581 complete twin pairs; 42% monozygotic; and 54% female) who completed the young adult follow-up assessment. Among those interviewed at age 14, sex significantly predicted young adult participation (OR = 5.48, 95% CI [2.64, 11.36]), such that females (78% retention rate) were more likely to participate in follow-up than males (62% retention rate). Zygosity and AD symptoms at age 14 did not significantly predict study retention.
Measures
Adolescent risk and protective factors
At ages 12 and 14, twins reported on their depressive symptoms; activities; sleeping difficulties; parental autonomy granting, discipline, monitoring, tension, and warmth; time spent with parents; alcohol expectancies; and pubertal development. At age 14, participants also reported their cigarette use; daily smoking; frequency of alcohol use and intoxication; aggression; impulsivity; truancy; depression; self-esteem; social anxiety; adjustment; peer deviance, drinking, drug use, and smoking; physical health; physical activity; stressful life events; and perceived difficulty of those events. Executive functions (inhibition, set-shifting, and visuospatial ability) and DSM-III-R clinical criterion counts for AD, attention deficit hyperactivity disorder (ADHD), CD, marijuana abuse, oppositional defiant disorder (ODD), anorexia nervosa, bulimia, and overanxious disorder were also measured at age 14. Aggression, impulsivity, depression, social anxiety, and adjustment were reported by parents, teachers, classmates, and co-twins. Grade point average was reported by parents and teachers. Table 1 provides additional measurement information for each adolescent factor.
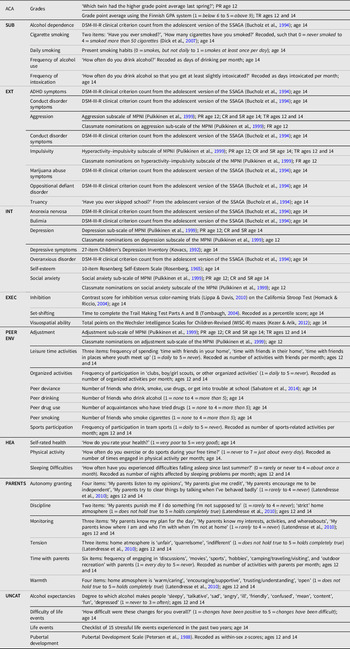
Table 1. Adolescent predictors of alcohol dependence

Note: ACA, Academic Achievement; SUB, Early Adolescent Substance Use; EXT, Externalizing Problems; INT, Internalizing Problems; EXEC, Executive Functioning; PEER ENV, Peer Environment; HEA, Physical Health; PARENTS, Relationship with Parents; UNCAT, Uncategorized Predictors; CR, co-twin-reported; FR, peer-reported; PR, parent-reported; SR, self-reported; TR, teacher-reported; DSM-III-R, Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised; MPNI, Multidimensional Peer Nomination Inventory; SSAGA, Semistructured Assessment for the Genetics of Alcoholism; WISC-R, Wechsler Intelligence Scale for Children, Revised.
Alcohol dependence symptoms
Lifetime DSM-IV AD clinical criterion counts were measured in young adulthood using the Semistructured Assessment for the Genetics of Alcoholism (SSAGA; Bucholz et al., Reference Bucholz, Cadoret, Cloninger, Dinwiddie, Hesselbrock, Nurnberger, Reich, Schmidt and Schuckit1994).
Statistical Methods
Construction of factor scores for adolescent risk and protective factors
We grouped adolescent predictors into the following domains: academic achievement, early adolescent substance use, externalizing problems, internalizing problems, executive functioning, peer environment, physical health, and relationship with parents. We performed item reduction using a split-half exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) approach, randomly selecting one twin from each pair for inclusion in each split-half. We determined the number of retained factors within each domain using parallel analysis (Horn, Reference Horn1965). We then conducted factor analysis in the first split-half using the ‘umxEFA’ function in the R {umx} package (Bates et al., Reference Bates, Maes and Neale2019), using a factor-loading cutoff of 0.30.
Next, we conducted CFAs in the first split-half using the ‘cfa’ function in the R {lavaan} package, with a comparative fit index (CFI) > 0.90 and a standardized root mean squared residual (SRMR) < 0.08 as criteria for acceptable model fit (Hu & Bentler, Reference Hu and Bentler1999). We conducted CFAs in the second split-half to confirm acceptable model fit and then used the ‘lavPredict’ function in the R {lavaan} package (Rosseel, Reference Rosseel2012) to derive factor scores for the full sample within each domain. Several variables (alcohol expectancies, life events, perceived difficulty of life events, and pubertal development) did not logically fit into the domains identified above and were examined separately (i.e., not included in item reduction).
Individual-level and co-twin analyses
First, we examined associations of each factor score with AD clinical criterion count in individual-level analyses, using a Poisson generalized linear mixed model to account for nonindependence of the data. Individual-level analyses were conducted using the R {glmmTMB} package (Brooks et al., Reference Brooks, Kristensen, Benthem, Magnusson, Berg, Nielsen, Skaug, Mächler and Bolker2017) and included sex as a covariate. We specified a separate model for each factor score to avoid potential issues with colinearity or suppression effects.
Each factor score was then examined using a twin fixed-effects model. This model examines whether differences between twins in purported risk or protective factors predict differences in AD symptoms, effectively controlling for genetic and environmental influences shared by co-twins. In the equation, Yij = βXij + γWj +αj + ϵij, the effect of the vector of within-family risk factors X on Y for twin i in family j is conditional upon a vector of covariates that vary between families (e.g., SES), W, and another vector of unmeasured fixed effects that vary between families, α, plus a random error term, ϵ ij . In a comparison of two twins, the equation could be expressed as Y2j -Y1j = (βX2j + γWj + αj + ϵ2j) – (βX1j + γWj + αj + ϵ1j) = β(X2j -X1j) + (ϵ2j–ϵ1j). The effects of all covariates that do not vary within families are, therefore, cancelled out of the model (Fitzmaurice et al., Reference Fitzmaurice, Laird and Ware2011). Fixed-effects Poisson models were estimated using the R {pglm} package (Croissant & Millo, Reference Croissant and Millo2018) and included sex as a covariate in opposite-sex twin pairs. We adopted p < .05 as the criterion for statistical significance in all analyses, given that our directional hypotheses and analytic plan were preregistered (Nosek et al., Reference Nosek, Ebersole, DeHaven and Mellor2018; Rubin, Reference Rubin2017).
Results
Adolescent Risk and Protective Factors
First, we categorized adolescent predictors into a series of domains, including academic achievement, early adolescent substance use, externalizing problems, internalizing problems, executive functioning, peer environment, physical health, and relationship with parents. We then performed item reduction using a split-half EFA and CFA approach, which involved: (1) parallel analysis to identify the number of latent factors that should be retained; (2) EFA in the first split-half sample to investigate which observed variables contributed to latent factors within each domain; (3) CFA in the first split-half sample to evaluate model fit and adjust the model specification, if needed; (4) CFA in the second split-half sample to confirm acceptable model fit; and (5) CFA in the full sample to derive factor scores. We summarize the results of these analyses by domain below. The results of parallel analysis are described in Table 2, and factor loadings for EFA in the first split-half sample can be found in the Supporting Information (Table S1). For adolescent predictors that were included in the computation of factor scores, descriptive statistics and factor loadings are shown in Table 3.
Table 2. Criteria for factor retention
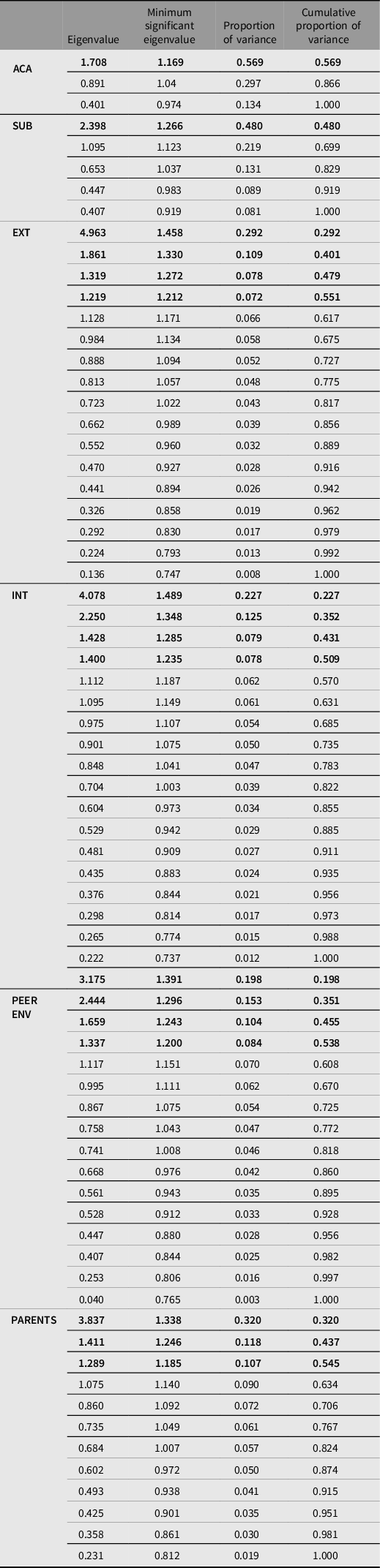
Note: Retained factors are shown in bold font. ACA, Academic Performance; SUB, Early Adolescent Substance Use; EXT, Externalizing Problems; INT, Internalizing Problems; PEER ENV, Peer Environment; PARENTS, Relationship with Parents.
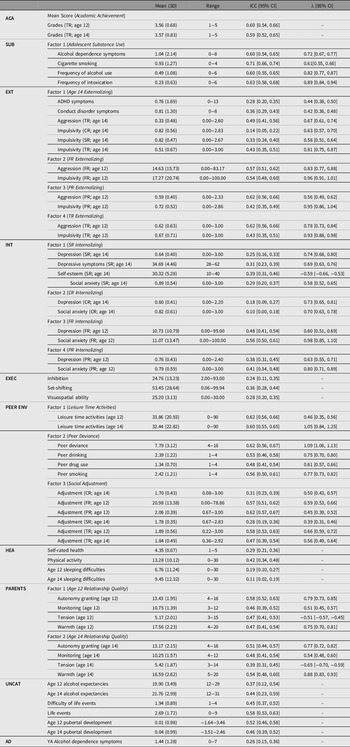
Table 3. Descriptive statistics and factor loadings for adolescent predictors and alcohol dependence outcome

Note: SD, standard deviation; ICC, sibling intra-class correlation coefficient; CI, confidence interval; ACA, Academic Achievement; SUB, Early Adolescent Substance Use; EXT, Externalizing Problems; INT, Internalizing Problems; EXEC, Executive Functioning; PEER ENV, Peer Environment; HEA, Physical Health; PARENTS, Relationship with Parents; UNCAT, Uncategorized Predictors; AD, Alcohol Dependence Outcome; CR, co-twin-reported; FR, peer-reported; PR, parent-reported; SR, self-reported; TR, teacher-reported; YA, young adult.
Academic achievement domain
Within the academic achievement domain, parent- and teacher-reported grades were included as indicators. Parallel analysis indicated that one factor should be retained (Table 2). In EFA, only teacher-reported grades at ages 12 and 14 exhibited factor loadings above 0.30. Therefore, we computed a mean score to be used in individual-level and co-twin comparison analyses.
Early adolescent substance use domain
Frequency of alcohol consumption, frequency of intoxication, AD clinical criterion count, frequency of cigarette use, and a binary measure of daily cigarette use were included as indicators. Parallel analysis indicated that one factor should be retained (Table 2); only daily smoking exhibited a factor loading below 0.30 in EFA (Table S1) and was not carried forward for subsequent analyses. CFA in the first split-half sample demonstrated acceptable model fit (CFI = 0.940, SRMR = 0.041). Therefore, we did not modify the model before conducting CFAs in the second split-half (CFI = 0.908, SRMR =0.051) and full samples (CFI = 0.970, SRMR = 0.032). Factor loadings are reported in Table 3.
Externalizing problem’s domain
Eighteen potential predictors were categorized in the externalizing problems domain. Parallel analysis indicated that four factors should be retained (Table 2). The following indicators exhibited factor loadings above 0.30 (Table S1) and were carried forward for CFA in the first split-half sample: for Factor 1, ADHD, CD, and ODD clinical criterion counts; teacher-, self-, and co-twin-reported impulsivity at age 14; and teacher-, self-, and co-twin-reported aggression at age 14; for Factor 2, peer-reported impulsivity and aggression at age 12; for Factor 3, parent-reported impulsivity and aggression at age 12; and for Factor 4, teacher-reported impulsivity and aggression at age 12. CFA in the first-split-half sample demonstrated insufficient model fit (CFI = 0.852, SRMR = 0.070). Because the 95% confidence intervals (CIs) for ODD clinical criterion count, self-reported aggression, and twin-reported aggression factor loadings overlapped 0.30, these indicators were removed from the model. CFA was repeated in the first split-half sample and demonstrated acceptable model fit (CFI = 0.918, SRMR = 0.056). Therefore, we did not further modify the model before conducting CFAs in the second split-half (CFI = 0.908, SRMR = 0.053) and full samples (CFI = 0.909, SRMR = 0.048). Indicators included in the computation of factor scores are shown in Table 3.
Internalizing problem’s domain
Eighteen potential predictors were categorized in the internalizing problems domain. Parallel analysis indicated that four factors should be retained (Table 2). The following indicators exhibited factor loadings above 0.30 (Table S1) and were carried forward for CFA in the first split-half sample: for Factor 1, overanxious disorder clinical criterion count; depressive symptoms at ages 12 and 14; self-esteem; and social anxiety; for Factor 2, co-twin-reported depression and social anxiety; for Factor 3, peer- and teacher-reported depression and social anxiety; and for Factor 4, parent-reported depression and social anxiety. CFA in the first split-half sample yielded unacceptable model fit (CFI = 0.760, SRMR = 0.070). In a series of model modifications, overanxious disorder clinical criterion count, teacher-reported depression and social anxiety, and self-reported depressive symptoms at age 12 demonstrated the lowest factor loadings and were removed from the model. After these modifications, CFA in the first split-half (CFI = 0.919, SRMR = 0.050), second split-half (CFI = 0.928, SRMR = 0.038), and full samples (CFI = 0.926, SRMR = 0.039) demonstrated satisfactory model fit. Indicators included in the computation of factor scores are shown in Table 3.
Executive functioning domain
Inhibition, set-shifting, and visuospatial ability at age 14 were included as indicators within the executive functioning domain. However, in light of low inter-item correlations, each variable was examined separately in individual-level and co-twin comparison analyses.
Peer environment domain
Sixteen potential predictors were categorized in the peer environment domain. Parallel analysis indicated that four factors should be retained (Table 2). The following indicators exhibited factor loadings above 0.30 (Table S1) and were carried forward for CFA in the first split-half sample: for Factor 1, leisure time activities at ages 12 and 14; for Factor 2, peer deviance, drinking, drug use, and smoking; for Factor 3, parent-, peer-, self-, teacher-, and co-twin-reported social adjustment; and for Factor 4, sports involvement at ages 12 and 14. However, when CFA was conducted in the first split-half sample, factor loadings for Factor 4 were not statistically significant. Therefore, CFA was repeated in the first split-half sample with the first three latent factors and demonstrated acceptable model fit (CFI = 0.922, SRMR = 0.058). We did not further modify the model before conducting CFAs in the second split-half (CFI = 0.927, SRMR =0.059) and full samples (CFI = 0.920, SRMR = 0.054). Indicators included in the computation of factor scores are shown in Table 3.
Physical health domain
Physical activity, self-rated health, and sleeping difficulties were included as indicators in the physical health domain. However, in light of low inter-item correlations, each variable was examined separately in individual-level and co-twin comparison analyses.
Relationship with parent’s domain
Twelve potential predictors were categorized in the relationship with parent’s domain. Parallel analysis indicated that three factors should be retained (Table 2). The following indicators exhibited factor loadings above 0.30 (Table S1) and were carried forward for CFA in the first split-half sample: for Factor 1, parental autonomy granting, monitoring, warmth, and tension at age 12; for Factor 2, parental autonomy granting, monitoring, warmth, and tension at age 14; and for Factor 3, parental discipline at ages 12 and 14. Though CFA in the first split-half sample demonstrated acceptable model fit (CFI = 0.906, SRMR = 0.051), factor loadings for Factor 3 were not statistically significant when CFA was conducted in the second split-half sample. Therefore, CFA was repeated in the second split-half sample with the first two latent factors and exhibited satisfactory model fit (CFI = 0.914, SRMR = 0.053). We did not further modify the model before conducting CFA in the full sample (CFI = 0.932, SRMR = 0.047). Indicators included in the computation of factor scores are shown in Table 3.
Individual-Level and Co-Twin Comparison Analyses
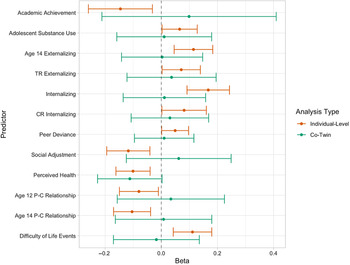
Because individual-level and co-twin comparison analyses employed a Poisson distribution, we first evaluated evidence for overdispersion. The dispersion ratio ranged from 0.663 to 0.823 across the models tested, suggesting that a Poisson model provided an appropriate fit to the data. Results for individual-level and co-twin Poisson regression analyses are shown by domain in Table 4, and statistically significant effects from individual-level analyses are reviewed in Figure 1. In individual-level analyses, adolescents with higher levels of substance use, teacher-reported externalizing problems at age 12, externalizing problems at age 14, self- and co-twin-reported internalizing problems, peer deviance, and perceived difficulty of life events reported more symptoms of AD in young adulthood. Conversely, individuals with higher academic achievement, social adjustment, self-rated health, and parent–child relationship quality at ages 12 and 14 met fewer AD clinical criteria. Peer- and parent-reported externalizing problems, peer- and parent-reported internalizing problems, inhibition, set-shifting, visuospatial ability, leisure time activities, physical activity, sleeping difficulties, alcohol expectancies, pubertal development, and stressful life events in adolescence were not related to lifetime AD clinical criterion count.
Table 4. Results for individual-level and co-twin comparison analyses

Note: ACA, Academic Achievement; SUB, Early Adolescent Substance Use; EXT, Externalizing Problems; INT, Internalizing Problems; EXEC, Executive Functioning; PEER ENV, Peer Environment; HEA, Physical Health; PARENTS, Relationship with Parents; UNCAT, Uncategorized Predictors; CR, co-twin-reported; FR, peer-reported; PR, parent-reported; SR, self-reported; TR, teacher-reported; *p < .05.

Fig. 1. Examining adolescent predictors of AD symptoms in individual-level and co-twin analyses
Note: Error bars denote 95% confidence intervals of estimates. TR, teacher-reported; CR, co-twin-reported; P–C, parent–child.
When statistically significant predictors from individual-level analyses were examined within the co-twin comparison design, the CIs for these associations were larger and included zero (Table 4). To evaluate whether individual-level estimates were substantially attenuated within the co-twin comparison design, we first considered whether the co-twin comparison estimate was contained within the 95% CI of the individual-level estimate and, second, conducted a series of z tests to empirically examine whether these nominal differences were statistically significant (p < 0.05). As shown in Figure 1, point estimates appeared to be attenuated for academic achievement (z = 1.45, p = .07), age 14 externalizing problems (z = 1.37, p = .09), self-reported internalizing problems (z = 1.85, p = .03), social adjustment (z = 1.74, p = .04), parent–child relationship characteristics at ages 12 (z = 1.10, p = .14) and 14 (z = 1.19, p = .12), and perceived difficulty of life events (z = 1.50, p = .07), as the beta estimates from co-twin comparison analyses were not contained within the 95% CIs of the individual-level estimates. However, z tests, which account for larger standard errors within the co-twin comparison design, demonstrated that individual-level associations were significantly reduced for self-reported internalizing problems and social adjustment only. Conversely, the beta estimates from co-twin comparisons of adolescent substance use (z = 0.60, p = .28), teacher-reported externalizing problems (z = 0.39, p = .35), co-twin-reported internalizing problems (z = 0.62, p = .27), peer deviance (z = 0.66, p = .25), and self-rated health (z = 0.17, p = .57) were contained within the 95% CIs of the individual-level estimates. The corresponding z tests similarly indicated no statistically significant differences between the estimates from the individual-level and co-twin comparison analyses.
Discussion
The current study used a co-twin comparison design to evaluate prospective predictors of AD symptoms. In individual-level analyses, we replicated many well-known adolescent correlates of later AD. Specifically, we found that higher levels of adolescent substance use, teacher-reported externalizing problems at age 12, externalizing problems at age 14, self- and co-twin-reported internalizing problems, peer deviance, and perceived difficulty of life events were associated with more AD symptoms by young adulthood. On the other hand, individuals with higher academic achievement, social adjustment, self-rated health, and parent–child relationship quality met fewer AD clinical criteria. These findings are consistent with prior studies demonstrating the relevance of individual characteristics, features of the parent–child relationship, and characteristics of the social environment to the development of alcohol problems by young adulthood (Edwards et al., Reference Edwards, Gardner, Hickman and Kendler2016; Maggs et al., Reference Maggs, Patrick and Feinstein2008; Merline et al., Reference Merline, Jager and Schulenberg2008).
In addition to individual-level analyses, we also examined the contribution of each adolescent factor to young adult AD using the co-twin comparison design, which evaluates whether differences between twins in adolescence predict differences in their young adult AD symptoms after accounting for genetic and environmental influences that twin siblings share. Though a number of adolescent factors were associated with AD symptoms in individual-level analyses, we found that differences between twins in adolescence were not related to within-pair differences in AD symptoms. One possible explanation for this pattern of statistically nonsignificant associations within the co-twin comparison design is that relations between adolescent factors and later alcohol problems are confounded by factors that vary between families, such as SES, neighborhood characteristics, or familial genetic load. However, it is also plausible that we did not have sufficient power to detect significant associations in co-twin comparison analyses. Indeed, though point estimates were reduced after controlling for genetic and environmental influences that twin siblings share, the individual-level beta estimates for adolescent substance use, externalizing problems, co-twin-reported internalizing problems, peer deviance, perceived difficulty of life events, academic achievement, self-rated health, and parent–child relationship quality were not statistically significantly attenuated within the co-twin comparison design. Furthermore, the magnitude of the association between self-rated health and AD symptoms was larger within the co-twin comparison design than in individual-level analyses, though the point estimate had a larger standard error within co-twin comparisons, which use the twin pair as the unit of analysis. This suggests that associations with each of these adolescent factors may remain relevant after accounting for family-level influences, though they did not reach conventional significance thresholds.
These results should be considered in light of several limitations. First, the co-twin comparison design controls for genetic and environmental influences that twin siblings share but does not account for potential confounding by unmeasured individual-level characteristics (e.g., one co-twin’s affiliation with a deviant peer group). Second, co-twin comparisons compound measurement error (McGue et al., Reference McGue, Osler and Christensen2010) and effectively reduce sample size using the twin pair as the unit of analysis (Boardman & Fletcher, Reference Boardman and Fletcher2015), which yields increased risk for Type II error when compared to individual-level analyses. For this reason, we focused our inferences on whether the magnitude of the effect sizes changed across the individual-level and co-twin comparison methods rather than on statistical significance within the co-twin design.
Our study has some notable strengths, as well. We assessed a population-based sample of all twins born over a 5-year period in Finland, with no selection based on sociodemographic factors or place of residence. Only Swedish-speaking families were excluded from this intensively studied cohort, given the extra cost of translation and interviewer training in a second language. Data were gathered from multiple reporters, including co-twins, parents, peers and teachers, as well as from the twins themselves. Finally, the longitudinal nature of the study is a notable strength: we collected information on social, behavioral, and psychiatric factors at ages 12 and 14 when alcohol-related problems are quite rare and infrequent.
In summary, the current study illustrates the utility of co-twin comparisons for understanding pathways to alcohol problems by young adulthood. The co-twin comparison design controls for genetic and environmental influences that twin siblings share; thus, relative to a study of singletons, co-twin comparisons strengthen inferences about whether purported adolescent risk factors are predictive above and beyond these confounding familial factors. Our findings highlight academic achievement, externalizing and internalizing problems, substance use, parent–child relationship characteristics, self-rated health, and features of the peer environment as predictors of AD. Moreover, the associations between adolescent substance use, teacher-reported externalizing problems, co-twin-reported internalizing problems, peer deviance, self-rated health, and AD symptoms were of a similar magnitude in co-twin comparisons. Ultimately, we hope that results from this study can inform preventive intervention efforts by refining our understanding of the nature of associations between a host of commonly studied risk factors and the development of alcohol problems.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/thg.2021.36.
Funding
This work was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under award numbers R01AA012502, R01AA015416, K02AA018755, and K01AA024152; and the Academy of Finland (grants 100499, 205585, 118555, 141054, 265240, 263278, and 264146). JK and AL have been supported by the Academy of Finland (grants 265240, 263278, 308248, and 312073 to JK; grants 308698 and 314196 to AL). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Conflict of Interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.