The diagnosis of personality disorder covers a wide range of conditions with disparate presentations. Given the plurality of approaches, the limited evidence base and the overlap between models, choosing an approach is difficult. In response to this, the National Personality Disorder Development Programme undertook an evaluation of 11 pilot community personality disorder services. The evaluation found widespread agreement about the principles that should underpin service delivery, including the need for ‘open communication, explicit boundaries [and a] consistent theoretical model’. Reference Crawford1
Among presentations, the poor impulse control, self-harm and aggression to other people that characterise cluster B personality types (dramatic, emotional, erratic) are highlighted as major burdens to psychiatric settings. 2,Reference Bender, Dolan, Skodol, Sanislow, Dyck and McGlashan3 A high rate of acute in-patient admission is further associated with a high incidence of suicide among people with borderline personality disorder, estimated at 10%. Reference Schneider, Schnabel, Wetterling, Bartusch, Weber and Georgi4 Partial hospitalisation over a 5-day week with a mentalisation-based treatment (MBT) approach to care has been shown to decrease this burden, reducing the duration of in-patient care among patients with borderline personality disorder, Reference Bateman and Fonagy5 in addition to a reduction in rates of self-harm and suicidality. Reference Bateman and Fonagy6,Reference Bateman and Fonagy7 The provision of inexpensive open-access service user network (SUN) groups has also demonstrated effectiveness in reducing emergency department attendance among patients with personality disorder. Reference Miller and Crawford8
A working party survey of the London Borough of Croydon previously highlighted the need for service development geared towards intervention for people with personality disorder, with an estimated 4000 people having a diagnosis of personality disorder 9 but with no access to a specialist intervention. In a departure from existing specialist personality disorder service models, the new specialist service proposed to use both MBT and SUN models of care, each consistent and explicit in the theoretical approach, and with the combined approach then catering for a wider population of patients than could be reached by either model alone. This ‘inter-digitation’ of the two models offered an acceptable balance of catering for a large number of patients and offering a specific, evidence-based intervention for patients exhibiting borderline pathology.
The construction gave rise to three subgroups of patients. Patients offered a place on either of the two MBT programmes (2-day or 3-day) exhibited borderline pathology at clinical assessment, with confirmation of the diagnosis of borderline personality disorder through subsequent Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) assessment (Table 1). Both MBT programmes adopted therapeutic community principles comprising individual and group therapy but differed in the frequency of individual therapy, community meetings and creative structures. The patients with greater disturbance (in terms of self-harm and service use) were offered a place on the 3-day programme, with weekly individual sessions, while the patients on the 2-day programme were offered individual sessions every 2 weeks.
TABLE 1 Demographic and diagnostic data for the whole sample
| SUN group (n = 41) |
2-day MBT programme (n = 16) |
3-day MBT programme (n = 15) |
Total (n = 72) | |
|---|---|---|---|---|
| Age, years: mean (s.d.) | 42 (12.97) | 40 (10) | 35 (11.39) | 39 (12.30) |
| Gender, % (n) | ||||
| Male | 31.7 (13) | 31.25 (5) | 0 (0) | 25 (18) |
| Female | 68.3 (28) | 68.75 (11) | 100 (15) | 75 (54) |
| Ethnic origin, % (n) | ||||
| White | 82.9 (34)87.5 (14) | 93.3 (14) | 86.11 (62) | |
| Black | 0 (0) | 6.25 (1) | 0 (0) | 1.39 (1) |
| Mixed race | 2.4 (1) | 6.25 (1) | 6.67 (1) | 4.17 (3) |
| Other | 14.6 (6) | 0 (0) | 0 (0) | 8.33 (6) |
| SCID-II categories, n: mean (s.d., range) | 3.31 (2.18, 0-8) | 3.57 (1.6, 1-7) | 3.43 (1.91, 0-8) | |
| SAPAS score (threshold 3), mean (s.d., range) | 5.18 (0.85, 4-7) | 5.18 (0.85, 4-7) |
MBT, mentalisation-based therapy; SAPAS: Standardised Assessment of Personality – Abbreviated Scale; SCID, Structured Clinical Interview for DSM-IV Axis II Personality Disorders; SUN, service user network.
The SUN project offered open access to four groups per week, using therapeutic community principles alongside coping process and psychoanalytical theories, but catering for a wider range of personality disorder subtypes. Patients in the MBT programme could also access the SUN project if they wished, to varying degrees (Fig. 1). The process of service development has been described fully elsewhere. Reference Jones and Miller10 Briefly, patients presenting at assessment and exhibiting borderline pathology, assessed as having a ‘mentalising deficit’ and viewed by the assessing pair as potentially being able to make use of MBT were offered a place on the MBT day programme. Patients who declined the offer of the MBT programme and self-presented without referral were thought either to not exhibit borderline pathology or to be too disordered in their functioning and were signposted to the open-access SUN project.
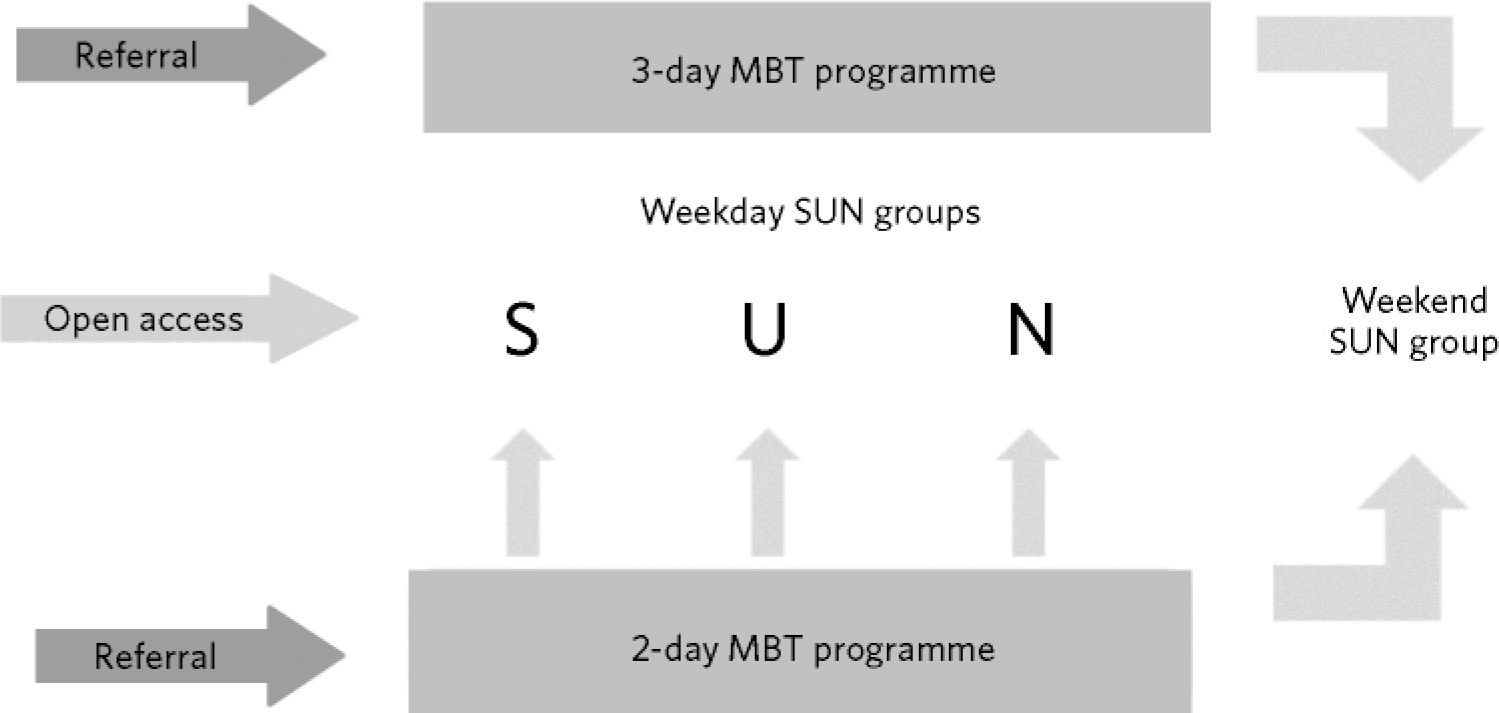
FIG. 1 Service structure.
MBT, mentalisation-based therapy; SUN, service user network.
This article focuses on the impact of the new service on psychiatric bed use for all patients receiving an intervention.
Method
Two methods were used to clarify the presence of personality disorder: (a) the diagnosis was ascertained by a single rater using SCID-II on entry of patients into either arm of the 18-month MBT programme; and (b) as the open-access, open-ended nature of the SUN project did not allow for the same diagnostic measure, the Standardised Assessment of Personality – Abbreviated Scale (SAPAS) was sent to every member who attended the SUN project as a result of an initial leafleting exercise aimed at attracting potential members. The SAPAS is a validated eight-item self-report questionnaire with established psychometric properties, where a cut-off score of 3 or more indicates the likely presence of a personality disorder. Reference Moran, Leese, Lee, Walters, Thornicroft and Mann11
At the point of study, all patients reaching 6 months or more across the three treatment groups were identified (n = 72). As a subset, patients reaching at least 12 months of treatment in each of the three groups were also identified (n = 41). All patients reaching 6 months and 12 months of intervention were included. Patients who dropped out of MBT before 6 months (n = 10) or before 12 months (n =5) were not included in the relevant part of the audit. The open-access policy of the SUN project meant every patient retained access to the groups once membership had been granted, so all SUN members were included in the sample, irrespective of attendance rates. Demographic data and durations of psychiatric in-patient stays (bed days) were collected using the electronic patient record system of patients’ case notes.
Data analysis was carried out using SPSS version 17 for Windows. We used two-tailed non-parametric statistical tests throughout because of the uncertain direction of change in the early stages of treatment and the positively skewed distribution of the data on bed days. The within-group statistical significance of changes in bed usage between 6 months and 12 months before treatment and 6 months and 12 months after starting treatment was determined using the paired-samples Wilcoxon signed-ranks test. The three treatment groups were compared with regard to the 6 months before treatment and the 6 months after starting treatment period, and the 12 months before treatment and the 12 months after starting treatment, using the Mann-Whitney U-test. Patients attending both the SUN project and either of the MBT programmes (n = 12) were excluded from SUN/MBT between-groups analysis; the majority of these patients (n = 10) were from the 2-day MBT programme.
Sample description
The sample characteristics are shown in Table 1.
An overrepresentation of women was found across treatment groups, but the age range of patients presenting appeared similar across groups. Black and minority ethnic patients were underrepresented across groups compared with the borough's demographic data. 12 For patients attending the 2-day and 3-day MBT programmes, most met threshold criteria for numerous personality disorder diagnoses, and 86% met criteria for borderline personality disorder.
Of the patients attending the MBT programmes (including those who subsequently dropped out), 91.7% met SCID-II threshold criteria for at least one category of personality disorder. The remaining patients exhibited borderline traits that did not meet diagnostic threshold. The majority of patients typically met criteria for a combination of three categories. Alongside borderline personality disorder, the two most common SCID-II diagnostic categories were avoidant personality disorder and paranoid personality disorder. The combination of these three subcategories was particularly evident among patients on the 3-day MBT programme. By comparison, more patients on the 2-day MBT programme met diagnostic threshold for the obsessive-compulsive and antisocial subcategories alongside borderline personality disorder.
Of the 53.7% of patients attending the SUN project who returned the SAPAS questionnaire, 100% scored positive for three or more criteria, indicating that the diagnosis of personality disorder was likely.
Results
Whole service impact
A Wilcoxon signed-ranks test showed that overall bed use reduced dramatically after starting treatment. The number of bed days in the 6 months before treatment was significantly greater than the number of bed days in the 6 months after starting treatment. The number of bed days used by patients in the 12 months before treatment was also significantly greater than the number of bed days used in the 12 months after starting treatment (Fig. 2 and Table 2).
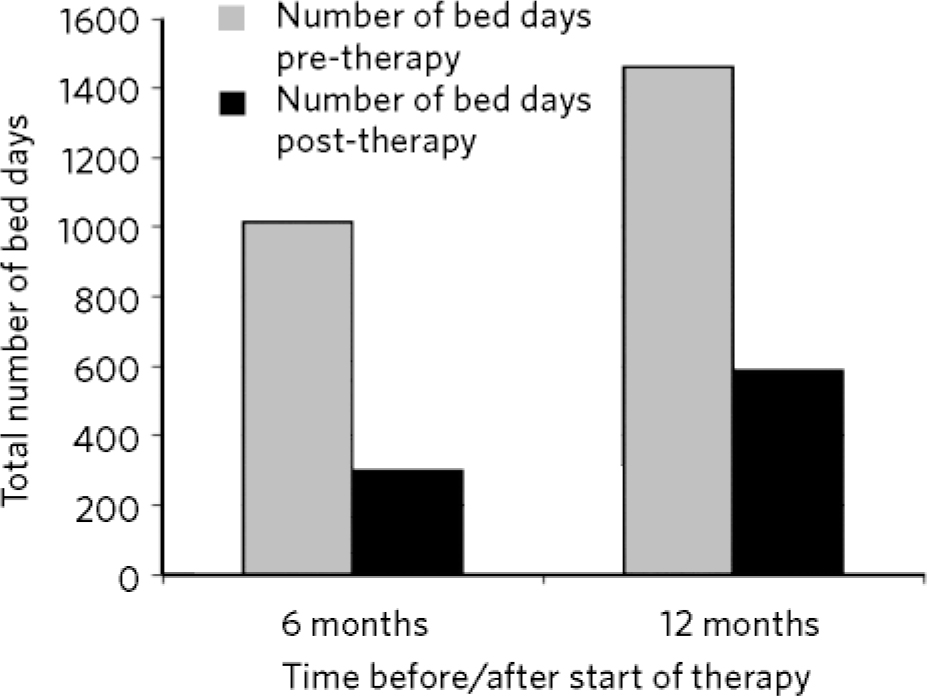
FIG. 2 Total bed days 6 months and 12 months before and after start of therapy.
TABLE 2 Changes in bed use across the whole sample
| Overall service evaluation | Bed days before treatment |
Bed days after treatment |
Wilcoxon signed-ranks test | ||
|---|---|---|---|---|---|
| z-score | P | Effect size (r) | |||
| 6 months (n = 72) | |||||
| Total | 1014 | 299 | –3.522 | <0.001* | –0.415 |
| Mean | 14.08 | 4.15 | |||
| s.d. | 29.12 | 10.12 | |||
| Median | 0 | 0 | |||
| IQR | 17 | 3.5 | |||
| 12 months (n = 41) | |||||
| Total | 1460 | 588 | –2.483 | 0.013Footnote * | –0.293 |
| Mean | 35.61 | 14.34 | |||
| s.d. | 67.46 | 35.09 | |||
| Median | 0 | 0 | |||
| IQR | 55.5 | 9 | |||
IQR, interquartile range.
* Indicates a result of statistical significance at the 95% confidence interval.
Within-group analysis
2-day MBT programme
Wilcoxon signed-ranks tests showed that bed use in the 6 months before treatment (median 0, interquartile range (IQR) 5.5) did not differ significantly from bed use in the 6 months after starting treatment (median 0, IQR = 6.5) among the 2-day MBT programme attendees (z = –0.169, P = 0.866, r=–0.042). Similarly, bed use in the 12 months before treatment (median 3, IQR = 111) did not differ significantly from bed use in the 12 months after starting treatment (median 7, IQR = 30, z = –1.069, P = 0.285, r = –0.404).
3-day MBT programme
Bed use in the 6 months before treatment (median 12, IQR = 60) differed significantly from bed use in the 6 months after starting treatment (median 0, IQR = 4) among the 3-day MBT programme attendees (z = –2.667, P = 0.008, r = –0.689). This finding corroborated the initial clinical assessment of high service use among this group of patients and highlighted the impact of treatment on bed use. However, bed use in the 12 months after starting treatment (median 13, IQR = 57) did not differ significantly from bed use in the 12 months before treatment (median 55, IQR = 97.5, z = –1.461, P = 0.144, r = –0.731).
SUN project
A statistically significant reduction in bed use was found when comparing the 6 months after starting SUN (median 0, IQR = 0.5) with the 6 months before joining the programme (median 0, IQR = 10, z = –2.580, P = 0.01, r = –0.403). The same median values highlight the skewed nature of the data and the fact that a small number of patients account for the majority of bed days. Bed use in the 12 months before starting the SUN project (median 0, IQR = 0) did not differ significantly from bed use in the 12 months after starting treatment (median 0, IQR = 0, z = –1.600, P = 0.11, r = –0.292).
Between-group analysis
SUN versus MBT
The Mann-Whitney U-test showed that during the 6 months before treatment, patients attending SUN (median 0, IQR = 5) did not differ significantly in use of psychiatric beds from the patients attending either of the MBT programmes (median 8, IQR = 54, U = 216.00, P = 0.053, r = –0.274). The number of bed days used by SUN attendees 6 months after starting treatment (median 0, IQR = 0) continued to differ insignificantly from the number of bed days used by patients in the MBT programmes (median 0, IQR = 4, U = 248.00, P = 0.169, r = –0.194). A significant difference was found, however, when comparing SUN bed use at 12 months after starting treatment (median 0, IQR = 0) with bed use among the combined MBT group (median 3, IQR = 17). It must be noted that the between-group sample size after excluding patients attending both SUN and MBT was very small for the MBT group (n =5) compared with the SUN group (n = 21) 12 months after starting treatment.
MBT groups
A comparison between the two MBT programmes revealed that bed use by patients on the 3-day programme (median 0, IQR = 4) differed insignificantly from bed use in the 2-day programme (median 0, IQR = 6.5) 6 months after starting treatment (U = 114.50, P = 0.799, r = –0.046). In contrast, bed use by patients on the 3-day programme (median 12, IQR = 60) was significantly greater than bed use by patients on the 2-day programme (median 0, IQR = 5.5, U =69, P = 0.025) 6 months before treatment. Bed use by patients on the 3-day programme (median 13, IQR = 57) was not significantly different from bed use by patients on the 2-day programme (median 13, IQR = 57) 12 months after starting treatment – that is, bed use by patients in the two groups became increasingly similar as treatment progressed.
Alongside the reduction of in-patient bed days across the whole sample, no completed suicidal acts were recorded during the year-long study period.
Discussion
This audit suggests that a two-model specialist personality disorder service had a significant impact on psychiatric bed use 6 months after starting treatment, with a reduction in use highlighted. This effect was maintained 12 months after starting treatment. It has been argued that the apparent improvement in prognosis in borderline personality disorder over the past few decades reflects, in part, shorter hospitalisations. Reference Fonagy and Bateman13 Given the 86% overall treatment retention rate at 6 months, the 88% overall retention rate at 12 months, and the fact that no completed suicides occurred within the context of reducing the duration of hospitalisation, the link to improved prognosis appears to find support in our results. This echoes similar findings of reduced in-patient stays from naturalistic studies undertaken by other community personality disorder services. Reference Pretorius, Albeniz and Broom14 The demographic data suggest that Black and minority ethnic patients are less likely to access the service. In part, this may be explained by bias in the referral pathway to the MBT programme, although the fact that the SUN project is open access suggests additional cultural differences.
Analysis of changes within each treatment group shows a large effect size of the 3-day MBT programme (r = –0.731) when comparing the 12 months before and after starting treatment, which differed little from the corresponding comparison of the 6 months before and after starting treatment (r = –0.689), which was found to be highly significant. This suggests that the insignificant change in bed days for the analysis at 12 months might also reach significance if a larger sample size were used.
By contrast, analysis of the 2-day MBT programme does not reach significance in the same way as the 3-day MBT programme at 6 months of treatment. The effect size is negligible when comparing the 6 months before and after starting treatment (r = –0.042) for the 2-day MBT programme. When comparing the 12 months before and after starting treatment, the effect size is medium (r = –0.404), but without reaching statistical significance. Again, this may reflect a small sample size and the need for further data collection.
That no significant reduction in bed use was found specifically within the 2-day MBT programme at 6 months may reflect a differing sample population compared with the 3-day MBT programme. The apparent variation in SCID-II comorbidity between these groups is in keeping with this suggestion, as is the initial difference highlighted through the clinical allocation process. Subsequent differences in treatment ‘doses’ may further account for this finding. It would appear that treatment has little impact on bed use during the first 6 months within the 2-day MBT group, whereas within the 3-day MBT programme there exists a dramatic reduction in bed use in the first 6 months, such that bed use by the two groups becomes increasingly similar over time.
Analysis of the SUN project at 6 months before and after treatment highlighted a significant reduction in bed use, with a medium effect size (r = –0.403). At 12 months, however, the significance is absent and the effect size is reduced (r = –0.292). It appears that the greatest effect in reduction of bed use is achieved within the first 6 months of SUN attendance. Further data collection at 12 months is required to ascertain whether a significant effect remains. Although a significant difference was obtained when comparing SUN and the combined MBT sample on bed use at 12 months after starting treatment (excluding patients attending both SUN and MBT), the results should be interpreted with caution. A very small remaining sample size may not represent the wider sample at this stage, and therefore further study with a larger sample size is indicated.
Finally, the diagnostic profile of the SUN sample in this study is reflective of a similar finding in a previous study, in which over 91% of patients scored three or more points on the Standardised Assessment of Personality (SAP) in the 44% of the sample returning the SAP questionnaire. Reference Miller and Crawford8 Our clinical knowledge of the remaining patients not returning the SAPAS leads us to suggest that they are at least as likely to meet the threshold for the diagnosis of personality disorder. We must concede, however, that the robustness of the diagnosis is less in the SUN sample than in the MBT samples, where the SCID-II was formally conducted. A further study is planned and will entail the administration of the SAPAS screening tool to all groups of patients, irrespective of subsequent administration of the SCID-II, to afford greater comparability between patient groups.
There are a number of limitations to this study, including the lack of a control group, without which no definitive statement about the effectiveness of the three interventions offered can be stated. Randomisation to specific intervention groups was not conducted. Some very small post-treatment sample sizes, particularly with the MBT sample, may have reduced the ability of the analyses to reach significance. There exists no control group against which to compare the size of reduction in bed use. A remaining question exists regarding whether reduction in bed use is maintained once the 18-month MBT treatment is completed and indeed whether reduction is linked to frequency of attendance. These three facets indicate the need for further study.
With that caveat, and given the current zeitgeist for cost savings, the suggestion that a cheap, open-access, community-based intervention offers the prospect of significantly reducing psychiatric bed use by 6 months (comparable to the reduction afforded by an MBT programme) warrants ongoing investigation.







eLetters
No eLetters have been published for this article.