Research shows that actively assessing and addressing patient-rated unmet needs is a useful starting point for healthcare delivery.Reference Salvi, Leese and Slade1,Reference Slade, Leese, Cahill, Thornicroft and Kuipers2 The Camberwell Assessment of Need (CAN) questionnaire is the most widely used needs-assessment tool.Reference Wennström, Sörbom and Wiesel3 We searched the PubMed, PsycINFO and PsycARTICLES databases for publications on CAN using the following terms: addiction, drug dependence, heroin AND methadone; the search yielded only four studies, conducted primarily in mental healthcare systems.Reference Baksheev, Thomas and Ogloff4–Reference Van Vugt, Kroon, Delespaul, Dreef, Nugter and Roosenschoon7 Nevertheless, surveys using non-standardised assessments have found high levels of unmet needs, particularly legal, basic, financial, family, social services, medical and mental healthcare, in addiction patient groups.Reference Pringle, Emptage and Hubbard8–Reference Etheridge, Craddock, Dunteman and Hubbard11 Unmet need is a predictor of perceived quality of care; therefore, enhancing patients’ access to services that meet their additional needs promotes treatment engagement and outcomes.Reference Pringle, Emptage and Hubbard8–Reference Joe, Simpson and Sells10,Reference Asche and Harrison12 Most opioid-dependent individuals manifest ongoing polysubstance use, have related complex needs, and present major treatment challenges because no single treatment service is likely to meet all their needs.Reference Etheridge, Craddock, Dunteman and Hubbard11,Reference Kumar and Rajwal13 The levels of unmet need for specific ancillary services during intensive specialised care such as methadone maintenance treatment (MMT) programmes are unclear.Reference Pringle, Emptage and Hubbard8
Benzodiazepine use is a major public health problem. Lifetime use of benzodiazepines among opioid-dependent individuals is reported to be 66–100%, with estimates of problematic benzodiazepine misuse or dependence in people on MMT being 18–50%.Reference Lintzeris and Nielsen14 Research indicates that benzodiazepine misuse or dependence is associated with complex needs and negatively influences MMT outcomes.Reference Darke, Swift, Hall and Ross15–Reference Maremmani and Shinderman19 There are many reasons why patients on MMT use benzodiazepines. Benzodiazepine misuse may signify a desire for drug experience no longer achieved by opioids due to greater tolerance and methadone-induced narcotic blockade.Reference Maremmani and Shinderman19 Benzodiazepine misuse may also represent an attempt to negate the increasing tolerance to opioids by accessing other drugs that provide alternative rewarding effects.Reference Maremmani and Shinderman19,Reference Fatséas, Lavie, Denis and Auriacombe20 Compared with patients on MMT who do not use benzodiazepines, patients on MMT who use benzodiazepines manifest higher levels of polysubstance use (heroin, cocaine), higher levels of psychopathology (including depression and anxiety), poorer social functioning (including unemployment and criminal activity), higher levels of injecting practices that carry a blood-borne virus risk, and greater overdose history. In addition, patients on MMT who use benzodiazepines often receive higher methadone doses than those who do not use benzodiazepines.Reference Lintzeris and Nielsen14–Reference Maremmani and Shinderman19
In addition to morbidity, benzodiazepine misuse and dependence is implicated in 20–80% of methadone-related deaths.Reference Lintzeris and Nielsen14
In this study, we examined MMT patients’ perceptions of unmet needs for comprehensive treatment care and explored the relationship between benzodiazepine misuse and severity of need. Our hypothesis was that use of non-prescribed benzodiazepines would be associated with a higher severity of unmet needs.
Method
The Research Ethics Committee of the Drug Treatment Centre Board in Dublin approved the study. This is the oldest, largest addiction treatment centre in Ireland, providing a broad range of out-patient treatments, including specialist psychiatric, psychological, social and medical interventions. Only service users who were opioid-dependent and who had received MMT for at least 3 months were eligible for inclusion in the survey. Service users with acute or end-stage medical problems (e.g. AIDS) were excluded. To maximise participation, all eligible service users were sent a personal letter explaining the study and inviting them to participate. Service users who did not respond to this letter were approached personally and verbally invited to participate.
Sociodemographic data and information on substances used in the 30 days preceding the study were obtained using the appropriate section of the Maudsley Addiction Profile. Each respondent completed the Camberwell Assessment of Need Short Appraisal Schedule, patient-rated version (CANSAS-P). This tool was chosen because of its good psychometric properties. The CANSAS-P exhibits comparable detection of needs with the Camberwell Assessment of Need Short Appraisal Schedule (CANSAS), good reliability and validity, especially for unmet needs. The CANSAS-P is better at identifying the needs that patients are less likely to admit to on CANSAS, and is generally positively evaluated by patients.Reference Trauer, Tobias and Slade21 Slade and colleagues asserted that patient ratings of need are more reliable than staff ratings.Reference Slade, Leese, Taylor and Thornicroft22 The CANSAS-P assesses need on 22 items. The rater indicates any perceived need and determines whether this need is being met (0 = no need; 1 = not a serious problem because of help received, i.e. met need; 2 = current serious problem despite help received, i.e. unmet need). The CANSAS-P provides scores on total needs, unmet needs and met needs; higher scores indicate higher severity of need.Reference Slade, Phelan, Thornicroft and Parkman23 For the purpose of this study, only information about perceived need and whether it was met or unmet was used.
Statistical analysis
Descriptive data are presented as percentages and means. Comparisons were made between benzodiazepine users’ and non-users’ ratings of need. In the absence of any study using CANSAS in the opioid-dependent groups, we estimated that the mean unmet need would be 5, based on studies in mental healthcare, and considered that a difference of 2 between benzodiazepine users and non-users would be clinically meaningful.Reference Boardman, Hodgson, Lewis and Allen24 With the expected standard deviation (s.d.) of 3.0, we required 102 participants to have 90% power to detect such difference, with a P-value of 0.05. Categorical variables were analysed using the Pearson x03C7;2 test for independence, and group differences for continuous variables were analysed using the independent t-test. Linear regression ‘enter’ method analysis was used to test the predictive ability of benzodiazepine misuse on the severity of needs, while controlling for polysubstance use in the multivariable analysis. All analyses were carried out using PASW version 18.0 (SPSS Inc, Chicago, Illinois, USA, 2009; www.spss.com).
Results
A total of 191 eligible patients were invited to participate in the study. Of these, 107 agreed to participate (response rate 56%). Non-responders either actively declined to participate (n = 43), failed to respond to verbal and written invitations to participate (n = 38), had time constraints preventing them meeting with the researchers (n = 1), died (n = 1) or were acutely psychiatrically unwell during the survey period (n = 1). No significant difference existed between the responders and the decliners with respect to the examined sociodemographic data.
The demographic and substance use characteristics of the respondents are presented in Table 1. Of the 107 respondents, 52 (48.6%) reported using non-prescribed benzodiazepines in the 30 days preceding the study; 51 of these respondents (47.7%) reported oral use only and 1 respondent (0.9%) reported both oral and intravenous use. The days of reported use ranged from 1 to 30 days (mean = 13.8, median = 9.5). Of the users of non-prescribed benzodiazepines, 47 (90.4%) gave benzodiazepine-positive urine samples at routine urinalysis drug screens in the 30 days preceding the study. Users of non-prescribed benzodiazepines differed significantly from non-users in terms of marital status, educational attainment, and extent of cocaine and heroin use in the past month (Table 1).
TABLE 1 Comparison of demographics and substance use history between benzodiazepine users and non-users in a methadone maintenance treatment programme
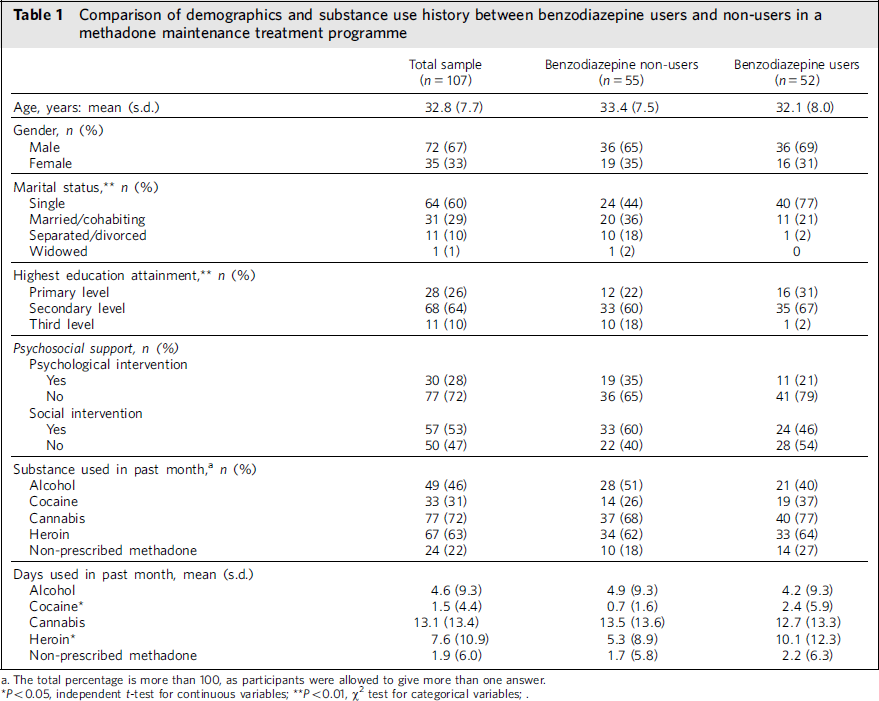
a. The total percentage is more than 100, as participants were allowed to give more than one answer.
* P < 0.05, independent t-test for continuous variables;
** P < 0.01, w2 test for categorical variables;.
CANSAS-P
The proportions of perceived need, met need and unmet need for each CANSAS-P item are presented in Table 2. Among all the respondents, the mean number of total needs was 7.1 (s.d. = 3.3), with 1.7 (s.d. = 1.4) needs met and 5.4 (s.d. = 2.9) needs unmet.
TABLE 2 Prevalence of needs among patients on methadone maintenance treatment, comparing benzodiazepine users and non-usersFootnote a

a. The total percentage for each collumn exceeds 100, as participants were allowed to indicate multiple areas of need.
* P<0.05, σ2 test;
** P<0.01, σ2 test.
The proportion of unmet needs exceeded that of met needs in 15 of the 22 items. The five items with the highest proportions of unmet need were drug use, psychological distress, daytime activities, social company, and physical health. The items with the fewest perceived needs were telephone access, self-care, looking after the home, and safety of others.
Benzodiazepine use and perception of need
The mean number of needs identified by users of benzodiazepines was 7.8 (s.d. = 3.1), and the mean number of total needs identified by non-users was 6.4 (s.d. = 3.3, F = 0.001, d.f. = 105, P = 0.02). The mean number of met needs identified by users of benzodiazepines was 1.8 (s.d. = 1.4, F = 0.007, d.f. = 105, P = 0.53), and the mean number of met needs identified by non-users was 1.6 (s.d. = 1.4). The mean number of unmet needs identified by users of benzodiazepines was 5.9 (s.d. = 2.8), and the mean number of unmet needs identified by non-users was 4.7 (s.d. = 2; F = 0.163, d.f. = 105, P = 0.02). The areas in which these differences were statistically significant were drug use and daytime activities.
Substances associated with severity of needs
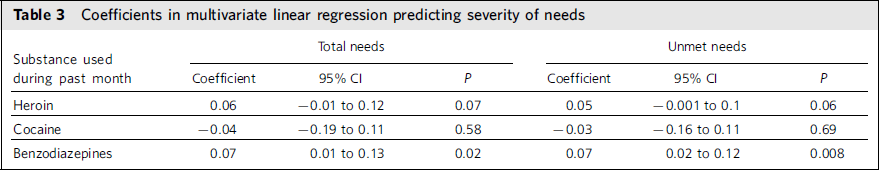
On univariate analysis, the mean number of days of reported use of heroin, non-prescribed methadone and cocaine was higher in the benzodiazepine-user group. These differences attained statistically significant levels for heroin and cocaine (Table 1). The effects of benzodiazepine use on total and unmet need scores after controlling for heroin and cocaine use in the multivariate linear regression analyses are presented in Table 3. In accordance with our hypothesis, we found that a higher number of days of benzodiazepine use is significantly associated with higher total and unmet need scores.
TABLE 3 Coefficients in multivariate linear regression predicting severity of needs
Discussion
There are a wide variation and high levels of unmet need for treatment of substance misuse, daytime activities, social company, money budgeting and benefits, psychological distress and physical health in this study. These findings are consistent with rates observed on the receipt of needed services during addiction treatments, as reported in previous research.Reference Pringle, Emptage and Hubbard8,Reference Joe, Simpson and Hubbard9,Reference Etheridge, Craddock, Dunteman and Hubbard11 Contrary to the results of previous studies, basic needs (accommodation, food, telephone access, self-care) were generally met. Similar to the results of previous studies, areas that facilitate engagement in treatment (e.g. childcare, transportation) were met. The findings reported in the present study lend support to arguments that providing ancillary supports for addiction-related psychosocial problems is critical to treatment retention.Reference Pringle, Emptage and Hubbard8 A major goal of addiction treatment is to improve quality of life. Patient-rated unmet needs relate to poor quality of life;Reference Slade, Leese, Cahill, Thornicroft and Kuipers2 therefore, using patient-rated needs as a way of targeting service provision should provide a guide to improving the quality of addiction care treatment.
Ongoing polysubstance use was common in the study sample. Cannabis and heroin use in the past month far exceeded 50% for both benzodiazepine users and non-users. About 49% of the respondents reported use of non-prescribed benzodiazepines in the past month. As reported by Manthey and colleagues, these benzodiazepine users are more likely to be single and to have lower educational attainment, compared with non-users.Reference Manthey, Van Veen, Giltay, Stoop, Neven and Penninx25 These findings probably contribute to the high rating for perceived unmet need of substance misuse treatment observed in the study. Chen and colleagues reported that opioid-dependent patients have anxiety problems before entering MMT and have pre-existing anxiety problems before their initiation of opiate use.Reference Chen, Berger, Forde, D'Adamo, Weintraub and Gandhi17 They suggested that most MMT programmes fail to address the issues of co-occurring anxiety problems, and MMT triggers the onset or worsening of benzodiazepine misuse. This possibly explains why benzodiazepine misuse has independently predicted increasing severity of needs in our study. Therefore, our findings further highlight that MMT services need to focus on and re-evaluate the present treatments for benzodiazepine misuse or dependency, because benzodiazepine misuse or dependency affects MMT outcomes.
Strengths and limitations
The study has several strengths. First, to the best of our knowledge, no study has previously used the CAN in assessing unmet needs in addiction treatment care. Second, this study describes a representative group of opioid users in the oldest and largest MMT programme in Ireland, during a defined period of standard clinical practice. Third, by using a patient-friendly version of CAN and not relying on the ratings of service providers, the data collected are more likely to reflect patients’ actual perceptions and facilitate comparison with similar patient groups elsewhere.
The study is not without limitations. Although the study sample may be representative of opioid dependent users, generalisability of the study findings should be applied in the context of its modest response rate of 56%. Therefore, it is essential to replicate the study's findings in other MMT populations. Information regarding the level of engagement with psychosocial interventions and external supports offered to the respondents was not collected. Opioid-dependent patients are known to have low levels of motivation for engaging satisfactorily with non-pharmacological treatment approaches.Reference Seivewright, Donmall and Daly26 Furthermore, coexisting anxiety disorders are common among opioid-dependent patients, particularly patients who use benzodiazepines.Reference Chen, Berger, Forde, D'Adamo, Weintraub and Gandhi17 Data on anxiety and other psychopathology would be interesting, but such data were beyond the scope of the present study. Finally, the results are from an Irish urban population, and levels of available service and support may vary in other settings with different cultural, treatment and socioeconomic characteristics.
Implications for service development
We identified high levels of unmet needs, particularly for treatment of substance misuse and daytime activities. Assessing literacy skills during substance misuse treatments may increase self-esteem, increase individual autonomy and lead to better employment prospects, thereby satisfying the unmet need for daytime activities. Further, we found evidence to support our suggestion that benzodiazepine misuse by patients on MMT predicts severity of unmet need. Of note, this study focuses on assessing need and does not propose that fulfilling unmet needs will necessarily alter benzodiazepine misuse among opioid users. Future studies investigating the impact of addressing unmet needs and benzodiazepine misuse in MMT are desirable.
Conclusions
We recommend formal and active assessments of the needs of patients on MMT to help offer the necessary information and advice and to facilitate engagement with the appropriate psychosocial services. Interventions aimed at targeting rapid access to evidence-based treatment approaches for benzodiazepine misuse and dependence are essential.






eLetters
No eLetters have been published for this article.