Nidotherapy (after nidus, ‘nest’) was first introduced as a treatment for people with complex personality disorders who had failed to respond to other treatment. Reference Tyrer1 It involves the systematic assessment and modification of the environment to help in minimising the impact of any form of mental disorder on the individual or on society. Reference Tyrer, Sensky and Mitchard2,Reference Tyrer and Bajaj3 The treatment does not aim to treat the patient directly; it involves an environmental analysis of personal, social and physical environments, the setting of environmental targets, constructing a plan for environmental change (nidopathway), as well as monitoring the progress of this and making changes as necessary. Reference Tyrer4
A randomised controlled trial of nidotherapy was carried out in a population with patients in an assertive outreach team in which enhanced care with nidotherapy was compared with ordinary assertive outreach treatment alone. Reference Ranger, Tyrer, Miloseska, Fourie, Khaleel and North5 This included 52 patients with comorbid personality disorder and severe mental illness and showed non-significant reductions in bed usage, clinical symptoms and social functioning, but with sufficient reduction in cost to regard the treatment as cost-effective. These patients also included many with additional pathology, notably comorbid substance misuse, which in previous investigations Reference Cleary, Hunt, Matheson, Siegfried and Walter6 has proved very difficult to treat, with no single approach having clear effectiveness over ordinary care. Because of this and because this group of patients accounts for many days of in-patient treatment, the outcome of 37 patients with substance misuse and psychosis who were randomised in the trial Reference Ranger, Tyrer, Miloseska, Fourie, Khaleel and North5 was felt to be of sufficient interest to carry out a secondary analysis of the data, and this is reported in this paper.
Method
The methodology of the study has been described elsewhere. Reference Ranger, Tyrer, Miloseska, Fourie, Khaleel and North5 It involved a simple parallel design with two treatment arms: nidotherapy-enhanced assertive treatment (referred to henceforth as nidotherapy group) and standard assertive outreach treatment (control group). In both the original study and our secondary analysis the main null hypothesis being tested was that nidotherapy and ordinary assertive outreach treatment would reduce the usage of hospital beds equally. The secondary hypotheses were that reduction of psychiatric symptoms and improvement in social functioning and engagement would also be similar in nidotherapy and control groups. These were a priori hypotheses for the main trial and transferred to the secondary analysis. No power calculation was made to establish the sample size and it was appreciated that definitive data were unlikely to be obtained from this small study.
Patients
The patients in this secondary study were all those diagnosed with substance dependence and a psychotic disorder recruited from the case-load of an assertive outreach and rehabilitation team in central London. The sample comprised 37 patients, randomised over 13 months, with 35 and 26 assessed at 6 and 12 months respectively, and with service usage data and costs on 34 patients. The diagnosis was derived from case notes using ICD-10 diagnoses and in equivocal cases the OPCRIT system Reference McGuffin, Farmer and Harvey7 was used to confirm substance dependence.
Inclusion and exclusion criteria
Patients were selected from the existing clientele in the assertive outreach team if they had severe mental illness and personality disorder. For the secondary analysis they needed to satisfy the diagnostic criteria for schizophrenia, schizoaffective disorder or bipolar disorder, together with dependence on amphetamines, opiates, cocaine, cannabis or alcohol. They were also required to give informed consent and were not in a stable phase at the time of recruitment (i.e. they were clinically unwell or unstable, despite receiving appropriate, evidence-based treatment). Exclusion criteria included inability to understand the questionnaires or procedures because of English language competence or intellectual disability, and age under 18. In addition to clinical assessment, patients also had their personality status assessed, using the ICD-10 version of the Personality Assessment Schedule (PAS-I). Reference Tyrer8 Ethical approval was given by St Mary's Hospital ethical committee.
Procedure
After baseline assessment, those who satisfied the eligibility criteria and who were part of the case-load of the assertive outreach team between August 2003 and September 2004 were recruited. They were randomly allocated by an independent statistician, using a random numbers design with no stratification of groups, to either nidotherapy or control groups. Patients were assessed at baseline and at 6 and 12 months by M.R. and I.K., who remained blind of trial allocation; this was assisted by the fact that the nidotherapists in the team also worked as support workers with other patients and so their involvement did not disclose their therapeutic role.
Assessments
Assessments were made of:
-
• clinical psychopathology, using the Brief Psychiatric Rating Scale (BPRS) Reference Overall and Gorman9
-
• social function, using key-worker and patient self-rated versions of the Social Functioning Questionnaire (SFQ) Reference Tyrer, Nur, Crawford, Karlsen, McLean and Rao10
-
• in-patient bed usage, from an independent assessment of hospital record data
-
• engagement with services, using the Engagement and Assessment Scale (EAS) Reference Park, Elsworth, Fox, Tyrer and McDonald11
-
• all service costs, using the Secure Facilities Service Use Schedule (SFSUS), Reference Barrett and Byford12 which covers every possible service contact for those with severe mental illness in secure facilities and in the community.
Primary and secondary outcomes
The duration of psychiatric admissions after 1 year was selected in advance as the primary outcome because the positive value of nidotherapy is judged by its ability to keep patients in a harmonious relationship with their home environment. All other outcomes were secondary and tested at 6 months and 1 year.
Interventions
Nidotherapy group
Those allocated to nidotherapy-enhanced assertive treatment received up to 15 sessions of nidotherapy, of variable length, from two nidotherapists following a standard format. Reference Tyrer and Bajaj3 This involved a combination of environmental analysis, articulation of the patient's needs at a physical, social and personal environmental level, and setting of targets. A flexible approach was used in the timing and frequency of sessions as the plan created (nidopathway) is determined by both therapist and patient. Where changes suggested by the nidotherapist conflicted with those of the clinical team, discussion followed and an agreed consensus was reached. In some instances, no major changes were suggested in the environment, but adjustments were made to suit patient preferences. Patients in this group continued to be seen by the assertive outreach team and no treatment approach normally used by the team was denied them.
Control group (ordinary assertive outreach)
Patients allocated to this group received the standard outreach therapy of the team. (A previous randomised trial had established that this particular team was at least as effective as other assertive outreach teams. Reference Tyrer1 )
Economic evaluation
Costs were assessed from the perspective of service providers, including the health, social, voluntary and criminal justice services. The SFSUS was used to record service use during the 6 months immediately before randomisation and the 12 months after randomisation. All costs were calculated for the financial year 2004/2005. The cost of the nidotherapy was based on the time spent by the therapist interviewing the patient and reporting to the clinical team responsible for their care, plus relevant overheads. In order to calculate total costs, unit costs were applied to each service. Hospital services were costed using National Health Service reference costs, 13 with published unit costs applied to community health and social services, Reference Curtis and Netten14,Reference Finn, Hyslop and Truman15 medication 16 and criminal justice services. 17,18
Statistical analysis
All analyses were carried out on an intention-to-treat basis; analysis of covariance with adjustment for baseline differences was used with the rating scale data. To compare the differences in bed days occupied between the two groups, we used the method of Welsh & Zhou Reference Welsh and Zhou19 in combining the logistic and log-transformed multiple regressions into a common framework. To allow for baseline differences, we planned to calculate the average (original scale, unlogged) 12-month admission days for both treatment groups for a patient with an average number of baseline admissions and to provide confidence intervals for the two treatment means to allow an assessment of differences at 12 months.
Clinical outcomes
The clinical data measured on each occasion were analysed by repeated measures analysis of variance, with adjustment for baseline values, and analysis of data by last observation carried forward (LOCF) as well as case analysis of full data. Bed usage was recorded by measuring the number of days spent in hospital in the previous 6 months, adjusted for baseline (also the previous 6 months) and treatment group. The analysis of variance was run on SPSS 13 for Windows.
Evaluation of costs
Costs were compared between the nidotherapy group and the control group using standard t-tests, despite the skewed distribution of cost data. This method enables inferences to be made about the arithmetic mean. Reference Thompson and Barber20 Non-parametric bootstrapping was used to assess the robustness of confidence intervals to non-normality of the cost distribution. Reference Efron and Tibshirani21
Results
Of 52 patients included in the trial, there were 37 with substance misuse: 19 were allocated to the nidotherapy group and 18 to the control group. With regard to ethnic background, 22 of the patients were White (59%), 8 were Black African or Caribbean (2%) and 7 were from other ethnic background (19%). These were similarly distributed, apart from African Caribbeans, who were disproportionately represented in the nidotherapy group (5 in nidotherapy, 1 in control). As far as substance misuse is concerned, 25 regularly used cannabis (68%), 15 had alcohol dependence (41%), 4 misused cocaine (11%), 2 benzodiazepines (5%), and 1 each misused antiparkinsonian drugs and amphetamines (3%); 10 were dependent on more than one drug (27%). All patients satisfied the criteria for at least one personality disorder so, in effect, this could be described as a ‘triple-diagnosis study’. Reference Tyrer8 One patient with polydrug use allocated to the control group died 2 months after randomisation. The data reported therefore relate to 36 patients, except with regard to hospital admissions. A CONSORT diagram shows the pathway of patients through the trial (Fig. 1).
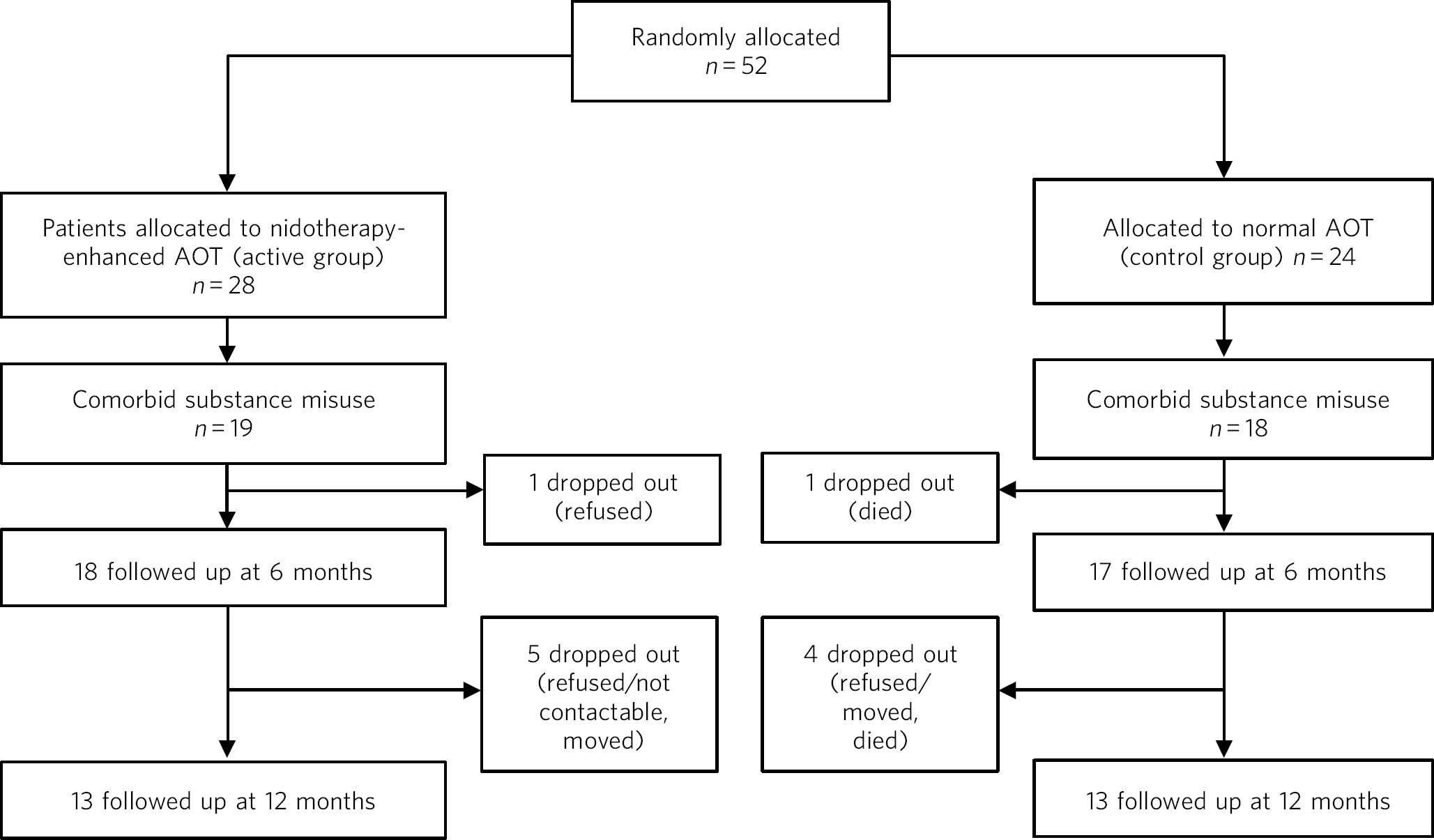
Fig 1 CONSORT diagram of selection of patients and their pathway through the trial. AOT, assertive outreach treatment.
Primary outcome
Data for all time points up to 12 months were available for 35 patients. There was a 110% difference in bed usage at one year (nidotherapy group reduction 2%; control group increase 108%; P = 0.035). However, the variance in the data was considerable. As bed usage increased in the control group with only a small reduction of bed usage in the nidotherapy group, the data illustrate the increasing problem of hospital bed use in those with dual diagnosis (substance misuse and psychosis).
Secondary outcomes
There were no meaningful differences between the outcomes in each group for clinical symptomatology and engagement, but also no evidence of inferiority for those allocated to nidotherapy. In the LOCF analysis there was also greater improvement in social functioning in those allocated to nidotherapy (P=0.045) (Table 1).
Table 1 Results of the secondary outcomes of clinical symptomatology (BPRS), social functioning (SFQ-KW) and engagement with services (EAS) in nidotherapy and control groups for participants with substance misuse problems at baseline

| F | Between-group difference based on estimated marginal means | ||||||
|---|---|---|---|---|---|---|---|
| Measure | Baseline (s.d.) | 6-month estimated marginal mean (s.d.) | 12-month estimated marginal mean (s.d.) | Main effect of group | Time × group interaction effect | Mean (s.d.) | 95% CI |
| BPRS available case analysis | 0.98 | 0.27 | −2.6 (13.3) | −8.0 to 2.8 | |||
| Nidotherapy, n = 13 | 32.7 (11.3) | 27.2 (6.1) | 25.7 (9.7) | ||||
| Control, n = 13 | 38.2 (10.6) | 28.8 (6.1) | 29.3 (9.7) | ||||
| BPRS LOCF analysis | 0.29 | 0.26 | −1.7 (18.6) | −4.7 to 8.1 | |||
| Nidotherapy, n = 18 | 32.9 (10.9) | 30.0 (8.9) | 29.0 (11.0) | ||||
| Control, n = 17 | 37.0 (11.1) | 31.0 (8.9) | 31.3 (11.0) | ||||
| SFQ-KW available case analysis | 2.14 | 0.25 | −1.6 (5.6) | −3.8 to 0.6 | |||
| Nidotherapy, n = 13 | 11.7 (4.7) | 12.4 (2.9) | 11.8 (3.3) | ||||
| Control, n = 13 | 12.7 (5.4) | 13.7 (2.9) | 13.7 (3.3) | ||||
| SFQ-KW LOCF analysis | 4.38* | 0.28 | −2.0 (5.6) | −4.0 to −0.1 | |||
| Nidotherapy, n = 17 | 11.9 (4.8) | 12.4 (2.9) | 11.9 (3.2) | ||||
| Control, n = 17 | 12.0 (5.8) | 14.1 (2.9) | 14.1 (3.2) | ||||
| EAS available case analysis | 1.60 | 0.65 | 1.1 (4.6) | −0.7 to 3.0 | |||
| Nidotherapy, n = 13 | 10.4 (3.4) | 10.2 (2.6) | 10.2 (2.6) | ||||
| Control, n = 13 | 7.6 (3.7) | 8.6 (2.6) | 9.5 (2.6) | ||||
| EAS LOCF analysis | 0.07 | 0.75 | 0.23 (5.2) | -1.6 to 2.1 | |||
| Nidotherapy, n = 17 | 10.2 (3.3) | 9.5 (2.8) | 9.5 (2.8) | ||||
| Control, n = 17 | 7.7 (3.9) | 9.0 (2.8) | 9.7 (2.8) | ||||
Together, these findings support the view that nidotherapy did not achieve its reduction in bed use at the cost of adverse clinical outcomes. Service use data were available for 34 study participants with substance misuse, 19 in the nidotherapy group and 15 in the control group; of the three participants for whom service use data were not available, two individuals had left the country and one person died. Average total costs are detailed inTable 2 and follow a similar pattern to those seen in the main analysis, Reference Ranger, Tyrer, Miloseska, Fourie, Khaleel and North5 although the differences in costs are more pronounced, with an increase in bed usage in those in the control group. Over the 12 month follow-up total costs were £ 14 705 less in the nidotherapy group compared with the treatment as usual group and this difference in cost was significant at the 10% level (P = 0.072). The difference in costs was primarily due to the substantial difference in the number of in-patient stays between the nidotherapy and treatment as usual groups, which is reflected in hospital costs of £10 938 in the nidotherapy group compared with £27 871 in the treatment as usual group. This was the main component behind the cost savings of £14 705 per patient overall.
Table 2 In-patient stays and total cost of services used over 12 months’ follow-up
| Nidotherapy group, n=19 Mean (s.d.) | Control group, n=15 Mean (s.d.) | Mean difference | |
|---|---|---|---|
| In-patient stays, nights | 54 (75) | 139 (135) | -85 |
| Healthcarea | 15 173 (15 786) | 31 105 (27 290) | -15 932 |
| Hospital costsb | 10 938 (14 990) | 27 871 (26 986) | -16 932 |
| Community health services | 3159 (1628) | 2065 (1256) | 1094 |
| Medication | 1076 (1704) | 1170 (875) | -94 |
| Social and voluntary services | 3559 (5622) | 2561 (4466) | 998 |
| Community | 1101 (1288) | 717 (682) | 383 |
| Accommodation | 2458 (5628) | 1844 (4618) | 615 |
| Criminal justice | 181 (787) | 2 (7) | 179 |
| Total costs | 18 963 (19 010) | 33 668 (27 022) | -14 705c |
Discussion
The findings with this substantial subpopulation recruited to the randomised trial were quite surprising. The original trial of patients with severe mental illness and personality disorder showed some evidence of benefit and cost savings, Reference Ranger, Tyrer, Miloseska, Fourie, Khaleel and North5 but these were magnified greatly in this smaller population. A trial of 37 patients can in no way be regarded as definitive, but the substantial impact of nidotherapy on bed usage was responsible for considerable cost savings that could be of clinical and economic importance. As patients with comorbid substance misuse and psychosis tend to remain in hospital for long periods Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry22,Reference Keown, Mercer and Scott23 and are generally resistant to complex interventions, Reference Johnson, Thornicroft, Afuwape, Leese, White and Hughes24 any treatment strategies that can reduce bed usage without impairing clinical outcomes are valuable.
The outcomes in this study suggest that there was no clinical handicap associated with addition of nidotherapy to the treatment programme and that social functioning, one of the main aims of nidotherapy, Reference Tyrer, Sensky and Mitchard2 also improved. Engagement with services was not improved by nidotherapy, but as good engagement is one of the outcomes of assertive outreach that is superior to that of conventional community mental health teams, Reference Killaspy, Bebbington, Blizard, Johnson, Nolan and Pilling25 this finding is not unexpected. The possible difficulties in the separation of the nidotherapist from the main clinical services could have an impact on engagement. Reference Spencer, Rutter and Tyrer26
Limitations
Despite these results, the study suffers from several limitations that reduce the strength of its conclusions. The main study hypothesis was not concerned with substance misuse and psychosis and this paper describes a secondary analysis only. The numbers are too small to reach any definitive conclusions and the drop-out rate of nearly 30% for the clinical data collection over the latter half of the 12-month period is too great to have confidence in the results of these measures. However, the independent collection of the economic data had only 8% of patients unaccounted for, so more reliance can be placed on the differences in these data. We also have reasonable confidence that the research assessors were blind to the allocation of patients when recording their data because the nidotherapists involved in the study also worked with the patients in the control groups as support workers.
It is difficult to determine where nidotherapy might have had particular value in this population. Since it is concerned with getting a better environmental fit for the patient, it could promote more appropriate placements for patients after discharge. The role of the nidotherapist in acting as an advocate for the patient Reference Spencer, Rutter and Tyrer26 may also be important here, as the ability to get over personal wishes and needs to the clinical team in a coherent and consistent way was useful in effecting change. The wish most fervently expressed by the patients allocated to nidotherapy was that for greater autonomy and this was also taken account of in planning the nidotherapy strategy. One recurring theme in the patients with substance misuse was the wish to have greater personal control and not be persistently asked to stop misusing substances. In the practice of nidotherapy the emphasis on achieving a harmonious environmental fit quite independently of clinical pathology Reference Tyrer4,Reference Tyrer and Kramo27 may be relevant here; individuals begin to notice that substance misuse may spoil the environmental fit and they may modify it accordingly without any external pressures.
The practice of nidotherapy is a complex process still undergoing development. Practitioners need to be skilled in accepting patients for what they are and not what they would like them to be, to work with them in a collaborative, non-judgemental way, and to be sensitive in separating unrealistic wants from genuine needs when deciding on an environmental change. All nidotherapists who have been trained to date have been independent practitioners, with skills that are primarily those of engagement and encouragement (our two nidotherapists were also acting as support workers in this study and had no specific mental health qualifications). This may have been an asset with a population that is generally sceptical of any psychiatric intervention because of past experiences. Reference Tyrer4 The additional role of advocate is also much appreciated in this group Reference Spencer, Rutter and Tyrer26 and, by taking every aspect of the patients’ wishes seriously and considerately, fits in well with the promotion of recovery. The fact that not only bed usage was reduced in this study but community placements were made relatively cheaply (Table 2) suggests that the role of nidotherapist in ‘customising’ accommodation so that it makes a better fit for the patient is cost-effective. The possibility that this could bring wider benefit needs to be extended further in definitive randomised trials.
Funding
The study was supported by a grant from the Nicola Pigott Fund. International Trial no.: ISRCTN 73227556.
Acknowledgements
We thank Kofi Kramo, Andrew MacDonald, Sandra O'Sullivan, Nancy Ababio and Deirdre Dolan for their assistance in promoting the trial and ensuring that assessments were made blind of knowledge of allocation, Bharti Rao for acting as an independent randomiser of patients and Sandra O'Sullivan for administrative support throughout the trial.






eLetters
No eLetters have been published for this article.