Introduction
Children and young people with genetic syndromes have a particularly high likelihood of developing an emotional or behavioural difficulty. Some genetic disorders have specific behavioural phenotypes, which are distinctive characteristics and consistent behaviour patterns (for example Waite et al., Reference Waite, Heald, Wilde, Woodcock, Welham, Adams and Oliver2014). Other studies reveal that children with genetic disorders may not have specific behavioural phenotypes but have higher rates of all common emotional and behavioural problems – likely as a result of both genetic and environmental risk factors. Several studies have found that children and young people with rare genetic conditions, such as XXYY syndrome and 22q11 deletion syndrome, are significantly more likely to experience the common mental health problems that occur in the general child population. For example, they have higher rates of emotional and behavioural problems and meet diagnostic criteria for depression, anxiety disorders and oppositional defiant disorder (ODD) compared with matched controls (Baker and Skuse, Reference Baker and Skuse2005; Hodapp et al., Reference Hodapp, Ly, Fidler and Ricci2001; Richman et al., Reference Richman, Belmont, Kim, Slavin and Hayner2009; Srinivasan et al., Reference Srinivasan, Wolstencroft, Erwood, Raymond, Van Den Bree and Hall2019). A case-control cohort online phenotyping study of 186 children with intellectual disability (ID) and copy number variants found that children with genetic mutations were also more likely to meet criteria for psychiatric and neurodevelopmental disorders, such as attention deficit hyperactivity (ADHD) and autism spectrum disorder (ASD), compared with controls, suggesting a complex genomic risk for psychiatric disorders in children with genetic disorders (Chawner et al., Reference Chawner, Owen, Holmans, Raymond, Skuse, Hall and van den Bree2019). Chawner and colleagues (Reference Chawner, Owen, Holmans, Raymond, Skuse, Hall and van den Bree2019) conclude that ‘this patient group clearly warrants clinical and educational attention and intervention’; data from the same cohort demonstrated that parents of these young people reported significantly elevated emotional distress and also report a need for mental health support (Baker et al., Reference Baker, Devine, Ng-Cordell, Raymond and Hughes2021). In addition, clinicians working in generic child and adolescent mental health services may be concerned that the ordinary, evidence-base treatments for common child emotional and behavioural problems may not be appropriate in children with rare diseases.
The current literature on low-intensity mental health interventions for the paediatric population is emerging and suggests that it is not only feasible and acceptable (Bennett et al., Reference Bennett, Heyman, Varadkar, Coughtrey and Shafran2017b; Bennett et al., Reference Bennett, Heyman, Coughtrey, Varadkar, Stephenson and Shafran2021a; b) but also effective for emotional and behavioural difficulties in children with long-term physical health conditions (Catanzano et al., Reference Catanzano, Bennett, Sanderson, Patel, Manzotti, Kerry and Shafran2020). Low-intensity interventions may have particular value in this group as they minimise the need for further hospital visits in groups who may already be disadvantaged through school absences. Furthermore, a large proportion of children with long-term physical conditions and co-morbid emotional and/or behavioural difficulties may also have neurodevelopmental disorders and genetic conditions (57% of children with neurodevelopmental disorders who attended a mental health drop-in centre in a paediatric hospital had genetic abnormalities; Stock et al., Reference Stock, Catanzano, Rojas, Ching, Shafran, Bennett and Liangin preparation).
A possible way of meeting the mental health needs of children with genetic conditions may be through low-intensity psychological interventions, defined as the use of self-help materials to provide six or less hours of contact time by trained practitioners (Shafran et al., Reference Shafran, Myles-Hooton, Bennett and Öst2021). A systematic review and meta-analysis found that low-intensity interventions like guided self-help produced moderate to large effects on symptoms of anxiety, depression and challenging behaviour in children and young people and is similarly efficacious as face-to-face psychological therapy (Bennett et al., Reference Bennett, Cuijpers, Ebert, McKenzie Smith, Coughtrey, Heyman and Shafran2019). This type of intervention may be an economical and accessible approach to meeting the large unmet need in evidence-based psychological interventions in children; interventions are usually briefer and require fewer resources for providers, can be delivered by trained practitioners (e.g. assistant psychologists without clinical qualifications), and completed over telephone or email (Shafran et al., Reference Shafran, Myles-Hooton, Bennett and Öst2021; Williams and Martinez, Reference Williams and Martinez2008).
We describe a case series report on the delivery of low-intensity psychological intervention for emotional and behavioural difficulties in eight children and young people attending genetics clinics at a paediatric hospital in the UK.
Method
Participants and procedure
The low-intensity intervention was offered as a service to all children and young people attending the paediatric hospital as part of an extension project of a wider study during the coronavirus (COVID-19) pandemic. The wider study was evaluating a psychological wellbeing and mental health drop-in centre situated in a paediatric hospital in the UK offering evidence-based mental health support for patients, their siblings, and parents/carers (Catanzano et al., Reference Catanzano, Bennett, Kerry, Liang, Heyman, Coughtrey and Shafran2021). The main inclusion criterion was the presence of emotional and/or behavioural difficulties (anxiety, obsessive compulsive disorder (OCD), depression and/or conduct difficulties) that were interfering with current functioning. Families must not have been currently under the care of the hospital’s paediatric psychology services and needed a sufficient grasp of English to facilitate engagement with assessment and treatment. Families/patients provided written informed consent and completed baseline measures over email/telephone. Following this, an initial triage assessment was carried out over telephone/video conference. All participants were then discussed in a weekly meeting with clinical psychologists and child and adolescent psychiatrists and allocated to intervention as appropriate. Outcome measures were collected 6 months following baseline over email/telephone by a researcher who was independent from the delivery of the intervention.
Eight children and young people attending genetics clinics at the hospital consented to the main study between August 2020 and March 2021; four of these were referred by clinicians and four parents self-referred by emailing/telephoning the team running the service after being signposted by their clinician. All eight were considered appropriate for low-intensity intervention, and seven of these participants consented to their inclusion in the present case series. The eighth patient was not approached for consent as they were transitioning to a different service. Their characteristics are provided in Table 1. Genetic conditions (not included to preserve anonymity) included Fragile X syndrome (n=1), Neurofibromatosis Type 1 (n=1), Wiedemann-Steiner syndrome (n=2), 3M syndrome (n=1), XYY syndrome (n=1) and Trisomy 8 Mosaicism (n=1).
Table 1. Characteristics of participants (n=7)

ADHD, attention deficit hyperactivity disorder; ASD, autism spectrum disorder; ID, intellectual disability; IMD, index of multiple deprivation decile; OCD, obsessive compulsive disorder.
Course of therapy
The treatment was low-intensity psychological interventions administered through the parent/participant depending on treatment target (behavioural difficulties were administered through the parent) and child age. Parent/participant were provided with hand-outs used as self-help materials from The Modular Approach to Treatment of Children with Anxiety, Depression, Trauma or Conduct Problems (Participants 1–3 and 5–7; MATCH-ADTC; Chorpita and Weisz, Reference Chorpita and Weisz2009) or Breaking Free from OCD self-help book (Participant 4; Robinson et al., Reference Robinson, Turner, Derisley and Heyman2008). Although MATCH-ADTC was not designed to be delivered as a low-intensity psychological intervention, it has been successfully adapted and used as guided self-help teletherapy for children with co-morbid neurological and mental health needs in a paediatric setting (Bennett et al., Reference Bennett, Heyman, Varadkar, Coughtrey, Walji and Shafran2021b). Parents/participants received seven weekly contacts with a research assistant/assistant psychologist (B.C.F.C.) who acted as the trained practitioner over telephone/video conference: one 1-hour goal-setting session and further assessment, and six 30-minute treatment sessions.
Goal-setting session (session 1)
In this initial appointment, treatment goals were developed collaboratively by practitioner and parents/participants that addressed areas and difficulties where change would be meaningful to them (Law and Wolpert, Reference Law and Wolpert2014). Further assessment of difficulties was conducted in this session if necessary to inform the development of treatment goals.
Treatment sessions (sessions 2 to 7)
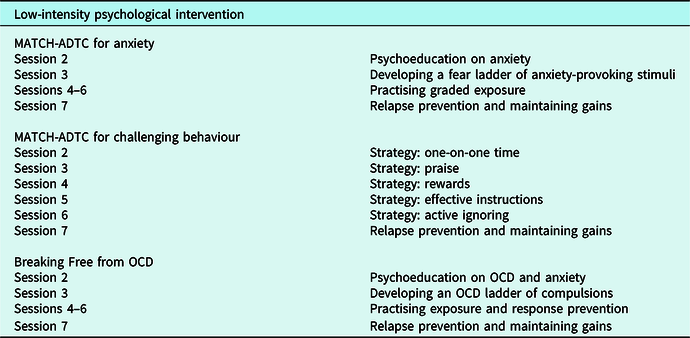
The sessions reviewed modules for anxiety or behavioural difficulties from MATCH-ADTC for children and young people presenting with anxiety (n=1) or behavioural problems (n=5), and key chapters for OCD for the young person with OCD (n=1). The modules covered specific evidence-based strategies, such as praise, rewards, graded exposure and relapse prevention (see Table 2 for further details). Training of the practitioner was delivered remotely and before treatment commenced (Batchelor et al., Reference Batchelor, Catanzano, Kerry, Bennett, Coughtrey, Liang and Shafran2020). The role of the practitioner was to monitor progress, encourage and guide the parent/participant through the self-help materials, review concepts and information from the materials, apply strategies to their individual difficulties and contexts, and help problem-solve challenges that arose. For example, a parent/participant would independently work through self-help materials on graded exposure outside of the treatment sessions. During the treatment sessions, the practitioner would review progress and help problem-solve difficulties faced in exposure practices, but not deliver in vivo exposure. As such, whilst low-intensity interventions are generally less time-intensive for practitioners, they importantly are not perceived as low-intensity to the parent/participant. Weekly 1-hour supervision was provided by clinical psychologists (S.D.B. and/or R.S.).
Table 2. Structure and content of the low-intensity psychological interventions and treatment sessions

Measures
Pre–post intervention measures
Child anxiety and behavioural difficulties were assessed using the Strengths and Difficulties Questionnaire (SDQ; Goodman, Reference Goodman1997), a parent-report measure for children aged 2–17 (Goodman and Goodman, Reference Goodman and Goodman2011). Child quality of life was assessed using the Pediatric Quality of Life Inventory (PedsQL; Varni et al., Reference Varni, Seid and Rode1999), where the appropriate form was used depending on child’s age. It contains subscales across four dimensions: physical, emotional, social, and school functioning. Both measures have demonstrated strong psychometric properties in children and young people (Goodman, Reference Goodman2001; Varni et al., Reference Varni, Seid and Kurtin2001; Varni et al., Reference Varni, Burwinkle and Seid2005). The SDQ is also a measure in the Child Outcomes Research Consortium (CORC) used to assess child mental health in clinical and general settings and was the primary outcome used in the NHS Digital Mental Health of Children and Young People in England Survey (NHS Digital, 2018), enabling future data to be benchmarked against national datasets.
Child OCD was assessed using the Children’s Obsessional Compulsive Inventory-Revised (ChOCI-R; Uher et al., Reference Uher, Heyman, Turner and Shafran2008) for the young person with OCD, a 32-item parent/self-reported measure of the presence and severity of symptoms of OCD. The ChOCI-R has demonstrated acceptable internal consistency, convergent and divergent validity in children and young people (Uher et al., Reference Uher, Heyman, Turner and Shafran2008). It is briefer and can be used independently without clinician rating unlike other comparable measures (Bennett et al., Reference Bennett, Coughtrey, Shafran and Heyman2017a; Conelea et al., Reference Conelea, Schmidt, Leonard, Riemann and Cahill2012).
Session-by-session measures
In participants presenting with anxiety/OCD, symptoms of anxiety were assessed weekly using the parent-report version of the ‘How are things? Generalised Anxiety Disorder Assessment’ (Child Outcomes Research Consortium, 2015a) from the first treatment session (session 2). Parents score each item as ‘never’, ‘sometimes’, ‘often’ or ‘always’ for their child.
In participants presenting with disruptive behaviour, symptoms of disruptive behaviour disorder were assessed weekly using the ‘How are things? ODDp’ (Child Outcomes Research Consortium, 2015b) from the first treatment session (session 2). This is a parent-reported measure where parents score each item as ‘not true’, ‘sometimes true’ or ‘certainly true’ for their child.
Goals for treatment (up to three) were identified by parent/participant at the initial appointment (Child Outcomes Research Consortium, 2015c). Progress towards the goals was rated on a scale of 1–10 at the start of each session (with 1 being no progress towards goal, and 10 being goal is fully achieved) from session 1.
Treatment satisfaction
A slightly modified version of the Client Satisfaction Questionnaire (CSQ-8; Attkisson and Greenfield, Reference Attkisson, Greenfield and Maruish1994) was used, where additional items were added (i.e. items eliciting potential improvements), some were reworded, and open text was provided for some items. Modifications were made to ensure items were relevant to the drop-in centre. Responses were on a 5-point scale and ranked 0–4: ‘not at all’, ‘only a little’, ‘somewhat’, ‘quite a bit’ and ‘totally’.
Feasibility measures
Feasibility was assessed through treatment completion rates, number of modules/chapters completed, number of sessions parent/participant did not attend (DNAs), adverse events, and need for onward referral following the intervention.
Analysis
Descriptive statistics for SDQ, PedsQL and ChOCI-R scores at baseline and 6-month follow-up were calculated, including Cohen’s d and 95% confidence intervals (Cohen, Reference Cohen2013). Individual level reliable and clinically significant change analysis for SDQ scores from baseline to 6-month follow-up were calculated by determining whether change in scores was statistically reliable, accounting for the variance of the SDQ [reliable change index (RCI); Goodman, Reference Goodman2001], and if scores fell within or outside the clinical range (Jacobson and Truax, Reference Jacobson and Truax1991). SDQ scores that were categorised as ‘high’ or ‘very high’ ranges were considered in the clinical range. Based on these criteria, participants were either classed as recovered (RCI<1.96 and their post-intervention score was no longer in the clinical range), improved (RCI<1.96 but post-intervention score was still in the clinical range), not reliably changed (RCI>1.96), or deteriorated (RCI<1.96 and post-intervention score was worse than baseline). Session-by-session measures were analysed visually and descriptive statistics were provided. Individual scores on the CSQ-8 were visually inspected, descriptive statistics were provided and all open-text data were collated.
Results
Table 3 demonstrates baseline and 6-month follow-up outcomes for the SDQ, PedsQL and ChOCI-R total scores. Table 4 demonstrates individual participant reliable and clinically significant change on the SDQ and change on the PedsQL. SDQ total scores reduced for six out of the seven participants at 6-month follow-up, with three demonstrating reliable recovery (scores within the very high range at baseline and close to average range following treatment), and four demonstrating unreliable change. PedsQL total scores improved for five out of the seven participants at 6-month follow-up. For the young person with OCD, parent-reported ChOCI-R total symptom and impairment scores reduced from 44 and 33 at baseline, to 27 and 8 at 6-month follow-up, respectively. A smaller reduction was seen in young person-reported scores in the ChOCI-R and SDQ: ChOCI-R total symptom and impairment scores from 41 and 20 at baseline, to 40 and 19 at 6-month follow-up, respectively, and SDQ total score from 8 at baseline, to 9 at 6-month follow-up.
Table 3. Mean scores (SD) and Cohen’s d (95% confidence intervals) on standardised measures at baseline (T1) and 6-month follow-up (T2)

SDQ, Strengths and Difficulties Questionnaire; PedsQL, Pediatric Quality of Life Inventory; ChOCI-R, Children’s Obsessional Compulsive Inventory-Revised.
Table 4. Change on parent-reported SDQ and PedsQL scores from baseline (T1) to 6-month follow-up (T2) in each participant
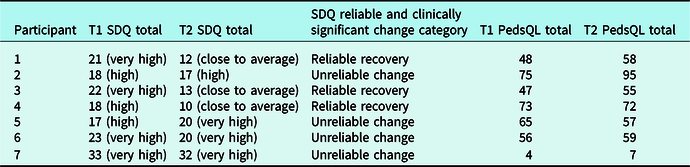
PedsQL total scores are rounded to integers.
Session-by-session measures
Over the course of treatment, all participants saw increases in mean goal progress from session 1 (median=1, IQR: 1–2) to the final treatment session (median=8; IQR: 5–9). Five participants saw steep goal progress from baseline to end of treatment, while the remaining two participants saw only minor progress. Of the five participants who received treatment for challenging behaviour, the session-by-session measure of symptoms of challenging behaviour on average reduced from the initial rating at the start of treatment (median=10; IQR: 6–13.5) to the last treatment session (median=5; IQR: 4–13.5).
Participant 1 did not provide a measure of symptoms of challenging behaviour at the start of treatment. Similarly, participant 3 did not provide a measure of anxiety at the start of treatment. Therefore, the session-by-session measures of symptoms of challenging behaviour and anxiety at start of treatment only represent five participants. Except at start of treatment, data completeness was achieved for all measures at 6-month follow-up. Of the two participants who received treatment for anxiety and OCD, respectively, the session-by-session measure of symptoms of anxiety on average reduced from the initial rating at the start of treatment (median=18) to the last treatment session (median=9). The participant who was treated for anxiety saw steep improvements in treatment, and similarly with the participant who was treated for OCD, although initially her symptoms deteriorated between treatment sessions 1 and 2 before improvement. Changes in symptoms of challenging behaviour across the five participants were variable, where participants 1 and 2 saw reduced challenging behaviour, participant 6 saw a slight increase, and participants 5 and 7 saw little-to-no change. See Figs 1 and 2 for the session-by-session trajectories of change for each participant across goals and behaviour and anxiety symptoms.
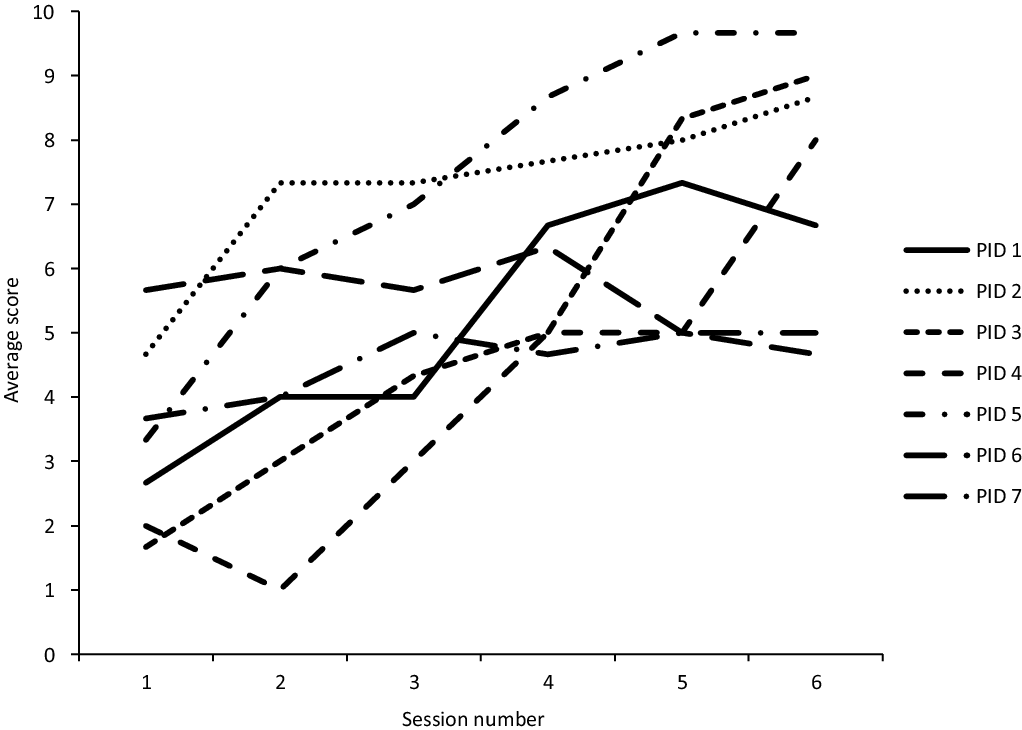
Figure 1. Session-by-session goals (goal-based outcome) for each participant in the goal-setting (session 1) and treatment sessions (sessions 2 to 7).
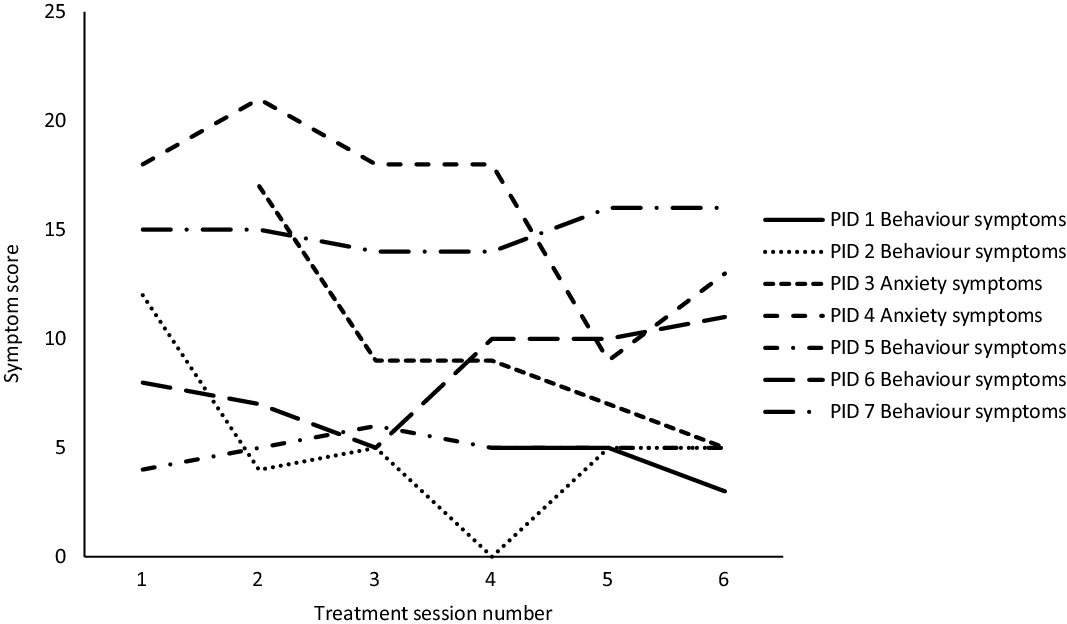
Figure 2. Session-by-session behaviour and anxiety symptoms for each participant in the treatment sessions.
Treatment satisfaction
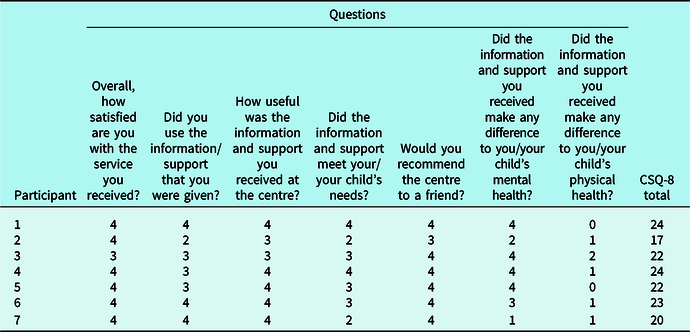
The median score was ‘4’ (‘totally) for the CSQ-8 questions about overall satisfaction (IQR: 4), how useful the information and support received was (IQR: 3–4), whether parent would recommend the centre to a friend (IQR: 4), and whether the information and support received made a difference to parent/participants’ mental health (IQR: 2–4). The median response to all other items was ‘3’ (‘quite a bit’) except for the question about whether the information and support received made a difference to parent/participants’ physical health, where the median response was ‘1’ (only a little’; IQR: 0–1). See Table 5 for individual treatment satisfaction scores for each CSQ-8 item across participants.
Table 5. Treatment satisfaction of participants in the CSQ-8

CSQ-8 scoring (0 = ‘not at all’, 1 = ‘only a little’, 2 = ‘somewhat’, 3 = ‘quite a bit’, 4 = ‘totally’).
We provide brief qualitative data from open text sections on parent feedback of their experiences of the intervention. Parents of three participants felt that the intervention provided them with ‘tips’, ‘strategies’ and ‘techniques’ to manage their difficulties which made ‘things better’. One parent expressed that the intervention provided space for them to learn about their child and seek further professional help:
‘None of you were judgemental, just tried to help me, giving me tips to make things better. I have learnt more about my kids and the centre helped me get a paediatrician. I understand [child] better, what sets her off, and how to deal with it, instead of being frustrated. It has helped me be a better parent and better person and we have more fun and time together.’ [Parent of participant 1]
The weekly sessions were reported by a parent of one participant to be useful as having a ‘third party’ meant they were held accountable for reviewing and practising the self-help materials. This also meant that parents were able to have help to individualise and apply the strategies and troubleshoot challenges that arose throughout the course of treatment:
‘I think a friendly helpful and supportive talk every week was greatly appreciated. I also found the strategies very useful and though most were common sense it was good to talk through how they should be applied and how effective they were (ways to tweak them to the situation).’ [Parent of participant 6]
Parents of three participants expressed being able to identify tangible change in their lives and found the intervention beneficial:
‘[Child] is significantly better since her sessions and this is a huge improvement to our family life. Whilst she has not lost the OCD completely, it is under control much more than it was before.’ [Parent of participant 4]
‘Thank you very much. We would highly recommend receiving this type of support and we appreciated it very much. [Practitioner] was very positive and that was great for us as we needed a bit of that given that so many things had felt quite negative.’ [Parent of participant 6]
With regard to how the intervention could be improved, one parent expressed wanting ‘a longer intervention’ (parent of participant 6) and another felt that some goals set at the start of treatment ‘were not applicable at the end’ so being able to change goals throughout treatment would have been helpful (parent of participant 5).
Feasibility measures
All participants completed the one goal-setting session and six sessions of treatment. Of the six participants who received MATCH-ADTC, all modules and materials that were offered were completed: six modules for challenging behaviour and four modules for anxiety. Of the one participant who received Breaking Free from OCD, all seven chapters and materials that were offered were completed. All scheduled sessions were attended by participants. Regarding adverse events, one participant (participant 7) reported one incident of self-harm behaviour in between treatment sessions. A clinical risk assessment was conducted which concluded that the self-harm behaviour was not intended to inflict harm on self but out of frustration due to ASD and sensory difficulties and not as a result of the intervention. Only participant 7 required onward referral to their local Child and Adolescent Mental Health Service (CAMHS) due to clinical risk issues.
Discussion
We demonstrate that low-intensity psychological interventions for emotional and behavioural difficulties in children and young people with genetic conditions can be delivered feasibly. Participants completed all treatment sessions, including the triage assessment and goal-setting session. Parents and participants completed all modules and materials provided as part of the low-intensity intervention and attended the telephone/video conference appointments. The qualitative open text from the CSQ-8 also demonstrated that the intervention was enjoyed, accessible and acceptable in the context of the pandemic. Parents expressed how the guided aspect of having weekly sessions with a practitioner was helpful and enhanced the usefulness of the evidence-based materials. The intervention was also feasibly delivered by a practitioner with brief training and regular supervision, who prior to the study, had no experience in delivering low-intensity interventions.
We preliminarily showed that low-intensity intervention may be beneficial for clinical outcomes in children and young people with genetic conditions. Changes in session-by-session measures demonstrate that the low-intensity intervention, which included materials that covered psychoeducation and strategies, was sufficient in effectively working towards goals that were meaningful to families and reduce symptoms of anxiety and challenging behaviour on a weekly basis. We demonstrate that the brief intervention can improve measures of anxiety and behavioural difficulties and quality of life through pre–post SDQ, PedsQL and ChOCI-R measures. In particular, effect sizes seem to be largest for SDQ Impact score, which suggests low-intensity intervention may improve distress and impairment associated with emotional and behavioural difficulties in this population. Importantly, three out of the seven participants demonstrated reliable recovery at 6-month follow-up in SDQ total and SDQ impact scores, where they no longer scored in the clinical range of their difficulties. Although all participants scored in the clinical range of the SDQ at baseline, the low-intensity intervention was feasibly delivered without the need for onward referral for more intensive treatment except for one participant with complex neurodevelopmental, psychological and behavioural needs.
These results suggest that low-intensity intervention delivered as part of a stepped care service could be a feasible method of ensuring access to mental health interventions for children and young people with genetic conditions. The use of trained practitioners with little prior therapy experience may reduce costs associated with psychological treatments and holds potential for providing interventions at scale by maximising the use of the psychology workforce (e.g. research assistants, assistant psychologists, psychological wellbeing practitioners, and clinical associate psychologists). This aligns with the NHS Improving Access to Psychological Therapies model (Clark, Reference Clark2011).
The findings need to be considered within the limitations of the study. Firstly, the small sample limited the analyses to individual level reliable and clinically significant change analysis and descriptive statistics. Future research should use larger samples and control comparators to determine the effectiveness of low-intensity intervention on child outcomes. Similarly, these studies should also consider the impact on the wider family unit and investigate the impact on parental and sibling outcomes. In the main study investigating the drop-in centre for children with long-term physical health conditions which offered low-intensity intervention presented in this study, we found that parental mental health also improved significantly after attending the centre for support for the child (Bennett et al., Reference Bennett, Kerry, Fifield, Ching, Catanzano, Liang and Shafran2021c). We must also consider the variation in presenting problems and genetic conditions in our sample when drawing conclusions from the study for wider commissioning of services. We only included young person-reported measures of symptoms for the participant receiving treatment for OCD due to their age, which was significantly different from their parent-reported measure. This suggests that it is integral to include young person-reported measures in conjunction with parent-reported measures to assist with understanding the holistic impact on the mental health of children with genetic conditions. Moreover, the qualitative open text was brief and future qualitative studies need to explore parents of children and young people with genetic conditions’ experiences of similar interventions for emotional and behavioural difficulties. We need to understand how low-intensity interventions may be experienced differently than traditional face-to-face interventions and whether there are factors that facilitate or act as barriers to treatment access and impact. This is especially the case as we know parents of children and young people with genetic conditions face many difficulties, especially in the diagnosis, management and coping of their child’s physical health and its impact on the child and family (Rivard and Mastel-Smith, Reference Rivard and Mastel-Smith2014). These in-depth qualitative investigations also need to gain the perspective of children and young people themselves. Although the treatment for challenging behaviour was done solely through the parent, the two participants who were treated for anxiety and OCD were involved in the intervention together with their parent. It is important to understand their experiences of the intervention and how the guided and remote format was received.
Increased recognition and early treatment of emotional and behavioural difficulties in children with genetic disorders can be supplemented by understanding and researching any distinctive patterns or features which may occur in this population. Current evidence suggests that standard mental health treatments need little or no modification for special populations (Shafran et al., Reference Shafran, Bennett, Coughtrey, Welch, Walji, Cross and Moss-Morris2020); however robust outcome studies are required.
The study adds value to the existing literature around the feasibility and impact of low-intensity psychological intervention for children and young people with genetic conditions and co-morbid emotional and behavioural difficulties. Being a pilot feasibility case series, the findings present initial data on how this form of intervention can be used to address the mental health and quality of life of this population. One obvious strength is that it is less costly than intensive psychological treatment and can be delivered by trained practitioners. It is especially pertinent to investigate the use of brief, evidence-based low-intensity interventions for mental health difficulties in children in the context of COVID-19 as many services have moved to remote service provisions to ensure needs of children and families are continuously met.
Conclusion
The current study is the first evaluation of low-intensity psychological interventions for mental health difficulties in children and young people with genetic conditions in a tertiary hospital setting. We provide initial evidence that it is feasible and acceptable to deliver brief, evidence-based low-intensity psychological interventions for emotional and behavioural difficulties in children and young people with genetic conditions. We demonstrate that the guided self-help format may be potentially beneficial for goal-based outcomes, symptoms of anxiety and challenging behaviour, and quality of life in children that is clinically meaningful. Together, our findings suggest this cost-effective treatment nested within a stepped care model can be feasibly delivered within NHS services. Further research is warranted to examine the effectiveness of low-intensity interventions in this group with larger samples and control groups.
Key practice points
-
(1) Low-intensity psychological interventions have been found to be promising for emotional and behavioural difficulties in children and young people with long-term physical health problems.
-
(2) The present feasibility case series provides initial data for the feasibility, acceptability, and potential benefit of low-intensity psychological interventions for emotional and behavioural difficulties in children and young people with genetic conditions.
-
(3) The findings suggests that this less costly psychological intervention can be delivered by trained practitioners to address the mental health and quality of life of children and young people with genetic conditions using a stepped care model.
Data availability statement
The data that support the findings of this study are available on reasonable request from the corresponding author, R.S. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Acknowledgements
We would like to acknowledge the contribution of Kate Fifield, our colleagues in Clinical Genetics at Great Ormond Street Hospital who supported recruitment, and the GOSH Young Person’s Advisory Group. Most importantly, we would like to thank the children and young people and their families who participated. All research at Great Ormond Street Hospital NHS Foundation Trust and UCL Great Ormond Street Institute of Child Health is made possible by the NIHR Great Ormond Street Hospital Biomedical Research Centre. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health.
Author contributions
Brian Ching: Conceptualization (supporting), Data curation (equal), Formal analysis (lead), Investigation (equal), Methodology (supporting), Project administration (lead), Visualization (equal), Writing – original draft (lead), Writing – review & editing (lead); Sophie Bennett: Conceptualization (equal), Funding acquisition (supporting), Investigation (equal), Methodology (equal), Project administration (equal), Supervision (equal), Validation (equal), Writing – original draft (supporting), Writing – review & editing (supporting); Natalia Rojas: Data curation (equal), Formal analysis (supporting), Investigation (supporting), Methodology (supporting), Project administration (supporting), Visualization (equal), Writing – original draft (supporting), Writing – review & editing (supporting); Isobel Heyman: Funding acquisition (equal), Methodology (equal), Writing – review & editing (supporting); Holan Liang: Funding acquisition (equal), Methodology (equal), Writing – review & editing (supporting); Matteo Catanzano: Methodology (equal), Writing – review & editing (supporting); Anna Coughtrey: Funding acquisition (equal), Methodology (equal), Writing – review & editing (supporting); Tazeen Ashraf: Resources (equal), Writing – review & editing (supporting); Wendy Jones: Resources (equal), Writing – review & editing (supporting); Alison Male: Resources (equal), Writing – review & editing (supporting); Roz Shafran: Conceptualization (lead), Funding acquisition (lead), Investigation (equal), Methodology (lead), Project administration (equal), Supervision (lead), Writing – original draft (equal), Writing – review & editing (supporting).
Financial support
This work was supported by The Beryl Alexander Charity and Great Ormond Street Hospital Children’s Charity (grant number VC0221/20PP18).
Conflicts of interest
The authors declare none.
Ethical standards
Authors have abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the BABCP and BPS. Ethical approval for this research project was granted by the London Riverside Research Ethics Committee (REC reference number: 16/LO/1915).








Comments
No Comments have been published for this article.