A number of studies in the early 1990s suggested that many people resident in special hospitals did not need to be there as far as their security was concerned (Reference Maden, Curie and MeuxMaden et al, 1993; Reference Shaw, McKenna and SnowdenShaw et al, 1994; further details available from the first author upon request). Previously, concern had been expressed about the difficulties in transferring patients out of special hospitals (Reference DellDell, 1980). Some management initiatives followed: for example, a programme to discharge long-stay patients with learning disabilities and to reduce the number of women in special hospitals. The current study seeks to examine the constitution of annual cohorts of resident patients between 1 January 1986 and 31 December 1995, and to test for changes in discharge patterns and lengths of stay in special hospitals.
METHOD
The sample and indicators of flow
The population examined consisted of all patients resident in a special hospital at any time between January 1986 and December 1995.
Departures were counted by episode rather than person. Similarly, in-patient episodes were used for analysis. An inpatient episode was defined at one end by the date of admission to hospital and at the other by discharge date or the census point (31 December 1995), whichever came first. Length of stay was calculated per episode.
Data collection
Data were extracted from the Special Hospitals' Case Register; methods of collection and classification are described in the companion paper.
Statistical analysis
All deaths were omitted from the discharge cohort analysis. This also applied to remand order cases, for which the residency is by definition under three months (six months for the little-used interim treatment order), except where a person, after reappearing in court was returned to hospital within 28 days, when residency was treated as a single episode.
Frequencies for residency in hospital and discharges (adjusted for available population) and grouped by Mental Health Act 1983 (MHA) classification of disorder and type of discharge were analysed using a Poisson model with robust standard errors. Rate ratios and their 95% confidence intervals (95% CIs) are per year unless otherwise stated; the year was fitted as a linear trend. STATA v5.0 (StataCorp, 1997) and SPSS v6.1 (SPSS, 1994) were used for the analyses.
RESULTS
Residency
The total number of patients ever resident in a special hospital between the beginning of 1986 and the end of 1995 was 3263; 2679 (82%) men and 584 (18%) women. They accounted for 3522 resident episodes in special hospitals. In 236 cases (7.2%), the data thus relates to the same individual admitted on more than one occasion. Just over one-fifth of patients (n=696, 21.3%) were resident for the whole of the 10-year period, and 247 episodes (7%) began prior to 1972, the year the case register was started. The 10-year average for the number of resident episodes per year was 1826 and the average daily population of patients over the 10 years was 1650.
Table 1 shows that, overall, the number of in-patient episodes fell over the 10 years, whether calculated by average daily or annual populations. MHA disorder groups were, however, differently affected. While residency fell slightly overall, the numbers of women, especially those in the group with mental impairment, showed the most striking reduction: rate ratio 0.89 (95% CI 0.87-0.91) for this last group. Unlike other groups, the number of men resident who were detained under the mental illness category did not alter much; rate ratio 1.00 (95% CI 1.00-1.02).
Table 1 Special hospitals in-patient episodes by Mental Health Act classification

| Year | Mental Illness | Psychopathic Disorder | (Severe) Mental Impairment | Total daily population 30 June | Total daily population 31 December | Total annual population | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men n (%)1 | Women n (%)2 | Total n (%)3 | Men n (%)1 | Women n (%)2 | Total n (%)3 | Men n (%)1 | Women n (%)2 | Total n (%)3 | ||||
| 1986 | 917 (62) | 172 (47) | 1089 (59) | 369 (25) | 109 (30) | 478 (26) | 193 (13) | 85 (23) | 278 (15) | 1645 | 1694 | 1848 (3) |
| 1987 | 966 (63) | 172 (47) | 1138 (60) | 376 (25) | 118 (32) | 494 (26) | 189 (12) | 78 (21) | 267 (14) | 1704 | 1724 | 1902 (3) |
| 1988 | 986 (64) | 176 (47) | 1162 (61) | 368 (24) | 160 (34) | 498 (26) | 183 (12) | 72 (19) | 255 (13) | 1731 | 1732 | 1919 (4) |
| 1989 | 999 (65) | 174 (46) | 1173 (61) | 369 (24) | 140 (37) | 509 (27) | 168 (11) | 64 (17) | 232 (12) | 1733 | 1720 | 1818 (4) |
| 1990 | 994 (65) | 165 (45) | 1159 (61) | 360 (24) | 140 (39) | 500 (27) | 166 (11) | 58 (16) | 224 (12) | 1706 | 1689 | 1885 (2) |
| 1991 | 1004 (66) | 157 (46) | 1161 (62) | 357 (23) | 130 (38) | 487 (26) | 160 (11) | 57 (17) | 217 (12) | 1713 | 1684 | 1866 (1) |
| 1992 | 1039 (67) | 153 (47) | 1192 (64) | 356 (23) | 122 (37) | 478 (25) | 150 (10) | 51 (15) | 201 (11) | 1681 | 1657 | 1872 (1) |
| 1993 | 1053 (68) | 149 (49) | 1202 (65) | 355 (23) | 113 (37) | 468 (25) | 143 (9) | 44 (14) | 187 (10) | 1609 | 1596 | 1857 (0) |
| 1994 | 1005 (69) | 153 (53) | 1158 (65) | 348 (23) | 102 (35) | 450 (25) | 127 (9) | 33 (11) | 160 (9) | 1563 | 1517 | 1768 (1) |
| 1995 | 985 (69) | 152 (55) | 1137 (67) | 324 (23) | 97 (35) | 421 (25) | 114 (8) | 25 (9) | 139 (8) | 1491 | 1488 | 1697 (1) |
Departures from special hospital
Deaths
Table 2 shows that between 1986 and 1995 142 deaths occurred (113 men (80%) and 29, women (20%)) among patients who were the responsibility of the special hospitals. Unnatural deaths (suicide, homicide, accidental and open verdicts) accounted for 33 (23%) of the deaths and ‘natural deaths’ for the majority (n=109, 77%). Annual rates as a proportion of the number of residents in the year were similar between years of the study, for both natural and unnatural deaths. Further details are available from the first author upon request.
Table 2 Number and percentage of all special hospital patients discharged (including deaths) in each study year

| Year of discharge | Deaths n | % | Remand discharges n | % | Other discharges n | % | Total discharged n |
|---|---|---|---|---|---|---|---|
| 1986 | 10 | 6.58 | 6 | 3.95 | 136 | 89.47 | 152 |
| 1987 | 13 | 7.34 | 6 | 3.39 | 158 | 89.27 | 177 |
| 1988 | 15 | 8.02 | 6 | 3.21 | 166 | 88.77 | 187 |
| 1989 | 13 | 6.37 | 13 | 6.37 | 178 | 87.25 | 204 |
| 1990 | 24 | 12.31 | 14 | 7.18 | 157 | 80.51 | 195 |
| 1991 | 13 | 7.07 | 16 | 8.70 | 155 | 84.24 | 184 |
| 1992 | 16 | 7.41 | 32 | 14.81 | 168 | 77.78 | 216 |
| 1993 | 15 | 5.77 | 27 | 10.38 | 218 | 83.85 | 260 |
| 1994 | 16 | 6.32 | 32 | 12.64 | 205 | 81.00 | 253 |
| 1995 | 7 | 3.36 | 33 | 15.86 | 168 | 80.76 | 208 |
| Total | 142 | 6.97 | 185 | 9.08 | 1709 | 83.93 | 2036 |
Remand orders
During the 10 years, 510 patients were detained in a special hospital on a court remand order (n=244: Section 35 (n=83), Section 36 (n=12) or 38 (n=149)) or a prison remand order (n=266; Sections 48 and 48/49). Over 70% of these episodes came in the last five years of the study. Four per cent of remand order admissions were of patients with an MHA classification of mental impairment. One hundred and thirty-one remand cases were under the MHA classification of psychopathic disorder, 121 of whom were detained under Section 38 after conviction for a criminal offence (and constituting 81% of all those who were received under Section 38). The remaining 359 patients (70% of the total remand cases) were detained under the mental illness classification of disorder. By the end of the study 232 of these patients were still resident in hospital, the majority, 93% (n=216) detained under hospital orders (Section 37±41 or Criminal Procedures (Insanity) Act (1964/1991)). Table 2 shows that 185 remand order patients, including 63 Section 38 subjects, had been discharged from hospital on their original order and had not returned within 28 days. These episodes are not considered further.
Discharges
With the above exceptions, all patients leave special hospital, after treatment, generally with clinical agreement that they no longer need high security; in restricted cases agreement is reached in conjunction with the Home Office. The total number of discharges after treatment constituted an increasing proportion of the available resident episodes from year to year over the 10-year period (odds ratio per year 1.04 (95% CI 1.03-1.06)). This overall trend, however, masks some variation in particular years (P=0.02, for years as 10-category variable compared to year as linear trend). There was a decrease in 1990-91, followed by a particularly large increase in 1992-93.
Types of discharge
For the majority of patients, the most likely placement on leaving special hospital was another institution (77%). Table 3 confirms that 410 people in all (24%) went directly back into the community, but 1068 (62%) went to another hospital and 209 (12%) back to prison. Community placement was usually in independent accommodation or residency supervised by paid workers (n=238 (56%)) and less often with family or close acquaintances (n=101 (25%)). In 80 cases the nature of the placement was not specified.
Table 3 Number of patients discharged from special hospital into various facilities (except remand order and death cases)

| Year discharged | Community | NHS | Prison | Total cases1 | |||
|---|---|---|---|---|---|---|---|
| M | F | M | F | M | F | ||
| 1986 | 32 | 7 | 64 | 20 | 11 | 136 | |
| 1987 | 34 | 9 | 85 | 14 | 15 | 1 | 158 |
| 1988 | 32 | 7 | 89 | 19 | 16 | 1 | 166 |
| 1989 | 25 | 9 | 90 | 36 | 14 | 1 | 178 |
| 1990 | 24 | 18 | 62 | 22 | 27 | 1 | 157 |
| 1991 | 28 | 18 | 60 | 24 | 21 | 2 | 155 |
| 1992 | 36 | 10 | 74 | 24 | 18 | 1 | 167 |
| 1993 | 33 | 14 | 114 | 25 | 29 | 1 | 218 |
| 1994 | 38 | 9 | 98 | 27 | 32 | 205 | |
| 1995 | 23 | 4 | 90 | 31 | 18 | 168 | |
| Total | 305 | 105 | 826 | 242 | 201 | 8 | 1708 |
The type of placement varied over time (P<0.001). Community discharges were more or less constant over the years: rate ratio 1.00 (95% CI 0.96-1.03, P=1.00), but discharges to another hospital increased significantly: rate ratio 1.4 (95% CI 1.01-1.06, P=0.006), these rates being similar for men and women. The number of men discharged back to prison also rose (rate ratio 1.08, 95% CI 1.02-1.14, P=0.01), notwithstanding the low figure in the last year of analysis. The numbers of women involved in prison transfers were too small for analysis.
Length of stay of discharged patients (excluding deaths and remand cases)
The median length of stay for patients discharged at any time during the 10 years studied was 6.3 years (mean 8.2 years, range 0.01-52.3). Women, with a median length of stay of 7.5 years (mean 10.1 years, range 0.03-52.3), tended to stay longer than men (median 7.0 years; mean 8.8 years, range 0.02-51.5). As median figures allow better for the variation within the groups, they were used in all other subsequent calculations. Between the mental disorder groups there was something of a hierarchy, with the small group of people detained under severe mental impairment staying longest (median 19.9 years, range 0.7-51.5), followed by those under mental impairment (median 8 years, range 0.2-40.6), and those in the mental illness category (median 6.1 years, range 0.03-44.7), while those with psychopathic disorder represented the shortest stay group (median 5.3 years, range 0.1-36.2).
The nature of the act that had precipitated admission appeared to have had little effect per se on the length of stay, but a criminal conviction was associated with shorter lengths of stay (median 7.0 years, range 0.01-42.9) than behaviour which had been contained within the health services, albeit inclusive of transfer to special hospital (median 10.8 years, range 0.2-52.3). The figures for length of stay by nature of detention order reflected this, with civil cases (Section 3) staying longer (median 10.4 years, range 0.38-42.9) than hospital order cases (Section 37±41 and Criminal Procedures (Insanity) Act) (median 7.3 years, range 0.08-34.2) and in turn sentenced prisoners (Section 47±49) (median 2.7 years, range 0.08-34.2). Analysis of variance of log-transformed length of stay showed significant differences for MHA classification of disorder and legal detention (P<0.01 in both cases). On controlling for these, there was no gender difference (P=0.6).
Trends in length of stay
When considering all patients discharged during the period, that is, regardless of admission date, the median length of stay remained constant year by year. However, taking only the subgroup of patients who were also admitted (excluding the remand order cases) within the study period (n=1691), there was evidence that the chance of being discharged increased slightly in each subsequent admission group. A Cox regression model of stay against year of admission showed that the rate of discharge increased with admission year (P=0.001, Hazard Ratio 1.06, 95% CI 1.02-1.09). Controlling for MHA classification of disorder, gender and legal form of detention as covariates confirmed this trend.
THE NET EFFECT ON ADMISSION AND DISCHARGE TRENDS
Figure 1 summarises the numbers of referrals, admissions (see companion paper pp. 253-259, this issue), discharge episodes and resident episodes in the special hospitals between 1986 and 1995. A reduction in the number of admissions and an increase in discharges have combined to account for the reduction of resident populations.
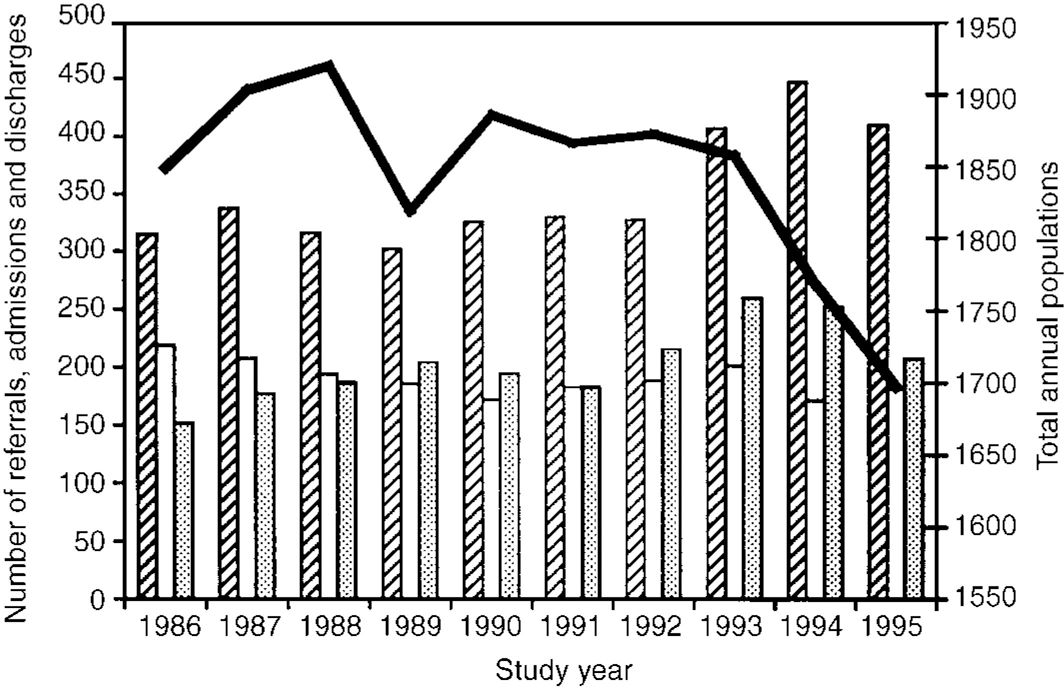
Fig. 1 Summary of special hospital referral, admission, resident population and discharge episodes. ▨, referrals; □, admissions; ▩, discharges; —, total population.
DISCUSSION
Trends in resident populations
Studies completed in the middle of the period studied here (Reference Maden, Curie and MeuxMaden et al, 1993; Reference Shaw, McKenna and SnowdenShaw et al, 1994; further details available from the first author upon request) suggested that no more than 50% of the resident patients needed high-security care, and yet the average increase in discharges of 4% per year over the period following these findings would not, even cumulatively, have achieved a comparable reduction in residency. By 1996, it was recognised that both research and clinical estimates of readiness for a lesser degree of security in these series might have been overstated. Reasons included documented pessimism about projected changes in mental state and the likelihood of deterioration under the stress of transfer (Reference Taylor, Maden and JonesTaylor et al, 1996). For the 10 years of this study, 10-15% of the people in the annual discharge cohorts were readmitted to special hospitals, the lower figure reflecting the later years, with shorter time at risk of return. Further, the figures do not take account of people who had returned during a period of trial leave, so they actually yield a considerable underestimate of returning patients.
Just as there appears to be a possibility that admission cases are becoming more challenging, it would seem that people for whom discharge cannot be achieved and discharged patients returning may result in a growing residual population, posing exceptional difficulties even by the standards required for detention in a special hospital. Increasing chance of discharge implies shorter lengths of stay for successive admission cohorts over the 10-year period, even when ‘remand only’ cases have been excluded from the calculations. The possible reasons for this were not tested in this study, but may included improved specific treatments for the majority of the mental illness group, for whom the diagnosis of schizophrenia is most common, and better liaison and planning for discharge in conjunction with colleagues elsewhere in the National Health Service (NHS) and social services under the Care Programme Approach. For planning purposes, all these issues have to be balanced against the small reduction in the size of the resident population.
Patient subgroup differences
The different patterns of discharge and length of stay for subgroups of patients were only partly expected. As noted, the Special Hospitals' Service Authority (SHSA) had set up a number of initiatives to reduce the number of resident women and mentally retarded individuals, and the timing of the most marked reductions in their numbers and proportions would suggest that the change was an effect of these initiatives. There was no plan to reduce the number of places for people with a personality disorder, and yet, save for the unlikely possibility that there was a considerable upsurge in the number of cases in which mental illness was used as the grounds for their detention (as happens in a minority of cases: Reference Taylor, Leese and WilliamsTaylor et al, 1998), admission episodes fell and discharges rose, with the inevitable effect on residency. Special hospitals would not have been immune to the growing general disquiet about the compulsory treatment in hospital of people with a personality disorder, but one of the special hospitals also faced specific criticisms in this regard. One major relevant official inquiry took place within the study period (Reference Blom-CooperBlom-Cooper, 1992), focused on Ashworth Hospital. Ashworth was disproportionately affected by a reduction in the number of patients resident under the psychopathic personality disorder category, but had started from a higher baseline (215 Ashworth residents with personality disorder in 1986; peak 234, in 1989; 175 in 1995; whereas Broadmoor had 107, a peak of 124 in 1994, and 116 in 1995, respectively; Rampton had 156, a peak of 157 in 1988/91, and 129 in 1995). In spite of psychiatrists' reluctance to provide for this group of people now extending to the special hospitals, a clinical need has been identified (Reference Gunn, Maden and SwintonGunn et al, 1991; Maden et al, Reference Maden, Curie and Meux1993, Reference Maden, Taylor, Brook and Gunn1995; Reference Taylor, Maden and JonesTaylor et al, 1996), the challenge will not go away, and the government is demanding a better health service response (Jack Straw, The Times, 31 October 1998).
The greater length of stay for the minority group of patients who had not been convicted of a criminal offence prior to admission to special hospital and were detained only under Section 3, without Home Office restrictions on discharge or transfer, at first sight seems counterintuitive. Nevertheless, this is consistent with an earlier study by Dell, in Reference Dell1980. It is probably partly related to the type of people most likely to be detained under this provision, viz. those with a learning disability. Alternative facilities are, if possible, even scarcer than for other patients. Perhaps the position becomes more understandable, however, if we remember that this group consists of people who had almost invariably been transferred to a special hospital from another NHS placement, when that had irretrievably broken down because of violence to other patients or staff. Memories are long, and with a shortage of psychiatric beds, these are perhaps the least welcome patients.
Changes elsewhere in the health service
The changes in numbers resident in special hospitals must also be considered as a possible reflection or effect of national changes elsewhere in the health services for England and Wales. We could not find figures for total bed occupancy in other health service facilities over the same period, but in any case, since all special hospital patients are compulsorily detained, it is probably more appropriate to consider them side by side with other detained patients. During the 10 years under study, the number of patients subject to civil detention orders increased considerably, nationwide and in all services. Focusing on treatment orders (Section 3 of the MHA), the only civil provision used at all regularly in the special hospitals, a 38% reduction in special hospital cases is in the opposite direction from the overall 75% national increase (2012 in 1986 to 9275 in 1995/96) (Department of Health, 1998).
In contrast, there has been an increase in all parts of the health service in the numbers of people detained under restriction orders (Sections 37/41, 47/49 and 48/49) (overall increase 41%, from 1758 to 2478) (Reference Kershaw and RenshawKershaw & Renshaw, 1997). Hospitals outside the high-security system have taken on an increasing proportion of cases, from 35% in 1986 to 50% in 1995; however, this burden is distributed across a large number of settings, so that the proportion of such patients resident in any one hospital other than the special hospitals remains very small. Within the special hospitals, the proportion of patients with restrictions placed on their discharge has risen from two-thirds to three-quarters of the annual resident populations, another likely indicator of increasing demands on special hospital staff. There has been an increase in the number of medium secure beds during this period, from 810 (1988/1989) to 1370 (1995/1996) (Department of Health, 1997). This may have contributed to shortening of the lengths of stay, partly through its impact on the stage of admission of criminal cases (patients are now more likely to have spent time in a secure unit first (see companion paper pp. 253-259, this issue), and partly through having the conditions and the staff able to accept patients at a notionally earlier stage of rehabilitation than other health service facilities.
In a study such as this, detail is inevitably sparse, but with the exception of the referrals data noted in the previous paper, it provides indicators of overall trends in special hospital use over the 10 years considered, and as such is likely to be a more reliable aid to service planning than either cross-sectional snapshots or estimates of need by researchers or clinicians which have hitherto been presented. This study and its companion paper suggest that both input and output changes are making the resident population more of a challenge.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Overall the number of discharges from special hospitals has increased both to prison, (almost invariably for prison transfers) and to other NHS (mainly mediumsecure) units. The number of discharges direct to the community has remained constant.
-
▪ Although overall trends in the length of stay of treated patients remained constant, taking only those patients also admitted within the study period, there were indications of a decrease in length of stay over time, from the proportion of such people in the later admission cohorts who were discharged.
-
▪ The length of stay for the group indicates the chronic nature of the presenting disorders. Long-term care is likely to be required after discharge from special hospital.
LIMITATIONS
-
▪ Referral data were not collected consistently over time and across sites, so that it is not possible to interpret accurately the apparent increase in 1993. Increases in referrals over time were consistent within each band of homogeneous data collected.
-
▪ Full clinical details of the patients referred and admitted to special hospital were unavailable. Therefore the Mental Health Act classification of disorder was used as a surrogate measure of mental disorder; however, it provides only an indicator of the complexity of diagnosis, and little data on severity.
-
▪ The nature of the study necessarily confined analysis to referrals and admissions of people already identified as likely to be suitable for a special hospital bed. Potentially suitable cases not recognised by prison doctors or psychiatrists can only be estimated from independent studies of other services.
APPENDIX
Glossary of powers of compulsory admission to hospital referred to in these papers
Mental Health Act 1983 : The most recent mental health legislation for England and Wales. Powers under this Act:
Transfers to hospital (no concurrent criminal offence) in the interests of the patient's health or safety or with a view to the protection of others.
Section 2 : Admission for assessment; and
Section 3 : Admission for treatment
Pre-trial derected transfers to hospital when charged with a criminal offence:
Section 35 : For report } From court,
Section 36 : For treatment } 12 weeks maximum
Section 48 : For urgent treatment (mental illness and severe mental impairment only) from prison; Secretary of State, Home Office authorisation; until trial.
Following conviction for an imprisonable criminal offence, except where life sentence mandatory
Section 38 : Interim hospital order (trial of treatment), six months' maximum (for the study period).
Section 37 : Hospital order, in lieu of sentence, six months, renewable.
Following conviction and imprisonment :
Section 47 : Transfer from prison to hospital; Home Office authorisation; until earliest release date, then notional Section 37 may be applied.
Restrictions on discharge : The court ( Section 41 ), in conjunction with a hospital order, or the Home Office ( Section 49 ) in connection with prison transfers, may impose restrictions on discharge from the order, such that the clinicians may not discharge without the approval of the Home Office or a mental health review tribunal chaired by someone with judicial experience.
Mental health review tribunal : A body independent of the hospital (or Home Office) authorities, consisting of a lawyer chairman, a doctor with special psychiatric expertise and a lay person, which may order the discharge of the detaining order.
Criminal Procedures (Insanity and Unfitness to Plead) Act 1991 : Allows determination in court of incapacity to stand trial or, where trial possible, a finding of ‘not guilty by reason of insanity’ with disposal according to demonstrated need and risk, which may include detention in hospital.
ACKNOWLEDGEMENTS
This paper could not have been written without the help of the Ashworth, Broadmoor and Rampton case register workers, Diane Fawcett, Mollie Jackson and Rita Dacey. Our thanks also go to Dana Ferraro for her help with this project. The authors also express their appreciation for the help and advice provided by Graham Dunn.







eLetters
No eLetters have been published for this article.