Post-traumatic stress disorder (PTSD) is the only psychiatric condition in DSM-IV (American Psychiatric Association, 1994) that requires a specific event to have occurred as a criterion for the diagnosis. The event should involve actual or threatened death, or serious injury. There is room for debate on how immediate this threat to life should be. Research in the past decade has shown that a long-term threat, as is the case with a terminal illness, can also give rise to PTSD (Reference Schut, de Keijser and Van den BoutSchut et al, 1991; Reference Cleiren, Diekstra and KerkhofCleiren et al, 1994; Reference Kelly, Raphael and JuddKelly et al, 1998; Reference Cordova, Studts and HannCordova et al, 2000; Reference Lindberg and WellischLindberg & Wellisch, 2004). This raises the question whether more common stressors such as chronic diseases and serious problems with work and relationships, which (by upsetting the normal order of things and the way we picture ourselves in our world) pose a threat to life in a more symbolic manner, also lead to the disorder. There is some evidence to support this hypothesis for employment-related problems and parental separation (Reference Ravin and BoalRavin & Boal, 1989; Reference Scott and StradlingScott & Stradling, 1994; Reference Joseph, Mynard and MayallJoseph et al, 2000). To investigate this issue further we compared PTSD symptoms in the general population after a range of traumatic events (DSM-IV criterion A1) with symptoms after more common events such as chronic disease, problems with relations, study or work (here called ‘life events’).
METHOD
Study design
A cross-sectional study design was used in which a random sample of adults from a family practice population completed a self-report questionnaire (Reference Mol, Dinant and Vilters-van MontfortMol et al, 2002). The family practice population in The Netherlands is representative of the general population, since practically every Dutch inhabitant is registered with a family practice.
Study population
The study recruited a random sample of the 67 500 patients registered with 12 practices and their 31 general practitioners. The practices participate in the Registration Network of Family Practices at the University of Maastricht in the province of Limburg. The population in this network resembles the population of The Netherlands as a whole in terms of age, gender, education, medical insurance and type of household (Reference Metsemakers, Höppener and KnottnerusMetsemakers et al, 1992).
The questionnaire was sent to 2997 patients randomly selected from the Registration Network, aged 20 years and over, with a covering letter inviting people with and without adverse experiences to participate. The questionnaires were completed between February and April 1997. Half of the questionnaires were returned (43% of respondents were men, mean age 50 years). The majority (85%) of the respondents lived with family or partner, 14% lived alone and 1% in other circumstances. A third (33%) had private health insurance and 67% had national health insurance; 44% had only primary education, 43% had completed secondary education and 13% had completed higher education. Except for insurance type, the demographic variables differed significantly (P<0.05) between respondents and non-respondents. The differences considered relevant were the following:
-
(a) gender (43% of the respondents were male v. 52% of the non-respondents);
-
(b) education (56% of respondents had secondary or higher education v. 44% of non-respondents);
-
(c) age (respondents were 2 years older on average, with an overrepresentation of those aged 60-70 years and under-representation of those aged 20-30 years).
Of 1498 respondents, 832 were eligible for the purpose of our study, the comparison of PTSD scores after traumatic v. life events. Reasons for exclusion were not having experienced any event, not having specified one's worst event or having chosen more than one worst event. Those whose worst event had happened in 1997 were also excluded, as some of these individuals could have been suffering from an acute stress disorder (symptoms of acute stress within 1 month of an event).
Measures
A questionnaire was developed covering demographic data and several health status correlates (use of medical care, drugs, alcohol and sedatives). This was followed by a checklist asking about personal experience - ‘ever in one's life’ - of accidents, burglaries, robberies, sexual or physical abuse (in childhood or adulthood), disaster or war, or chronic serious illness or sudden death of a loved one. The next questions were: ‘Are there other stressful events that you have not noted in this questionnaire up to now? If yes, please describe them below’ and ‘What was the worst event you experienced in your life? In which year did you experience this event?’ Next, the respondents were asked to fill out Part 3 of the Post-traumatic Stress Symptom Scale - Self-Report version (PSS-SR; Reference Foa, Riggs and DancuFoa et al, 1993), keeping this worst event in mind.
Part 3 of the PSS-SR consists of the 17 criteria on the three sub-scales for PTSD as listed in DSM-III-R or DSM-IV. There are five items on re-experiencing, seven on avoidance/numbing and five on arousal. The respondents were asked how often they had experienced each symptom in the past month (never, 0; a few times a month, 1; a few times a week, 2; a few times a day or continuously, 3). The first eight questions (five items on re-experiencing and three items on avoidance/numbing) explicitly ask about symptoms related to this worst event, e.g. ‘How often in the past month did you have bad dreams or nightmares about the event?’ The maximum score on Part 3 of the PSS-SR is 51. As the distribution of PTSD scores on the PSS-SR was skewed to the right, we performed a transformation: log10(total PTSD score +1), referred to as ‘log PTSD score’. The transformed score was our main outcome variable; when relevant it was converted back to the original score (geometric mean).
Criteria for missing values on the PSS-SR were the following: one missing value was allowed on each of the five-item sub-scales, and two missing values on the seven-item sub-scale (B. E. Foa, personal communication, 1997). The score filled in for the missing value was the average of the respondent's values on that sub-scale.
The PSS-SR was originally validated in two American samples - sexually abused women and a group of people who had experienced various forms of trauma (Reference Foa, Riggs and DancuFoa et al, 1993). The reliability of the Dutch version of the checklist, studied in patients referred to ambulatory care for symptoms of post-traumatic stress (n=63), showed Cronbach's α=0.88 for the total score (further information available from the authors upon request). In a sample of 113 Dutch women who had experienced a miscarriage, α=0.8 (Reference Engelhard, van den Hout and ArntzEngelhard et al, 2001). In our sample α=0.92 for the total score; for the three sub-scales of re-experiencing, avoidance and arousal α values were 0.83, 0.83 and 0.78, respectively.
Analysis
Based on the examples given in DSM-IV, the following were classified as traumatic events: accidents, robbery, sudden death of a loved one, murder or suicide of a loved one, physical or sexual abuse as an adult or child, disaster, war, learning about trauma experienced by a loved one and witnessing violence. Burglary without confrontation with the burglar, relational problems, problems with study or work, chronic illness or non-sudden death of a loved one and serious illness (self) were classified as life events. When it was not clear whether a death was sudden or not, it was classified as non-sudden.
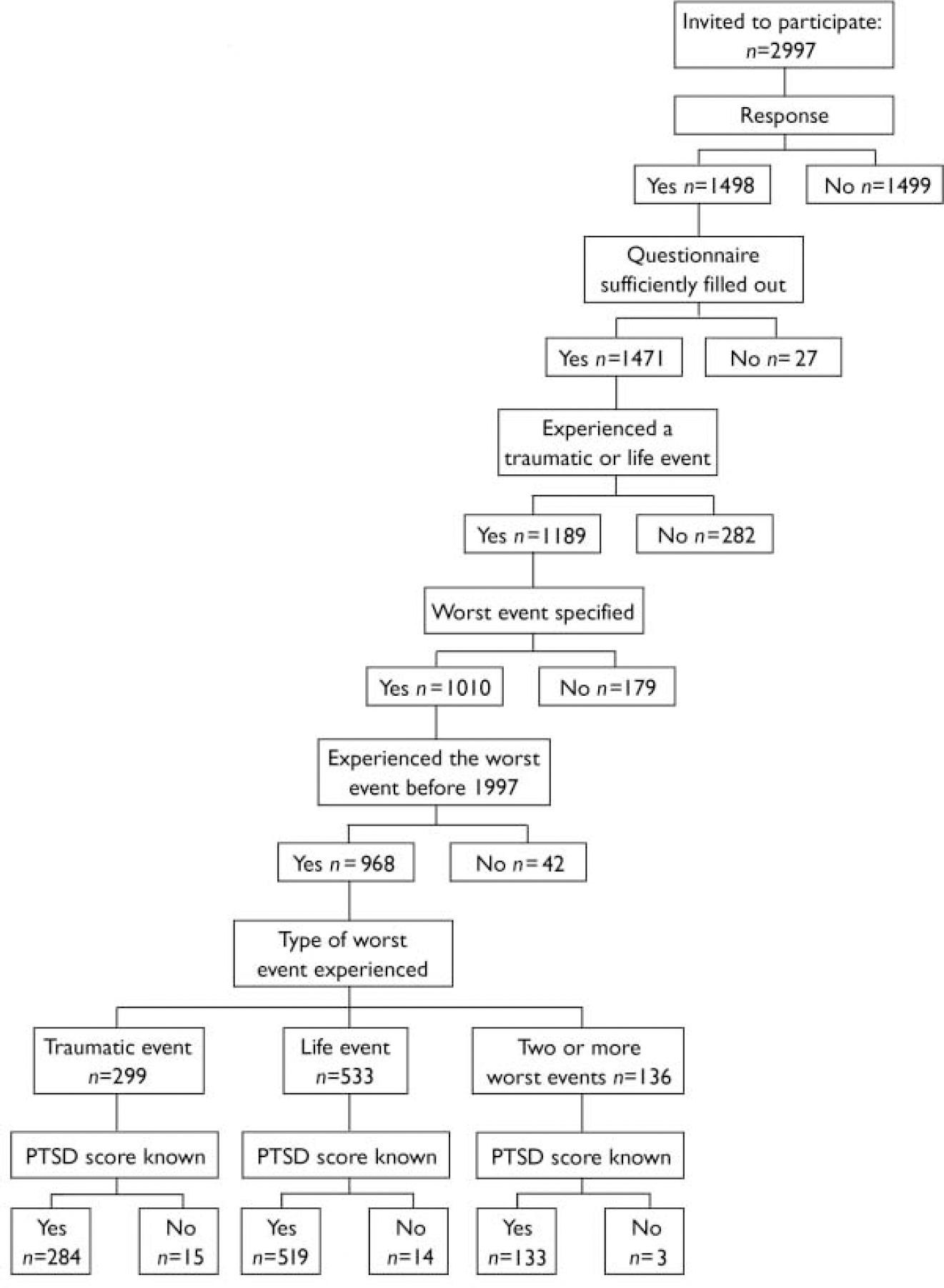
Fig. 1 Group allocation of respondents (PTSD, post-traumatic stress disorder).
The demographic characteristics and history of stressful events of the respondents in the traumatic events group and the life events group were compared, using t-tests and chi-squared tests for statistical significance. Log PTSD scores were calculated per type of event. Next, the mean log PTSD scores (total and three sub-scales) for the traumatic events group and life events group were calculated. This was followed by an analysis of covariance in which the mean log PTSD scores were again calculated, but were adjusted for differences between the two groups in terms of demographic factors and history of stressful events. All variables shown in Table 1 were included in the latter analysis.
Table 1 Demographic characteristics and history of stressful events: traumatic v. life events groups (n=832)

| Worst event was traumatic event (n=299) | Worst event was life event (n=533) | |
|---|---|---|
| Demographic factors (%) | ||
| Age, years1 | ||
| < 45 | 48 | 46 |
| 45-64 | 30 | 34 |
| > 64 | 22 | 20 |
| Gender1 | ||
| Men | 44 | 40 |
| Country of birth1 | ||
| Non-Dutch | 7 | 4 |
| Marital status1 | ||
| Single | 20 | 16 |
| Married | 67 | 68 |
| Divorced/widowed | 13 | 16 |
| Living situation1 | ||
| Living alone | 15 | 14 |
| With partner (and children) | 76 | 77 |
| One-parent family | 3 | 3 |
| Living with parents/family/home | 7 | 7 |
| Highest education1 | ||
| Lower | 41 | 35 |
| Middle | 28 | 32 |
| Higher | 32 | 32 |
| Occupation1 | ||
| Elementary | 13 | 14 |
| Lower | 30 | 28 |
| Secondary | 33 | 34 |
| Higher | 19 | 20 |
| Academic | 5 | 5 |
| History of stressful events | ||
| Confronted with other people's traumatic events and life events on a day-to-day basis1 | ||
| Yes (%) | 10 | 11 |
| Abused as a child (physically or sexually)1 | ||
| Yes (%) | 7 | 5 |
| Total number of traumatic events (PTSD-type) | 0.8 | 0.8 |
| excluding index event (mean n)2 | ||
| Years since worst event2** | 18 | 12 |
To see whether respondents from the traumatic events group would score significantly higher on certain items of the PSS-SR scale, and whether those from the life events group would score higher on other items, a non-parametric test (Mann-Whitney) was chosen (the distributions of the item scores were skewed to the right). Because of the large number of items (17), Bonferroni correction was done.
RESULTS
There were 299 respondents whose worst event could be classified in the traumatic events group and 533 in the life events group (Fig. 1). Table 1 shows the minor differences in demographic characteristics between the two groups. The only variable showing a statistically significant difference is years since the worst event: those whose worst event was a traumatic event experienced it 18 years ago on average, compared with 12 years for those whose worst event was a life event. Table 2 shows that, except for physical and sexual abuse - which lead to the highest PTSD scores - the scores for the traumatic events and the life events are in the same range.
Table 2 Total scores on Part 3 of the Post-traumatic Stress Symptom Scale per type of worst event (n=803)
| n 1 | Total log PTSD score2 (mean) | Original score (geometric mean) | |
|---|---|---|---|
| Traumatic events | |||
| Accidents | 42 | 0.53 | 2.4 |
| Sudden death of loved one (not murder, or unknown whether murder) | 142 | 0.58 | 2.8 |
| Witnessing violence | 4 | 0.60 | 3.0 |
| Disaster | 16 | 0.61 | 3.1 |
| Murder or suicide of loved one | 26 | 0.68 | 3.8 |
| War | 23 | 0.71 | 4.1 |
| Robbery | 5 | 0.88 | 6.6 |
| Physical abuse (adult) | 9 | 0.94 | 7.7 |
| Sexual abuse (adult) | 4 | 1.09 | 11.3 |
| Physical abuse or sexual abuse (child) | 13 | 1.09 | 11.3 |
| Life events | |||
| Burglary without confrontation of burglar | 11 | 0.54 | 2.5 |
| Death of loved one (non-sudden or unclear whether sudden or not) | 208 | 0.59 | 2.9 |
| Miscellaneous, not traumatic | 14 | 0.61 | 3.1 |
| (Chronic) illness of loved one | 95 | 0.71 | 4.1 |
| Serious illness (self) | 91 | 0.82 | 5.6 |
| Problems with study/work | 19 | 0.83 | 5.8 |
| Relational problems | 81 | 0.88 | 6.6 |
The average total PTSD score (Table 3) is higher for those whose worst event was a life event than for those whose worst event was a traumatic event. The three sub-scales follow the same pattern. None of the differences between the two groups is significant. Possibly the fact that the traumatic events, on average, happened earlier than the life events could explain this finding. To check for this, a post hoc analysis was done, comparing total log PTSD scores per group after stratification (before 1939, 1940-1945, 5-year strata for 1946-1995, 1996). For five out of the six strata before 1966, the average log PTSD scores are highest for the traumatic events. In contrast, from 1966 onwards the life events group had higher scores in all strata. The differences, however, were non-significant for each stratum (t-tests, P<0.05). Next, taking 1966 as a cut-off point, two new strata were formed. For events before 1966 the mean log PTSD scores were 0.78 and 0.56 for the traumatic and life event groups respectively (t=-1.9, d.f.=90, P=0.056). The relation reversed after 1966, the scores being 0.61 and 0.71 respectively (t=2.8, d.f.=703, P=0.006). Therefore, for events that happened in the past 30 years, current PTSD scores are higher in those whose worst event was a life event than in those whose worst event was a traumatic event.
Table 3 Mean crude log PTSD scores for the traumatic events and life events groups
| Worst event | Log PTSD scores1 | Original scores | |||
|---|---|---|---|---|---|
| Sub-scale A Re-experiencing | Sub-scale B Avoidance | Sub-scale C Arousal | Total | Total PTSD score (geometric mean) | |
| Traumatic event (n=284)2 | 0.29 | 0.33 | 0.42 | 0.64 | 3.4 |
| Life event (n=519)2 | 0.34 | 0.38 | 0.45 | 0.71 | 4.1 |
After adjusting for differences between the two groups in demographic factors and history of stressful events, the average PTSD score is significantly lower in the traumatic events group than in the life events group (estimated marginal means of log PTSD score 0.62 and 0.71 respectively; F=5.11, d.f.=685, P=0.024). This analysis was repeated for each of the two large strata (before and since 1966). This generates the following corrected scores: before 1966, traumatic event 0.70 and life event 0.68 (F=0.031, d.f.=65, P=0.86); since 1966, traumatic event 0.59 and life event 0.71 (F=7.8, d.f.=607, P=0.005).
Post hoc we postulated that there might be a difference in the distribution of the PTSD scores between the two groups, in the sense that there might be a number of people with very high PTSD scores from traumatic events. The maximum log PTSD scores were 1.67 (original geometric mean score 46) for the traumatic events and 1.64 (original geometric mean score 43) for the life events group. Our second approach was to count the number of persons in each of the two groups that scored higher than the 90th percentile score of the total group (log PTSD score 1.32, original geometric mean score 20). In the traumatic events group 10% scored higher than 1.32, compared with 11% in the life events group (χ2=0.065, d.f.=1, P=0.79). This indicates that among the respondents whose worst event was a life event, the top range of PTSD scores is reached as often as among the otherwise traumatised.
Another explanation for the PTSD score being higher in the life events group than in the traumatic events group was sought in our assignment of events to the categories. The sudden death category (categorised as a traumatic event) contained events of a wide range of severity, from witnessing a partner's violent death to hearing about the fatal heart attack of a relative. This could have decreased the PTSD scores in the traumatic events group. Therefore, the effect of assigning the sudden deaths to the life events group was studied: the total log PTSD score of the traumatic events group now rose above that of the life events (0.71 v. 0.68 respectively, t= -0.53, d.f.=801, P=0.60), as did the scores on the sub-scales. However, the difference was only significant for the arousal sub-scale (0.49 and 0.43 respectively; t= -2.1, d.f.=810, P=0.036). Another group of events, deaths about which it was not clear whether they had been sudden, had in the first instance been allotted to the non-sudden death category (life events). Therefore this group could include a number of sudden deaths too, disproportionately increasing the scores in the life events group. To check for this, the analysis was repeated putting all deaths (non-sudden and sudden) into the traumatic events group. This had a considerable effect: the total life events score rose to 0.77 on average, whereas the total traumatic events score fell to 0.62 (t=4.7, d.f.=801, P<0.01). In summary, whichever group the deaths are assigned to, the total PTSD scores of the life events group are no lower than those of the traumatic events group.
The mean ranks of all of the 17 PSS-SR items except three (Table 4: items 8, 16 and 17) are higher in the life events group. After Bonferroni correction none of the differences is significant. Therefore, none of the PTSD symptoms seems more typical for either traumatic or life events.
Table 4 Mean ranks of post-traumatic stress disorder scores per item, traumatic v. life events groups (n=803)
| Item | Traumatic events group | Life events group | |
|---|---|---|---|
| 1 | Upsetting thoughts or images about the event | 393 | 419 |
| 2 | Bad dreams or nightmares about the event | 409 | 411 |
| 3 | Reliving the event, acting or feeling as if it were happening again | 395 | 411 |
| 4 | Feeling emotionally upset when reminded of the event | 406 | 412 |
| 5 | Experiencing physical reactions when reminded of the event | 398 | 414 |
| 6 | Trying not to think about, talk about or have feelings about the event | 391 | 415 |
| 7 | Trying to avoid activities, people or places that are reminders of the event | 403 | 412 |
| 8 | Not being able to remember an important part of the event | 412 | 403 |
| 9 | Having much less interest or participating much less often in important activities | 399 | 415 |
| 10 | Feeling distant or cut off from other people | 398 | 410 |
| 11 | Feeling emotionally numb | 403 | 413 |
| 12 | Feeling as if future plans or hopes will not come true | 392 | 416 |
| 13 | Having trouble falling or staying asleep | 402 | 417 |
| 14 | Feeling irritated or having fits of anger | 396 | 413 |
| 15 | Having trouble concentrating* | 386 | 419 |
| 16 | Being overly alert | 409 | 403 |
| 17 | Being jumpy or easily startled | 413 | 402 |
DISCUSSION
Main findings
To our knowledge, ours is the first study in an adult population on the propensity of a range of severe difficulties in life that do not fulfil the DSM-IV PTSD stressor criterion A1 to give rise to PTSD symptoms. Our findings show that people from the general population whose worst event is a life event, such as chronic illness, marital discord or unemployment, on average have more PTSD symptoms from this event than people whose worst event is traumatic, such as an accident or disaster. As this is a rather unexpected finding, we have tried to refute it in several ways. After stratifying for the only difference found in demographic and trauma characteristics between the two groups - time since the event - we found that the finding holds true for events that occurred at some time in the past 30 years. This finding perhaps implies that in the very long run the impact of a life event wears out, in terms of PTSD, whereas that of a traumatic event is more persistent.
One could argue that the average difference in total PTSD score between the two groups, at 0.7 on the PSS-SR, is not clinically relevant. Yet, although this difference is indeed small, the finding remains curious as one would expect the life events group to have fewer, not more, symptoms. Also, as was shown by comparing the distributions of the PTSD scores, the scores at the top end of the range after both types of events are comparable. This means that considerable suffering results from both types of events in terms of PTSD.
Another explanation for our finding was sought in the allocation of those whose worst event was a sudden or a non-sudden death of a loved one to either the life events group or the traumatic events group. The results, however, did not counter our first finding.
If no difference could be found between the two groups in terms of total PTSD score there could still be a difference on the item level; perhaps some of the 17 symptoms of post-traumatic stress typically occur after life events and others after traumatic events. Our analyses showed that this was not the case.
Limitations of our study
The reliability of the PSS-SR checklist was found to be good in selected populations and it was also found to be reasonably predictive of PTSD diagnosed by interview (Reference Foa, Riggs and DancuFoa et al, 1993; Reference Engelhard, van den Hout and ArntzEngelhard et al, 2001). However, use in open populations has not been documented. The reliability in our sample, expressed as Cronbach's α, was good. However, as the PSS-SR checklist is a written questionnaire, we were unable to check whether the respondents understood all the items correctly. For example, the question about ‘reliving the event, acting or feeling as if it were happening again’ might be interpreted as actively remembering the event, rather than as an intrusive memory, by those who have never experienced a traumatic event. Another limitation of this study is that we did not confirm the occurrence of the events and symptoms, but relied on self-report.
We excluded all respondents who had chosen two or more worst events because the variable ‘number of years since the worst event’ could not be calculated in this group. Besides, we would have been unable to include those who had a worst event in each category in the item analysis, because it would not have been possible to tell to which type of event (life or traumatic) they were referring when responding to a particular item.
There may be complicated relationships between life events, traumatic experiences and general psychological distress. To name a few, life events and daily hassles might increase general psychological distress, which in turn might trigger PTSD symptoms related to an earlier trauma; or, experiencing a trauma might increase general psychological distress, reducing the capacity to deal with other life stressors, increasing in turn the level of general psychological distress. Both experience of a trauma and general psychological distress, separately or in interaction, might increase the risk of experiencing a trauma and of developing PTSD symptoms after a trauma or a life event. Our study was not designed to unravel these complicated relationships. Nevertheless, our finding that life events give rise to symptoms similar to those caused by traumatic events indicates that further study of the interaction of these factors is needed.
Although a higher response than 50% would have been preferable, our response rate is not unusual, taking into account the taboo around some of the topics in the questionnaire (Reference Koss, Woodruff and KossKoss et al, 1991). Also, the questionnaire was quite lengthy and complicated: besides a section on PTSD, there were questions about general health, and a detailed section about care sought and received for a number of traumatic events experienced by the respondent.
Another point to be considered is whether the non-response was selective. The questionnaire contained a list of eight traumatic events and only two life events (burglary and illness of a loved one), followed by an open question about other events experienced. If a person has experienced one event only, a mild life event, the memory of that mild event might not be evoked by the open question, and respondents might therefore not feel the questionnaire pertains to them personally. The memory of a severe life event might be evoked more easily, triggered by reading the list of mostly traumatic events. Non-response among those who had experienced a mild life event (other than burglary or illness of a loved one) might have ensued, resulting in relatively severe life events being reported. Yet we also know that some people prefer to avoid painful memories, and therefore people with severe life events might refrain from responding, countering the former effect. This would also hold true for the traumatic events: those without the experience of a traumatic event might think the questionnaire was not meant for them; those with such an experience might not want to be reminded of it and therefore not respond. Altogether, we have insufficient reason to think that there was a selection bias. Enhancing the total response in further research, however, is important.
Further research
To have a better idea of how patients interpret the questions of the PTSD checklist, for further studies an interview could be considered, although the costs in a population study would be tremendous. Questions on life events experienced, as well as daily hassles, should be included. Considering recent findings about the overlap of symptoms between patients labelled as having a depressive disorder and those suffering from PTSD (even for intrusive memories), including a depression scale would be important (Reference Reynolds and BrewinReynolds & Brewin, 1999). To enhance the response, paying home visits is a good option, as was shown in a Dutch mental health study (Reference Bijl, van Zessen and RavelliBijl et al, 1997).
Personality traits such as IQ and neuroticism have been shown to affect the development of PTSD after certain traumatic and life events (Reference McNally and ShinMcNally & Shin, 1995; Reference Engelhard, van den Hout and KindtEngelhard et al, 2003). It would be interesting to study whether the same relationship can be found after traumatic and life events in general.
Implications
Our study adds to the evidence that PTSD is perhaps not specific to A1 criterion traumatic events, but that it can also arise after life events. To quote Bremner:
‘There is a natural tendency to resist stress-related diagnoses, given their potentially explosive impact on societal approaches to responsibility and accountability. The challenge to our field is to find the appropriate balance’ (Reference BremnerBremner, 1999).
Should we now advise clinicians to ask about symptoms of post-traumatic stress after life events? Or should we reconsider the validity of the diagnosis of PTSD (Reference Kudler, Shalev, Yehuda and McFarlaneKudler, 2000)? It is too early for either of these actions, but our study does stress the importance of looking for more empirical evidence on the consequences of events other than typically traumatic ones, in terms of PTSD.
Acknowledgements
We thank the following people for their contribution to this study: Professor B. P. R. Gersons, Mrs V. Pigmans, Dr G. Hutschemaekers, and Mr W. van Duin (of the Achmea Foundation Victim and Society, which funded the study). We are also grateful to the participants for filling out the questionnaire.








eLetters
No eLetters have been published for this article.