Comprehensive analyses of suicides in Denmark show that people with severe mental illness form a particularly high-risk group. They also show that the greatest risk of suicide occurs just after admission to hospital or just after discharge and that the first year of treatment is associated with 60% increased risk of suicide. Individuals with first-episode psychosis comprise a greater risk of suicidal behaviour compared with the normal population (Reference Mortensen and JuelMortensen & Juel, 1993; Reference Nordentoft, Laursen and AgerboNordentoft et al, 2004; Reference Qin and NordentoftQin & Nordentoft, 2005).
Knowledge of risk factors for suicide is important in order to achieve better prevention.
It has previously been quoted that the lifetime risk of suicide in schizophrenia is 10% (Reference MilesMiles, 1977), but recent studies show that the risk is more likely to be somewhere between 4% and 6% (Reference Inskip, Harris and BarracloughInskip et al, 1998; Reference Palmer, Pankratz and BostwickPalmer et al, 2005).
The most accurate estimate of suicide risk in schizophrenia would be based on follow-up of first-episode individuals with schizophrenia so that bias is avoided from selection of the most severe cases and/or the survivors of the period with a high risk of suicide after first admission (Reference Inskip, Harris and BarracloughInskip et al, 1998).
Few randomised controlled trials (RCTs) have been conducted with the aim of reducing suicidal behaviour in schizophrenia, and there is hardly any evidence proving the effect of interventions on suicidal behaviour and mortality. This problem is partly due to the fact that studies would need high numbers of participants to show a significant, clinically relevant difference between two or more treatment groups. If suicide is the outcome, and integrated treatment were to reduce suicide rate from 4% to 2%, 1522 participants would be needed in each treatment group to detect with a power (β) of 0.90 and a significance level of (α) 0.05 (Reference PocockPocock, 1996).
The OPUS study investigates a large incidence cohort with good representativity, standardised and comprehensive assessments by validated psychometric instruments, and complete register-based follow-up of suicides and deaths. To our knowledge, the present study is the largest prospective 5-year follow-up of an incident cohort of individuals with schizophrenia-spectrum psychosis that investigates the risk factors and rates of suicidal behaviour and death.
Within the RCT of 2-years of integrated treatment v. standard treatment, we examined suicidal behaviour, suicides and death as secondary outcome measures.
Some risk factors are similar in the normal population to those in schizophrenia, but there are also risk factors that are specific to the group with schizophrenia, and there are some risk factors in the normal population that do not seem to be present for people with schizophrenia (Reference Hawton, Sutton and HawHawton et al, 2005). Hawton and colleagues found in their review that the differences between men and women with schizophrenia who commit suicide are much smaller than in the normal population. Furthermore, married or cohabiting individuals with schizophrenia do not seem to have a lower risk of suicide than those with the same status in the normal population. Nor do those who are single or divorced have a greater risk, as is the case in the normal population. For the schizophrenic group, Hawton's review discloses that hopelessness and depressive symptoms, suicidal thinking and suicidal attempts, agitation and motor restlessness, fear of mental disintegration, poor adherence to treatment and recent loss were the strongest risk factors, as was drug (but not alcohol) misuse.
A review of risk factors for suicide attempt in schizophrenia identified past or recent suicidal ideation, previous deliberate self-harm, past depressive episode, drug misuse or dependence, and higher mean number of psychiatric admissions as predictors (Reference Haw, Hawton and SuttonHaw et al. 2005). Haw concludes that large prospective studies of deliberate self-harm in schizophrenia are needed to further define risk factors and to build on the findings of their review.
Already published data show that the integrated treatment has positive effects on psychotic and negative symptoms, substance misuse, use of bed days and client satisfaction at first-and second-year follow-ups (Reference Petersen, Jeppesen and ThorupPetersen et al, 2005).
The focus of this paper is on suicidal ideation and behaviour at 1-year and 2-year follow-up, and suicide and death at 5-year follow-up. We hypothesise that (a) there is an increased risk of suicide in our first-episode sample compared to the normal population, (b) integrated treatment was able to inhibit or postpone death by suicide and suicide attempts, and (c) suicidal thoughts and plans, depressive symptoms and drug misuse predicts suicidal attempts at 1-year and 2-year follow-up.
METHOD
Participants
Participants were included from all inpatient and out-patient mental health services in Copenhagen (Copenhagen Hospital Corporation) and Aarhus County. From January 1998 until December 2000, 547 participants aged 18–45 years with a diagnosis in the schizophrenia spectrum (F2 according to ICD–10 research criteria; World Health Organization, 1992) and no exposure to antipsychotic medications exceeding 12 weeks of continuous medication were included in the trial. The local ethics committee approved the trial.
All participants were centrally randomised to integrated treatment or standard treatment. In Copenhagen, randomisation was carried out through centralised telephone randomisation at the Copenhagen Trial Unit. The allocation sequence was computer generated, 1:1, in blocks of six, and stratified for each of five centres. In Aarhus, the researchers contacted a secretary by telephone when they had finished the entry assessment of the participants. The secretary drew one lot from among five red and five white lots out of a black box. When the block of 10 was used, then the lots were redrawn. Block sizes were unknown to investigators.
Interventions
The trial is pragmatic, comparing integrated treatment as defined by a set of protocols v. treatment as usual (Reference Roland and TorgersonRoland & Torgerson, 1998).
Integrated treatment
Integrated treatment can be defined as an assertive community treatment model with family involvement and social skills training. Two multidisciplinary teams in Copenhagen and one in Aarhus were established and trained to provide integrated treatment. Case-load reached a level of approximately 10. Each participant was offered integrated treatment for a period of 2 years. A primary team member was designated for each participant who was then responsible for maintaining contact and co-coordinating treatment within the team and across different treatment and support facilities. The participants were visited in their homes or other places in their community, or they were seen at the office, according to their preference. During hospitalisation, treatment responsibility was transferred to the hospital, but a team member visited the participant once a week. A crisis plan was developed for each participant. If they were reluctant about treatment, the team stayed in contact with them and tried to motivate them to continue treatment.
Psychoeducational family treatment according to McFarlane's manual for Psychoeducational Multiple-Family Group Treatment (Reference McFarlane, Lukens and LinkMcFarlane et al, 1995) was offered, and team members always tried to make contact with at least one family member and motivate participants and families to participate in a psychoeducational group.
Participants with impaired social skills were offered social skills training, focusing on medication, coping with symptoms, conversation, and problem-solving skills in a group of maximum 6 participants and 2 therapists (Reference Liberman, Mueser and WallaceLiberman et al, 1986).
Standard treatment
Standard treatment usually offered the participant was treatment at a community mental health centre. Each participant was usually in contact with a physician, a community mental health nurse, and in some cases also a social worker. Home visits were possible, but office visits were the general rule. A staff member's case-load in the community mental health centres varied between 1:20 and 1:30.
Transition from integrated treatment to standard treatment for the intervention group
After 2 years of integrated treatment participants from the intervention group were transferred to standard treatment; for a few participants this implied only their GP. The transition to standard treatment was carried out gradually and as gently as possible, but naturally the break of relationship with the contact person in the OPUS team, and the lower intensity of contact in standard treatment could have caused feelings of loss for several participants.
Antipsychotic medication
Participants in both treatment groups were offered antipsychotic medication according to guidelines from the Danish Psychiatric Society, which recommend a low-dose strategy for individuals with first-episode psychosis and use of second-generation antipsychotic drugs as first choice.
Assessments
Only independent investigators were involved in follow-up interviews at 2 years. For practical reasons, they could not be kept blind for treatment allocation. At entry and 1-year follow-up, 2-year follow-up and 5-year follow-up, we carried out a comprehensive assessment. For this study, the following collected assessments are important: main diagnosis and comorbidity based on Schedule for Clinical Assessment in Neuropsychiatry (SCAN 2.0, SCAN 2.1 since 1999) (World Health Organization, 1998), Scale for Assessment of Positive Symptoms and Scale for Assessment of Negative Symptoms (SAPS and SANS; Reference Andreasen and OlsenAndreasen & Olsen, 1982), socio-demographic factors, Global Assessment of Functioning, suicide attempts and suicidal ideation based on self-reporting (Reference Nordentoft, Jeppesen and AbelNordentoft et al, 2002), and duration of untreated psychosis as assessed with Interview for Retrospective Assessment of Onset of Schizophrenia (Reference Hafner, Riecher-Rossler and HambrechtHafner et al, 1992).
Using algorithms based on ratings of definitely present selected items in the section in SCAN covering depressed mood and ideation, thinking, concentration, energy, interests, and bodily functions, it was investigated whether patients fulfilled general criteria for depression in ICD–10.
Information on mortality was collected from the cause of death register and death certificates were obtained for 15 of the 16 participants who died during the period up to the 5-year follow-up. Full medical records were used as a source of data with regard to service use, medication and treatment adherence.
All investigators were trained in the SCAN interview at the WHO Collaborating Centre and trained bimonthly in SAPS with live interviews.
At 1-year follow-up, drop out was positively associated with allocation to standard treatment, foreign citizenship, higher age and non-compliance with antipsychotic drugs. Factors associated with lower attendance at 2-year follow-up were standard treatment, living in Copenhagen, harm and dependence syndrome, having only secondary school education and not having obtained an interview with a relative at entry. When examining the participants who had not given information about suicidality, we found no significant associations, the group giving information on suicidal ideation and behaviour being representative for the entire sample.
Statistical methods
All tests were two-tailed at P=0.05. The univariate relationships between the clinical and demographic characteristics 1 year prior and outcome regarding suicidal plans and attempts at 1-year and at 2-year follow-up were analysed by logistic regression analysis (Table 2). The suicidal behaviour at 1 year and at 2 year were modelled with logistic regression analysis with stepwise backward regression (Wald test) to evaluate the independent, predictive value of gender, age, depression, hopelessness, psychotic symptoms, negative symptoms, disorganised symptoms, treatment site, being a parent, being single, employment, duration of untreated psychosis, having ever attempted suicide, having suicidal thoughts and having had suicidal plans at least once in the past week. Since the examined predictors of suicidal plans and attempts at follow-up were rated 1 year earlier, we modelled the suicidal behaviour after 1 year by the clinical and social status at entry; and the suicidal behaviour after 2 years by the clinical and social status at 1-year follow-up. Cox regression was used to examine suicide and mortality at 5-year follow-up, using the same covariates as for Table 2.
Table 2 Univariate and multivariate backwards stepwise regression models.

| Suicidal plans in past year, 1-year follow-up | Suicidal attempts in past year, 1 year follow-up | Suicidal plans in past year, 2-year follow-up | Suicidal attempts in past year, 2-year follow-up | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate | Multivariate | Univariate | Multivariate | Univariate | Multivariate | Univariate | Multivariate | |||||||||
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| Male | 0.72 | (0.47-1.08) | 0.44 | (0.23-0.83) | 0.65 | (0.40-1.08) | 0.44 | (0.2-0.98) | ||||||||
| Age (increasing) | 0.94 | (0.91-0.97) | 0.94 | (0.88-0.99) | 0.96 | (0.92-1.01) | 0.96 | (0.89-1.03) | ||||||||
| Hopelessness | 1.59 | (0.91-2.77) | 1.45 | (0.63-3.32) | 2.25 | (1.19-4.28) | 2.1 | (0.84-5.27) | ||||||||
| Depression | 1.16 | (0.74-1.83) | 1.54 | (0.78-3.02) | 2.55 | (1.46-4.45) | 4.62 | (2.1-10.17) | 2.84 | (1.17-6.72) | ||||||
| Psychotic symptoms | 0.93 | (0.81-1.07) | 1.12 | (0.09-1.4) | 1.31 | (1.09-1.57) | 1.33 | (1.02-1.74) | ||||||||
| Disorganised symptoms | 0.89 | (0.72-1.11) | 0.62 | (0.41-0.93) | 0.92 | (0.58-1.44) | 0.85 | (0.42-1.74) | ||||||||
| Negative symptoms | 0.87 | (0.73-1.05) | 0.91 | (0.69-1.20) | 0.59 | (0.36-0.97) | 1.12 | (0.9-1.4) | 1.06 | (0.76-1.48) | ||||||
| Standard treatment | 0.98 | (0.65-1.48) | 0.96 | (0.51-1.73) | 1.29 | (0.87-2.12) | 1.44 | (0.67-3.1) | ||||||||
| Harm or dependence | 1.48 | (0.93-2.33) | 1.59 | (0.81-3.06) | 0.82 | (0.42-1.6) | 1.8 | (0.76-4.3) | ||||||||
| Suicidal thoughts1 | 4.07 | (2.5-6.63) | 4.79 | (2.25-10.17) | 2.6 | (1.32-5.13) | 3.36 | (1.87-6.03) | 4.1 | (1.82-9.31) | ||||||
| Suicidal plans1 | 3.66 | (1.91-7.0) | 2.31 | (1.02-5.26) | 4.61 | (1.46-14.5) | 7.01 | (4.06-12.1) | 5.11 | (2.76-9.45) | 10.6 | (3.93-29.05) | 5.12 | (1.68-15.58) | ||
| Attempted suicide in past year | 1.2 | (0.64-2.25) | 0.89 | (0.35-2.25) | 5.7 | (2.71-12.2) | 2.45 | (1.04-5.74) | 11.3 | (4.77-27.2) | 4.36 | (1.63-11.6) | ||||
| Employment | 1.28 | (0.83-1.97) | 1.74 | (0.85-3.57) | 1.68 | (0.97-2.9) | 1.24 | (0.54-2.85) | ||||||||
| Being a parent | 0.97 | (0.53-1.77) | 2.55 | (1.23-5.29) | 1.93 | (0.98-3.79) | 1.33 | (0.47-3.69) | ||||||||
| Being single | 1.45 | (0.59-3.5) | 0.48 | (0.17-1.35) | 0.91 | (0.34-2.4) | 2.19 | (0.28-16.9) | ||||||||
| Duration of psychosis | 0.94 | (0.85-1.04) | 1.07 | (0.91-1.26) | 0.92 | (0.81-1.04) | 0.89 | (0.74-1.08) | ||||||||
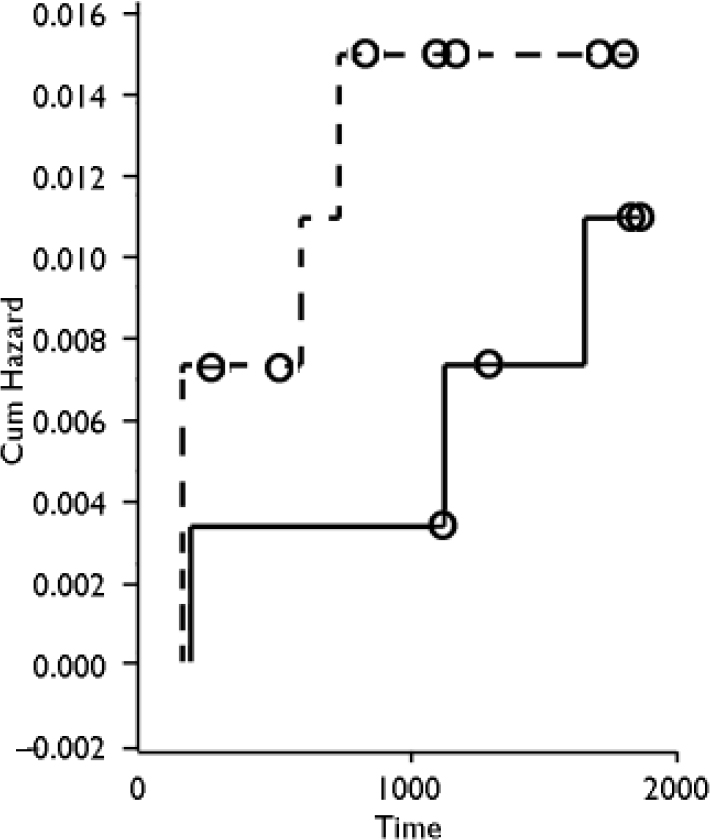
Fig. 1 Probability of death by suicide in the two treatment groups as a function of time (days). Treatment groups: —, standard treatment; —, integrated treatment; o, censored.
All statistical analysis was performed using SPSS 11.0 for Windows.
If it were to be possible to detect a clinically significant difference in mortality between 2% and 4% using Pocock's formula (Reference PocockPocock, 1996), 1522 patients would be required for each study group.
The study has sufficient power to detect a difference in proportion attempting suicide. With an α=0.05 and β=0.90, a sample of 184 patients in each treatment group is necessary to detect a difference of 5% v. 15%. Thus, the study has enough power to detect large differences in suicide attempts during the period studied.
RESULTS
Figures 1 and 2 show times of death and suicide over the 5-year period. Sixteen people had died, 7 of them from suicide, 1 from natural causes; 2 died by accident, and 6 deaths were unaccounted for or it was not possible to determine manner of death.
Of the suicides in the integrated treatment, 1 took place only 4 months after entry, whereas the other 2 suicides happened after 3 years and 4 years, thus after the 2 years of integrated treatment had ended.

Fig. 2 Probability of death (all causes) in the two treatment groups as a function of time (days). Treatment groups: —, standard treatment; —, integrated treatment; o, censored.
In the standard treatment, all 4 suicides happened during the first 2 years: 2 suicides happened after 4 months, the next after 1 year and 6 months, and the fourth 1 year and 9 months after entry.
Table 1 shows the basic characteristics of the population at entry. At entry, 547 patients were included, of which 419 were interviewed again 1 year later and 369 after 2 years.
Table 1 Socio-demographic and clinical characteristics among 547 participants with first-episode psychosis at baseline

| Baseline | |
|---|---|
| Socio-demografic characteristics | |
| Males, n (%) | 323 (59) |
| Age, years: mean, (s.d) | 26 (6.3) |
| 11, 12 or 13 years school education, n (%) | 181 (33.1) |
| Married, n (%) | 30 (5.5) |
| Being a parent, n (%) | 79 (14.4) |
| Employment or under education, n (%) | 168 (30.7) |
| Clinical characteristics | |
| Schizophrenia, n (%) | 362 (66.2) |
| Depression as comorbidity | 139 (25.4) |
| Harm or dependence syndrome as comorbidity | 146 (26.7) |
| Psychotic dimension, mean (s.d.) | 2.6 (1.4) |
| Negative dimension, mean (s.d.) | 1.0 (0.94) |
| Disorganised dimension, mean (s.d.) | 2.1 (1.1) |
| Suicidal behaviour and ideation | |
| Suicidal thoughts at least once last week1 | 123 (22.5) |
| Suicidal plans at least once in past week1 | 54 (9.9) |
| Suicide attempt last year1 | 100 (18.3) |
| Suicide attempt ever1 | 154 (28.2) |
| Hopelessness, moderate or severe1 | 78 (14.3) |
| Standard treatment, n (%) | 272 (49.7) |
| DUP weeks, mean, median, (IQR) | 103, 31 (4.2, 120.3) |
Figure 3 shows the distribution of suicidal ideation and behaviour from entry to 2-year follow-up. It is noteworthy that at entry as many as 18% of participants had attempted suicide during the past year, and 28% had done so at some point in their lifetime. Though not significant, it seems that these figures decrease after 1 year and again after 2 years. There were no significant differences between treatment groups with regard to suicidal thoughts, plans and attempts after 1 and 2 years.
Table 2 shows that having had suicidal ideation (i.e. plans and thoughts) predicted suicidal plans and attempts at 1-year follow-up. Being a parent was associated with increased risk of suicide attempts at 1 year. Young age predicted suicidal plans and attempts, meaning that the risk for having suicidal plans or attempts at 1 year decreases by 6% per year.
Male gender and disorganised symptoms were inversely associated with suicide attempts at 1 year, seemingly having a protective effect on suicidal attempts. Entering all variables into the multivariate analysis, only having suicidal thoughts predicted suicidal plans at 1-year follow-up; and suicidal plans predicted suicide attempts at 1 year. Negative symptoms were inversely associated with suicide attempts at 1 year in the multivariate analysis, but since the univariate is not significant, this estimate must be interpreted with caution.
After 1 year of treatment, we looked at the same predictive factors again, and a strong association was found between depression, suicidal thoughts, plans and previous attempts with regard to suicidal plans and attempts at 2 years, both in the univariate and the multivariate analyses. There was the same trend of younger age being predictive of suicidal plans and attempts, and also female gender continued to have a higher risk of attempting suicide at 2 years.
The psychotic dimension was analysed for hallucinations and delusions separately (not shown), and showed hallucinations to be significant with regard to suicidal plans and attempts at 2 years (OR 1.3 (95% CI 1.12–1.53), 1.32 (1.05–1.65)). The fact that this is significant at 2-year follow-up indicates that the patients that are difficult to treat are also most likely to be the patients at highest risk of having suicidal plans and attempts.
Table 3 examines suicide and overall mortality at 5-year follow-up. It was not possible to find any significant effect of treatment, risk factors such as gender, age, duration of untreated psychosis, depressive symptoms, the degree of psychotic and negative symptoms, socio-demographic issues, or harm and dependence at entry, because of lack of power. Though not significant, it seems that being male and having misused drugs are associated with death at 5-year follow-up. Also, there seems to be an association between young age and suicide and death (OR 0.98 and 1.02). Age in the normal population shows an OR of 1.09, which reflects that overall risk increases with age. Though not significant, there is a trend towards a higher risk of suicide and death at younger age.
Table 3 Survival analysis of suicide and death at 5-years follow-up

| Suicide 5-year follow-up Univariate | Death 5-year follow-up Univariate | |||
|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | |
| Male | 3.5 | (0.41-3.0) | 3.05 | (0.87-10.7) |
| Age (increasing) | 0.95 | (0.82-1.1) | 1.02 | (0.95-1.09) |
| Hopelessness | 1.45 | (0.16-12.9) | 1.44 | (0.4-5.13) |
| Depression | 1.87 | (0.31-11.2) | 1.4 | (0.48-4.11) |
| Psychotic symptoms | 1.42 | (0.76-2.64) | 0.95 | (0.68-1.33) |
| Disorganised symptoms | 0.85 | (0.34-2.12) | 0.97 | (0.58-1.65) |
| Negative symptoms | 1.71 | (0.81-3.59) | 1.35 | (0.86-2.13) |
| Harm or dependence | 2.79 | (0.56-13.8) | 2.17 | (0.81-5.84) |
| Standard treatment | 1.02 | (0.2-5.0) | 1.71 | (0.62-4.7) |
| Suicidal plans | 1.52 | (0.17-13.0) | 2.08 | (0.58-7.4) |
| Suicidal thoughts | 0.55 | (0.06-4.7) | 0.74 | (0.2-2.68) |
| Suicide attempt ever before | 1.12 | (0.2-6.12) | 1.68 | (0.58-4.85) |
| Attempted suicide in past year | 0.69 | (0.08-5.9) | 0.57 | (0.12-2.58) |
| Employment | 1.06 | (0.19-5.81) | 0.71 | (0.22-2.2) |
| Being a parent | 0.85 | (0.1-7.34) | 0.51 | (0.16-1.59) |
| Being single | 3.38 | (0.34-23.9) | 0.97 | (0.58-1.65) |
| Duration of psychosis | 1.22 | (0.79-1.88) | 1.21 | (0.92-1.59) |
Predictors of suicide and death were examined by univariate analysis only; because of the relatively small numbers of death and suicide, a multivariate analysis was not appropriate.
DISCUSSION
Standard mortality rate was 11 compared to the general population in Copenhagen and Århus County, aged 18–45 years. A 100% follow-up rate on suicide and death at 5-year follow-up of the OPUS cohort revealed that 16 people had died, 7 from suicide. We were not able to detect a significant difference between suicide and mortality between the two treatment groups; thus, integrated treatment was not able to postpone or inhibit suicide or suicide attempts. The strongest predictors for suicidal plans and attempts were previous suicide attempts, suicidal thoughts and plans, depressive symptoms, female gender and young age. We did not find that drug misuse was a predictive factor for suicide attempts at 2-year follow-up.
Limitations
Suicide is a rather uncommon event, therefore, even in the normal population, it is very difficult to make predictions about it, owing to the large sample sizes needed.
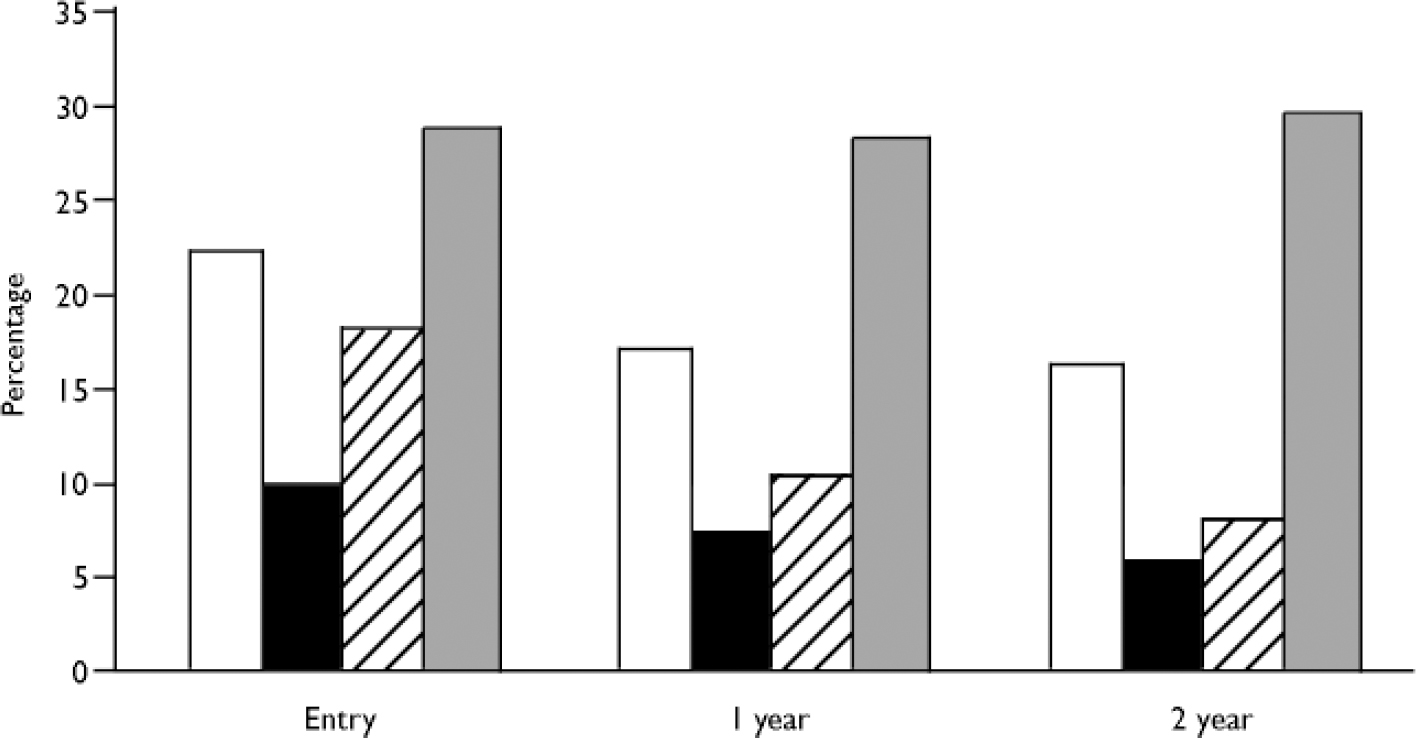
Fig. 3 Suicidal ideation and behaviour at entry, one year and two years.□,
suicidal thoughts;▪, suicide plans; ![]() , suicide attempts in past year; ░, suicide
attempts ever before.
, suicide attempts in past year; ░, suicide
attempts ever before.
Previous published data on the OPUS trial have shown positive effects on a number of outcomes (Reference Petersen, Jeppesen and ThorupPetersen et al, 2005). It could be anticipated that these promising results would also influence suicide and overall deaths, but our study does not have the necessary power to detect possible differences between the two treatment groups.
In examining the death certificates, the manner of death of 6 patients was classified as unknown. It is very likely that 2 or 3 of the 6 deaths were actually suicides.
Assessing suicidal ideation and behaviour, raters were not blind to treatment allocation, which could have biased the results. Furthermore it is possible that suicidal ideation and attempts are under-reported in the standard group, because the patients in the standard group were not followed so closely as the integrated group, leaving some doubt as to whether some suicide attempts could have been forgotten or reported in a wrong time period.
Finally, suicide attempts were based on the interviews we made with the participants and were not in all cases confirmed by medical records.
Predictors of suicide, suicidal ideation and behaviour
We found no significant predictors of suicide and deaths after 5 years. The manner of death of 6 people was unexplained, but from reading through the death certificates, it was found that several of these individuals had died from drug misuse, making it difficult to determine whether the manner of death was an accident or perhaps suicide. On the other hand, there was no doubt about the 7 suicides, as they were all carried out with very violent methods.
The risk factors found in our study are in accordance with the findings from Haw's review (Reference Haw, Hawton and SuttonHaw et al, 2005); we also found that previous suicide attempts, suicidal ideation and behaviour, and depressive symptoms were strong predictors for suicide attempts. Furthermore, we found psychotic symptoms, especially hallucinations, to be predictive of suicide attempts at 2-year follow-up, which has not previously been shown. The fact that psychotic symptoms became significant after 1 year of treatment indicates that those individuals who are difficult to treat, and thus are still experiencing hallucinations after 1 year of treatment, are at higher risk of suicide attempts 2 years later. This stresses the need for closer attention to be paid to this subgroup of individuals.
Examining the predictive values over time, it became clear that in spite of crisis plans being worked out for all participants in integrated treatment, suicidal ideation and behaviour were still strong predictors for suicide attempts, stressing that those individuals who continuously report suicide thoughts and plans should be taken seriously, since this comprises an actual risk. This finding indicates that it is a very complex task to develop specific and appropriate preventive treatment for suicidal ideation and behaviour in this group of individuals with first-episode psychosis, and that, unfortunately, integrated treatment did not succeed in protecting the participants from this serious risk.
There was a trend towards a higher risk of suicide and death at a younger age compared to the normal population, where the risk for suicide per year a person becomes older is higher. This is in line with the findings from Qin and colleagues (Reference Qin and NordentoftQin & Nordentoft, 2005) and indicates that there is a need to pay particular attention to young individuals with first-episode psychosis.
The finding that being a parent is a risk for suicide attempts is contrary to the risk found in the normal population, where this is usually a protective factor for suicide attempts. Examining the data revealed that a majority of the participants counted as parents in our study did not actually live together with their children, because in many cases the women had their children taken away from them, and most often the men did not live with their offspring. This raises the question about what is the protective factor of being a parent. Our findings suggest that being a parent is perhaps only protective against suicide when the parents experience having daily contact with their children and the responsibility for their everyday life and well-being. Furthermore, only 14% of the cohort was a parent at entry, which makes it possible that the participants not living with their children, owing to severe illness, distort the results.
Our finding that suicidal ideation and behaviour, depressive and psychotic symptoms, young age and female gender continue to be strongly associated with suicidal plans and attempts even after 1 year of treatment stresses the fact that there is a need for future development of special treatment programmes focused on suicidal ideation and behaviour, wherein specific crisis plans are worked out for the person individually. Also, there is still a need for interventions aimed at this high-risk group of individuals with first-episode psychosis.
Acknowledgements
The OPUS project was funded by grants from the Danish Ministry of Health (jr.nr. 96-0770-71), the Danish Ministry of Social Affairs, University of Copenhagen, Copenhagen Hospital Corporation, Danish Medical Research Council (jr. nr. 9601612 and 9900734), Slagtermester Wørzners Foundation and Stanley Research Foundation. Philip Hougaard supervised the statistical analyses.









eLetters
No eLetters have been published for this article.