
A diagnostic construct in psychiatry ideally should: (a) have some link with a measurable phenotype that exists in nature; (b) be valid in the classic sense of combining aetiological, symptomatic, prognostic and treatment specificity, setting it apart from other disorders; and (c) be useful and acceptable. Previous authors have argued that these three elements in combination do not apply to the diagnostic construct of schizophrenia. Reference Brockington1,Reference Kendell and Jablensky2 The question, therefore, arises whether anything has changed and, if it has not, whether schizophrenia should continue to feature in DSM–V and ICD–11.
How does psychosis exist in nature and how does this relate to schizophrenia?
The various definitions of schizophrenia and related disorders in DSM, ICD, Research Diagnostic Criteria (RDC) and other classification systems in practice combine a mix of positive, negative, cognitive, depressive and manic symptoms in the context of need for care (formal or informal). However, the symptoms that characterise patients with psychosis seen in mental health clinics are also prevalent in the community. A recent meta-analysis reported prevalence rates (around 8%) and incidence rates (around 3%) of positive psychotic experiences that are around 10 (prevalence) and 100 (incidence) times greater than reported rates for psychotic disorder. Reference van Os, Linscott, Myin-Germeys, Delespaul and Krabbendam3 Subclinical psychotic experiences are typically expressed in adolescence and young adulthood and are usually transitory. Reference Poulton, Caspi, Moffitt, Cannon, Murray and Harrington4 Nevertheless, they show a degree of epidemiological, psychopathological, longitudinal, familial and aetiological continuity with psychotic disorders and even display some syndromal continuity with diagnostic constructs such as schizophrenia. Reference van Os, Linscott, Myin-Germeys, Delespaul and Krabbendam3
What are the implications for diagnosis? First, psychotic disorders appear to be unclear in that they blur into normality. Second, when a ‘first episode’ of psychotic illness is diagnosed, it may in fact be more correct to regard this as the poor outcome of a phenotype representing subclinical dimensions of psychosis that is transitory in the great majority of cases. Reference van Os, Linscott, Myin-Germeys, Delespaul and Krabbendam3 Third, if psychotic experiences are frequent, their diagnostic value will be low in relation to the rare disorder of schizophrenia. Research has shown that even if the follow-up period is extended to more than 15 years, the probability of developing a psychotic disorder does not exceed 25%. Reference Poulton, Caspi, Moffitt, Cannon, Murray and Harrington4 Therefore, understanding the diagnosis of psychotic disorder in part becomes understanding the onset of need for care (formal or informal) in the context of subclinical psychotic experiences with variable frequency, distress, preoccupation and influence on behaviour.
Schizophrenia: validity?
A recent study showed that the total lifetime prevalence of psychotic disorders is 3.5%, divided over 12 different diagnostic categories. Reference Perala, Suvisaari, Saarni, Kuoppasalmi, Isometsa and Pirkola5 This prevalence estimate is much higher than any previous investigation has suggested. Thus, the myriad diagnostic categories in DSM and ICD that remain without scientific validation may have blinded us to the true prevalence of psychotic disorders, hampering scientific progress. Reference Brockington1
As argued before, Reference Brockington1,Reference Kendell and Jablensky2 there is no consistent evidence for specificity in terms of symptoms, aetiology, treatment and prognosis between diagnostic categories of psychotic disorders. A traditional misunderstanding is to suggest that mean differences on some variable between traditional categories have diagnostic relevance. For example, first-rank symptoms may be more common in schizophrenia than in bipolar disorder but their diagnostic value is too low to be of diagnostic significance, as indicated by a diagnostic likelihood ratio (the likelihood of being a true positive rather than a false positive) of less than 2. Reference Peralta and Cuesta6 Similarly, differences in cognitive impairment and level of negative symptoms do not translate to diagnostic significance. Reference Cuesta, Peralta and Zarzuela7 Research to date suggests that of all psychopathological domains, manic symptoms in particular have the highest level of specificity and represent the greatest diagnostic value. Reference Brockington, Roper, Copas, Buckley, Andrade and Wigg8 Outside psychopathology, ‘points of rarity’ between diagnostic categories of psychotic disorders are also rare, although some prominent differences are apparent. The problem, however, is that not all observed differences flow in the same direction. For example, in terms of genetics, it is increasingly clear that there is considerable overlap in genetic susceptibility across the traditional binary classification of psychosis. Reference Owen, Craddock and Jablensky9 However, the environmental risk associated with growing up in an urban environment may be specific for schizophrenia. Reference Murray, Sham, Van Os, Zanelli, Cannon and McDonald10 Translating these findings to diagnosis would mean that one aetiological factor favours ‘lumping’ of categories, at least in part, whereas the other favours ‘splitting’. Recent meta-analytic work Reference Arts, Jabben, Krabbendam and van Os11 indicates that in both bipolar disorder and schizophrenia, patients and their first-degree relatives display alterations in neurocognition, but in bipolar disorder to a much lesser degree than in schizophrenia. Similarly, the childhood developmental cognitive impairments preceding onset of schizophrenia are not detectable in bipolar disorder. Reference Murray, Sham, Van Os, Zanelli, Cannon and McDonald10
The challenge for DSM–V and ICD–11 is to make use of the evidence suggesting specificity, such as the relative specificity of manic symptoms for bipolar disorder and (familial) developmental impairment for schizophrenia, Reference Murray, Sham, Van Os, Zanelli, Cannon and McDonald10 while at the same time acknowledging that in many other areas no specificity appears to exist. Also, better research evidence for diagnostic validity is needed, not just in terms of the classic single diagnostic dissociation (e.g. variable 1 is associated with category A but not category B) or even the double diagnostic dissociation (e.g. single dissociation plus evidence that a second variable, variable 2, is associated with category B but not category A), but in terms of evidence that is truly logically inconsistent with a single underlying process such as the demonstration of non-monotonic or reversed associations of validating variables across diagnostic categories. Reference Dunn and Kirsner12 For example, based on this method, Linscott et al showed that, given the assumption that a monotonic process leads to unipolar depressive morbidity in relatives of patients in different diagnostic classes, the notion that the same process could possibly lead to bipolar morbidity in relatives could be rejected. Reference Linscott, Allardyce and van Os13
Schizophrenia: utility?
Although the diagnostic constructs of DSM, ICD or RDC schizophrenia do not appear to be valid, they may nevertheless be useful ‘by virtue of the information about outcome, treatment response, and aetiology that they convey’. Reference Kendell and Jablensky2 However, there may be room for improvement. First, a growing number of studies suggest that when dimensional representations (i.e. scoring patients' symptoms along continuous axes of positive, negative, disorganisation, depressive, manic and cognitive symptoms) and categorical representations (i.e. grouping patients in categories of schizophrenia, bipolar disorder, schizoaffective disorder, schizophreniform disorder, etc.) of samples of patients with a range of psychotic disorders are compared in terms of the utility criterion of how much information about aetiology, treatment needs and outcome they convey, the combination of categorical and dimensional representations in these patients does better than either representation alone. Reference Van Os, Fahy, Jones, Harvey, Sham and Lewis14 Second, although some patients and their relatives may find it useful to learn that their experiences can be reduced to a dichotomous medical diagnostic construct, others will feel victimised by the label of a highly stigmatised medical diagnosis that paradoxically cannot be validated scientifically.
Therefore, in terms of utility the following conclusions may be drawn. First, although criticisms about the diagnostic construct of schizophrenia may be deflected with the argument that it is merely a syndrome (the association of several clinically recognisable features that often occur together for which a specific disorder may or may not be identified as the underlying cause), the problem is that its very name and the way mental health professionals use and communicate about the term results in medical reification and validation through professional behaviour rather than scientific data, exposing psychiatry to ridicule and hampering scientific progress. Reference Brockington1 It may be argued, therefore, that if it is a syndrome, calling it as such may serve to remind professionals (and downstream of these, the rest of the world) of the relatively agnostic state of science in this regard. Second, given the fact that maximum utility in terms of conveying clinical information may be obtained by combining categorical with dimensional representations of psychopathology, DSM–V and ICD–11 may be best served by creating separate categorical and dimensional axes of the psychopathology of psychotic disorders.
From schizophrenia to salience dysregulation syndrome?
Many people with impaired glucose regulation also have several other continuous cardiovascular risk factors – they have a tendency to occur together. This is referred to as the metabolic syndrome. Analogous to the metabolic syndrome, although in need of improving on the weaknesses that since its introduction have become apparent, many people with positive psychotic experiences, that have been shown to constitute a fundamental alteration in salience attribution, Reference Kapur15 also display evidence of alterations in other dimensions of psychopathology such as mania, disorganisation and developmental cognitive deficit. This may be referred to as the salience dysregulation syndrome. If the values of the dimensional components in this syndrome rise above a certain threshold, need for care (formal or informal) may arise. Depending on which combinations of dimensional psychopathology are most prominent in this salience dysregulation syndrome and taking into account which elements have been shown to possess the best diagnostic specificity, as discussed above, the categorical representation of this dimensional psychopathology may be expressed using three sub-categories: with affective expression (high in mania/depression dimension); with developmental expression (high in developmental cognitive deficit/negative symptoms); and not otherwise specified (Fig. 1). The first two sub-categories are based on evidence of specificity and the more agnostic category of ‘not otherwise specified’ reflects the continuing gap in knowledge.
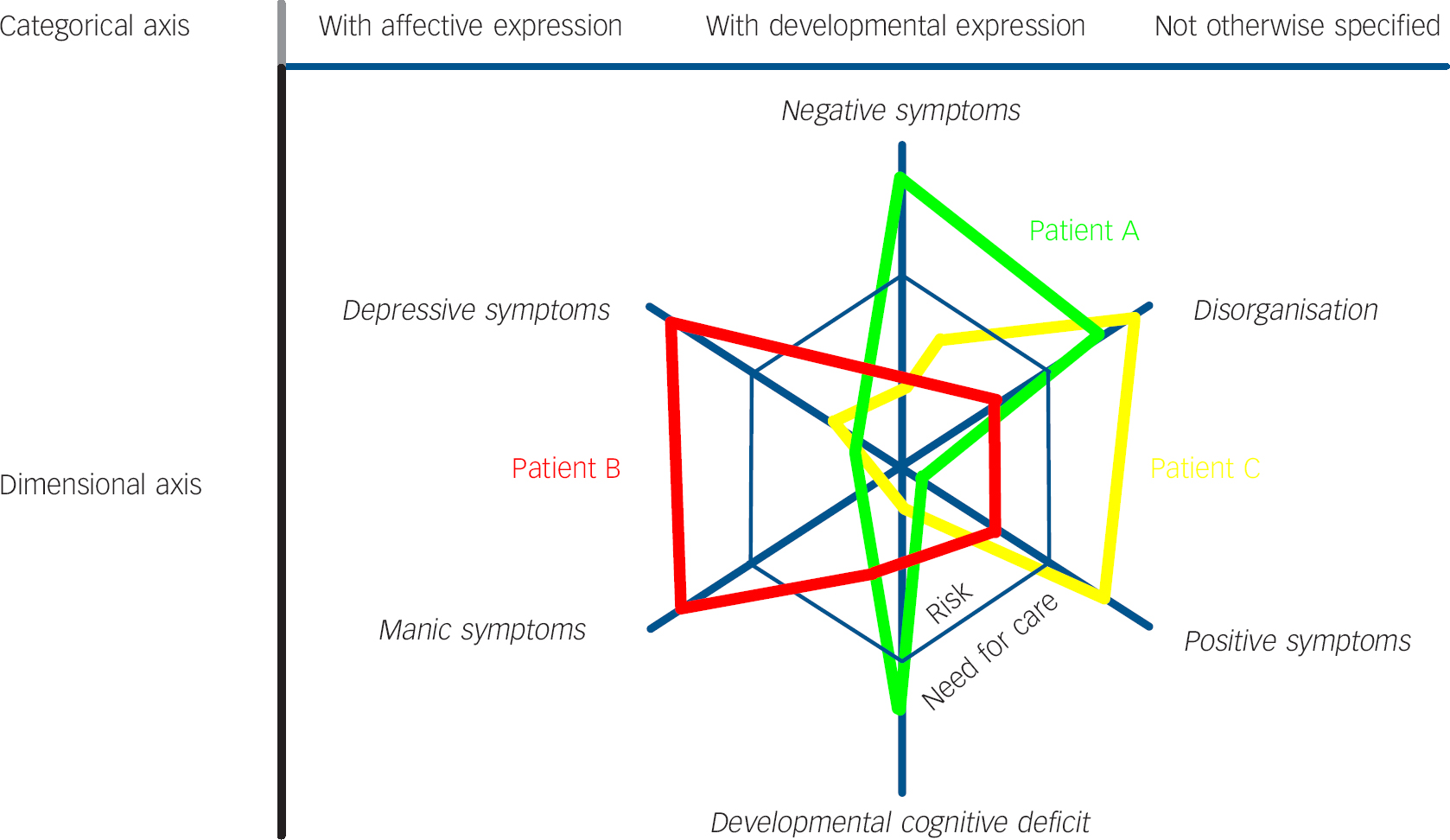
Fig. 1 Salience dysregulation syndrome. Six dimensions that tend to co-occur make up the salience dysregulation syndrome. Individuals may make the transition from ‘risk’ to ‘need for care’ if they pass the threshold on one or more dimensions, and accordingly may fit sub-categories ‘with affective expression’, ‘with developmental expression’ and ‘not otherwise specified’. Patient A: ‘typical’ salience dysregulation syndrome with developmental expression; Patient B: ‘typical’ salience dysregulation syndrome with affective expression; Patient C: salience dysregulation syndrome not otherwise specified. Position of subcategories and dimensions with respect to each other is arbitrary.
Research agenda
It is proposed that the combination of categorical and dimensional representations presented in salience dysregulation syndrome be further investigated, particularly with regard to clinical utility and patient acceptability, focusing on non-monotonicity rather than traditional single or double dissociations as supportive evidence. Many issues need to be resolved. For example, research data are needed in order to determine whether or not to retain ‘psychotic depression’, characterised by mood-congruent psychotic symptoms, within major depressive disorder. Conversely, research should determine whether or not mania without psychotic symptoms should be classified under salience dysregulation syndrome. Other basic questions include: which symptoms are required for a diagnosis of salience dysregulation syndrome? How to assess developmental cognitive deficits, given the fact that a cognitive measure separating premorbid and current level of functioning that can be used worldwide for the purpose of diagnosis is not available yet? Indeed, which dimensions should be included in this syndrome and which symptoms in each dimension? Should patients scoring highly on both mania and developmental cognitive deficit be retained in the ‘with affective symptoms’ sub-category, using the simultaneous presence of dimensional ratings to show differences in the level of comorbid developmental cognitive deficit?
Transforming these questions into researchable hypotheses will require a major effort but there are many suitable data-sets worldwide in which these and other questions can be addressed in order to develop a more evidence-based and less parochial system of diagnosis for patients with severe mental illness. Reference Arts, Jabben, Krabbendam and van Os11
Acknowledgements
J.v.O. is a member of the APA DSM–V Psychotic Disorders Work Group. The views expressed are his own. Thanks to Professors Robin Murray and Assen Jablensky, and Drs Judith Allardyce and Catherine van Zelst for critical comments on earlier versions of this manuscript.




eLetters
No eLetters have been published for this article.