The role of psychotherapy in borderline personality disorder treatment
Although borderline personality disorder (BPD) has been regarded as mostly unresponsive to psychotherapy since its introduction into the DSM in 1980,1 the development of disorder-specific treatment approaches has led to therapeutic optimism. To date, psychotherapy is recommended as the primary treatment for BPD,Reference Simonsen, Bateman, Bohus, Dalewijk, Doering and Kaera2–5 and drug treatment only plays an adjunctive role.Reference Stoffers-Winterling, Völlm and Lieb6 Since pharmacotherapy is not associated with convincing, sustainable effects on BPD pathology,Reference Stoffers-Winterling, Storebø and Lieb7 therapeutic research now primarily focuses on psychotherapy.
Current evidence
In 2020, the Cochrane review on psychological therapies for people with BPD was updated.Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8 Since the publication of its previous version in 2012,Reference Stoffers, Vollm, Rucker, Timmer, Huband and Lieb9 the number of eligible studies had more than doubled, and the 2020 review included 75 randomised controlled trials (RCTs). The 2020 Cochrane review supports the primary role of psychotherapies in BPD treatment. Specifically, a clinically relevant reduction in BPD symptom severity by disorder-specific psychotherapies of any kind was observed, compared with treatment as usual (TAU) (standardised mean difference (SMD) −0.52, 95% CI −0.70 to −0.33, n = 22 RCTs, n = 1244 participants), and there was also evidence of superiority in terms of self-harm (SMD −0.32, 95% CI −0.49 to −0.14, n = 13 RCTs, n = 616 participants), suicide-related outcomes (SMD −0.34, 95% CI −0.57 to −0.11, n = 13 RCTs, n = 666 participants) and psychosocial functioning (SMD 0.45, 95% CI 0.22–0.68, n = 22 RCTs, n = 1314 participants).Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8
Although a broad variety of treatments have been investigated in RCTs, a large proportion of treatments have only been evaluated in a single trial. If the evidence is restricted to a single study, it must be interpreted cautiously, especially in this field of research: The observation size per study is usually very small (only five out of the 75 primary studies of the 2020 Cochrane review included 100 or more participants). Additionally, the treatment developers themselves are usually the first to evaluate their respective therapies, so a risk of affiliation bias is present in the majority of cases where there is only one study available. Overall, the certainty of the evidence is usually very low if only a single study is available. Therefore, this paper concentrates on any psychotherapeutic treatment with corresponding evidence from at least two RCTs. Furthermore, this paper analyses psychological therapies that were delivered as the primary treatment separately from those interventions that supplemented already ongoing individual psychotherapies. This is done to reduce clinical heterogeneity among primary studies and enhance the applicability of findings to individual clinical situations of people affected by BPD.
Method
This review was conducted in accordance with the Cochrane guidelines.Reference Higgins10 Its protocol was published open-access in the Cochrane Database of Systematic Reviews (CDSR) in February 2018, and also on the PROSPERO website (registration number PROSPERO 2018 CRD42018091043).Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Kielsholm12 Data extraction was started upon notice of acceptance of the protocol to be published in the CDSR on 22 January 2018. Although the pre-registered methods of the 2020 full reviewReference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8,Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Kielsholm11 are maintained, this subsidiary paper focuses on comparisons of active treatments and unspecific controls, updates the search and applies a more nuanced perspective, as any adaptations of a standard treatment are analysed individually (e.g. standard dialectical behaviour therapy (DBT) and DBT skills training (DBT-ST) are subject to separate analyses). Interventions are classified as standalone or add-on treatments: standalone treatments are defined as necessarily including individual psychotherapy, be it as the sole treatment component or in combination with other treatment elements, or modules. For example, standard mentalisation-based treatment (MBT) or DBT, which include both individual and group interventions, would be classified as standalone treatments, as would any other individual psychotherapy without complementing group. In contrast, add-on interventions are defined as interventions that complement any ongoing individual BPD treatment.
Moreover, we concentrate on adult samples in this paper, adolescent samples being subject to other systematic reviews.Reference Wong, Bahji and Khalid-Khan13,Reference Jørgensen, Storebø, Stoffers-Winterling, Faltinsen, Todorovac and Simonsen14 The review methods had been declared in the Cochrane protocol.
The same literature search methods are applied as in the 2020 Cochrane review, where comprehensive searches were done in 21 databases and trial registries up to 19 March 2019.Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8 For this publication, the complete searches were updated on 6 October 2020 (see Supplementary Material available at https://doi.org/10.1192/bjp.2021.204 for search strings). Additionally, we emailed researchers working in the field to ask for unpublished data. We also checked abstracts of key conferences for BPD and asked for any relevant unpublished data. On 9 February 2021, we additionally updated the searches in PubMed and the Cochrane Central Register of Controlled Trials, and also traced up any references included as ongoing in the 2020 Cochrane review,Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8 for full publications. There were no language or publication format restrictions.
As for the 2020 Cochrane review,Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8 at least 70% of the study participants had to have a formal diagnosis of BPD according to the DSM,1,15–18 or emotionally unstable personality disorder, borderline type, according to the ICD-10.19 We included trials with BPD subsamples of <70% BPD if we had obtained separate data for them from the study authors upon our request. We included studies with or without co-occurring psychiatric conditions. We excluded trials of participants with mental impairment, organic brain disorder, dementia or other severe neurologic or neurodevelopmental diseases.
We included RCTs comparing an active treatment with any kind of unspecific control treatment (i.e. excluding any defined psychotherapeutic BPD treatment), be it TAU, waiting list, case management, standard care or similar. In contrast to the 2020 Cochrane review,Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8 we pooled comparisons to any of these controls in the same analyses in this study, since post hoc subgroup analyses of the 2020 Cochrane review revealed no differences between comparisons with different kinds of unspecific controls, supporting the pooling of such data within the same analysis.Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8
Global BPD symptom severity, self-harm, suicide-related outcomes (covering suicidal ideation and suicidal behaviour) and psychosocial functioning were the primary outcomes. Secondary outcomes included single BPD symptoms according to criteria from the DSM-III1,18 to DSM-5, depression and attrition. If trials reported two or more measures for a particular outcome, we selected the one used most often among all included trials, to minimise heterogeneity of outcomes in form and content. If a trial reported data of two assessment instruments that were equally frequently used, two review authors discussed the issue and chose the one most appropriate for the assessment of people affected by BPD. We did not calculate effect estimates for the outcome of attrition from studies including no treatment or waiting list controls, since participants allocated to these conditions did not receive any treatment that they could have dropped out from (see Supplementary Material, PICOS table).
Review authors worked in pairs and independently screened titles and abstracts of all records retrieved by the searches. We reported the reason for exclusion for all relevant studies. The methodological quality of the studies was independently assessed by two reviewers regarding the risk of bias, using the Cochrane Collaboration risk of bias tool.Reference Higgins, Altman, Gotzsche, Juni, Moher and Oxman20 We developed data extraction forms to facilitate the standardisation of data extraction. Working in pairs, all review authors extracted data independently, using the data collection form to ensure accuracy. As for study selection, we resolved disagreements by discussion or by involving a third reviewer. Effect sizes were calculated with RevMan 5, 64 bit version for windows.21
For continuous outcomes, we compared the mean difference and presented this with 95% confidence intervals to combine the same outcome measures from trials. We calculated the SMDs on basis of post-treatment results in the meta-analysis if there were two or more different instruments used to measure the same construct. If trials did not report mean values and s.d. but reported other values like t-tests and P-values, we tried to transform these into s.d. values. The inverse-variance meta-analysis method was used for pooling the data. For dichotomous data, the risk ratio was calculated. We used the random-effects model for our meta-analyses, as we expected clinical heterogeneity to be present in most analyses. We calculated effect sizes on basis of intention-to-treat data, if possible. We investigated statistical heterogeneity by both visual inspection of the graphs and the I 2 statistic.Reference Higgins, Thompson, Deeks and Altman22 We considered I 2 values 0–40% as indicating low heterogeneity, 30–60% as indicating possibly moderate heterogeneity, 50–90% as indicating possibly substantial heterogeneity and 75–100% as indicating considerable heterogeneity.Reference Higgins and Green23 The overlap of intervals allows for individual factors when interpreting the importance of inconsistency of study estimates included in the same analysis, e.g. the magnitude and direction of effect, and the strength of evidence for heterogeneity.Reference Higgins10
We applied the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) toolReference Guyatt, Oxman, Akl, Kunz, Vist and Brozek24 to assess the quality, or certainty, of the overall body of evidence. All ratings were discussed by the two primary authors (J.M.S.-W. and O.J.S.). The following five domains were taken into account to rate the certainty of the findings for any primary outcome: risk of bias in primary studies (based on Cochrane Risk of Bias toolReference Higgins, Altman, Gotzsche, Juni, Moher and Oxman20 ratings), inconsistency (i.e. high heterogeneity) of primary study findings, indirectness of the evidence, imprecision (finding based on a single trial, wide confidence intervals) and publication bias (i.e. bias owing to the non-publication of studies with negative undesired results). We drew funnel plots for the primary and secondary outcomes with the highest numbers of available study effect estimates, to investigate the possibility of publication bias.
Ethical considerations
For preparing this systematic reviewer and meta-analysis, no deeply personal, sensitive or confidential information was collected from individual participants. Any data was anonymised and drawn from publicly accessible documents. Therefore, no formal ethics approval was sought.
Results
Of the 75 RCTs included in the 2020 Cochrane review,Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8 30 were eligible for inclusion in this focused review of comparisons with unspecific control interventions in adult samples (Fig. 1). The updated searches done for the present review retrieved 54 records, two of which referred to two unique new eligible RCTs. In total, 32 trials were available for qualitative analysis. We excluded one RCT from the quantitative analyses because of substantial concerns about the study validity (see next section). Finally, 31 RCTs, including 1870 participants, were included in the quantitative analyses (Table 1).
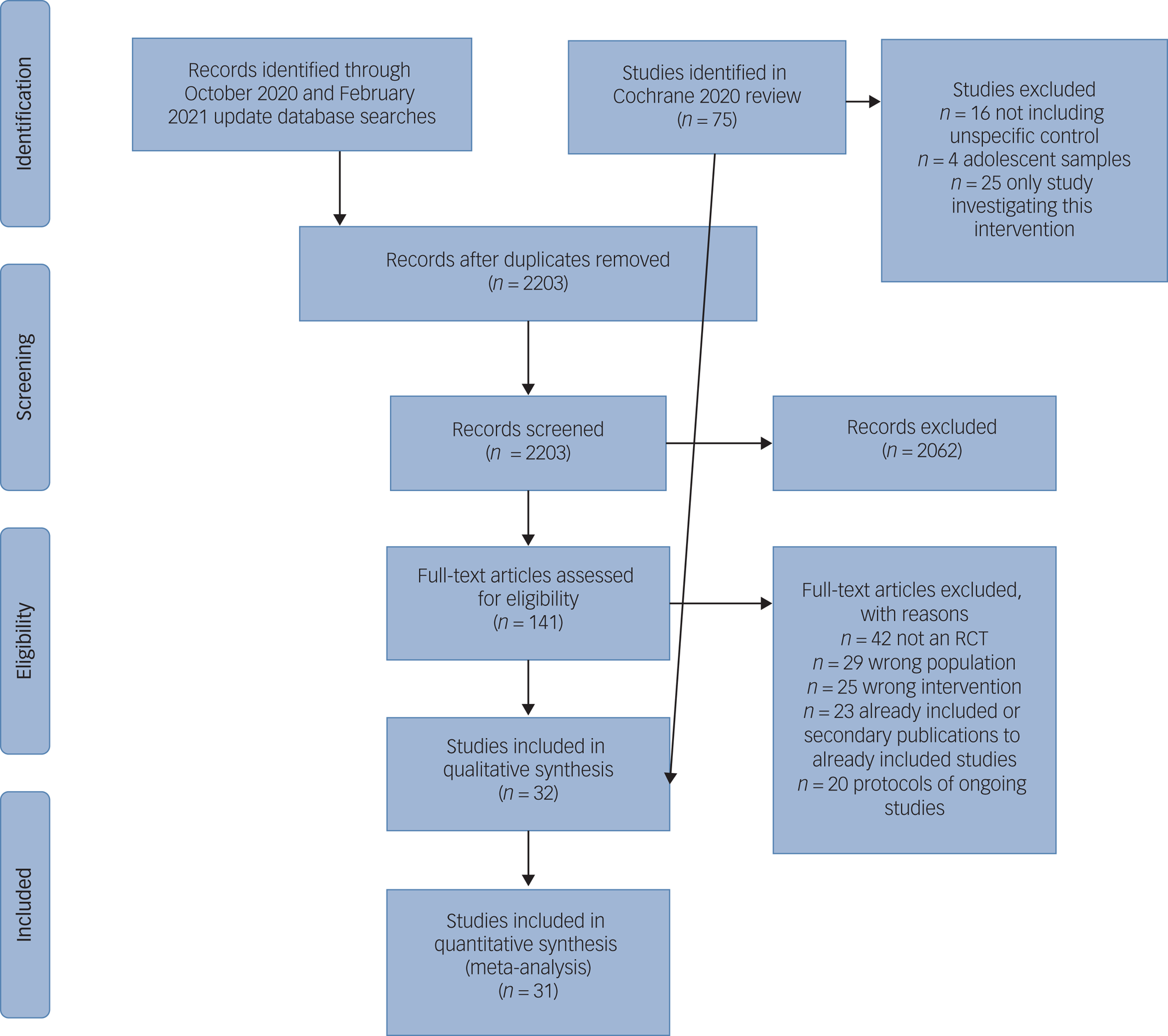
Fig. 1 Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2009 flow diagram.
Table 1 Characteristics of included studies

TAU, treatment as usual; PTSD, post-traumatic stress disorders; E-TAU, treatment as usual by experts.
a. As required for inclusion in primary study.
b. Borderline personality disorder subsample data.
c. Forensic.
d. Not included in quantitative analyses.
Description of studies and risk of bias
Fifteen RCTs were conducted in Europe, 14 in North America, two in Iran and one in New Zealand. The publication period spanned almost three decades (1991–2020), but only three RCTs were published before 2000.Reference Linehan, Armstrong, Suarez, Allmon and Heard25–Reference Bateman and Fonagy27 Twelve samples included women only,Reference Linehan, Armstrong, Suarez, Allmon and Heard25,Reference Linehan, Tutek, Heard and Armstrong26,Reference Carter, Willcox, Lewin, Conrad and Bendit28–Reference Zanarini, Conkey, Temes and Fitzmaurice37 whereas oneReference Bianchini, Cofini, Curto, Lagrotteria, Manzi and Navari38 concentrated on men only. The remaining studies consisted predominantly of females (58–96%). The sample mean age ranged from 19.3 to 45.7 years. In two RCTs, distinct co-occurring psychiatric disorders were required for study inclusion, i.e. comorbid post-traumatic stress disorderReference Kredlow, Szuhany, Lo, Xie, Gottlieb and Rosenberg39 or active alcohol misuse or dependence.Reference Gregory, Chlebowski, Kang, Remen, Soderberg and Stepkovitch40 Most of the remaining studies did, however, not preclude the co-occurrence of psychiatric disorders. The vast majority of RCTs were conducted in outpatient settings, whereas only two trials took place in an in-patient settingReference Mohamadizadeh, Makvandi, Pasha, Bakhtiarpour and Hafezi31,Reference Bianchini, Cofini, Curto, Lagrotteria, Manzi and Navari38 and two trials took place in a day hospital setting.Reference Bateman and Fonagy27,Reference Laurenssen, Luyten, Kikkert, Westra, Peen and Soons41 Observation periods ranged from 6 weeks to 18 months (see Table 1).
Twenty out of the 32 included trials investigated standalone treatments: DBT (n = 10), MBT (n = 4), interpersonal therapy adapted for BPD (IPT-BPD; n = 2), cognitive–behavioural therapy (CBT; n = 2) and dynamic deconstructive psychotherapy (DDP; n = 2).
DBT is based on CBT and, as a multi-modal treatment, combines individual psychotherapy, group skills training, regular therapists team consultations and crisis telephone coaching if needed.Reference Linehan42,Reference Linehan43 MBT also includes individual and group sessions. It is a psychodynamic therapy that draws from attachment and cognitive theory, and aims to enhance the impaired capacity to identify and understand mental states in oneself and others usually found in individuals with BPD.Reference Bateman and Fonagy44 IPT-BPD is an adaption of IPT that had originally been developed for the treatment of major depression.Reference Klerman, Weissman, Rounsaville and Chevron45 BPD is conceptualised as a chronic mood disorder, and the IPT-BPD adaptation includes a longer treatment duration, more flexibility in treatment settings and treatment intensity, and more focus on the therapeutic relationship.Reference Markowitz, Skodol and Bleiberg46 Recently, it has been suggested to complement IPT-BPD with a family intervention aiming to educate significant others about BPD.Reference Bellino and Bozzatello47 CBT includes psychoeducation and focuses on restructuring maladaptive core beliefs and patterns of behaviour, and aims to develop new, more adaptive beliefs about the self and others, and more adaptive strategies of behaviour.Reference Davidson48 DDP is a psychodynamic treatment with a strong experiential component that has been developed to specifically meet the needs of individuals with BPD and co-occurring substance use disorder or antisocial personality disorder. It aims to activate impaired neurocognitive functions (e.g. disrupted linkages among affective experiential capacities, memory and verbal/symbolic attribution) by verbalising and elaborating effects and interpersonal experiences.Reference Gregory and Remen49 Twelve more studies focused on psychotherapeutic add-on interventions that are intended to complement ongoing individual psychotherapies and are usually delivered in a group format: DBT-ST groupReference Linehan42 (n = 4), emotion regulation groupReference Gratz and Gunderson33 (ERG; n = 2), manual-assisted cognitive therapyReference Schmidt and Davidson50 (MACT; n = 2), psychoeducationReference Zanarini and Frankenburg36,Reference Zanarini, Conkey, Temes and Fitzmaurice37 (n = 2) and systems training for emotional predictability and problem solvingReference Blum51,Reference Black, Blum, Pfohl and St. John52 (STEPPS; n = 2; see Table 1). The DBT-ST group is part of standard DBT and usually complements DBT individual treatment by introducing and training mindfulness, distress tolerance, emotion regulation and interpersonal effectiveness skills.Reference Linehan42 Several studies, however, have tested the effects of DBT-ST alone. ERG is a group intervention combining elements of DBT, classic CBT, acceptance- and commitment therapy, and emotion-focused psychotherapy to target emotion dysregulation, and emotional avoidance specifically, among self-harming women.Reference Gratz and Gunderson33 MACT is a brief, six-session intervention aimed at helping individuals understand their self-harming behaviour better, and to reduce distress by enhancing problem-solving skills.Reference Schmidt and Davidson50 This treatment is designed to comply with a self-help manual that is used by treatment-seeking individuals in their preparation for each session. Psychoeducation programmes intend to provide the latest information about BPD epidemiology, phenomenology and treatment options to newly diagnosed individuals with BPD, either in the format of an in-person presentation using slides, or a booklet-type web-based presentation.Reference Zanarini and Frankenburg36,Reference Zanarini, Conkey, Temes and Fitzmaurice37 STEPPS is a cognitive–behavioural systems-based group programme that includes skills training to specifically address cognitive distortions and emotional dysregulation, and involves significant others.Reference Black, Blum, Pfohl and St. John52
Comparison treatments were, as required for inclusion into this review, unspecific control conditions. To rule out the effects of the specific experimental interventions, most trials provided TAU (n = 20)Reference Linehan, Armstrong, Suarez, Allmon and Heard25–Reference Koons, Robins, Tweed, Lynch, Gonzalez and Morse29,Reference van den Bosch, Verheul, Schippers and van den Brink32–Reference Weinberg, Gunderson, Hennen and Cutter35,Reference Bianchini, Cofini, Curto, Lagrotteria, Manzi and Navari38–Reference Gregory, Chlebowski, Kang, Remen, Soderberg and Stepkovitch40,Reference Priebe, Bhatti, Barnicot, Bremner, Gaglia and Katsakou53–Reference Blum, St John, Pfohl, Stuart, McCormick and Allen59 or expert TAU, meaning that control participants were referred to usual treatment for BPD in that specific area or health system (n = 2)Reference Linehan, Comtois, Murray, Brown, Gallop and Heard30,Reference Laurenssen, Luyten, Kikkert, Westra, Peen and Soons41 . In other trials, supportive treatment (n = 4)Reference Kredlow, Szuhany, Lo, Xie, Gottlieb and Rosenberg39,Reference Jørgensen, Freund, Bøye, Jordet, Andersen and Kjølbye60–Reference Majdara, Rahimmian, Talepassand and Gregory62 or clinical management (n = 3)Reference Bellino, Rinaldi and Bogetto63–Reference Bateman and Fonagy65 was provided. Others put the participants who had been assigned to the control group on a waiting list where they were free to use any treatment besides the treatment under test or no treatment at all (n = 2),Reference Zanarini and Frankenburg36,Reference McMain, Guimond, Barnhart, Habinski and Streiner66 or provided no treatment (n = 2).Reference Mohamadizadeh, Makvandi, Pasha, Bakhtiarpour and Hafezi31,Reference Zanarini, Conkey, Temes and Fitzmaurice37
Across studies, detection and selection bias were deemed to be the least problematic, with 71.8% and 68.8% of included studies being rated as having low risks of bias in this regard (Fig. 2, Supplementary Material, Risk of Bias in Primary Studies). Other risk of bias was deemed to be present in more than half of all trials (55.25%). This category includes the risk of bias resulting from affiliations of the study authors to one of the treatments under test, unequal amounts of attention spent to the treatment groups or non-adherence to treatments. Affiliation bias accounts for the main part of high-risk ratings in this category. One trial testing DBT against a control treatmentReference Mohamadizadeh, Makvandi, Pasha, Bakhtiarpour and Hafezi31 was removed from the quantitative analyses because of a very low reporting quality in combination with reporting of obviously escalating treatment effects: none of the assessed risks of bias could be rated because of a lack of information, and all effect estimates translated into SMDs >11.0, which is beyond expectations for any psychotherapeutic treatment.

Fig. 2 Risk-of-bias graph. RCT, randomised controlled trial.
Effects of interventions: standalone psychotherapies
The highest number of individual RCTs was available for standard DBT (n = 10 studiesReference Linehan, Armstrong, Suarez, Allmon and Heard25,Reference Linehan, Tutek, Heard and Armstrong26,Reference Carter, Willcox, Lewin, Conrad and Bendit28–Reference Linehan, Comtois, Murray, Brown, Gallop and Heard30,Reference van den Bosch, Verheul, Schippers and van den Brink32,Reference Bianchini, Cofini, Curto, Lagrotteria, Manzi and Navari38,Reference Priebe, Bhatti, Barnicot, Bremner, Gaglia and Katsakou53,Reference Feigenbaum, Fonagy, Pilling, Jones, Wildgoose and Bebbington56,Reference Stanley67 ), followed by MBT (n = 4 studiesReference Bateman and Fonagy27,Reference Laurenssen, Luyten, Kikkert, Westra, Peen and Soons41,Reference Jørgensen, Freund, Bøye, Jordet, Andersen and Kjølbye60,Reference Bateman and Fonagy65 ). For each of the remaining standalone treatments under test, two RCTs were identified (CBT,Reference Kredlow, Szuhany, Lo, Xie, Gottlieb and Rosenberg39,Reference Davidson, Tyrer, Gumley, Tata, Norrie and Palmer54 DDP,Reference Gregory, Chlebowski, Kang, Remen, Soderberg and Stepkovitch40,Reference Majdara, Rahimmian, Talepassand and Gregory62 IPT-BPDReference Bellino, Rinaldi and Bogetto63,Reference Bozzatello and Bellino64 ). All effect estimates are displayed in Table 2, along with the number of comparisons, participants, the 95% confidence intervals, P-values and I 2 scores that indicate the percentage of the variability in effect estimates resulting from heterogeneity rather than sampling error (or chance) alone.68,69
Table 2 Effects of interventions

Bold text indicates statistically significant effects (95% Confidence Interval); BDI, Beck Depression Inventory; BDI-II, Beck Depression Inventory-II; BEST, Borderline Evaluation of Severity overTime; BPDSI-IV, Borderline Personality Disorder Severity Index-IV; BPRS, Brief Psychiatric Rating Scale; CGI-BPD, Clinical Global Impression Scale for Borderline Personality Disorder; CGI-S, Clinical Global Impression Scale-Severity subscale; CI, Confidence Interval; CUDOS, Clinically Useful Depression Outcome Scale; DASS, Depression and Anxiety Stress Scale; DDP, Dynamic Deconstructive Psychotherapy; DERS, Difficulties in Emotion Regulation Scale; DES, Dissociative Experience Scale; DSHI, Deliberate Self-Harm Inventory; GAS, Global Assessment Scale; HADS, Hospital Anxiety and Depression Scale; Ham-D, Hamilton Depression Scale; IIP-BPD, BPD-related composite of the Inventory of Interpersonal Problems; IIP-SC, Inventory of Interpersonal Problems-Short Circumplex; LPC, Lifetime Parasuicide Count; MD, mean difference; PHI, Parasuicide History Interview; RR, risk ratio; SAS, Social Adjustment Scale; SASII, Suicide Attempt Self Injury Interview; SAS-SR, Social Adjustment Scale-Self-Rating; SCID-II, Structured Clinical Interview for DSM-IV Axis II Personality Disorders; SDS, Sheehan Disability Scale; SFQ, Social Functioning Questionnaire; SMD, standardized mean difference; SPS, Social Provisions Scale; STAXI, Stait Trait Anger Expression Inventory; WHO-QoL-Bref, World Health Organisation Quality of Life Questionnaire-abbreviated version; Zan-BPD, Zanarini Rating Scale for Borderline Personality Disorder.
a. Negative mean differences, negative standardised mean differences or Risk Ratios < 1 indicate beneficial effects by the experimental treatment data.
b. Log-transformed data.
For DBT, statistically significant moderate-to-large effectsReference Cohen70 were observed in the primary outcomes of self-harm (SMD −0.54, 95% CI −0.92 to −0.16, n = 3 studies, n = 110 participants, I 2 = 0%) and psychosocial functioning (SMD −0.51, 95% CI −0.90 to −0.11, n = 3 studies, n = 115 participants). Similarly, there was also a statistically significant effect on the secondary outcome of anger (SMD −0.83, 95% CI −1.43 to −0.22, n = 2 studies, n = 46 participants). Statistical heterogeneity was marginal for all of these effect estimates (0–5%; see Table 2).
MBT was assessed in four studies. The risk of engaging in self-harm (risk ratio 0.51, 95% CI 0.34–0.75, n = 2 studies, n = 172 participants) or suicidal behaviour (risk ratio 0.10, 95% CI 0.03–0.32, n = 2 studies, n = 172 participants) was found to be significantly lower in the MBT-treated groups (statistical heterogeneity 0% for both estimates, see Table 2). There were no statistically significant effects for any of the secondary outcomes, but two effect estimates (interpersonal problems, depression) were just beyond the boundaries of significance (P = 0.06 and P = 0.07). However, statistical heterogeneity among the four reporting RCTs was substantial for both of these outcomes.
All remaining standalone treatments were subject to two RCTs each. For CBT, depression was the only outcome reported by both corresponding RCTs, which resulted in a statistically non-significant effect and substantial heterogeneity. A statistically significant effect on BPD severity was found by the smaller of these two studies, in terms of 3.08 fewer positive BPD items on the Structured Clinical Interview for DSM-IVReference First, Gibbon, Spitzer, Williams and Benjamin71 (95% CI −4.99 to −1.17, n = 1 study, n = 26 participants) at the end of treatment. The larger study did not find a statistically significant difference in terms of the proportions of participants still meeting diagnostic BPD criteria after treatment (see Table 2).
For DDP, two RCTs were available. Their pooled findings resulted in a statistically significant effect estimate of −9.49 points on the 15-point Borderline Evaluation of Severity Over Time (BEST)Reference Pfohl, Blum, John, McCormick, Allen and Black72 questionnaire (95% CI −18.04 to −0.94, n = 2 studies, n = 55 participants). There was also a large pooled, statistically significant effect estimate for the outcome of depression (SMD −0.87, 95% CI −1.64 to −0.10, n = 2 studies n = 56 participants). Statistical heterogeneity was moderate (depression: I 2 = 45%) to considerable (BPD severity: I 2 = 67%).69 Additionally, one of the studies found a statistically significant effect for the outcome of psychosocial functioning in terms of more days paid for work during the past 30 days (mean difference −16.60, 95% CI −22.61 to −10.59; see Table 2).
Although we observed no statistically significant effects of IPT-BPD for any primary outcome, there were several for secondary outcomes, all of which were assessed by the Borderline Personality Disorder Severity Index-IV (BPDSI-IV).Reference Arntz, van den Hoorn, Cornelis, Verheul, van den Bosch and de Bie73 There were statistically significant findings from both corresponding studies for the outcome of impulsivity (mean difference −1.69, 95% CI −3.05 to −0.33, n = 2 trials, n = 80 participants) and interpersonal problems (mean difference −1.74, 95% CI −3.01 to −0.47, n = 2 trials, n = 80 participants). Both were associated with considerable statistical heterogeneity (I 2 = 84% and I 2 = 72%, respectively). Another statistically significant effect was observed for the outcome of affective instability in one of the studies (mean difference −1.02, 95% CI −1.66 to −0.38, n = 1 trial, n = 44 participants).
Notably, we did not observe a significant effect on outcomes of the so-called cognitive cluster of BPD symptoms, which includes identity disturbance and dissociation/stress-related paranoia, for any of the standalone treatments. There were also no statistically significant attrition rates in experimental and control treatments.
Effects of interventions: add-on/group psychotherapies
Twelve RCTs evaluated the effects of five different add-on interventions that are intended to supplement ongoing treatments like individual psychotherapy, or drug treatment. DBT-ST that is usually delivered as a component of standard DBT was subject to four RCTs.Reference Mohamadizadeh, Makvandi, Pasha, Bakhtiarpour and Hafezi31,Reference Kramer, Pascual-Leone, Berthoud, de Roten, Marquet and Kolly57,Reference Soler, Pascual, Tiana, Cebria, Barrachina and Campins61,Reference McMain, Guimond, Barnhart, Habinski and Streiner66 Two trials each investigated ERG,Reference Gratz and Gunderson33,Reference Gratz, Tull and Levy34 MACT,Reference Weinberg, Gunderson, Hennen and Cutter35,Reference Davidson, Brown, James, Kirk and Richardson55 psychoeducationReference Zanarini and Frankenburg36,Reference Zanarini, Conkey, Temes and Fitzmaurice37 and STEPPS.Reference Bos, van Wel, Appelo and Verbraak58,Reference Blum, St John, Pfohl, Stuart, McCormick and Allen59
For DBT-ST alone, statistically significant moderate effects were observed for the primary outcomes of BPD severity (SMD −0.66, 95% CI −1.08 to −0.25, n = 3 studies, n = 184 participants) and psychosocial functioning (SMD −0.45, 95% CI −0.75 to −0.16, n = 3 studies, n = 184 participants). Heterogeneity was moderate (47%) or nonexistent (0%). There were moderate-to-large statistically significant effects from pooled effect estimates for secondary outcomes related to the impulsive symptom cluster (impulsivity: SMD −0.47, 95% CI −0.80 to−0.14, n = 2 studies, n = 143 participants), emotionally dysregulated cluster (anger: SMD −1.01, 95% CI −1.36 to −0.66, n = 2 studies, n = 143 participants; affective instability: SMD −1.04, 95% CI −1.39 to −0.69, n = 2 studies, n = 143 participants) and depression (SMD −0.72, 95% CI −1.14 to −0.29, n = 2 studies, n = 143 participants). Heterogeneity was nonexistent to low (0% in all cases, except for depression, which had an I 2 of 35%). Another statistically significant effect in terms of a reduction of psychotic symptoms was observed in a single study (mean difference −3.15 points on the Brief Psychiatry Rating Scale,Reference Overall and Gorham74 95% CI −5.57 to −0.73, n = 1 study, n = 59 participants).
ERG showed statistically significant effects for the primary outcome of BPD severity in terms of an 8.49 points reduction on the BEST questionnaireReference Pfohl, Blum, John, McCormick, Allen and Black72 (95% CI −11.51 to −5.46, n = 2 studies, n = 83 participants). As for secondary outcomes, statistically significant effects were found in terms of a –25.51 points reduction on the Difficulties in Emotion Regulation (DERS) questionnaireReference Gratz and Roemer75 total score (95% CI −42.53 to −8.48, n = 2 studies, n = 83 participants), impulsivity (mean difference −0.46 points on the DERS impulsivity subscale, 95% CI −0.86 to −0.07, n = 2 studies, n = 83 participants) and depression (mean difference −9.13 points on the Depression and Anxiety Stress ScalesReference Lovibond and Lovibond76 depression subscale, 95% CI −13.25 to −5.01, n = 2 studies, n = 83 participants). Statistical heterogeneity was nonexistent or low for all secondary outcomes, except affective instability (I 2 = 71%).
There were statistically significant effects of MACT on the primary outcomes of self-harm in terms of a greater reduction of parasuicide frequency (mean difference −3.03 points on the Parasuicide History Interview frequency subscale,Reference Linehan, Wagner and Cox77 95% CI −5.68 to −0.38, n = 1 study, n = 28 participants), and a large effect on suicide-related outcomes (SMD −0.96, 95% CI −1.62 to −0.29, n = 2 studies, n = 43 participants, I 2 = 0%). Finally, there was another single study-based, statistically significant effect for depression (mean difference −11.77 points on the Hospital Anxiety and Depression Scale,Reference Zigmond and Snaith78 95% CI −18.05 to −5.49, n = 1 study, n = 15 participants).
For psychoeducation, no statistically significant effects were observed for any primary outcome, besides the secondary outcome of impulsivity. The pooled effect estimates of the two corresponding trials resulted in a statistically significant reduction of impulsivity in terms of a reduction of −0.46 points on the Zanarini Rating Scale for Borderline Personality Disorder (Zan-BPD;Reference Zanarini, Vujanovic, Parachini, Boulanger, Frankenburg and Hennen79 95% CI −0.86 to −0.07, n = 2 studies, n = 130 participants). There was no statistical heterogeneity present (I 2 = 0%).
STEPPS was associated with a moderate, statistically significant effect on the primary outcomes of BPD severity (SMD −0.48, 95% CI −0.78 to −0.18, n = 2 studies, n = 176 participants) and psychosocial functioning (mean difference –7.00 points on the Global Assessment Scale,Reference Endicott, Spitzer, Fleiss and Cohen80 95% CI −11.43 to −2.57, n = 1 study, n = 124 participants). For secondary outcomes, a statistically significant effect in terms of a reduction of interpersonal problems (SMD −0.38, 95% CI −0.67 to −0.08, n = 2 studies, n = 177 participants) and cognitive cluster symptoms (mean difference −1.00 points on the Zan-BPD cognitive cluster subscale, 95% CI −1.83 to −0.17, n = 1 study, n = 124 participants) was found. There was also a higher proportion of attrition in the STEPPS-treated groups (risk ratio 1.91, 95% CI 1.03–3.39, n = 2 studies, n = 203 participants). All pooled effect estimates for STEPPS were free of substantial statistical heterogeneity (I 2 = 0% for all comparisons).
Quality of the evidence
The quality of the evidence was rated very low for most outcomes and comparisons, primarily because of imprecision (based on single trials only, wide confidence intervals) and risk of bias in primary studies. Table 3 summarises the findings on primary outcomes along with GRADE ratings of the evidence quality.
Table 3 Summary of findings (primary outcomes) and quality of the evidence

Evidence key: ++++, high quality; +++, moderate quality; ++, low quality; +, very low quality. Bold text indicates statistically significant effects (95% confidence interval); BEST, Borderline Evaluation of Severity over Time; BPD, borderline personality disorder; BPDSI-IV, Borderline Personality Disorder Severity Index-IV; CBT, cognitive-behavioural therapy; CGI-S, Clinical Global Impression Scale-Severity subscale; CI, Confidence Interval; DBT, dialectical behaviour therapy; DDP, dynamic deconstructive psychotherapy; DSHI, Deliberate Self-Harm Inventory; ERG, emotion regulation group; GAS, Global Assessment Scale; GRADE, Grading of Recommendations, Assessment, Development and Evaluations; IPT-BPD, interpersonal psychotherapy adapted for borderline personality disorder; LPC, Lifetime Parasuicide Count; MACT, manual-assisted cognitive therapy; MBT, mentalisation-based treatment; MD, Mean Difference; PHI, Parasuicide History Interview; RR, Risk Ratio; SAS, Social Adjustment Scale; SAS-SR, Social Adjustment Scale Self-Rating; SASII, Suicide Attempt Self Injury Interview; SCID-II, Structured Clinical Interview for DSM-IV Axis II Personality Disorders; SDS, Sheehan Disability Scale; SMD, Standardised Mean Difference; SPS, Social Provisions Scale; STEPPS, Systems training for emotional predictability and problem solving; Zan-BPD, Zanarini Rating Scale for Borderline Personality Disorder.
a. Negative mean differences, negative standardised mean differences, or Risk Ratios < 1 indicate beneficial effects by the experimental treatment
b. Downgraded because of imprecision (wide confidence interval).
c. Downgraded because of imprecision (based on one trial only).
d. Downgraded because of high risk of bias.
e. Downgraded because of inconsistency (high heterogeneity).
f. Log-transformed data
The quality, or certainty of the evidence was not rated high for any comparison and outcome. It was considered moderate for DBT-ST (BPD severity, suicide-related outcomes, psychosocial functioning) and low for DBT (BPD severity, self-harm, suicide-related outcomes, psychosocial functioning), IPT-BPD (self-harm), MBT (BPD severity, self-harm, suicide-related outcomes), ERG (BPD severity), MACT (self-harm, suicide-related outcomes) and STEPPS (BPD severity). The quality of all remaining comparisons and outcomes was regarded as very low.
To assess the risk of bias from publication bias as well as small-study effects, we drew a funnel plot for the two most prevalent outcomes across all studies, BPD severity and depression (Fig. 3). While the visual inspection of the funnels identified a trend of asymmetry in terms of missing unfavourable results from more imprecise, smaller studies, a small-study effect became evident for both outcomes,Reference Sterne and Egger81 as effect estimates of smaller studies clearly differed from those of larger studies. Therefore, a non-reporting bias due to the inavailability of smaller trials with unfavourable outcomes cannot be ruled out. On the other hand, asymmetry might also be caused by the tendency of smaller studies to be associated with exaggerated effects of estimates.Reference Page, Higgins, Clayton, Sterne, Hróbjartsson and Savović82

Fig. 3 Funnel plots. SMD, standardised mean difference.
Discussion
This review is based on a comprehensive search and updates and complements the 2020 Cochrane review,Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8 with a more nuanced view on individual treatment approaches. By investigating treatment effects of standalone psychotherapies and add-on interventions, we found beneficial effects for both regarding the primary outcomes of BPD severity, psychosocial functioning, self-harm and suicide-related outcomes, and the secondary outcomes of specific BPD diagnostic criteria and depression. However, the quality or certainty of the evidence was rated low or very low in the majority of cases. Among standalone treatments, statistically significant effect estimates as supported by at least low-certainty evidence were only found for DBT (self-harm, psychosocial functioning) and MBT (self-harm, suicide-related outcomes). The quality of the evidence for some add-on treatments was good, with moderate-quality evidence of beneficial effects by DBT-ST groups on the primary outcomes of BPD severity and psychosocial functioning.
Although head-to-head comparisons of treatments were not examined in this paper, the results support the conclusion that beneficial effects can be observed by different interventions. More research is needed to foster our understanding of helpful treatment components across distinct treatment methods. In recent years, suggestions have been made regarding individual methods and pointing to the need to accompany and guide individuals with BPD long term, using generalist methods, with the most prominent being general psychiatric management.Reference Choi-Kain83
Completeness of the evidence
As in the 2020 Cochrane review,Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8 the samples included in the primary studies were predominantly female. Therefore, the applicability of the findings to male individuals with BPD is limited, as BPD manifests differently according to gender.Reference Hoertel, Peyre, Wall, Limosin and Blanco84,Reference Neacsiu, Eberle, Keng, Fang and Rosenthal85 For example, men tend to respond to negative affect more explosively, aggressively or impulsively, whereas women respond with greater levels of self-focus.Reference Hoertel, Peyre, Wall, Limosin and Blanco84
Unfortunately, we were not able to identify any two or more RCTs evaluating the same comorbidity-specific treatment. Although adaptations of BPD therapies for defined comorbidities are now available and have been tested in single RCTs, e.g. for DBT (DBT-adapted for post-traumatic stress disorder,Reference Bohus, Dyer, Priebe, Krüger, Kleindienst and Schmahl86,Reference Bohus, Kleindienst, Hahn, Müller-Engelmann, Ludäscher and Steil87 DBT prolonged exposureReference Harned, Korslund and Linehan88) and MBT (MBT adapted for eating disorders,Reference Robinson89 MBT adapted for co-occurring substance use disorderReference Philips, Wennberg, Konradsson and Franck90), replication studies are presently lacking.
Furthermore, we were unable to identify any two or more RCTs testing the prominent therapies of transference-focused therapy (TFP) and schema-focused therapy (SFT) in their standard formats against unspecific controls. There was only one RCT testing TFP against an unspecific control treatment,Reference Doering, Hörz, Rentrop, Fischer-Kern, Schuster and Benecke91 and SFT was only tested head-to-head against alternate treatmentsReference Giesen-Bloo, van Dyck, Spinhoven, Van Tilburg, Dirksen and Van Asselt92,Reference Nadort93 or conducted in a non-standard group format.94 However, RCTs testing standard SFT against DBTReference Fassbinder, Assmann, Schaich, Heinecke, Wagner and Sipos95 and SFT delivered in a group format against an unspecific control are under way.Reference Wetzelaer, Farrell, Evers, Jacob, Lee and Brand96
Control treatments varied across the studies. However, sensitivity analyses of the 2020 Cochrane review revealed no substantial difference in effect estimates observed by comparisons with TAU or waiting list/no treatment,Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8 supporting the joint analysis of corresponding effect estimates in the same analysis. It seems that comparisons with TAU in older studiesReference Linehan, Armstrong, Suarez, Allmon and Heard25–Reference Bateman and Fonagy27 (where typical care for individuals with BPD was certainly poorer than today) or in countries where TAU is of lower qualityReference Majdara, Rahimmian, Talepassand and Gregory62 might be associated with larger effect estimates, whereas more recent comparisons of the same treatments and outcomesReference Carter, Willcox, Lewin, Conrad and Bendit28,Reference Laurenssen, Luyten, Kikkert, Westra, Peen and Soons41,Reference Feigenbaum, Fonagy, Pilling, Jones, Wildgoose and Bebbington56,Reference Jørgensen, Freund, Bøye, Jordet, Andersen and Kjølbye60,Reference Bateman and Fonagy65 or studies in higher-income countriesReference Gregory, Chlebowski, Kang, Remen, Soderberg and Stepkovitch40 result in smaller effects. However, a recent meta-analysis found evidence that participants allocated to TAU in general tend to improve to a limited extent, with possible reasons being the disclosure of the diagnosis, involvement of a concerned healthcare professional and time effects.Reference Finch, Iliakis, Masland and Choi-Kain97 This finding points to the need for conducting RCTs to find out the very treatment effects beyond these general factors.
In terms of outcomes, it is evident that there still is no consensus about a core battery of outcomes and measures to be used in BPD treatment evaluation studies. Although specific treatments build on different aetiology models and postulate different core problems,Reference Karterud and Kongerslev98 they tend to prioritise and assess different outcomes. For instance, MBT considers a lack of the ability to mentalise, i.e. to identify mental states (such as beliefs, wishes, feelings, thoughts, etc.) in oneself and others, as the BPD core problem, which leads to interpersonal difficulties. DBT, however, considers a disturbed emotion regulation as the core problem, which leads to self-harming and suicidal behaviour. Therefore, MBT studies usually report on interpersonal problems, but not impulsive or affective-dysregulative outcomes, whereas the opposite is the case for DBT. However, it would be helpful to know how different therapies perform on a common set of BPD-specific outcomes, to identify their respective profiles of action. Fortunately, efforts have been made recently by an international consortium of researchers to identify a core standard battery of outcomes for individuals with personality disorders.Reference Prevolnik Rupel, Jagger, Fialho, Chadderton, Gintner and Arntz99 To date, BPD-specific measures are available that allow for a very detailed assessment of individual BPD symptoms, like the Zan-BPD,Reference Zanarini, Vujanovic, Parachini, Boulanger, Frankenburg and Hennen79 Clinical Global Impression Scale adapted for BPD (CGI-BPD)Reference Perez, Barrachina, Soler, Pascual, Campins and Puigdemont100 or BPDSI-IV.Reference Arntz, van den Hoorn, Cornelis, Verheul, van den Bosch and de Bie73 Until recently, several BPD-intrinsic outcomes that are specifically important for individuals affected are still neglected across all studies, like avoidance of abandonment, chronic feelings of emptiness or identity disturbance. Moreover, longitudinal findings point to the relevance of psychosocial outcomes, as many individuals affected by BPD experience impaired social and vocational functioning over sustained periods of time, even after BPD-specific symptoms have diminished and the full diagnostic criteria are no longer met.Reference Zanarini, Frankenburg, Reich and Fitzmaurice101–Reference Bohus, Stoffers-Winterling, Sharp, Krause-Utz, Schmahl and Lieb103 However, the evidence of long-term outcomes of psychotherapies in BPD is still scarce. More studies would be required to accurately evaluate these treatments.
Quality of the evidence
Across all included studies, incomplete outcome reporting (attrition bias) and other bias in terms of affiliations of the study authors to the treatment under test, or different amounts of attention spent to the treatment groups, were the most common reasons for a high risk-of-bias rating (34.4 and 56.3%). The quality of the overall evidence was rated very low for the majority of comparisons and outcomes, although there was also moderate-quality evidence available for some outcomes of DBT-ST, and low-quality evidence for DBT, MBT, ERG, MACT and STEPPS. The most limiting factor was imprecision of results because of the restriction to limited observations (single study effects only, small sample sizes) or risk of bias for the above-mentioned reasons in the primary studies. We observed a clear tendency of larger effect sizes in smaller samples, which may be a result of methodological issues in smaller samples or bias owing to non-publication of unfavourable results.Reference Sterne and Egger81,Reference Page, Higgins, Clayton, Sterne, Hróbjartsson and Savović82,104
Potential biases in the review process
Since we applied a maximally sensitive and comprehensive search strategy, including searches in a large number of bibliographic databases and study registers, tracing of reference lists and contacting study authors if relevant information was missing, and as we did not apply any language, publication format or publication date restrictions, we are confident that we have identified all relevant eligible evidence. As both data extractions and risk-of-bias ratings were doubly assessed by two reviewers independently, and disagreements resolved, we did our best to avoid any bias during the review process.
Agreements and disagreements with other systematic reviews and meta-analyses
Cristea et alReference Cristea, Gentili, Cotet, Palomba, Barbui and Cuijpers105 provided a systematic review and meta-analysis of psychotherapies for BPD, covering relevant studies published until November 2015. Not surprisingly, the evidence has accumulated since this time, so this paper included a substantially higher number of studies that were not available at the time that review was prepared.Reference Gratz, Tull and Levy34,Reference Bianchini, Cofini, Curto, Lagrotteria, Manzi and Navari38,Reference Kredlow, Szuhany, Lo, Xie, Gottlieb and Rosenberg39,Reference Laurenssen, Luyten, Kikkert, Westra, Peen and Soons41,Reference Davidson, Brown, James, Kirk and Richardson55–Reference Kramer, Pascual-Leone, Berthoud, de Roten, Marquet and Kolly57,Reference McMain, Guimond, Barnhart, Habinski and Streiner66,Reference Stanley67 For DBT, Cristea et al report an effect estimate of Hedge's g = 0.34 (95% CI 0.15–0.53) on BPD-relevant measures, which parallels the findings of this paper for the effect of standard DBT on self-harm (SMD −0.32, 95% CI −0.92 to −0.16). As substantially broader categories of interventions were applied by Cristea et al (i.e. treatments were grouped into DBT, psychodynamic approaches, CBT or other interventions), and so the remaining findings cannot be compared with the results of this paper.
Oud et al published another systematic review and meta-analysis of specialised psychotherapies for adults with BPD, which covers the evidence up to November 2017.Reference Oud, Arntz, Hermens, Verhoef and Kendall106 In contrast to our review, eligible interventions were restricted to DBT, MBT, SFT and TFP. As for the review of Cristea et al, new evidence has become available that had not been included in the Oud et al review (four studies on DBT,Reference Bianchini, Cofini, Curto, Lagrotteria, Manzi and Navari38,Reference Kramer, Pascual-Leone, Berthoud, de Roten, Marquet and Kolly57,Reference McMain, Guimond, Barnhart, Habinski and Streiner66,Reference Stanley67 one study on MBTReference Laurenssen, Luyten, Kikkert, Westra, Peen and Soons41). Nonetheless, the findings of Oud et al and this review do not differ substantially for those interventions that had been subject to both reviews. Also, the rating of the quality of the evidence as low or very low for the main part of findings still applies.
In conclusion, the findings of this review support the use of psychotherapy in BPD.Reference Simonsen, Bateman, Bohus, Dalewijk, Doering and Kaera2 Although the overall quality of the evidence is low to very low for most interventions, the evidence on drug treatments is neither more robust in the main part, nor does it suggest any substantial treatment effects for any single drug.Reference Stoffers-Winterling, Völlm and Lieb6,Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8,Reference Stoffers, Vollm, Rucker, Timmer, Huband and Lieb107 One of the major findings of this review is the evidence of promising effects of add-on group interventions, especially DBT-ST, ERG, MACT and STEPPS. Although this review does not allow for the assessment of the relative efficacy of individual versus group treatments, the results support the notion that add-on group interventions should be provided to individuals with BPD who already undergo treatment, if group treatments are not yet part of the therapy provided. As a recent meta-analysis found evidence of limited improvements in control treatments,Reference Finch, Iliakis, Masland and Choi-Kain97 it may be reasonable to supplement non-specialised treatment by BPD-specific group interventions, as long as no specialist individual treatment is available. However, individuals with BPD must not be detained from coherent, comprehensive treatments, as the encouraging effects of add-on interventions have only been observed in the context of ongoing treatments, Moreover, the long-term effects of add-on treatments are uncertain.
More replication studies are needed to increase the certainty of the evidence, and they should preferably be conducted by independent research groups not affiliated with any treatment in this field. More research is also needed for interventions that have been developed to meet the needs of individuals with BPD and defined comorbidities, such as post-traumatic stress disorder,Reference Bohus, Dyer, Priebe, Krüger, Kleindienst and Schmahl86–Reference Harned, Korslund and Linehan88 substance use disordersReference Philips, Wennberg, Konradsson and Franck90,Reference Santisteban, Mena, Muir, McCabe, Abalo and Cummings108 or eating disorders.Reference Robinson89 To date, no such treatment has ever been investigated in a second RCT, which would be necessary to have reasonable confidence in the evidence. Future research should include more men with BPD, if not solely focus on such samples, as BPD is equally prevalent in both genders, and gender-specific manifestations still lead to a gender biasReference Neacsiu, Eberle, Keng, Fang and Rosenthal85 in healthcare and research settings. In terms of outcomes, a common core battery of relevant outcomes in BPD treatment studies would be most desirable, and future studies should address these recommendations.Reference Prevolnik Rupel, Jagger, Fialho, Chadderton, Gintner and Arntz99 From our point of view, outcome assessment should at least include an assessment of any BPD criteria as defined by DSM, which can be done by the use of the Zan-BPD,Reference Zanarini, Vujanovic, Parachini, Boulanger, Frankenburg and Hennen79 BPSDI-IVReference Arntz, van den Hoorn, Cornelis, Verheul, van den Bosch and de Bie73 or CGI-BPD, for example.Reference Perez, Barrachina, Soler, Pascual, Campins and Puigdemont100 To reflect the reality of individuals affected by BPD, the observation periods should be extended so long-term effects could be followed up. This is true both for standalone and add-on treatments, the sustainability of which still needs to be established. Also, a consensus regarding adequate control treatments could help to understand the true effects of experimental treatments. Control groups need to be designed and sufficiently described to allow for ascribing observed between-group effects to individual experimentally manipulated factors, be it the use or non-use of a coherent treatment protocol, or the use of a specific treatment approach. In an ideal world, not only would participants be randomly allocated to treatment and control groups, but also intervenors, or intervenor teams to treatments. Finally, although we can be sure that psychotherapy in general is helpful for individuals with BPD,Reference Storebø, Stoffers-Winterling, Völlm, Kongerslev, Mattivi and Jørgensen8,Reference Cristea, Gentili, Cotet, Palomba, Barbui and Cuijpers105,Reference Oud, Arntz, Hermens, Verhoef and Kendall106 more research is needed to understand who benefits most from which kind of treatment. A project aiming to investigate this question using an individual patient data meta-analysis is under way.Reference Storebø, Ribeiro, Kongerslev, Stoffers-Winterling, Sedoc Jørgensen and Lieb109
Supplementary material
To view supplementary material for this article, please visit http://doi.org/10.1192/bjp.2021.204.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and/or its supplementary materials.
Acknowledgements
We thank Trine Lacoppidan Kæstel for conducting the bibliographic literature searches.
Author contributions
J.M.S.-W. and O.J.S. designed and conceived the study, and drafted the manuscript. J.M.S.-W. was responsible for statistical analyses. All authors revised the manuscript. All authors have agreed on the final manuscript and the decision to submit it for publication.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Declaration of interest
J.M.S.-W. is a board-certified psychotherapist (CBT) and received training in DBT. She has no financial conflicts of interest to declare. O.J.S. is trained in psychoanalytic group analysis and psychoanalytic child and adolescent individual psychotherapy and was involved in a trial of MBT for adolescents with BPD. He has no financial conflicts of interests to declare. M.T.K. is a certified MBT therapist and supervisor. He receives money from conducting MBT training. M.S.-J. is trained in DBT and psychodynamic therapy and was involved in a trial on MBT for adolescents with BPD. She has no financial conflicts of interests to declare. E.S. is trained in psychoanalytic group analysis. K.L. is a cognitive–behavioural psychotherapist with a special interest in schema therapy. E.F., A.T., C.P.S., H.E.C., J.P.R. and B.A.V. have no conflicts of interest to declare.










eLetters
No eLetters have been published for this article.