The glutamate hypothesis (Reference Goff and CoyleGoff & Coyle, 2001), one of the leading neurochemical theories of schizophrenia, originated in and remains to a considerable extent driven by the observation that phencyclidine and other glutamate antagonist drugs induce symptoms similar to those of schizophrenia. In an influential review, Javitt & Zukin (Reference Javitt and Zukin1991) drew attention to case reports describing florid psychotic states in individuals who misused phencyclidine, and also noted that, when given to healthy volunteers, the drug induced paranoia, perceptual changes and a wide range of other symptoms including disorganisation of thought, negativism, apathy, withdrawal, poverty of speech, perseveration and catatonic posturing. Phencyclidine is now considered too toxic for experimental use in humans, and interest has turned to its structural analogue, ketamine. Several studies have administered this drug to healthy participants and have shown that it causes increases in both positive and negative symptom scores on rating scales (Reference Krystal, Karper and SeibylKrystal et al, 1994; Adler et al, Reference Adler, Goldberg and Malhotra1998, Reference Adler, Malhotra and Elman1999; Reference Newcomer, Farber and Jevtovic-TodorovicNewcomer et al, 1999; Reference Lahti, Weiler and MichaelidisLahti et al, 2001). However, beyond noting the occurrence of heightened and distorted perception, ideas of reference and, at high dosage, thought disorder, these studies did not describe the symptoms induced in any great detail. As the effects of ketamine are currently being characterised as a model of schizophrenic psychopathology, it is important to document the psychopathological effects of the compound properly.
METHOD
Participants
By advertisement, 15 right-handed volunteers were recruited from the local community. History of psychiatric or physical illness, head injury, drug or alcohol dependence and smoking were exclusion factors. Participants were also screened to exclude major mental illness (i.e. schizophrenia, bipolar disorder or major depression) in first- and second-degree relatives. This was because of the potential risk of administering psychoactive drugs to individuals with increased vulnerability to mental illness, and also to reduce the possibility of reporting non-drug-related symptoms. Family history of alcoholism was also classed as an exclusion factor on the basis of earlier data showing differential susceptibility to N-methyl-d-aspartate receptor antagonists in these individuals (Reference Krystal, Petrakis and KrupitskyKrystal et al, 2003; Reference Petrakis, Limoncelli and GueorguievaPetrakis et al, 2004). There were 8 men and 7 women. Their mean age was 29±7 (range 20-47 years). Their mean IQ, estimated using the National Adult Reading Test (NART; Reference NelsonNelson, 1982) was 113±4. This study was approved by the Cambridge Local Research Ethics Committee. All participants gave written informed consent.
Drug administration
The participants attended a clinical research ward on two occasions, where they received either ketamine or placebo by means of a controlled infusion for approximately 2 h. The study was double masked - only the anaesthetist who supervised the procedure knew whether the individual was receiving ketamine or placebo. The sessions were separated by at least 3 weeks.
Bilateral intravenous catheters were inserted into the volunteers' forearms, one for ketamine infusion, the other for serial blood sampling to assay plasma ketamine levels. Racemic ketamine (1 mg/ml solution) was administered by bolus and then by continuous infusion using a computerised pump (Graseby 3500, Graseby Medical, UK). The pump was programmed (Anaetech, UK) to infuse ketamine continuously at varying doses in order to achieve constant estimated target plasma concentrations, using pharmacokinetic parameters of a three-compartment model (Reference Domino, Domino and DominoDomino et al, 1982).
While being infused, participants underwent a functional neuroimaging experiment during which they performed a series of cognitive tasks on a target level of ketamine of 100 ng/ml plasma (neuropsychological and functional imaging data will be reported elsewhere). Following the functional magnetic resonance imaging session (which lasted approximately 1 h) the infusion pump administering the drug was re-set to give a target plasma level of 200 ng/ml. After 20 min, further cognitive testing was administered, followed by a clinical assessment. In order to ensure that the intended target levels of the drug were achieved, blood was sampled 20 min after the dose increment. Volunteers were monitored for a further 45 min in order to ensure satisfactory post-medication recovery.
Assessment of symptoms
While receiving ketamine at the 200 ng/ml plasma target level, participants were interviewed using a shortened form of the Present State Examination, 9th edition (PSE; Reference Wing, Cooper and SartoriusWing et al, 1974). This covers a wide range of psychotic and non-psychotic psychopathology in a phenomenologically rigorous way.
The PSE interview produced extended speech in most of the volunteers. As an additional way of eliciting speech for assessment of thought disorder, they were engaged in general conversation, asked to describe their interests and a recent holiday or trip, and then asked to recount a fairy story or to describe the plot of a book or film they had read or seen recently.
The volunteers were also administered the Clinician Administered Dissociative States Scale (CADSS; Reference Bremner, Krystal and PutnamBremner et al, 1998). This scale has previously been used in studies of the effects of ketamine on healthy people (Reference Krystal, Karper and SeibylKrystal et al, 1994; Reference Curran and MorganCurran & Morgan, 2000). It consists of 19 items rated 0-4 by the participant (0=not at all, 4=extremely), covering questions such as:
-
• do things seem to be moving in slow motion?
-
• do you feel disconnected from your own body?
-
• do colours seem much brighter than you would have expected?
There are also seven observer-rated items in the scale which were not used in this study.
The interviews were video recorded and the tapes were viewed by two of the investigators (E.P.C. and P.J.M.). Responses to the PSE questions were rated using the conventions and anchor points of the schedule as far as possible. The main modification required concerned the duration of symptoms, which are normally rated over the preceding month. Thought disorder was rated using the version of the Thought Language and Communication (TLC) scale in the Comprehensive Assessment of Symptoms and History (Reference AndreasenAndreasen, 1987). For the purposes of this study, poverty of content of speech was classified as an element of positive formal thought disorder; this was on the grounds that it has been found to segregate with the disorganisation syndrome in factor-analytic studies (see Reference McKenna and OhMcKenna & Oh, 2005). Negative symptoms were rated using two sub-scales of the Schedule for the Assessment of Negative Symptoms (SANS; Reference AndreasenAndreasen, 1982), affective flattening or blunting and alogia. Two of the remaining three sub-scales of the SANS were considered unrateable in the context of this study; avolition-apathy contains only two items, grooming plus hygiene and impersistence at work or school; and anhedonia-asociality rates recreational interests and activities, sexual interest and activity, and ability to feel intimacy and closeness. It was considered inappropriate to rate attentional impairment in people taking a drug known to impair cognitive function.
RESULTS
Plasma ketamine levels at the time nearest to the clinical ratings were close to the target level (mean 209.6±48.0, range 130.7-303.3). Despite often feeling ill and having obvious difficulties concentrating, the participants gave surprisingly clear accounts of their experiences. In a few cases, when the drug was given on the first test occasion, the volunteers failed to disclose symptoms but then described them when questioned the next time; such retrospective accounts were included. It should be noted that, because of nausea and vomiting, obviously poor concentration and spontaneous descriptions of typical ketamine experiences, it was impossible to maintain masking in virtually all cases.
PSE ratings
PSE ratings for the 15 volunteers are shown in Table 1. A number of non-specific symptoms were universally or very frequently reported, including subjectively inefficient thinking and poor concentration. Tiredness was only slightly less frequent, being reported by ten people; ten also reported subjective nervous tension (which in the PSE corresponds to anxiety without autonomic accompaniments).
Table 1 PSE ratings in 15 volunteers receiving ketamine
| PSE symptom | No. of participants with rating 1 | ||||
|---|---|---|---|---|---|
| 1 | 2 | 1 or 2 | |||
| Tiredness | 6 | 4 | 10 | ||
| Subjective nervous tension | 5 | 3 | 8 | ||
| Autonomic anxiety | 2 | 2 | 4 | ||
| Subjectively inefficient thinking | 2 | 12 | 14 | ||
| Poor concentration | 3 | 11 | 14 | ||
| Depressed mood | 2 | 1 | 3 | ||
| Simple ideas of reference | 4 | 3 | 7 | ||
| Expansive mood | 2 | 0 | 2 | ||
| Subjective ideomotor pressure | 2 | 0 | 2 | ||
| Derealisation | 2 | 2 | 4 | ||
| Depersonalisation | 3 | 1 | 4 | ||
| Delusional mood | 3 | 0 | 3 | ||
| Heightened perception | 2 | 8 | 10 | ||
| Dulled perception | 1 | 0 | 1 | ||
| Changed perception | 5 | 8 | 13 | ||
| Changed perception of time | 1 | 10 | 11 | ||
| Auditory hallucinations | 0 | 0 | 0 | ||
| Visual hallucinations | 0 | 0 | 0 | ||
| Olfactory hallucinations | 0 | 0 | 0 | ||
| Delusion that participant smells | 0 | 0 | 0 | ||
| Delusions of control | 1 | 0 | 1 | ||
| Delusions of reference | 3 | 0 | 3 | ||
| Delusions of misinterpretation | 2 | 1 | 3 | ||
| Delusions of persecution | 0 | 0 | 0 | ||
PSE, Present State Examination; No., number
1. Some volunteers were rated 1 on the following symptoms during placebo: tiredness (6), subjective nervous tension (2), autonomic anxiety (1), subjectively inefficient thinking (2), poor concentration (2), expansive mood (1), derealisation (1), depersonalisation (1)
Alterations in perception were also frequent; ten people reported heightened perception which commonly took the form of increased sensitivity to noise but also, in some cases, increased brightness of colours. One individual reported both heightening and dulling of perception. Changed perception was even more common, being reported by 13 volunteers. Visual experiences of this type took a variety of forms, ranging from changes in sharpness: ‘Things don't look right, cabinets don't look hard, everything looks rounded, edges not sharp', or ‘I couldn't make out the outline of things', or ‘Colours are blurred into one’, to loss of depth: ‘You appear like a 2D image’, and alterations in size and shape: ‘My hands look small, but the fingers are really long’, or ‘My legs look very big and funny shaped, like another person's'. One participant described a more complex visual perceptual change where the interviewer, who was heavily pregnant, gradually came to look more and more like a dome with a pair of eyes on top.
There were also perceptual distortions in other modalilties: ‘Things feel more liquid when I touch them’, or ‘I am feeling like I am made of sandpaper’, or ‘I feel like I'm shrunken inside', or ‘Each limb seems separate, detached from each other’, or ‘Disconnected from arms’. Several people described feeling as if parts of their body or objects they were holding were moving or not in the position they knew they were in; for example, the keyboard was continually sliding off their lap, or their foot was sliding across the floor, their arms felt like they were crossed when they were by their sides or they were slouched forward when they were sitting upright.
Changed perception of time was described by 11 participants. This took the form of slowing in most cases, which was often marked: ‘It's stopped, feels like I've been here for hours', but in some cases there was an increase in subjective rate, or both. It is noteworthy that, although several individuals made statements pertaining to dreaminess and unreality: ‘It's a bit unreal', or ‘Not an out of body experience, but like I'm somewhere else', the phenomenologically rigorous forms of depersonalisation and derealisation in the PSE were only rated in four volunteers, one of whom also experienced it when receiving placebo. Descriptions here included: ‘People like acting, like in a movie’, or ‘Very strong feeling that things are an imitation of reality’, or ‘Like I'm watching a documentary, watching TV', or ‘It doesn't feel like there's anything outside this room'. Mean scores on the CADSS are shown in Fig. 1, and indicate the pervasiveness of this class of symptoms.
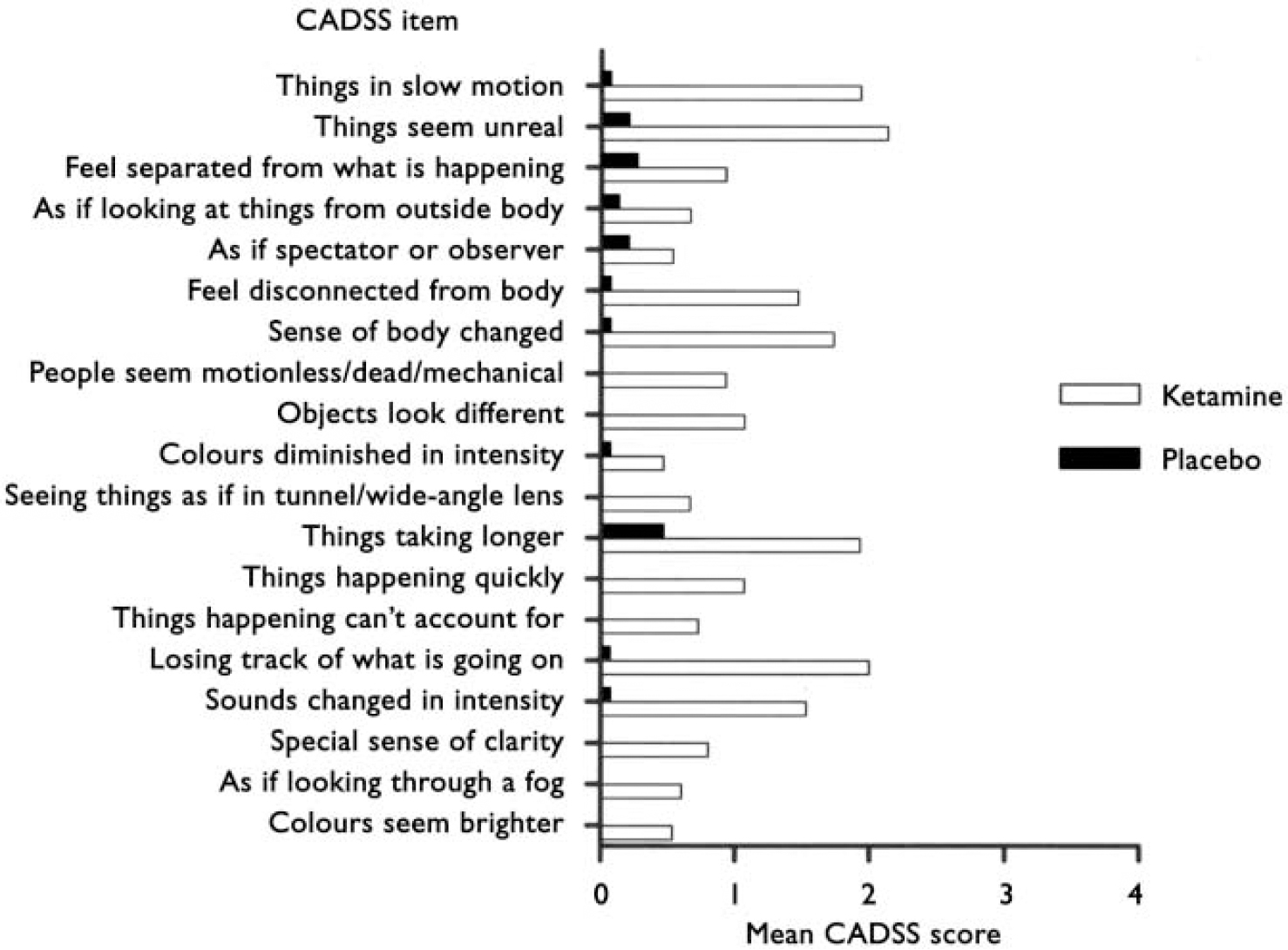
Fig. 1 Mean CADSS scores for 15 volunteers receiving ketamine or placebo. 0=not at all, 1=slightly, 2=moderately, 3=considerably, 4=extremely. CADSS, Clinician Administered Dissociative States Scale.
Several people described a peculiar inertia: ‘Everything takes a long time, for example moving my foot’, or ‘There's a delay between the thought and your mouth', or ‘Not in control of my body, can't move', or ‘Feel like it would be impossible to stand up, body feels like a ten ton weight… noticeable delay between thinking about moving and it happening’, or ‘More like a statue, sitting in one position, frozen. I couldn't move when I tried to. The will wasn't there', or ‘I don't feel in control of my muscles any more - like a zombie is a very good description of it. There's something making me just stay here. Something in my head is telling me I can't move', or ‘My limbs feel like they've got a magnet and they're stuck to the arm of the chair like lead weights', or ‘The will's there but difficult to get my legs to do what I want them to do'.
No participant reported auditory or visual hallucinations. The only possible exception concerned one who gave the following retrospective account: Abnormal beliefs were reported by seven volunteers. In almost all cases these took the form of referential ideas which sometimes seemed classifiable as ideas of reference, sometimes as delusions of reference and/or misinterpretation, and in three cases delusional mood. However, the central experience tended to be similar from person to person (Appendix 1). In the PSE, delusions are rated as either partially held (1) or fully held (2). Only one individual was rated as 2, stating: ‘People at the scanner were spies, I was convinced’. One of the seven participants who reported referential ideas was also rated 1 on delusions of control, stating when questioned about passivity, ‘If I didn't have this drug, I'd feel as though someone else was controlling my movements'.
‘It felt like there were more people in the room than two, presence of four people. I could see shapes of people moving but I couldn't keep track and they were all talking. I could hear people talking but I couldn't tell who was doing the talking - so it could have been something inside my head, I don't know. But I was definitely hearing things that I couldn't just place to any specific person or thing'.
Several volunteers gave accounts of subjective alterations of thought. Three people described something similar to thought block, the subjective experience of having no thoughts in one's head persisting for some time: ‘At times it felt like my body was here but my mind wasn't. As if I had no thoughts at all'; or ‘You just sit there and your mind completely clears of everything. It's a hard thing to describe. I wouldn't say someone was stealing the thoughts, they're just not happening'; or ‘I haven't really got any thoughts. All of a sudden things fly into my mind but I don't feel like I've got any. I feel like I can't think outside this room'. Two individuals were rated on subjective ideomotor pressure: ‘Ideas keep barging in’; or ‘Full of ideas about my research’. One described a phenomenon possibly reminiscent of thought insertion: ‘There were thoughts that were happening that I wouldn't normally think about and it just seems that someone is putting them on there'. When asked ‘They are not your own thoughts?’, the reply was ‘They look like someone else's thoughts'. ‘Like telepathy?’ ‘Yeah. It's like it's your thought but it's coming from somewhere else.'
TLC ratings
The participants frequently indicated that they thought they were rambling, losing track of what they were supposed to be talking about, or not in control of what they were saying. Objectively, however, none of them became thought disordered to a degree that impaired the interview. Only 3 of 15 volunteers were given global TLC ratings of more than zero, and in all cases, this was 1 (questionable). Two were given ratings of 2 (mild) on individual TLC items, one on poverty of content of speech and the other on both poverty of content of speech and circumstantiality. In these two people speech remained understandable, but was vague and muddled at times and occasionally wandered off the point. Their recounting of fairy tales and other stories was also obviously affected by poor recollection. Examples of their speech are given in Appendix 2.
Circumstantiality was also observed to a minor extent (rating of 1) in four more participants, one of whom also showed it when receiving placebo. Two more individuals showed single instances of use of odd or inappropriate phrases; one stated that nothing looked ‘straight cut’ when describing perceptual changes. Another used the term ‘beer goggles’ to describe the way the world looked on ketamine. One confabulated when telling the story of one of the Harry Potter films, talking about the hero growing up.
SANS ratings
As shown in Table 2, 5 of the 15 volunteers were given a global score of 2 (mild) on the SANS sub-scale for affective flattening, 2 scored 3 (moderate) and 1 scored 4 (moderately severe). Most of the individual items in this sub-scale were rated in the volunteers, with the exception of inappropriate affect.
Table 2 Ratings1 on SANS affective flattening and alogia in participants receiving ketamine
| SANS item | S1 | S2 | S3 | S4 | S5 | S6 | S7 | S8 | S9 | S10 | S11 | S12 | S13 | S14 | S15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Global rating of affective flattening | 0 | 1 | 4 | 2 | 0 | 1 | 1 | 2[1] | 2[1] | 3 | 0 | 0 | 3 | 2 | 2 |
| Unchanging facial expression | 0 | 1 | 4 | 2 | 0 | 1 | 1 | 3[2] | 2[2] | 3 | 0 | 0 | 4 | 1 | 2 |
| Decreased spontaneous movements | 0 | 2 | 3 | 2 | 0 | 2 | 1 | 2 | 3[1] | 3[1] | 0 | 0 | 3 | 2 | 3 |
| Paucity of expressive gestures | 0 | 0 | 3 | 3 | 0 | 1 | 1 | 2 | 2[1] | 3 | 0 | 1 | 3 | 3 | 2 |
| Poor eye contact | 0 | 0 | 4 | 3 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Affective non-responsivity | 0 | 0 | 4 | 3 | 0 | 1 | 1 | 0 | 2[1] | 2 | 0 | 0 | 3 | 1 | 1 |
| Inappropriate affect | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Lack of vocal inflections | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 1 | 1[1] | 0 | 0 | 0 | 2 | 0 | 0 |
| Global rating of alogia | 0 | 1 | 3 | 2 | 1 | 1 | 0 | 2[1] | 2 | 2 | 2 | 0 | 3 | 0 | 1 |
| Poverty of speech | 0 | 1 | 3 | 2 | 0 | 1 | 0 | 3[1] | 2 | 2 | 2 | 0 | 3 | 1 | 2 |
| Blocking | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Increased latency of response | 0 | 2 | 4 | 3 | 2 | 2 | 1 | 3[1] | 3[1] | 2 | 3 | 1 | 3 | 0 | 0 |
SANS, Scale for Assessment of Negative Symptoms; S, SANS rating
1. 0=absent, 1=questionable, 2=mild; 3=moderate, 4=moderately severe; 5=severe
Figures in square brackets indicate positive scores on placebo
Five participants also achieved a global score of 2 or greater on the SANS alogia sub-scale, with two scoring 3 (moderate). Of the individual abnormalities contributing to this overall score, poverty of speech was present in eight people and ten scored on increased latency of responding.
DISCUSSION
In this study, ketamine appeared to have four main effects:
-
(a) a general central nervous system (CNS) depressant and/or intoxicating effect;
-
(b) perceptual alterations but not hallucinations;
-
(c) referential ideas or delusions, plus other subjective changes in thinking;
-
(d) negative-type symptoms.
We were unable to replicate the widely cited finding that ketamine causes substantial levels of thought disorder; the changes in thought form seen in this study were infrequent and at most mild.
CNS depressant/intoxicating effects
This was attested to by the volunteers' universal complaints of subjectively inefficient thinking and poor concentration. Tiredness was probably also a feature, although this was not present in every case, and was also reported by six individuals receiving placebo. The effect was objectively evident in the participants' vagueness, muddling of thought, and poor recollection, which resembled the effects of alcohol and sedative drugs - in fact, some spontaneously stated that they felt like they were drunk. It is not surprising that an anaesthetic drug should have such effects. However, it may have a bearing on some of the other changes seen, particularly those in affect, speech and thinking.
Perceptual alterations
A second class of experience that ketamine induced was a range of perceptual alterations similar to those described in other studies of this drug and phencyclidine (Reference DoveDove, 1984; Reference Krystal, Karper and SeibylKrystal et al, 1994), which are often referred to as ‘dissociative’. The volunteers reported heightened, dulled and distorted perception in the visual, auditory and somatosensory spheres. Symptoms approximating to depersonalisation and derealisation were also described, but often it seemed as though the experiences were not captured particularly well by these terms. The frequency and intensity of reports of changed perception of time were also noteworthy, particularly as this symptom is otherwise encountered only rarely in psychiatry.
No one described visual hallucinations, and only one person reported anything that could be construed as auditory hallucinations - and this account was retrospective and not convincing. Such a finding is consistent with that of Krystal et al (Reference Krystal, Karper and Seibyl1994), who reported significant increases in scores on the Brief Psychiatric Rating Scale (BPRS; Reference Overall and GorhamOverall & Gorham, 1962) item, hallucinatory behaviour, but went on to state that the experiences were limited to illusions. In contrast, Lahti et al (Reference Lahti, Weiler and Michaelidis2001) stated that auditory or visual hallucinations occurred in 4 out of 18 healthy people when receiving ketamine; however, no description of the experiences was given. It is possible that the use of the BPRS in virtually all previous studies, where illusions are rated on the same scale as hallucinations, has helped propagate the belief that ketamine routinely induces hallucinations. Interestingly, in one of the original studies of phencyclidine, Luby et al (Reference Luby, Gottlieb and Cohen1962) stated that whereas distortions of body image and depersonalisation were universal, genuine hallucinations were not a characteristic effect of the drug.
Referential ideas and other subjective changes in thinking
Ketamine induced what appeared to be ideas or even partially held delusions of reference in approximately half the group studied. Other studies of the effects of ketamine on healthy volunteers have recorded similar phenomena. Krystal et al (Reference Krystal, Karper and Seibyl1994) stated that several of their group under study expressed ideas about staff in neighbouring rooms talking about them in ominous ways. Lahti et al (Reference Lahti, Weiler and Michaelidis2001) described suspiciousness in 1 of their 18 volunteers receiving ketamine, and ideas of reference in 2 of them. Bowdle et al (Reference Bowdle, Radant and Cowley1998) reported dose-dependent increases in rating scale scores for reference (e.g. ‘I had the idea that events, objects or other people had particular meaning that was specific for me’) and suspiciousness (e.g. ‘I had suspicious ideas or the belief that others were against me’).
The unmistakable impression in our study was that the volunteers were all experiencing a similar phenomenon, described in different ways and always with insight, but nevertheless compelling. The fact that their descriptions did not fit precisely into the PSE categories of ideas of reference, delusional mood or delusions of reference and misinterpretation is perhaps understandable, given that the abnormal ideas developed over a greatly compressed period of time compared with the typical evolution of symptoms in functional psychotic disorders.
Three of the group in this study described a subjective experience reminiscent of thought block. There were hints in their accounts of this and other subjective thought alterations of a willingness to entertain bizarre or delusional explanations, as for example in statements such as: ‘There were thoughts that were happening that I wouldn't normally think about and it just seems that someone is putting them on there'. This might also have applied to the person who, when questioned about his marked subjective inertia, stated: ‘If I didn't have this drug, I'd feel as though someone else was controlling my movements'. Possibly relevant in this regard, Lahti et al (Reference Lahti, Weiler and Michaelidis2001) mentioned that one of their participants stated that people could hear her thoughts.
Thought disorder
In this study, only three individuals developed anything resembling thought disorder and, in each case, their speech was only minimally difficult to follow. The main abnormalities rated were poverty of content of speech and circumstantiality. There were only very occasional uses of unusual or inappropriate words, such as ‘straight cut’ and ‘beer goggles’, the latter of which is a common British idiom, although not in the context in which the person used it. This finding thus fails to replicate that of Krystal et al (Reference Krystal, Karper and Seibyl1994), who found that ketamine at high dose, but not at low dose, induced formal thought disorder ‘with loosening of associations, derailment, stilted speech and other alterations’. In a study using the TLC scale, Adler et al (Reference Adler, Goldberg and Malhotra1998, Reference Adler, Malhotra and Elman1999) also found that ketamine produced significant increases in TLC total scores in ten healthy people, and this applied to sub-scales measuring both verbal productivity (poverty of speech) and disconnection (poverty of content, tangentiality, derailment, incoherence, circumstantiality and loss of goal). In their study, however, the highest ratings were on circumstantiality and loss of goal, and even so the mean scores (1.2 and 1.3 respectively on a 0-5 scale) were low.
It is still possible to argue that ketamine specifically caused poverty of content of speech and circumstantiality in this study (particularly as this latter abnormality was observed to a questionable degree in four more volunteers). However, as more typical schizophrenic phenomena such as derailment, tangentiality and neologisms were not observed, what was observed might equally well be considered to be the vague, muddled thinking, accompanied by poor memory, seen in states of intoxication. Once again, it is instructive to read the early description of the effects of phencyclidine by Luby et al (Reference Luby, Cohen and Rosenbaum1959). Under ‘disorganisation of thought’ they stated:
‘The subjects appeared to be struggling to describe feeling states which they were unable to define except in fragmentary phrases. To obtain information at the height of the drug effects, the examiner was forced to ask extremely simple and direct questions. Proverbs were interpreted in a fragmentary, concrete manner, or were simply repeated as though this implied meaning. Without the drug, in response to “a drowning man will clutch at a straw”, a subject responded: “A person who is desperate will grab at anything regardless of its value to him”. In the drug state, he answered: “I think it is - drowning man will clutch at a straw. It means a drowning man will clutch”. The loose and asyndetic quality of thinking is illustrated by the following response to TAT Card 8BM: “Oh, there is a doctor and a surgeon and a boy and a gun and a boy, boy, boy, boy, boy, knife, gun, man, card, surgeon…”. The performance of serial sevens became an impossible task for most subjects.'
Negative symptoms
In contrast to positive formal thought disorder, poverty of speech was evident in over half the sample, where it was rated as mild or moderate. This was associated with another element of Andreasen's alogia, increased latency of responding. Unchanging facial expression and other items in the SANS affective flattening category were also frequently noted and were rated up to moderately severe.
Even so, it is an open question whether ketamine genuinely induces negative symptoms. On the one hand, it is possible to construct an account whereby drugs such as ketamine and phencyclidine affect frontal systems and produce temporary symptoms of the frontal lobe syndrome, which is itself an analogue of negative symptoms according to leading contemporary theories (Reference LiddleLiddle, 1987; Reference WeinbergerWeinberger, 1988). On the other hand, the possibility has to be considered that the changes observed in this and other studies were simply manifestations of the drug's general CNS depressant effect. For example, the literature on phencyclidine contains numerous references to apathy, lethargy and even stupor (Reference Johnstone, Evans and BaigelJohnstone et al, 1959; Reference Luby, Cohen and RosenbaumLuby et al, 1959; Reference McCarron, Schulze and ThompsonMcCarron et al, 1981), but these were generally mentioned in close association with sedation. Our study, however, could be interpreted as pointing to a degree of dissociation between apathy and sedation, on three grounds. First, whereas ten of the group reported tiredness, this was only severe in four. Second, one of the anaesthetists who administered the drug commented that the participants were not objectively sedated, at least by clinical standards. Third, several of the subjective descriptions of inertia could also be considered to be a subjective counterpart of apathy rather than sedation.
In summary, this study suggests that ketamine has a limited psychotomimetic effect, which is most convincing with respect to an ability to induce referential beliefs similar to delusions. It may also induce experiences which could serve as a basis for certain first-rank symptoms, and possibly facilitate delusional explanations of these experiences. Auditory hallucinations do not appear to be part of the range of ketamine effects, and we were unable to confirm the findings that thought disorder is a characteristic effect of the drug. It may well be that ketamine causes affective flattening and poverty of speech, but this requires further investigation. Although the clear message has to be that acute ketamine administration does not reproduce the full picture of schizophrenia, the drug does seem to give rise to a subset of symptoms and it may prove useful in testing theories of specific symptoms such as delusions.
APPENDIX 1
Examples of volunteers' descriptions of referential ideas
Volunteer 4
I feel so enclosed, I almost feel as though I'm in a cage or… it's almost like a big brother type thing, people watching…. I know people aren't looking at me, but I feel as though people could be looking at me… as though there's cameras or something like that.
Volunteer 5
Some of the questions when I was in the scanner, it was like they were saying one thing but what they're actually trying to do is discover what's going on somewhere else. People saying what they're supposed to say. People seem to be saying things for effect, instead of saying what they actually want. Some of the questions in the scanner seemed like they were specially put to make you think about something else. [As] if one's doing something for a reason but trying to make it look like they don't mean to do it. Things specially arranged beyond the experiment…. It's like someone wants you to think something and so they make you.
Volunteer 9
I feel they may talk about me. I think that they're thinking that I'm the centre of the world, although I know they're probably not. Laughing, not critical.
I feel like a puppet, I feel guided by people around, to say things.
[Volunteer also retrospectively described that she thought the interviewer was controlling her replies to questions by looking at her: people at the scanner were maybe spies. I was convinced].
Volunteer 11
I feel paranoid that people are [looking at me] but I know that they're not, ‘cause I'm in an experiment, so I know that they're not. I feel like I've not got control over what I'm saying, so I feel like what I am saying is not right, and then people are just looking at me and… OK. I feel as if people's reactions are different to me, reacting differently to me, but I don't feel people are gossiping about me. They just seem to be giving me a lot more attention, a lot more time, everything seems a lot slower. It's like that film [The Truman Show].
I feel things have been specially arranged beyond the experiment. I've got that feeling but I know they haven't.
It feels like something's happening but I'm not quite sure what's going on. I don't quite know what it is.
I feel like I'm the focus, everyone is watching me, which obviously you are doing. I feel like there's more to it than what's actually happening. I feel like I'm not being told everything. Something going to happen and haven't been told.
Volunteer 14
[During second (placebo) interview] I suppose I did [feel self-conscious during the first session]. Maybe people were looking at me longer than they would normally. A bit, definitely…. I think it could have been because of my concentration - I couldn't really make out what they were saying, and so maybe I then thought they were talking about me, and maybe judging me, judging my reaction to it. At the time maybe I thought they were a bit critical.
Volunteer 15
It feels as if I'm on stage being watched by an audience. Things are not as they should be. People might be laughing at me because I'm not myself.
APPENDIX 2
Changes in thought form demonstrated by two volunteers remaining on ketamine
TLC, Thought, Language and Communication Scale.
These extracts show only the most disordered segments of speech. TLC ratings were based on speech during the whole interview.
Volunteer 11
[Telling the story of Little Red Riding Hood]
There's a girl who wears a cape that was red, and it has a red hood. And her grandmother knitted - made it for her. She goes into the woods, there's a wolf there. And a woodcutter and… her grandmother… of the girl, Red Riding Hood. It's all just spinning around in my mind… and… if you want me to put it into a story…. There was a… I'm getting confused with the little boy who cried wolf. [Long pause] I don't know what to think, I thought I knew it but I didn't.
[Derailment=1, circumstantiality=1, poverty of content=2; global TLC rating=1.]
Volunteer 12
[Asked about derealisation]
I was thinking that it all, everything seemed really surreal when I came out of the scanner and everything. And it did seem all really strange. ‘Cause I was thinking about when… ‘Cause I've just read a book, a Victorian period drama called Fingersmith, it's about, well it's er a lesbian romp, really. It's basically about two girls - a fingersmith is a pickpocket. And it basically shows where a pickpocket, it's showing scams of different things, and basically one of the people, one of the characters in the story ends up in a madhouse, and they're not actually mad and they're put into the madhouse and then given all the drugs and everything and then they actually have to run away, and they're treated as if they are mad… [interrupted]
[Derailment=1, circumstantiality=2, poverty of content=2; global TLC rating=1.]






eLetters
No eLetters have been published for this article.