Young people with mental health problems can get ‘lost’ during transition of care from child and adolescent mental health services (CAMHS) to adult mental health services (AMHS). 1–Reference Singh3 Disruption of care during transition adversely affects the health, well-being and potential of this vulnerable group. Reference Lamb, Hill, Kelvin and Van Beinum2–9 Ideally, transition should be a planned, orderly and purposeful process of change from child-oriented to adult models of care, taking into account both developmental and illness-specific needs. 1,Reference Blum, Garell, Hodgman, Jorissen, Okinow and Orr10–12 If the process is seen simply as an administrative event between CAMHS and AMHS, many health and social care needs may remain unmet. Reference Vostanis13
Transition is often discussed but rarely studied. The national policy in the UK emphasises the need for smooth transition from CAMHS to AMHS Reference Lamb, Hill, Kelvin and Van Beinum2,14–17 but there is no published evidence on the process, models and outcomes of transition. A systematic review of 126 papers on transition found only one on a mental health population and only within the US context. Reference While, Forbes, Ullman, Lewis, Mathes and Griffiths5 Transition is a critical aspect of continuity of care, yet we know little about who makes such transitions, what are the predictors and outcomes of the process, and how it affects service users and their carers. Without such evidence, mental health services cannot develop and evaluate efficient models that promote successful transition or plan the future development and training programmes to improve transitional care. The TRACK study was designed to answer some of these questions in the UK context.
The overall aims of the TRACK study were to:
-
1 conduct an audit of the policies and procedures relating to transition within six mental health trusts in London and the West Midlands (three trusts in each region) (Stage 1);
-
2 evaluate the process of transition by a case-note survey identifying all actual and potential referrals (see below for definitions) from CAMHS to AMHS in the preceding year, ‘track’ their journey and outcomes in terms of referral and engagement with adult services, and determine the predictors of successful transition (Stage 2);
-
3 conduct qualitative interviews across organisational boundaries and services within health and social care agencies to identify specific organisational factors that constitute barriers and facilitators to transition and continuity of care (Stage 3);
-
4 explore the views of service users, carers and mental health professionals on the process of transition experience from a subsample of service users (Stage 4).
In this paper we present findings from Stages 2 and 4. A paper from Stage 1 has already been published. Reference Singh, Paul, Ford, Kramer and Weaver18 The TRACK report including Stage 3 findings is available in full at www.sdo.nihr.ac.uk/projdetails.php?ref=08-1613-117. The study received ethical approval from Wandsworth Local Research Ethics Committee.
Method
We used the following definitions: actual referrals were all individuals that crossed the transition boundary and were accepted by AMHS; and potential referrals included individuals that crossed the transition boundary but did not complete transition to AMHS, regardless of the reasons for non-transition. Transition pathways were categorised as optimal or sub-optimal. The optimal transition criteria were developed from an audit of CAMHS transition protocols Reference Singh, Paul, Ford, Kramer and Weaver18 and literature on good practice in relation to continuity of care. Reference Freeman, Crawford, Weaver, Low and de Jonge19 These criteria included:
-
(a) information transfer (information continuity): evidence that a referral letter, summary of CAMHS care, or CAMHS case notes were transferred to AMHS along with a contemporaneous risk assessment;
-
(b) period of parallel care (relational continuity): a period of joint working between CAMHS and AMHS during transition;
-
(c) transition planning (cross-boundary and team continuity): at least one meeting involving the service user and/or carer and a key professional from both CAMHS and AMHS prior to transfer of care;
-
(d) continuity of care (long-term continuity) – either engaged with AMHS 3 months post-transition or appropriately discharged by AMHS following transition.
Sub-optimal transitions were those that failed to meet one or more of the above criteria.
Design
The study was undertaken in six mental health trusts (service provider organisations within the National Health Service), three in Greater London and three in the West Midlands, covering a population of 8.1 million with wide socioeconomic, ethnic and urban–rural heterogeneity. All CAMHS teams that managed young people until the age of transition were included. Highly specialised and tertiary services (e.g. a national eating disorder service) were excluded because of the atypical population served and the logistical problems of tracking individuals from services that accept referrals from across the country.
Case ascertainment
Case ascertainment was a two-stage process. First, central databases of all included CAMHS were searched for open cases of individuals who had reached age x or above (where x is the age boundary for transition to AMHS). Since the age boundary for different services (x) varied, for each service x was specifically defined as per that service's transition protocol. Reference Singh, Paul, Ford, Kramer and Weaver18 In the next stage, all CAMHS clinicians within included services were contacted by letter and email explaining the study and requesting details of actual and potential referrals during the study period. Initial contacts were followed up by further emails and telephone calls during the study period until all clinicians had submitted cases or provided a nil response. For the qualitative study, the young people identified for inclusion were contacted through their care coordinators to explain the study and seek informed consent.
TRACKING tool
Two data extraction tools, one each for actual and potential referrals were devised and piloted for reliability. Data were collected on sociodemographic and clinical variables, transition pathways and transition outcomes (for actual referrals) and reasons for non-transition in potential referrals. Interrater reliability was checked by two researchers independently extracting data from the tools from five actual referrals from a site unrelated to the project. Comparing 491 non-text variables for each of the five cases, an error rate of less than 2% was found. Study tools are available in the full study report.
Ascertaining diagnoses
Since CAMHS case notes vary in recorded diagnoses, we categorised presenting problems into seven diagnostic groups: serious and enduring mental disorders, including schizophrenia, psychotic disorders, bipolar affective disorder, depression with psychosis; emotional/neurotic disorders, including anxiety, depression (without psychosis), post-traumatic stress disorder, obsessive–compulsive disorder; eating disorders, including anorexia nervosa, bulimia nervosa, atypical eating disorder; conduct disorders, including behavioural disorders; neurodevelopmental disorders, including autism-spectrum disorders, intellectual disabilities; substance use disorders, including alcohol and/or drug misuse; and emerging personality disorder. Data on presenting problems were discussed with three CAMHS clinicians (M.P., T.F. and T.K.) to assign a diagnostic group. Comorbidity was defined as the presence of more than one diagnostic category from the seven above.
Predictors of transition
In the absence of previous evidence, we could not develop a prediction model for transition. Instead a two-stage analysis was conducted with initial identification of independent variables with an association (P<0.05) with the dependent variable using Pearson χ2-tests (Fishers exact tests where necessary) for categorical variables and unpaired t-tests for continuous variables. Prior to logistic regression, significant independent variables that were highly associated with each other were recoded into a composite variable to reduce co-linearity. Two logistic regression analyses were planned: first, to determine predictors of achieving transition (being an actual rather than a potential referral); and second, to determine predictors of optimal transition. However, the small numbers of individuals identified in the study who experienced optimal transition precluded the second regression analysis (see Results). It was felt inappropriate to conduct a multilevel analysis as the study did not aim to determine the impact of trust-level variables on transition outcomes. With only six trusts in the sample, there would be insufficient variation in trust-level data for such an analysis. However, to account for possible clustering within trusts, i.e. to account for individuals within trusts being less variable than individuals between trusts, the logistic regression was repeated and standard errors (and therefore 95% confidence intervals and P-values) adjusted for cluster effects (see Results). This analysis was conducted using Stata version 9 for Windows.
Qualitative case studies
Semi-structured qualitative interviews were conducted with a subsample of service users who had completed transition, and where possible their carers and CAMHS and AMHS care coordinators. A purposive sample of service users (n = 20) was initially identified comprising 10 service users, each in two groups: those who did or did not remain engaged with AMHS 3 months post-transition. Within each group we sampled individuals with or without evidence of joint working between CAMHS and AMHS. Within this primary sampling frame we sought to achieve range and diversity in terms of study site, diagnosis, gender, ethnicity and whether or not the service user was an age outlier at time of transition. Service users who declined to participate or who were deemed clinically unsuitable for inclusion were substituted with a matched case. Interviews were conducted by two researchers (K.H. and Z.I.) using topic guides developed by the project team and amended to incorporate emergent themes from all study components. The main focus was on preparation for transition, transition experiences, transition outcomes and factors identifiable as related to positive or negative transition outcomes.
Qualitative analysis
Interviews were recorded, transcribed and entered onto NVivo software (www.qsrinternational.com). K.H. led the development and application of a coding frame with input from Z.I. and the qualitative study lead (T.W.). Use of NVivo facilitated investigator checking of coding. Qualitative analysis was undertaken using the constant comparative method within the framework approach described by Ritchie & Spencer. Reference Ritchie, Spencer, Bryman and Burgess20 This approach was particularly appropriate for integrating a thematic analysis built upon multiperspective data.
Results
Quantitative study results
We encountered major difficulties when searching the central CAMHS databases and these could not be interrogated using the study criteria (see full report for details). We therefore relied primarily on clinician recall to identify cases. A total of 154 individuals were thus identified (London 112; West Midlands 42). The rate of actual and potential referrals per 100 000 population in the London sites were 2.68 and 1.49 respectively and in the West Midlands sites 2.23 and 2.97 respectively. The service boundary for transition from CAMHS to AMHS (x) ranged from 16 to 21 years (mode 18).
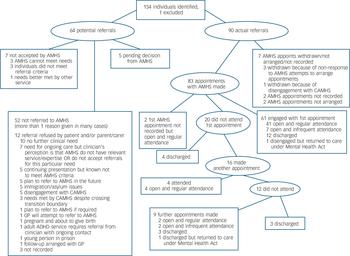
Fig. 1 Outcomes of all referrals from child and adolescent mental health services (CAMHS) to adult mental health services (AMHS).
GP, general practitioner; ADHD, attention-deficit hyperactivity disorder.
Transition pathways
Of the 154 participants, 90 (58%) were accepted by AMHS (i.e. actual referrals). Sixty-four (42%) were potential referrals (i.e. those who crossed the transition boundary during the study period but did not make a transition to AMHS). Transition pathways for the entire cohort are shown in Fig. 1.
Sample description
The total sample consisted of 78 (51%) males and 76 females with a mean age of 18.12 years (s.d. = 0.82). A third (31%) were White and 23% Black and minority ethnic, but ethnicity was not recorded in a large proportion (27%). The majority (71%) lived with their parents and nearly two-thirds were either in employment or education (60%). Diagnostically, half (n = 78) had emotional/neurotic disorders, a quarter (n = 38) had neurodevelopmental disorders and 22% (n = 34) had serious and enduring mental disorders. Other disorders included substance misuse (n = 14, 9%), conduct disorders (n = 6, 4%), eating disorders (n = 6, 4%) and emerging personality disorder (n = 4, 3%). For five individuals (3%) the presenting problem was not recorded. Almost a fifth (n = 29, 19%) had comorbid mental health disorders.
Sociodemographic and clinical variables
Table 1 shows sociodemographic and clinical details of the participants in the actual and potential referrals groups. Those in the actual referrals group were more likely to have been living with parents, having attended CAMHS with their parents, to be involved with a child protection agency or be a ‘looked after child’, been admitted to a psychiatric hospital, to have been detained under the Mental Health Act, to have a serious and enduring mental disorder, substance misuse, an emerging personality disorder or more than one category of presenting problem (comorbidity), but less likely to have an eating disorder. To reduce the number of variables to enter into the logistic regression, a known broader social risk score variable was created that equalled the sum of the following: ‘looked after child’, child protection involvement, youth offending team involvement, special educational needs or refugee/asylum seeker.
Table 1 Demographic variables comparing actual and potential referrals
| Variable | Actual referrals group (n = 90) | Potential referrals group (n = 54) | χ2 | P |
|---|---|---|---|---|
| Male, n (%) | 49 (54.4) | 29 (45.3) | 1.24 | 0.26 |
| Age at first referral to any CAMHS, years: mean (s.d.) | 13.34 (3.9) | 14.29 (2.9) | 1.69 | 0.09 |
| English as first language, n (%) | 82 (91.1) | 54 (84.4) | 1.64 | 0.200 |
| Living with parent, n (%) | 58 (64.4) | 52 (81.3) | 6.99 | 0.03 |
| Educational attainment GCSEs and below, n (%) | 43 (47.8) | 27 (42.2) | 1.35 | 0.51 |
| Parent attended CAMHS, n (%) | 34 (37.8) | 20 (31.3) | 11.64 | 0.003 |
| Positive family history of mental health problems, n (%) | 51 (56.7) | 22 (34.4) | 3.64 | 0.06 |
| ‘Looked after child’ while attending CAMHS, n (%) | 24 (26.7) | 8 (12.5) | 4.56 | 0.03 |
| Evidence of special educational needs, n (%) | 19 (21.1) | 10 (15.6) | 0.74 | 0.39 |
| Evidence of child protection involvement, n (%) | 12 (13.3) | 1 (1.6) | 6.70 | 0.01 |
| Evidence of youth offending team involvement | 7 (7.8) | 7 (10.9) | 0.45 | 0.5 |
| Refugee or asylum seeker status, n (%) | 10 (11.1) | 9 (14.1) | 0.02 | 0.96 |
| Serious and enduring mental illness, n (%) | 32 (35.6) | 2 (3.1) | 22.87 | < 0.0001 |
| Emotional/neurotic disorder, n (%) | 43 (47.8) | 35 (54.7) | 0.71 | 0.4 |
| Eating disorder, n (%) | 1 (1.1) | 5 (7.8) | 4.49 | 0.03 |
| Conduct disorder, n (%) | 3 (3.3) | 3 (4.7) | 0.81 | 0.67 |
| Substance misuse, n (%) | 12 (13.3) | 2 (3.1) | 4.76 | 0.03 |
| Emerging personality disorder, n (%) | 4 (4.4) | 0 | 2.92 | 0.09 |
| Comorbidity (2 or more disorders), n (%) | 23 (25.6) | 6 (9.4) | 6.41 | 0.01 |
| Admitted to hospital while attending CAMHS, n (%) | 31 (34.4) | 3 (4.7) | 19.25 | < 0.0001 |
| Detained under Mental Health Act, n (%) | 15 (16.7) | 1 (1.6) | 9.16 | 0.002 |
| Risk of self-harm at transition, n (%) | 5 (5.6) | 6 (9.4) | 1.50 | 0.22 |
| On medication at time of transition, n (%) | 69 (76) | 29 (45) | 15.89 | < 0.0001 |
Predictors of transition
Table 2 shows the results of the logistic regression conducted twice, with the second analysis controlling for clustering within trusts. Having a severe and enduring mental illness and being on medication at the time of transition predicted transition in both analyses. The effect of clustering among trusts was evident in two predictor variables: having ‘known broader social risk’ and having been admitted for in-patient care.
Table 2 Results of logistic regression: factors predicting actual transition with clustered results accounting for trust-level data
| Independent variable | Odds ratio | 95% CI | P | 95% CI, clustered | P, clustered |
|---|---|---|---|---|---|
| Known broader social risk (score) | 1.38 | 0.9–2.1 | 0.14 | 1.1–1.8 | 0.02 |
| English as first language | 0.76 | 0.3–2.3 | 0.62 | 0.4–1.3 | 0.30 |
| Parents attend CAMHS | 0.56 | 0.2–1.3 | 0.19 | 0.2–1.3 | 0.16 |
| Admitted as psychiatric in-patient | 5.05 | 1.0–26.8 | 0.05 | 0.2–147.3 | 0.34 |
| Admitted under the Mental Health Act | 5.0 | 0.5–48.3 | 0.165 | 1.6–15.5 | 0.01 |
| Eating disorder | 0.24 | 0.0–2.4 | 0.22 | 0.0–3.4 | 0.29 |
| Substance misuse | 1.66 | 0.3–11.0 | 0.59 | 0.3–8.7 | 0.55 |
| Comorbidity | 2.82 | 0.9–9.4 | 0.09 | 0.8–9.6 | 0.01 |
| Serious and enduring illness | 7.85 | 1.6–37.8 | 0.01 | 1.5–40.9 | 0.01 |
| On medication at the time of transition | 2.36 | 1.1–5.3 | 0.04 | 1.7–3.4 | < 0.01 |
Optimal transitions
Based on our four criteria, only 4 of the 90 individuals in the actual referrals group experienced optimal transition. They were 2 males and 2 females, all from Black and minority ethnic backgrounds. Three had a serious and enduring mental disorder and had been admitted to hospital, two under the Mental Health Act. All four were on medication and were from London. Three were referred from an adolescent service.
We were unable to explore predictors of optimal transition given how few individuals had experienced it. We therefore determined predictors of one of the key criterion of optimal transition – continuity of care. This was defined as ‘still engaged with AMHS or appropriately discharged 3 months post-transition’. Logistic regression revealed that individuals with emotional/neurotic disorder were a third less likely to experience optimal continuity of care (odds ratio (OR) = 0.34, 95% CI 0.12–0.96, P = 0.04). There was no association of continuity of care with any clinical, demographic or process variables.
Qualitative study results
Of the planned 20 service user participants, we could only interview 11. The most common reason for failing to recruit was no response from the service users to our requests for participation (25%). The second most common reason was that a clinician felt that the service user was too ill to participate (18%). A total of 27 interviews were conducted with 11 service users, 6 parents, 3 CAMHS clinicians and 6 AMHS clinicians.
Emergent themes
Emergent themes are reviewed briefly below, with some illustrative quotes set out in the online supplement to this paper.
Preparation for transition. Participants described three preparatory mechanisms for transition: transfer planning meetings, joint working and good information transfer. About half (54%) of young people interviewed reported attending at least one transition planning meeting, usually in the weeks preceding transition, with care coordinators from both CAMHS and AMHS and at least one parent. Service users and carers who did not have transition planning meetings thought that these would have been helpful. Both CAMHS and AMHS clinicians attributed lack of time as a barrier to such meetings. Two service users were told only at their last CAMHS appointment that they were going to be moved to AMHS.
Joint working. Child and adolescent mental health services were generally seen by AMHS colleagues as being in favour of joint working. The AMHS care coordinators appreciated the benefits of joint working (getting to know the service user, being ‘in the best interest of the client’) but expressed concern about ‘responsibility for someone on your case-load, should something go wrong’.
Parental involvement. Parents tended to be less involved with AMHS than with CAMHS. Although young people preferred not having their parents involved in their care any more, parents wanted to be more involved with adult services, in order to be able to express concerns or because they felt ‘left in the dark’. One parent stated: ‘I know he is now 18 but he is still my son and I worry about him’.
Outcomes of transition. Eight of the eleven young people were still engaged with AMHS at the time of the interview. In most cases (n = 7), young people felt that their mental health had improved since the transition to AMHS but did not necessarily attribute this improvement to transition to adult services. Care coordinator flexibility and persistence in the face of missed appointments helped with engagement, although this was more likely to happen when there was evidence of deteriorating mental health or emerging crises. Of the three young people no longer engaged with AMHS, one was discharged as his symptoms had resolved, one did not want to be seen and one was discharged because of non-attendance.
Other transitions. A number of young people experienced other transitions such as change of accommodation or educational status, becoming pregnant or becoming involved with other agencies. Only two young people were still living with their parents after transition. One young person was living with her partner and their child and another was homeless and living in his car. Of the five young women interviewed, three had unplanned pregnancies during the transition period. Four young people had physical health problems closely linked to their mental health and of these, two experienced parallel health service transitions from paediatric to adult care. Five young people had involvement with other services, including Social Services, health visitors, a homeless persons unit, the probation service, school/education support services, counselling services and an autism support service.
Discussion
It is a paradox that although treatment for mental disorders in young people have improved substantially in the past two decades, health system responses to young people with mental disorders have been inadequate. Reference Patel, Flisher, Hetrick and McGorry21 Despite adolescence being a risk period for the emergence of serious mental disorders, substance misuse, other risk-taking behaviours and poor engagement with health services, mental health provision is often patchy during this period. Reference Patel, Flisher, Hetrick and McGorry21,Reference McGorry22 By following a paediatric–adult split, mental health services introduce discontinuities in care provision where the system should be most robust.
To the best of our knowledge, TRACK is the first study in the international literature of the transition process, outcome and experience in a systematically identified cohort of young people who cross the boundary from CAMHS to AMHS. Our biggest methodological challenge was case ascertainment and we were hampered by the poor quality of CAMHS databases. Recall bias among clinicians is likely and our transition rates are certainly underestimates. Additionally, case notes may not accurately reflect the quality and content of services delivered. However, our qualitative results appear to complement the quantitative findings of inadequate transitional care. The requirement of the ethics committee that we seek service user consent through care coordinators meant that we could not interview individuals from the non-referred population (potential referrals) who were invariably out of contact with services. Our catchment was large and diverse, making our findings generalisable to other services in the UK. Internationally, there has been concern about adolescent mental health services in general Reference Patel, Flisher, Hetrick and McGorry21,Reference McGorry22 and about transition in particular. Reference Singh3,Reference Cosgrave, Yung, Killackey, Buckby, Godfrey and Standford23,Reference Davis, Geller and Hunt24 Our findings are likely to reflect similar problems internationally.
The findings from TRACK can be summarised as follows: although most service users who crossed the CAMHS transition boundary needed transfer to AMHS, a significant proportion (a third in this study) were not referred to AMHS. Those with neurodevelopmental disorders, emotional/neurotic disorders or emerging personality disorder were most likely to fall through the CAMHS–AMHS gap. Those with a severe and enduring mental illness, a hospital admission and on medication were more likely to make a transition to AMHS but many (a fifth of all actual referrals in this study) were discharged from AMHS care without being seen. Having social risks also predicted transition of care when clustering at trust level was taken into account. This might reflect a greater likelihood of the London sample experiencing such risks. Less than 4% of those accepted by AMHS experienced optimal transition. Although we cannot conclude that optimal transition equates with good clinical outcomes, it certainly equates with good patient experience, a key marker of service quality. In the TRACK cohort, basic principles of good practice identified in transition protocols Reference Singh, Paul, Ford, Kramer and Weaver18 were not implemented. For the majority of service users, transition from CAMHS to AMHS was therefore poorly planned, poorly executed and poorly experienced. Transition processes appeared to accentuate all the pre-existing barriers between CAMHS and AMHS. Reference Singh3,Reference Singh, Evans, Sireling and Stuart25
Aligning referral thresholds
We cannot say why young people with emotional/neurotic, neurodevelopmental or emerging personality disorders are not being referred to AMHS. It is possible that CAMHS may be adjusting their referral thresholds on knowledge and prior experience of local AMHS. If so, this obscures inadequacies in current provision. Where services exist, all young people with ongoing needs should be referred. Where services do not exist, notably those for young people with neurodevelopmental disorders, unmet service user needs should be systematically documented and made clear to AMHS providers and commissioners. Currently, neither CAMHS nor AMHS appear to accept responsibility for the health and welfare of this group. Their outcomes are not known and should be a serious cause for concern.
Transition boundary
Transition policies in the trusts recommend flexibility regarding transition boundaries based on service user need. Reference Singh, Paul, Ford, Kramer and Weaver18 Our study found little evidence of such flexibility. Perhaps services should use ‘age windows’ to decide the optimal time for transition rather than a strict age cut-off. A crisis should be a relative contra-indication to transition; transitions should only be planned and proceed at times of relative stability. There may be situations where transition can only occur during or immediately following a crisis, or where the transition process itself precipitates a crisis, but these occurrences should be relatively rare.
Transition preparation
Since most transitions can be long anticipated, there should be an adequate period of planning and preparing the service user and their carer for transition. Information about adult services, what to expect, differences in service provision, issues of confidentiality and parental involvement should all form a package of information that CAMHS share with service users and carers prior to transition. The completion of a ‘transition logbook’ would be a cheap and simple intervention to help structure the transition process. It would be jointly completed by the service user and their care coordinator and contain relevant details such as contact names and numbers, the dates and number of appointments with each agency, the final transition date and service user views on the experience. Such a tool can be easily evaluated on its impact on the process, outcomes and service user experience.
Improving information transfer
We found that current information technology systems, particularly in CAMHS, did not allow clinicians and managers to access high-quality information on case-loads. Information transfer was also hampered by a lack of understanding of each other's services, inconsistent documentation, different systems used for transfer of electronic information and transfer of referrals to lengthy waiting lists during which professional dialogue was reduced. Inadequate information technology systems in mental health services clearly hinder informational continuity. Reference Burns, Clement, Cathy, McLaren, Rees-Jones and Wykes26 The recent National CAMHS Review 27 notes the frustrations that arise as a result of separate, incompatible information technology systems across different agencies and the need for systems reform and resource support. We recommend that protocols for transition should explicitly specify information that should be transferred between agencies. Where possible, case notes should follow the young person and detailed referral letters, including risk assessments, should be sent to AMHS to facilitate planning. Introduction of electronic records offers an opportunity to facilitate standardisation across services and trusts.
Managing multiple transitions
Many young people had multiple transitions between AMHS teams, among care coordinators and in their personal circumstances, the cumulative effect of which was complex and unsettling for service users. From our data we cannot tell whether services were unaware of these multiple transitions or unequipped to deal with them. Mental health services, however, must pay attention to these multiple transitions through multi-agency involvement, in order to address the complex needs of this vulnerable group. Reference Lamb, Hill, Kelvin and Van Beinum2,7,28
Improving liaison between CAMHS and AMHS
Maitra & Jolley Reference Maitra, Jolley, Reder, McClure and Jolley29 have described a model where child and adult psychiatrists regularly attend each other's clinical meetings at which they jointly address the mental health needs of parents and children within families. Another approach is the development of designated transition workers with posts split between AMHS and CAMHS. Reference Forbes, While, Ullman, Lewis, Mathes and Griffiths4,30,31 Such innovations have several benefits, including a higher profile for children and young people within adult services, shaping of the process of referrals across services, improved scope for preventive work, possibilities of joint working and the availability of a forum for formal and informal discussions.
These strategies require closer collaboration between services and agencies, which is demanding of both time and personnel. In periods of fiscal austerity, it is difficult to make a case for enhancing existing services, creating new transition worker posts or developing specialist clinics such as for adults with attention-deficit hyperactivity disorder. The CAMHS–AMHS divide is also mirrored in the differing commissioning arrangements in the UK, where CAMHS are often commissioned by acute care or children's services, whereas AMHS is firmly within mental health commissioning. Research evidence such as TRACK therefore is the best way for academics and clinicians to influence policy and shape service provision. We believe that joint commissioning between mental health services for children and adults and shared commissioning approaches at a regional level are the best ways to improve transitional care. The Appendix outlines the overall recommendations of the TRACK project. Further recommendations can be found in the full report.
Bridging the divide
There are two contrasting approaches for improving care for young people undergoing transition from CAMHS to AMHS. We can improve the interface between services as these currently exist, or we can develop a completely new and innovative service model of integrated youth mental health services. Each has its advantages, limitations and resource implications. Common to both approaches is the need for services to pay attention to the developmental needs of this age group in areas beyond healthcare transition such as changes in educational and vocational domains, independent living and social and legal status. Although we call for further research into ways of improving transitional care, TRACK findings by themselves demand early and substantial service improvement, some of which can occur without new resources and by simply improving liaison, planning and joint working between CAMHS and AMHS.
In their review of youth mental heath services across the world, Patel et al Reference Patel, Flisher, Hetrick and McGorry21 concluded: ‘our single most important recommendation is the need to integrate youth mental health programmes, including those in the health sector (such as reproductive and sexual health) and outside this sector (such as education)’. The findings of TRACK highlight how far away we are from such integration, given the problems of transition revealed at the interface of CAMHS and AMHS. Even though we do not as yet know how to achieve best transitional care, the status quo of existing service barriers should not be acceptable. We certainly need evidence for any models of transitional care that we test in the future. The search for that evidence should be a goal, rather than a prerequisite for service change. We need to ensure that the vital need for improving youth mental health is not ignored for fear of dismantling long-standing and yet unhelpful service barriers.
Appendix
Overall recommendations from the TRACK study
-
(a) The needs of the service user should be central to protocol and service development regarding transition.
-
(b) Trusts should have regular updated mapping of local CAMHS, AMHS and voluntary services, identifying scope of operation, communication networks and key contacts.
-
(c) Protocols should be developed and implemented in collaboration with all relevant agencies and young people and their carers.
-
(d) Multidisciplinary training should be planned and delivered for transition, including local service structures, protocols and working with young people. This training should be linked to the appraisal process and skills and competency frameworks.
-
(e) Protocols should specify the time frame, lines of responsibility and who should be involved, how the young person should be prepared and what should happen if AMHS are unable to accept the referral.
-
(f) Protocols should stress flexibility in the age range to accommodate a range of needs and developmental stages, and have explicit referral criteria and service provision.
-
(g) Transition should occur at times of stability where possible; young people should not have to relapse in order to access a service.
-
(h) Agencies should try to avoid multiple simultaneous transitions.
-
(i) Improved information transfer between CAMHS/AMHS with the standardisation of record keeping or, where this is impossible, clear indication of what information should be made available. A referral letter summarising past contact, current state and risks is a bare minimum. If all records cannot be transferred, copies of all correspondence and contact summaries should be.
-
(j) Transition process should include collaborative working between CAMHS and AMHS, with cross-agency working or periods of parallel care.
-
(k) Carers' needs and wishes should be respected in the transition process and carer involvement in adult services should be sensitively negotiated between clinicians, service users and their carers.
-
(l) Services need to develop for young people with emotional/neurotic, emerging personality and neurodevelopmental disorders wherever there is gap in such provision.
-
(m) Active involvement by AMHS is required before CAMHS can discharge a case; transfer onto a long waiting list is unacceptable.
-
(n) Changes should be evidence based. Prospective research is required on the clinical course, service needs, health and social cost implications for the young people receiving little service provision after leaving CAMHS.
Acknowledgements
The TRACK study team included Professor Swaran Singh, Dr Ruth Belling, Dr Jenny Dale, Dr Navina Evans, Dr Tamsin Ford, Dr Nicole Fung, Ms Katherine Harley, Dr Daniel Hayes, Ms Kimberly Hovish, Dr Zoebia Islam, Dr Bob Jezzard, Dr Tami Kramer, Professor Susan McLaren, Dr Moli Paul, Dr Anne Rourke, Dr Tim Weaver and Dr Sarah White.






eLetters
No eLetters have been published for this article.