High comorbidity among psychiatric disorders is consistently reported (Reference Kessler, McGonagle and ZhaoKessler et al, 1994; Reference Merikangas, Angst and EatonMerikangas et al, 1996). Among many proposed explanations, one possibility is that personality mediates part of this comorbidity (Reference Jardine, Martin and HendersonJardine et al, 1984; Reference Clark, Watson and MinekaClark et al, 1994; Reference Battaglia, Przybeck and BellodiBattaglia et al, 1996; Reference Bienvenu, Brown and SamuelsBienvenu et al, 2001; Reference Krueger and MarkonKrueger & Markon, 2001). This study examines the association of variation in personality traits of neuroticism, extraversion and novelty seeking and the comorbidity among eight disorders: major depression, generalised anxiety disorder (GAD), panic disorder, any phobia, alcohol dependence, drug dependence, antisocial personality disorder and conduct disorder. This study not only attempts to replicate previous work using a large epidemiological sample, including more comprehensive diagnostic categories and different statistical methodology, but also attempts to quantify the proportion of comorbidity among psychiatric disorders explained by individual personality dimensions.
METHOD
Participants
Our sample derives from two related projects utilising the population-based Virginia Twin Registry, which was formed from a systematic review of all birth certificates in the Commonwealth of Virginia and now constitutes part of the Mid-Atlantic Twin Registry. The female-female (FF) twin pairs used in this study come from birth years 1934-1974. Twin pairs became eligible to participate if both members had responded previously to a mailed questionnaire, the response rate to which was 64%. Eighty-eight per cent of our sample were first interviewed face to face in 1987-1989 (wave 1) and subsequently have participated in up to three additional telephone interviews (waves 2-4).
The male-male and male-female (MM/MF) twin pairs, covering the birth years 1940-1974, were ascertained in a separate study beginning in 1993. We interviewed 72% of the eligible sample, usually by telephone, in our wave 1 study. This sample was followed up in a second wave of face-to-face interviews (1994-1998) that were completed with 79.4% of eligible participants.
We examine here the results of combined data from the MM/MF and FF samples, based on the second and fourth wave of interviews, respectively, because these were the most recent waves in which we had measured both personality and psychiatric diagnoses. Our sample consisted of 7588 individual twins, with 4240 males (55.9%) and 3348 females (44.1%). All participants were Caucasian, ranging in age from 20 to 58 years (mean=36.8, s.d.=8.9) at the time of the interview. Informed consent was obtained from all participants prior to assessment.
Measures
Psychiatric disorders
The outcome measures of interest, as outlined in the introduction, were lifetime diagnoses of common psychiatric disorders. In order to facilitate the discussion, we will use the concepts of internalising (propensity to express distress inwards, including major depression, GAD, panic disorder, any phobia) and externalising (propensity to express distress outwards, including alcohol and drug dependence, antisocial personality disorder, conduct disorder) disorders as described by Krueger et al (Reference KruegerKrueger, 1999; Reference Krueger and MarkonKrueger & Markon, 2001). With the exception of ‘any phobia’, all disorders were assessed using the Structured Clinical Interview for DSM-III-R (Reference Spitzer and WilliamsSpitzer & Williams, 1985). Diagnostic algorithms for GAD, panic disorder and alcohol dependence were modified to reflect DSM-IV criteria (American Psychiatric Association, 1994), whereas major depression, drug dependence, antisocial personality disorder and conduct disorder were based on DSM-III-R criteria (American Psychiatric Association, 1987) owing to the lack of items corresponding to DSM-IV criteria. The drug dependence diagnosis included dependence on marijuana, cocaine, opiates, hallucinogens, stimulants, sedatives or other drugs. Phobias were assessed with an adaptation of the phobic disorders section of the Diagnostic Interview Schedule, version III-A (Reference Robins and HelzerRobins & Helzer, 1985), and the diagnosis of ‘any phobia’ included agoraphobia, social, situational, animal, blood and miscellaneous phobias. The diagnostic algorithm for phobias has been described in detail previously (Reference Kendler, Myers and PrescottKendler et al, 2002).
Interviewers were carefully trained and supervised, and had at least a master's degree in a mental health-related field or a bachelor's degree in such a field and two years of clinical experience. Diagnoses for conduct disorder and antisocial personality disorder were based on self-report questionnaires; all other diagnoses were assessed using personal interview. Inter-rater reliability for diagnosis (based on a subsample of FF twins) was high (e.g. for major depression, mean (s.d.), κ=0.96 (0.04)), and test-retest reliability (based on an average interval of 4.5 weeks, range 2-8 weeks, between base and reliability interview) was also acceptable for most diagnoses (range=0.23-0.74, average κ=0.52). Finally, the comorbidity of antisocial personality disorder and conduct disorder was not examined because the diagnosis of antisocial personality disorder requires the onset of conduct disorder before age 15 years. Table 1 describes the prevalence of psychiatric disorders in our sample.
Table 1 Prevalence of psychiatric disorders by gender
| Disorder | Males (n/sample N)1 | Females (n/sample N)1 |
|---|---|---|
| Major depression | 29.5% | 41.0% |
| (1252/4240) | (1374/3348) | |
| Generalised anxiety disorder | 1.7% | 2.8% |
| (71/4226) | (95/3340) | |
| Panic disorder | 1.1% | 3.2% |
| (48/4214) | (108/3393) | |
| Any phobia | 22.0% | 31.7% |
| (929/4215) | (1055/3329) | |
| Alcohol dependence | 25.9% | 9.8% |
| (1092/4213) | (326/3332) | |
| Any drug dependence | 7.3% | 4.3% |
| (309/4240) | (144/3325) | |
| Antisocial personality disorder | 3.9% | 0.4% |
| (154/3947) | (12/2776) | |
| Conduct disorder | 10.1% | 1.7% |
| (402/3962) | (48/2781) |
Personality
Neuroticism and extraversion, as conceptualised by Eysenck (Reference Eysenck and EysenckEysenck & Eysenck, 1975; Reference Hirschfeld, Klerman and ClaytonHirschfeld et al, 1983), have been identified cross-culturally as major personality traits by nearly all subsequent investigators (Reference PervinPervin, 1990). Neuroticism reflects emotional instability, vulnerability to stress and anxiety proneness, whereas extraversion measures sociability and liveliness. Novelty seeking, another personality dimension, measures exploratory excitability, impulsiveness, extravagance and regimentation (Reference Cloninger, Przybeck and SvrakicCloninger et al, 1991). Personality measures of neuroticism and extraversion were obtained by self-report questionnaire in the MM/MF sample and were part of the telephone interview in the FF sample. Novelty seeking was assessed by self-report questionnaire only, in both samples. Neuroticism and extraversion were assessed with 12 and 8 items, respectively, from the shortened version of the Eysenck Personality Questionnaire - Revised (EPQ-R; Reference Eyesenck, Eysenck and BarrettEysenck et al, 1985; Reference Heath, Neale and KesslerHeath et al, 1992). Novelty seeking was evaluated by 18 items from the abbreviated 54-item version of the Tridimensional Personality Questionnaire (TPQ) of Cloninger (Reference Cloninger, Przybeck and SvrakicCloninger et al, 1991; Reference Heath, Cloninger and MartinHeath et al, 1994). For statistical analyses we used composite personality measures derived from individual items for each dimension, respectively.
Missing data
Valid data on all three personality measures and all eight psychiatric disorders were available for the vast majority (85.6%; n=6499) of the sample. Missing data for major depression, GAD, any phobia and alcohol and drug dependence were minimal (<0.6%). Rates of missing data for conduct disorder and antisocial personality disorder were somewhat higher (approximately 7-16%) because these diagnoses were assessed using a separate self-report questionnaire. Rates of missing data for the three personality measures were 2-16%, also due primarily to lower response rates for the self-report questionnaire. Preliminary analyses revealed no significant differences in mean levels of personality or psychiatric diagnosis due to missing data on other variables (results available from the authors upon request).
Statistical analysis
We performed logistic regression analyses to estimate the association of each personality dimension with each psychiatric disorder. Correction for the correlated structure of our twin data was done using generalised estimating equations (Reference Liang and ZegerLiang & Zeger, 1986) as implemented in the Statistical Analysis System (SAS) procedure GEN-MOD. Multiple logistic regression analyses were performed with all three personality measures as independent variables. Age, zygosity and gender were used as covariates. Scores for all personality measures were standardised to a mean of 0 and a variance of 1 to facilitate the direct comparison of their effects on the disorder of interest. Odds ratios with 95% confidence intervals and their statistical significance are reported. An odds ratio of >1 represents the increase in risk of disorder associated with each standard deviation (s.d.) increase in the score of the personality dimension. An odds ratio of <1 represents the decrease in risk associated with each s.d. increase in personality dimension score.
In order to calculate the proportion of comorbidity attributed to variation in normal personality, we conducted structural equation modelling analyses using the software program Mx (Reference Neale, Boker and XieNeale et al, 1999). As depicted in Fig. 1, the model we used allowed us to calculate the total covariance (i.e. comorbidity) between the disorders of interest. This covariance was broken down into the covariance attributed to personality and the residual covariance, which represents any remaining comorbidity after removing the covariation attributable to personality. Covariance due to personality comprised both direct and indirect effects. Direct effects are the direct effects of each personality measure on each of the two disorders. In path analyses, the contribution of personality to comorbidity can be assessed by multiplying the direct effects of a given personality variable on each of the two disorders. Indirect effects are effects of personality on disorder and comorbidity that occur through correlated personality dimensions. Because the overall correlation across personality measures was low to moderate (between neuroticism and extraversion=-0.19, neuroticism and novelty seeking=0.04, extraversion and novelty seeking=0.34) indirect effects of personality are ignored when calculating the contribution to covariance of each individual personality dimension (although they are included as a separate category; see Table 3 below).
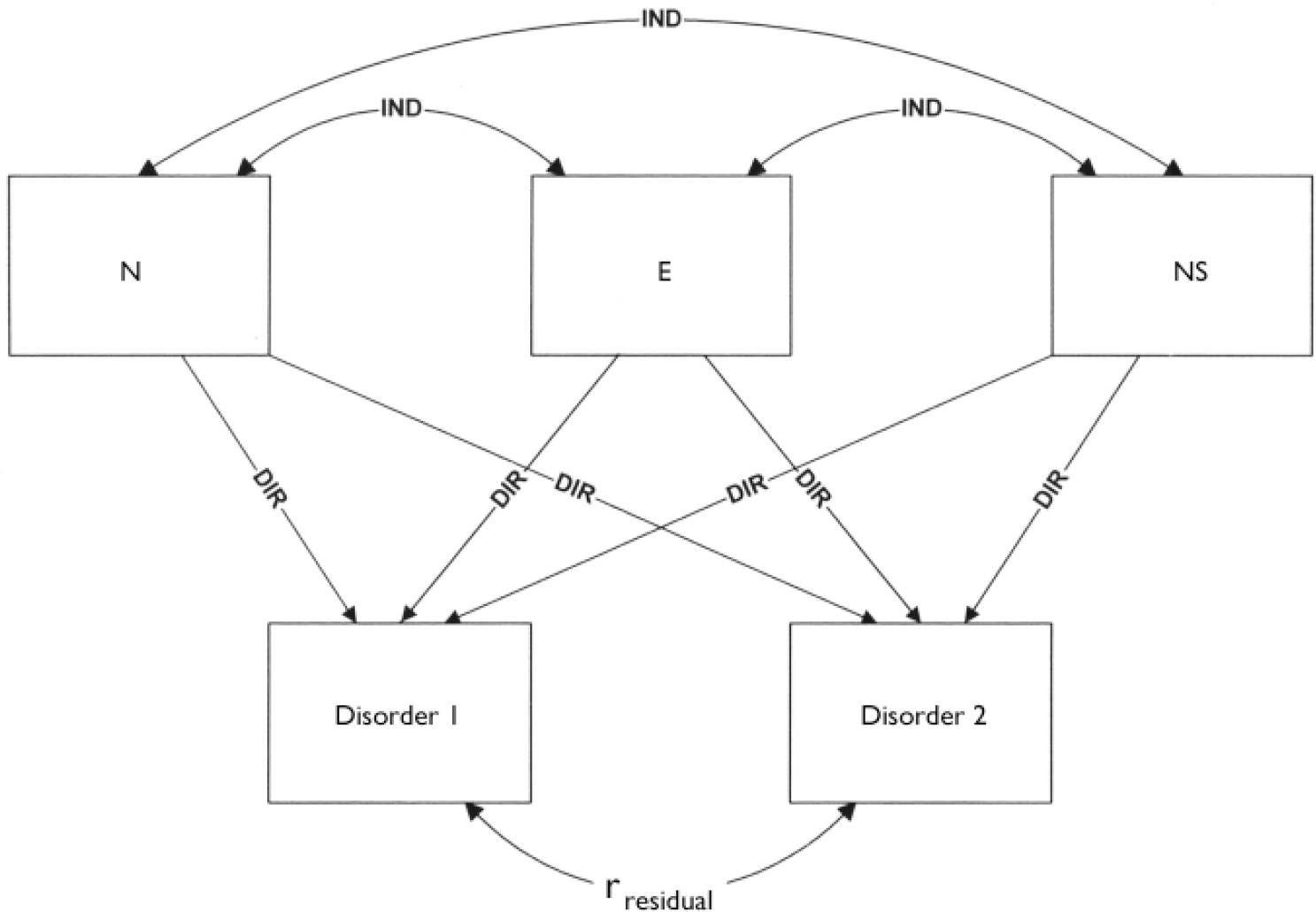
Fig. 1 Structural equation model to calculate the total and partial covariance between the personality measures of neuroticism (N), extraversion (E) and novelty seeking (NS) and the disorders of interest (e.g. major depression (disorder 1) and panic disorder (disorder 2)).
Table 2 Association of personality measures and common psychiatric disorders
| Personality dimension | Major depression | Generalised anxiety disorder | Panic disorder | Any phobia | Alcohol dependence | Any drug dependence | Antisocial personality disorder | Conduct disorder |
|---|---|---|---|---|---|---|---|---|
| Neuroticism | 1.95*** | 2.30*** | 1.93*** | 1.62*** | 1.57*** | 1.64*** | 1.44*** | 1.26*** |
| (1.85–2.06) | (2.01–2.63) | (1.61–2.31) | (1.54–1.71) | (1.47–1.67) | (1.50–1.79) | (1.26–1.65) | (1.15–1.38) | |
| Extraversion | 1.07* | 1.21* | 0.95 | 0.98 | 1.18*** | 1.24** | 0.92 | 0.93 |
| (1.01–1.13) | (1.01–1.45) | (0.77–1.18) | (0.92–1.04) | (1.09–1.26) | (1.08–1.41) | (0.77–1.09) | (0.83–1.04) | |
| Novelty seeking | 1.14*** | 0.92 | 1.10 | 1.08** | 1.37*** | 1.58*** | 1.83*** | 1.39*** |
| (1.09–1.22) | (0.76–1.10) | (0.88–1.36) | (1.03–1.16) | (1.28–1.46) | (1.42–1.76) | (1.57–2.13) | (1.26–1.54) |
The structural equation models were fitted to the raw data using maximum likelihood estimation, which allowed us to use all valid data, even if some responses or observations for a given individual are missing. Psychiatric disorders were coded as binary (1=present, 0=absent); thus, data were treated as ordinal, and thresholds for each disorder were estimated using z scores that corresponded to the prevalence of the given diagnosis. These thresholds were allowed to vary by gender to accommodate gender differences in the rates of psychiatric disorders. To test for significant gender differences, we constrained the thresholds to be equal for men and women and evaluated the overall fit of the model (using Akaike's information criteria, AIC) compared with the model where thresholds were allowed to vary by gender. Models with the lowest AIC values were considered to be the best-fitting models. We also tested for gender differences in the overall pattern of covariance by constraining the parameter estimates to be the same in males and females, and comparing the pattern of covariance with a model where parameters were allowed to vary by gender. Because Mx currently lacks the capability to analyse continuous and ordinal traits simultaneously, the continuously measured personality traits were divided into categories based on the maximum number of responses possible, and thresholds corresponding to the proportions of individuals in each category were estimated. For example, scores on the neuroticism variable were in the range 0-12. Thus, we used 12 thresholds to estimate the proportion of individuals within each response category.
RESULTS
Logistic regression for the effects of personality on psychiatric disorders
Table 2 shows the odds ratios from the logistic regression analyses for each of the three personality measures. Higher scores on neuroticism significantly increased the risk for all the disorders examined. For each s.d. increase in neuroticism, the highest (130%) risk increase was for GAD and the lowest (26%) for conduct disorder. Extraversion's impact was modest overall, with no consistent pattern across internalising and externalising disorders. Specifically, one s.d. increase in extraversion was associated with a 24% increased risk for drug dependence, with a smaller increase for GAD, alcohol dependence and major depression. Novelty seeking was most strongly associated with externalising disorders (alcohol and drug dependence, antisocial personality disorder, conduct disorder), with increase in risk ranging from 37% to 83%. Inspection of covariates revealed that internalising disorders (major depression, GAD, panic disorder and any phobia) were more prevalent in females whereas externalising disorders (alcohol and drug dependence, antisocial personality disorder, conduct disorder) were more prevalent in males (Table 1). Age was positively associated with internalising disorders (i.e. older subjects reported a higher prevalence of major depression, GAD, panic disorder and any phobia) and was negatively associated with the externalising disorders (i.e. younger subjects had higher rates of alcohol and drug dependence, antisocial personality disorder and conduct disorder). Zygosity was not associated with any of the psychiatric disorders.
We also tested for interactions between gender and each of our three personality measures for each of the disorders. Out of 24 possible interactions (8 disorders×3 interactions), only the interaction between gender and neuroticism for alcohol dependence was significant (β=0.06, s.e.=0.02, Wald χ2=5.22, P<0.05). In this case, the relationship between neuroticism and alcohol dependence was stronger for females than for males. However, it should be noted that this significant interaction may be a stochastic effect. Thus, for the structural equation modelling analyses of personality and comorbidity, males and females were combined into a single sample, although thresholds corresponding to psychiatric disorder were estimated separately for males and females.
Structural equation modelling of personality effects on comorbidity
For ease of interpretation, the results of the structural equation modelling analyses are depicted graphically in Fig. 2. The height of the bar represents the total phenotypic comorbidity of any two given disorders, and the differently shaded segments depict the direct covariance accounted for by each individual personality dimension, as well as any indirect effects, and the residual covariance. For example, the comorbidity (phenotypic correlation) between major depression and GAD is 0.41. Neuroticism accounts for the 0.16 of this comorbidity whereas the remaining comorbidity (0.25) was residual covariance. Extraversion, novelty seeking and indirect effects accounted for negligible (and negative) covariance. In order to facilitate the description, results from these analyses have been presented also as percentages of the total comorbidity (Table 3). Thus, in the case of comorbidity between major depression and GAD, Table 3 shows that 0.41 is total comorbidity. Neuroticism accounts for 39% of this comorbidity, with the remaining comorbidity due primarily to residual covariance (61%).

Fig. 2 Covariance between personality measures and comorbid psychiatric disorders. Bars represent total comorbidity and different segments provide a visual representation of the covariance of different personality measures, as well as residual covariance and indirect covariance. AD, alcohol dependence; AP, any phobia; APD, antisocial personality disorder; CD, conduct disorder; DD, drug dependence; GAD, generalised anxiety disorder; MD, major depression; PAN, panic disorder.
Table 3 Covariance between personality measures and comorbid psychiatric disorders, represented as percentage of total covariance (r tot)
| Variable | Major depression | Generalised anxiety disorder | Panic disorder | Any phobia | Alcohol dependence | Drug dependence | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r tot | N(%) | E(%) | NS(%) | r res(%) | IND(%) | r tot | N(%) | E(%) | NS(%) | r res(%) | IND(%) | r tot | N(%) | E(%) | NS(%) | r res(%) | IND(%) | r tot | N(%) | E(%) | NS(%) | r res(%) | IND(%) | r tot | N(%) | E(%) | NS(%) | r res(%) | IND(%) | r tot | N(%) | E(%) | NS(%) | r res(%) | IND(%) | |
| Generalised | 0.41 | 39.0 | 0.9 | -0.8 | 63.1 | -2.2 | ||||||||||||||||||||||||||||||
| anxiety | ||||||||||||||||||||||||||||||||||||
| disorder | ||||||||||||||||||||||||||||||||||||
| Panic disorder | 0.49 | 20.9 | 0 | 0.1 | 79.1 | 0 | 0.49 | 21.9 | -0.2 | -0.2 | 79.5 | -1.0 | ||||||||||||||||||||||||
| Any phobia | 0.30 | 39.1 | -0.1 | 0.7 | 60.2 | 0.1 | 0.28 | 44.9 | -0.5 | -1.0 | 58.0 | -1.4 | 0.42 | 20.0 | 0 | 0.1 | 79.6 | 0.3 | ||||||||||||||||||
| Alcohol | 0.34 | 30.6 | 0.8 | 2.8 | 65.9 | 0 | 0.13 | 88.1 | 7.4 | -7.5 | 16.2 | -4.2 | 0.27 | 27.8 | -0.4 | 0.7 | 72.6 | 0.7 | 0.25 | 33.5 | -0.4 | 3.2 | 64.1 | 0 | ||||||||||||
| dependence | ||||||||||||||||||||||||||||||||||||
| Any drug | 0.40 | 26.0 | 0.8 | 3.0 | 70.2 | 0 | 0.18 | 61.2 | 4.9 | -6.6 | 41.7 | -1.2 | 0.21 | 35.0 | -0.5 | 1.3 | 65.0 | -0.8 | 0.24 | 35.0 | -0.5 | 4.2 | 61.6 | 0 | 0.59 | 12.2 | 1.1 | 7.4 | 78.0 | 1.3 | ||||||
| dependence | ||||||||||||||||||||||||||||||||||||
| Antisocial | 0.29 | 23.9 | -0.3 | 5.8 | 67.4 | 3.2 | 0.19 | 39.5 | -1.4 | -10.0 | 62.2 | 7.7 | 0.19 | 25.5 | 0.1 | 1.3 | 71.0 | 2.1 | 0.19 | 28.9 | 0.1 | 7.1 | 61.6 | 2.3 | 0.46 | 11.4 | -0.5 | 12.1 | 74.8 | 2.2 | 0.52 | 10.0 | -0.4 | 14.0 | 74.5 | 6.0 |
| personality | ||||||||||||||||||||||||||||||||||||
| disorder | ||||||||||||||||||||||||||||||||||||
| Conduct | 0.19 | 26.3 | -0.6 | 5.4 | 65.4 | 3.5 | 0.09 | 56.9 | -4.9 | -13.2 | 48.6 | 12.6 | 0.18 | 19.5 | 0.2 | 1.2 | 77.1 | 2.0 | 0.13 | 30.4 | 0.3 | 6.5 | 59.9 | 2.9 | 0.29 | 12.5 | -1.0 | 12.5 | 74.0 | 2.0 | 0.34 | 10.7 | -0.9 | 13.6 | 74.9 | 1.7 |
| disorder | ||||||||||||||||||||||||||||||||||||
The overall pattern of results, as shown in Fig. 2 and Table 3, indicates that neuroticism accounts for the highest proportion of comorbidity within internalising disorders (20-45%, arithmetic average=31%) and between internalising and externalising disorders (19-88%, arithmetic average=36.8%). Neuroticism also explained 10-12% of the comorbidity within externalising disorders. Extraversion explained only a very small proportion of the comorbidity (-4.9 to 7.4%). Novelty seeking accounted for a negligible proportion of comorbidity within internalising disorders (-0.8 to 0.7%) and between internalising and externalising disorders (-13.2% to 5.8%); however, novelty seeking did account for 7.4-14% of the comorbidity within externalising disorders. Residual covariance (i.e. due to factors other than personality) accounted for most of the comorbidity, with an arithmetic average of 65%. Negative values in Fig. 2 and Table 3 reflect the effects of low extraversion (introversion) and low novelty seeking on comorbidity, although the majority of these effects are quite small.
Although the models where thresholds for psychiatric disorders were allowed to vary by gender consistently fit the data better than models assuming equal thresholds, there were no significant gender differences in the covariance structure (results available from the authors upon request). Thus, the pattern of comorbidity accounted for by personality was similar in males and females, despite the significant differences in the rates of psychiatric disorders.
DISCUSSION
Neuroticism
Our results suggest that normal personality dimensions of neuroticism not only contributed to individual diagnoses but also accounted for a significant part of the lifetime comorbidity of common psychiatric disorders. The most striking finding was that neuroticism, on average, accounted for 26% of the comorbidity among the disorders included in the study (range=12-88%). This finding is consistent with previous research (Reference Clark, Watson and MinekaClark et al, 1994; Reference Sher and TrullSher & Trull, 1994, Reference Krueger and MarkonKrueger & Markon, 2001; Reference Bienvenu, Brown and SamuelsBienvenu et al, 2001) and suggests neuroticism as a potential general underlying vulnerability factor for psychopathology.
Extraversion
Although extraversion was significantly, albeit weakly, associated with four of the eight psychiatric disorders in the logistic regressions, it explained very small proportions of comorbidity. This pattern of weak effects of extraversion on psychiatric disorders and comorbidity is inconsistent with previous research (Reference Sher and TrullSher & Trull, 1994) and probably stems from the restrictive definition of our extraversion scale, which only reflects sociability. Eysenck revised the extraversion scale in the EPQ-R and items that measured impulsivity were largely moved to the psychoticism scale (Reference NyborgNyborg, 1997).
Novelty seeking
High novelty seeking increased the risk for externalising disorders significantly (Table 2) when these disorders were examined individually. Novelty seeking also accounted for the largest proportion of comorbidity between externalising disorders (7-14%, arithmetic average=11.9%). Not surprisingly, novelty seeking was unrelated to the comorbidity within internalising disorders and, for the most part, between internalising and externalising disorders. However, somewhat surprisingly, the contribution of neuroticism to the comorbidity within externalising disorders was comparable with the effects of novelty seeking.
These results further support the existence of broader, underlying dimensions of core psychopathological processes. Neuroticism appears to be a robust underlying dimension not only for the comorbidity within internalising disorders but also between internalising and externalising disorders and within externalising disorders. This leads us to reconsider the issue of psychiatric classification and an age-old question of splitting neurosis (Reference TyrerTyrer, 1985). Our previous research has indicated that the comorbidity between major depression and GAD and, to some extent, between major depression and alcohol dependence largely results from common genetic factors (Kendler et al, Reference Kendler, Neale and Kessler1992, Reference Kendler, Heath and Neale1993a ) with notable gender differences (Reference Prescott, Aggen and KendlerPrescott et al, 2000). In a previous report, we also found that over 50% of the genetic liability for major depression was shared with neuroticism (Reference Kendler, Neale and KesslerKendler et al, 1993b ). Thus, the possibility of common genetic liability between personality and comorbid disorders appears to be a reasonable hypothesis and will be the subject of future investigation.
Limitations
The results of this study should be interpreted in the context of four potential methodological limitations.
First, we used scales of neuroticism and extraversion from the EPQ-R and novelty seeking from the TPQ. Although neuroticism and extraversion represent widely accepted higher dimensions of personality, there is no agreement about the lower-order dimensions among different personality researchers. Moreover, some would argue that these two scales provide an incomplete description of the structure of heritable personality differences (Reference Heath, Cloninger and MartinHeath et al, 1994). How much more of the covariation among disorders would have been explained if we used the complete EPQ-R (neuroticism, extraversion, psychoticism and lie scale) or the complete TPQ (novelty seeking, harm avoidance and reward dependence) is speculative. Similarly, although interrater agreement for diagnosis was high, test-retest reliability for some of the lower-prevalence disorders (i.e. GAD, panic disorder and antisocial personality disorder) was low (0.23-0.42). This lower reliability may have increased the variance due to random errors of measurement, lowering the strength of associations of comorbidity with personality.
Second, the cross-sectional nature of the data made it difficult to establish causality and had a potential to confound state, trait and scar effects. However, the use of lifetime diagnosis provided some assurance that the confounding effects were likely to be minimal.
Third, because of some relatively young individuals in our sample, the risk period for certain psychiatric disorders was not over. As a result, true prevalence may be underestimated in the present sample, with concomitant effects on covariance.
Fourth, the sample was limited to Caucasian individuals so the results may not be generalisable to other ethnic groups.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Comorbidity among psychiatric disorders is a common and consistently reported finding.
-
▪ The normal personality dimension of neuroticism appears to be a broad vulnerability factor for the comorbid psychiatric disorders.
-
▪ Novelty seeking is modestly important for the comorbidity between externalising disorders only.
LIMITATIONS
-
▪ The normal personality dimensions used were from two different scales.
-
▪ The cross-sectional nature of the data used has a potential to confound state, trait and scar effects.
-
▪ The sample was limited to Caucasian individuals so the results might not be generalisable to other ethnic groups.
Acknowledgements
Supported by National Institutes of Health (NIH) grants T32/MH-20030, MH-40828, MH/AA/DA-49492, DA-11287 and AA-09095. The authors thank Dr Steve. Aggen for his help in statistical analysis. We also acknowledge the. contribution of the Virginia Twin Registry, now part of the Mid-Atlantic Twin. Registry (MATR), to the ascertainment of subjects for this study. The MATR, directed by Drs L. Corey and L. Eaves, has received support from the National. Institutes of Health, the Carman Trust and the W. M. Keck, John Templeton and. Robert Wood Johnson Foundations.








eLetters
No eLetters have been published for this article.