Improving outcomes for early-course psychosis (ECP) is a recognised global mental health priority. This effort faces four key challenges: (a) accounting for and addressing heterogeneity of clinical presentation; (b) a need for better modelling of illness trajectories; (c) access and availability of early intervention; and (d) a need for new pathways to enhance use of existing treatments. Although there is no panacea, any solution must be scalable and cost-effective to meet the global mental health need. We suggest that digital health technology-based solutions using smartphones – the swiss army knife of the 21st Century – offer a viable and scalable avenue for advancing ECP care.
Use of smartphone applications
Contrary to popular belief, individuals experiencing psychosis use smartphones as part of their daily lifeReference Gay, Torous, Joseph, Pandya and Duckworth1 and are keen to incorporate them into their treatment.Reference Lal, Dell'Elce, Tucci, Fuhrer, Tamblyn and Malla2 Importantly, individuals with ECP (i.e. those in the first few years of psychotic illness) are typically younger individuals raised in an increasingly digital world who are interested in technology-enabled services for medication monitoring, psychoeducation, clinical scheduling, information on recovery,Reference Lal, Dell'Elce, Tucci, Fuhrer, Tamblyn and Malla2 and psychosocial treatment.Reference Lal, Nguyen and Theriault3 Case reports of individuals using smartphone applications (‘apps’) to supplement cognitive–behavioural therapy for psychosisReference Sandoval, Torous and Keshavan4 and to track auditory hallucinations,Reference Torous and Roux5 coupled with data indicating up to 40% of individuals with schizophrenia use their smartphone or computers to play music to block auditory hallucinationsReference Gay, Torous, Joseph, Pandya and Duckworth1 underscore that individuals with ECP are not waiting for the clinical community to sanction the use of digital technology in care.
Although not all younger people have smartphones, national data in the USA suggests a mean of 94% smartphone ownership for those age 18–29 compared with 77% for the total population.6 Data on smartphone ownership and use for mental health in ECP remains scarce although small survey studies offer ownership estimates of 70% and higher.Reference Lal, Dell'Elce, Tucci, Fuhrer, Tamblyn and Malla7, Reference Waters and Fernyhough8 With this generation-wide access, interest and early adoption already occurring, the evidence suggests that today's individuals with ECP may be ready to use smartphone apps and sensors in their care.
Here, as outlined in Fig. 1, we discuss evidence to date indicating how smartphone and related digital health technologies can advance care for ECP by better accounting for clinical heterogeneity, offering better predictive models, increasing access to early interventions, and enhancing existing treatment options. Although not a comprehensive review, we underscore the potential of this growing space, acknowledge barriers to technology adoption and offer some solutions.
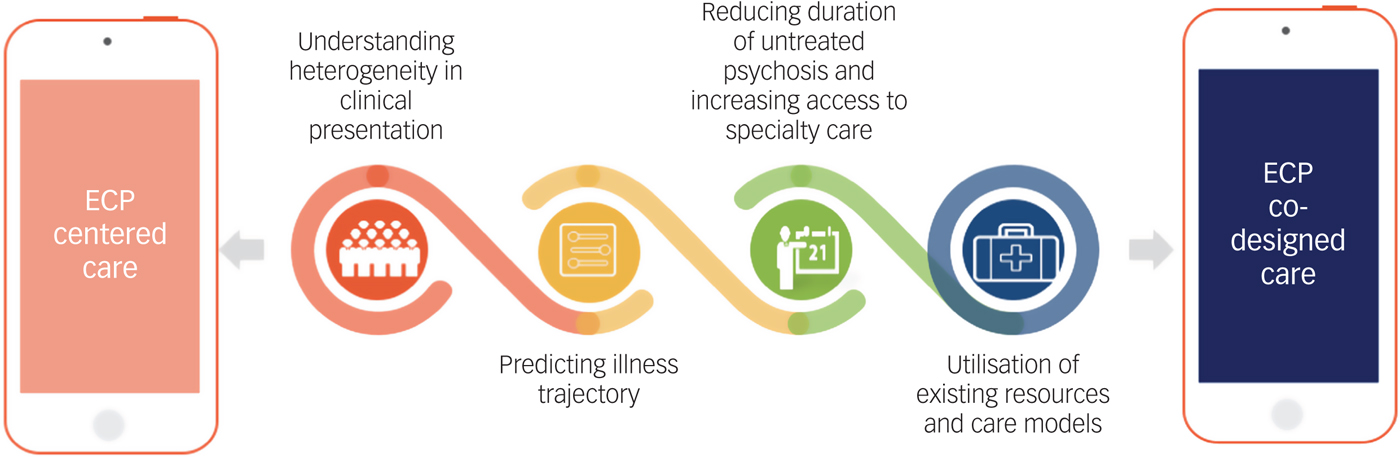
Fig. 1 Potential role of digital technology in improving early-course psychosis care.
Understanding heterogeneity in clinical presentation
Smartphones and related digital technologies offer a new strategy to approach heterogeneity of clinical presentation and produce a more personalised understanding of psychotic illness. Although hallucinations and unusual thoughts/delusions are characteristic of ECP, they are also present in other illnesses and are non-specific to psychotic disorders.Reference Waters and Fernyhough8 Indeed, the value of the term schizophrenia itself has been called into question as it becomes clear there is no discrete entity or single syndrome.Reference Murray9 Understanding this heterogeneity requires a better understanding of not only the clinical presentation of ECP, but also the lived experience. Smartphones and other wearable devices (such as smartwatches, fitness trackers) can now capture ecologically valid data in real-time on key behavioural and functional indicators, including: ecological momentary assessment data regarding symptoms and daily experiences via self-report surveys, physical activity and physiology data (for example heart rate, step counts), patterns of daily life such as attending work and daily mobility/distance travelled, and social outcomes such as phone call and text message reciprocity. Recent work on digital phenotyping – the ‘moment-by-moment quantification of the individual-level human phenotype in situ, using data from personal devices such as mobile phones’ – offers a practical means to achieve this.Reference Torous, Kiang, Lorme and Onnela10
Data show that capturing spatial trajectories through GPS (global positioning system) and social networking through call/text logs from the personal devices of those with psychotic disorders does not increase paranoia or cause known harm.Reference Torous, Staples and Onnela11 Rather this data offers potential insights into how symptom clusters may drive clinical presentations such as social withdrawal and social anhedonia via changes in call/text reciprocity, or avolition and lethargy via changes in movement tracked through GPS in ECP.Reference Torous, Staples, Barnett, Sandoval, Keshavan and Onnela12 This wealth of easily accessible, and often automatically collected information, offers a new lens to better characterise the lived experience of those with ECP and explore new subtypes and clusters of psychosis based on new data.
Just as recent research has used biomarker panels including neuropsychological, stop signal, saccadic control and evoked-response paradigm metrics to identify three neurobiologically distinct psychosis biotypesReference Clementz, Sweeney, Hamm, Ivleva, Ethridge and Pearlson13 – smartphones offer a complementary stream of data to transform clinical heterogeneity into unique social, functional, cognitive and physiological domains that previously have been difficult to capture or quantify.
Predicting illness trajectory
A long-recognised holy grail of ECP research is the ability to accurately predict illness trajectory to facilitate early intervention and prevent bad outcomes. This includes accurate prediction of: (a) psychosis onset from a high-risk state; (b) relapse of psychotic symptoms, and (c) individual differences in long-term outcomes. To date, success in these three domains has been limited: only 20–40% of individuals identified as at high-risk go on to develop a psychotic disorder;Reference Fusar-Poli, McGorry and Kane14 tools for understanding long-term outcomes are typically dichotomous and may miss important individual differences; and although there are known relapse predictors (for example early signs of symptom exacerbation), prediction is limited by a lack of real-time actionable data. It is now understood that a fine-grained understanding of racial, ethnic, diversity and social characteristics of an individuals’ environment is critical.Reference Richardson, Hameed, Perez, Jones and Kirkbride15
Smartphones and related wearable technologies offer a feasible and scalable method to capture day-to-day fluctuations in environmental, physiological and social indicators necessary to better understand, model and predict illness trajectory. Preliminary data support this: latent semantic analysis of speech samples captured via smartphone resulted in 72% accurate prediction of conversion to psychosisReference Corcoran, Carrillo, Fernández-Slezak, Bedi, Klim and Javitt16 – a significant improvement from current models, and a scalable method given the ubiquity of smartphones for capturing speech samples.
For relapse prediction, longitudinal data demonstrates that monitoring relapse predictors via smartphone is feasible in individuals with ECP, and that self-report surveys via smartphone are a viable and valid method for monitoring signs of relapse.Reference Niendam, Tully, Iosif, Kumar, Nye and Denton17 Further, a recent pilot study suggests that 2 weeks prior to relapse individuals with schizophrenia demonstrate significant changes in mobility indicators derived from GPS data, sociability indicators derived from text message and call data, and symptom exacerbation indicators derived from in-app self-report surveys – indicating that we may be able to capture digital indicators of relapse with minimal burden on the individual.Reference Barnett, Torous, Staples, Sandoval, Keshavan and Onnela18
Novel technologies for monitoring medication adherence – a primary risk factor for relapse – are also emerging. In 2017, the pharmaceutical company Otsuka received US Food and Drug Administration marketing approval for a new formulation of aripiprazole that uses a sensor to monitors ingestion via sending a signal when the medication is in the stomach. This ‘digital pill’ offers a low burden method for individuals with ECP and providers to monitor medication adherence and problem-solve non-adherence quickly to prevent relapse.
Although research on predicting illness trajectory using digital technology is still in its infancy, data gathered to date support feasibility and validity, and suggest that leveraging smartphone and related wearable/sensor technologies to create data-rich models of day-to-day fluctuations in symptoms and functioning could facilitate the identification of ‘digital biomarkers’ for ECP.Reference Torous, Staples and Onnela11
Reducing duration of untreated psychosis and increasing access to specialty care
A prolonged duration of untreated psychosis (DUP) predicts further disability, relapse and a higher cost of treatment over time.Reference Fusar-Poli, McGorry and Kane14 Reducing DUP requires both improved early identification and increased access to specialty care – smartphones and associated digital health tools could ameliorate both issues. For example, technology-enhanced population-level screening for psychosis and automatic referral to specialty care could potentially increase early identification rates and reduce DUP. Indeed, recent reports of technology-facilitated psychosis screening in schools and community health centres demonstrates high levels of acceptability with 75% of staff noting it did not increase their workload.Reference Savill, Skymba, Ragland, Niendam, Loewy and Lesh19 Beyond early identification, preliminary feasibility and acceptability data across international settings indicate smartphone and web-based care options could also address barriers related to access to, engagement with and continuity of ECP care.
In the USA, PRIME, a smartphone and web-based peer-to-peer intervention platform for improving motivation and quality of life in individuals with ECP, showed high feasibility and acceptability in preliminary testing.Reference Schlosser, Campellone, Kim, Truong, Vergani and Ward20 A subsequent study demonstrated that those who rarely used PRIME benefited as much as those who regularly engaged with the app, suggesting a lack of a dose effect.Reference Schlosser, Campellone, Truong, Etter, Vergani and Komaiko21 Promising pilot data have been reported for MOST, a web-based peer-to-peer intervention platform developed in Australia for improving social functioning in youth at risk for psychosis.Reference Rice, Gleeson, Leicester, Bendall, D'Alfonso and Gilbertson22 Newer technologies also promise to increase access to early interventions. Research on those at high risk for psychosis and with ECP has found virtual reality interventions to be both acceptable and feasible, without adverse events such as worsening paranoia or delusions.Reference Canty, Neumann and Shum23 Although virtual reality headsets are not commonly owned today, the rapid global rise of smartphone ownership exemplifies the scalability of digital tools. These data are promising and suggest that individuals with ECP in areas with no bricks-and-mortar specialty care programmes will be willing and able to access evidence-based treatments at scale via digital technology, independent of traditional care settings.
Utilisation of existing resources and care models
Even with access to existing specialised care, up to 40% of those with ECP may disengage with services despite continued clinical needs.Reference Doyle, Turner, Fanning, Brennan, Renwick and Lawlor24 Although apps are not a panacea, they can be integrated into existing care settings to offer the ECP community new tools and means to engage with care. Recent work indicates that integrating a digital technology platform in community-based ECP is feasible and perceived as valuable by clients and providers alike.Reference Kumar, Tully, Iosif, Zakskorn, Nye and Zia25 Similarly, the Heal Your Mind app, designed for cognitive–behavioural case management and symptom monitoring in ECP, has been well received by users in pilot studies.Reference Kim, Lee, Yu, Jung, Lee and Kim26 Preliminary efficacy data are also emerging: the app WellWave was successfully integrated into an early psychosis programme to boost levels of physical activity and help users better connect with peer staff,Reference Macias, Panch, Hicks, Scolnick, Weene and Öngür27 and a recent study pitting two apps against treatment as usual in the UK indicates positive treatment effects on negative, positive and mood symptoms.Reference Bucci, Barrowclough, Ainsworth, Machin, Morris and Berry28
Between both clinically integrated apps and self-care resources, technology-based solutions offer new avenues to increase utilisation and augment existing mental health resources for ECP. New care models that take full advantage of these technologies while still preserving the clinical therapeutic relationship necessary to fully use these tools may be a new horizon for the optimal use of these apps. The ECP digital clinic models in development at Beth Israel Deaconess Medical CenterReference Torous and Hsin29 and piloting at UC DavisReference Niendam, Tully, Iosif, Kumar, Nye and Denton17, Reference Kumar, Tully, Iosif, Zakskorn, Nye and Zia25 are examples of this novel pathway to augment and extend the impact of existing specialised care services.
Barriers
Despite these promising preliminary feasibility, acceptability and efficacy data, three key implementation issues face the field of digital health technology in ECP care: (a) implementation logistics; (b) implementation costs; (c) user-engagement and ethical issues.
Logistics are particularly relevant for tools implemented as part of traditional care settings. To date, the majority of feasibility studies have been conducted in academic research settings that do not emulate real-world clinical environments. For successful dissemination in ECP care settings, the practicalities of technical support, training clinical and administrative staff and the necessary infrastructure for data management and analysis must be addressed. This may require new partnerships between health systems and technology companies and begs the question of the second implementation issue – implementation costs.
To date studies of smartphone apps for psychotic disorders have not reported cost-effectiveness data. Although smartphones offer the potential to deliver scalable lower cost services, implementation still requires investment to provide smartphones (as necessary), technical support, data storage and analysis and technology upgrades. For health systems to widely adopt digital health tools, there must be clear cost savings, either in the form of reduced cost of care as a consequence of relapse prevention or as a consequence of increased capacity to serve those in need.
These technologies must be designed to be engaging as services delivered via an app will quickly loose users to drop out and app-based services that do not utilise healthcare interoperability standards for apps to transfer data to and from electronic medical records risk low engagement from the provider side. Involvement of both ECP clients and ECP care providers during product design is necessary to ensure the development of engaging digital health tools that enhance ECP care and outcomes.
Digital technology tools also raise important ethical issues regarding informed consent, privacy and responsible data use. Recent high-profile data breaches from large social media corporations in which user data were sold to third-party corporations without user informed consent have raised suspicion among users and highlights the need for clear and ethical data use and privacy practices. This is particularly important when vulnerable populations and private health information are involved. Standard End User License Agreements (EULA), typically several pages long and dense with legalese, are not effective tools for informed consent and predominantly serve to protect the company but not the user. This is problematic in the case of digital health tools involving collection of massive amounts of personal data (such as voice and text analysis, GPS identifying where the person sleeps at night). Although the purpose of this close monitoring is to improve ECP outcomes and empower individuals with ECP in their care, there is also potential risk of harm from a data breach or legal subpoena.
The digital health technology field should be held to the highest standards of informed consent and privacy practices and must proactively address key questions regarding data ownership and third-party data use to avoid misuse and abuse of vulnerable populations’ data. At minimum, we recommend comprehension checks for EULA and explicit agreement options for specific types of data sharing, rather than a catch-all agreement option. Importantly, treatment provision must not be contingent on an individual agreeing to digital health monitoring as this could disproportionately affect those who are most vulnerable. Other unintended consequences of digital health technology should be considered in order to build appropriate safeguards against later reuse of data for insurance coverage, employment decisions or marketing.
An equally pressing issue is informed consent in the digital age and willingness of patients to use digital phenotyping apps outside of research studies and actually as part of care. As remote clinical studies, in which ECP individuals partake in research without ever meeting the research team, become feasibleReference Schlosser, Campellone, Truong, Etter, Vergani and Komaiko21 it remains unclear how to ensure participants understand the risks and benefits. Research outside of ECP suggests that those with lower health literacy are more likely to have positive perceptions of the privacy afforded by health technologies, suggesting they may underestimate the risks.Reference Mackert, Mabry-Flynn, Champlin, Donovan and Pounders30 Conversely, recent survey data suggests that those with mental health disorders, including psychosis, are least comfortable sharing automatically collected GPS, phone audio and phone text message data.Reference Di Matteo, Fine, Fotinos, Rose and Katzman31, Reference Torous, Wisniewski, Liu and Keshavan32 This suggests the importance of a patient-centred approach, in which the digital health technology field must work closely with individuals with ECP from the inception of any digital health technology project to ensure data are collected and used in manners all stakeholders understand and agree upon.
Conclusions
Although digital health technology shows high feasibility and acceptability for advancing ECP care, technology alone is not a panacea. Important questions remain regarding the efficacy, privacy, usability and stability of digital health tools. These questions would likely be best addressed via academic research and technology industry partnerships, which will in turn require a solution to the mismatched incentive structures that can impede productive and ethical collaborations. However, we argue that these are questions worth addressing. The enormous potential and scalability of digital health technology offers an unparalleled opportunity to approach the challenge of improving ECP care with a new lens, new methods and new interventions.
Funding
This work was supported by a Building Interdisciplinary Research Careers in Women's Health award (K12 HD051958) awarded to L.M.T., funded by the National Institute of Child Health and Human Development (NICHD), Office of Research on Women's Health, Office of Dietary Supplements and the National Institute of Aging. J.T. is supported by a NIMH Career Development Award (K23 MH116130-01), a NARSAD Young Investigator Award from the Brain & Behavior Research Foundation and the Natalia Mental Health Foundation.



eLetters
No eLetters have been published for this article.