Background
The COVID-19 pandemic has resulted in radical changes to societies globally. As the number of infected cases and deaths increased, many countries adopted public health measures, including lockdown, social distancing, self-isolation and school and business closures, resulting in an unprecedented impact on the global economy, which may also have a profound effect on mental health.Reference Holmes, O'Connor, Perry, Tracey, Wessely and Arseneault1–Reference Brooks, Webster, Smith, Woodland, Wessely and Greenberg3 However, the extent to which mental health is affected by COVID-19 and its management, and who is at greatest risk, is still unclear. Evidence from previous outbreaks such as the severe acute respiratory syndrome epidemic,Reference Lam, Wing, Yu, Leung, Ma and Kong4–Reference Tsang, Scudds and Chan8 and rapid COVID-19 cross-sectional surveys, suggest that depression, anxiety and lower well-being may increase during the COVID-19 pandemic.Reference Qiu, Shen, Zhao, Wang, Xie and Xu9–12
Several rapid cross-sectional surveys during the pandemic have suggested a higher prevalence of anxiety, depressionReference Qiu, Shen, Zhao, Wang, Xie and Xu9,Reference Lai, Ma, Wang, Cai, Hu and Wei10 and low well-being compared with historical estimates.12 However, these studies lack pre-pandemic information on mental health assessments, and potential confounding factors, in the same people before the pandemic. This precludes accurate assessment of whether adverse mental health outcomes during the pandemic are largely accounted for by those with existing or previous mental health problems having poorer mental health as a result of COVID-19 mitigation efforts, or whether there are important contributions of the pandemic that are related to poor mental health in those with no previous history. Furthermore, selection bias (because of mental health influencing those who respond to surveys) and reporting bias (from those who perceive depression and anxiety as higher or are more likely to report symptoms when they feel there is a ‘valid’ reason) could threaten the validity of results from cross-sectional surveys. There is a need for longitudinal designs with well-characterised sampling frames and pre-pandemic data.Reference Pierce, McManus, Jessop, John, Hotopf and Ford13 Such studies can more accurately quantify differences in mental health from pre-pandemic levels, and identify groups that are most at risk of adverse mental health in response to the COVID-19 pandemic. These results can then inform development of interventions for those at heightened risk, and aid policy decisions regarding the immediate and subsequent management of the COVID-19 response. This includes plans for easing restrictions and monitoring at-risk groups as subsequent waves or epidemics occur, and plans for the longer-term care for groups whose mental health may be particularly affected.Reference Holmes, O'Connor, Perry, Tracey, Wessely and Arseneault1,Reference Xiang, Yang, Li, Zhang, Zhang and Cheung14 The COVID-19 pandemic is likely to exacerbate existing social and psychological inequalities.Reference Gunnell, Appleby, Arensman, Hawton, John and Kapur15 Previous studies have identified several groups who may be at greater risk of poorer mental health during the pandemic, including younger people, parents, women, healthcare workers and those with poorer financial or living circumstances.Reference Qiu, Shen, Zhao, Wang, Xie and Xu9–Reference Fancourt, Bu, Mak and Steptoe11,Reference McGinty, Presskreischer, Han and Barry16 However, many groups remain unexplored, such as individuals at risk of abuse and those at greater physical risk of COVID-19 (older age, and those with chronic conditions such as asthma or obesity).
Aims
We aimed to use data from two independent longitudinal cohort studies, both with rich pre-pandemic measures of mental health, to quantify how mental health changed from pre-pandemic levels to the COVID-19 pandemic, and identify groups within the population at greater risk of poorer mental health during the pandemic. The first of these is important for exploring the impact of COVID-19 and its management on mental health and potential increases in poor mental health long term. The second is important for targeting of mental healthcare needs now, and during any subsequent waves, and for identifying groups who might benefit from long-term monitoring after the pandemic.
Method
Samples
We selected two comparable cohort studies, to allow replication in different regions of the UK, both with similar timings of mental health measures before and during the COVID-19 pandemic.
The Avon Longitudinal Study of Parents and Children (ALSPAC) is an ongoing longitudinal population-based study that recruited pregnant women residing in Avon (South-West England) with expected delivery dates between 1 April 1991 and 31 December 1992.Reference Boyd, Golding, Macleod, Lawlor, Fraser and Henderson17,Reference Fraser, Macdonald-Wallis, Tilling, Body, Golding and Davey Smith18 The cohort comprised 13 761 mothers and their partners (hereafter referred to as ALSPAC-parents), and their 14 901 children, now young adults (hereafter referred to as ALSPAC-young).Reference Northstone, Lewcock, Groom, Boyd, Macleod and Timpson19 The study website contains details of all data, available through a fully searchable data dictionary (http://www.bristol.ac.uk/alspac/researchers/our-data/). Ethical approval for the study was obtained from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committees.
Generation Scotland: Scottish Family Health Study is a family longitudinal study of 24 084 individuals recruited across Scotland between 2006 and 2011.Reference Smith, Campbell, Linksted, Fitzpatrick, Jackson and Kerr20 Participants were recruited into the study if they were aged ≥18 years. Participants of Generation Scotland have been followed up longitudinally,Reference Navrady, Wolters, MacIntyre, Clarke, Campbell and Murray21 and further details can be found on the study website (http://www.generationscotland.org). Ethical approval for the study was approved by National Health Service Tayside Committee on Medical Research Ethics (reference 05/S1401/89). We assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. Written informed consent was obtained from all participants in both studies.
This study uses data from 3720 individuals in the ALSPAC-parents cohort and 2973 individuals in the ALSPAC-young cohort who completed an online questionnaire about the impact and consequences of the COVID-19 pandemic between 9 April and 14 May 2020 (see Supplementary Figs 1 and 2 available at https://doi.org/10.1192/bjp.2020.242).Reference Northstone, Haworth, Smith, Bowring, Wells and Timpson22 In Generation Scotland, data were from 4233 individuals who completed a similar online COVID-19 questionnaire between 17 April and 17 May 2020 (see Supplementary Fig. 3). Mitigation measures were announced in the UK on the 24 March 2020.
COVID-19 pandemic measures of mental health
The measures used here examine symptoms in the preceding 2 weeks, and thus represent mental health in the immediate period following mitigation. Depressive symptoms in ALSPAC were measured with the Short Mood and Feelings Questionnaire (SMFQ),Reference Angold, Costello, Messer and Pickles23 a 13-item instrument with scores ranging between 0 and 26, with higher scores indicting higher depressive symptoms. In Generation Scotland, depressive symptoms were measured with the Patient Health Questionnaire-9 (PHQ-9),Reference Kroenke, Spitzer and Williams24 a nine-item instrument with scores ranging between 0 and 27, with higher scores indicating worse depressive symptoms. Anxiety symptoms in ALSPAC and Generation Scotland were both measured with the Generalised Anxiety Disorder Assessment-7 (GAD-7),Reference Spitzer, Kroenke, Williams and Lowe25 a seven-item instrument with ranging between 0 and 21, with higher scores indicting greater generalised anxiety disorder symptoms. Mental well-being in ALSPAC and Generation Scotland were both measured with the Short Warwick-Edinburgh Mental Wellbeing Scale (SWEMWBS),Reference Stewart-Brown, Tennant, Tennant, Platt, Parkinson and Weich26 a seven-item instrument with scores ranging between 7 and 35, with higher scores indicating better mental well-being. These measures have recommended cut-offs for examining the proportion of individuals with probable depression (≥11 on the SMFQ and ≥10 on the PHQ-9),Reference Kroenke, Spitzer and Williams24,Reference Turner, Joinson, Peters, Wiles and Lewis27 generalised anxiety disorder (≥10 on the GAD-7)Reference Kroenke, Spitzer, Williams, Monahan and Lowe28 and poor mental well-being (≤17 on the SWEMWBS),29 with good sensitivity and specificity for identifying clinical disorder, using validated interviews and instruments, and are widely used in primary care and clinical trials. Herein, we refer to depressive symptoms as depression, and anxiety symptoms as anxiety.
Pre-pandemic assessments of mental health and factors
Pre-pandemic depression and anxiety were assessed in ALSPAC and Generation Scotland before the COVID-19 pandemic. In the ALSPAC-young cohort, pre-pandemic mental well-being was also assessed. The median length of time between the pre-pandemic assessments and COVID-19 pandemic assessments of mental health ranged from 2 to 7 years in the ALSPAC-young cohort, 7 to 20 years in the ALSPAC-parents cohort and 4 to 5 years in the Generation Scotland cohort. These measures, their timings and harmonisation are described in Table 1 and in Supplementary Methods, alongside detailed information on pre-pandemic factors that may be associated with poorer mental health during the COVID-19 pandemic in regression analyses. We refer to these as factors to make it clear that we are not assuming they are causal, but could be useful in the short term, for identifying at-risk groups. Factors included sociodemographic information, such as biological sex, age, educational background, financial circumstances, deprivation status, victimisation and being a parent with school-aged children. Additional factors included pre-existing mental health conditions, substance misuse, genetic risk for depression, cognitive styles, personality traits and difficulties accessing mental health information. Because of differences in data collection, several factors are only assessed in either ALSPAC or Generation Scotland. We also examined associations with several COVID-19-specific factors, including pre-pandemic obesity, pre-pandemic asthma, a self-reported suspected or confirmed diagnosis of COVID-19, isolation status, living alone, access to a garden and healthcare worker and key worker status.
Table 1. Pre-pandemic mental health measures and factors assessed in ALSPAC and Generation Scotland
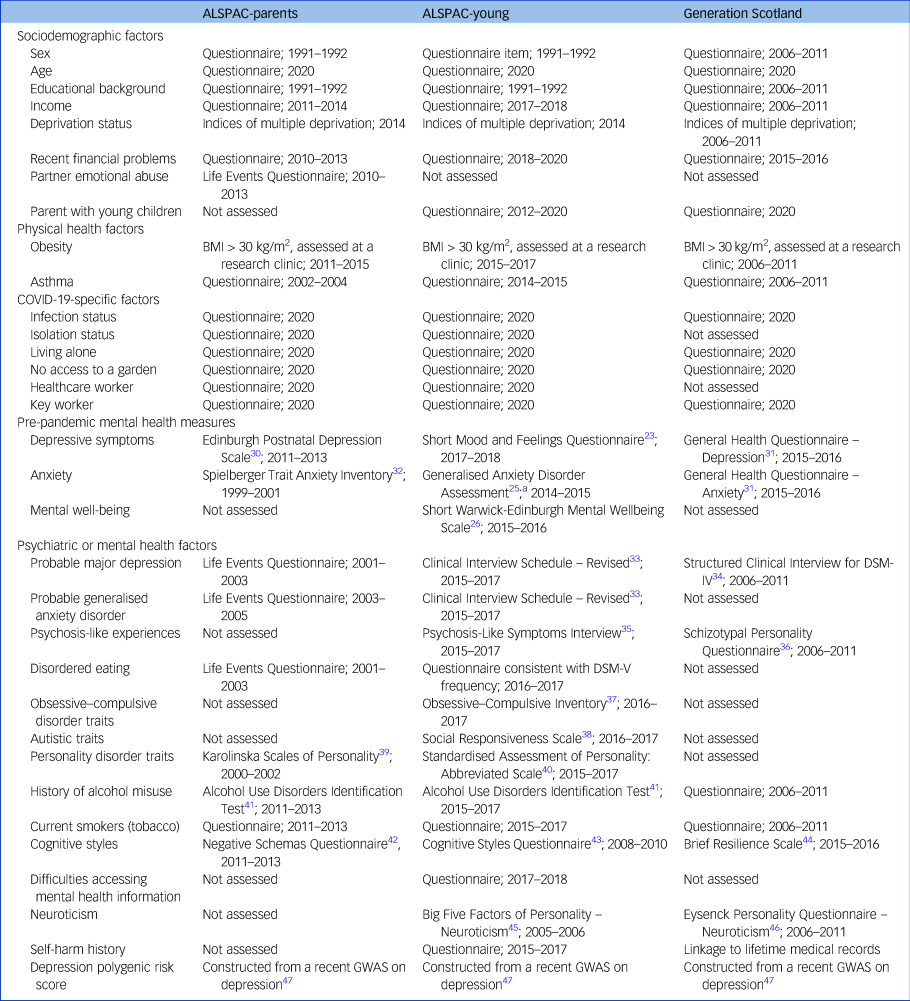
Data are shown in format: measure used in analyses; timing of assessment. Questionnaire refers to a single questionnaire item used. ALSPAC-parents, original parents in the Avon Longitudinal Study of Parents and Children; ALSPAC-young, original children in the Avon Longitudinal Study of Parents and Children; BMI, body mass index; GWAS, genome-wide association study.
a. We supplemented data with more recent timings of anxiety symptoms from the Clinical Interview Schedule – Revised between 2015 and 2017.
Statistical analysis
Analysis was conducted in StataSE, version 15 for Windows(StataCorp LLC). Initially, we described the prevalence of mental health outcomes during the COVID-19 pandemic in all cohorts. To answer our first research objective (How has the prevalence of mental health changed from pre-pandemic to COVID-19?), we used the ALSPAC-young cohort to quantify differences in mental health from pre-pandemic to COVID-19 levels, as this was the only cohort with the identical measures of mental health assessed before and during the pandemic (i.e., the SMFQ, GAD-7 and SWEMWBS). Our hypothesis is that the COVID-19 pandemic is likely to have caused a rise in depression and anxiety in the population as a whole. This hypothesis cannot be explicitly tested, given that COVID-19 mitigation efforts have been a universal exposure. However, looking at changes from baseline analysis provides some initial evidence for this hypothesis. The GAD-7 was only assessed once before the pandemic (between 2014 and 2015), so we also compared the prevalence of anxiety during the COVID-19 pandemic with probable anxiety disorder as assessed with the Clinical Interview Schedule – Revised,Reference Lewis, Pelosi, Araya and Dunn33 at two other occasions (between 2008 and 2010 and between 2015 and 2017). This was to provide more thorough pre-pandemic information on anxiety, and to harmonise timings for pre-pandemic mental health. We also analysed item-level responses for the SMFQ, GAD-7 and SWEMWBS to examine how specific mental health items differed before and during the pandemic.
To answer our second research objective (Are there groups within the general population that are at heightened risk of depression and anxiety during the COVID-19 pandemic?), we examined associations between factors measured before and during the pandemic with depression and anxiety during the COVID-19 pandemic, accounting for pre-pandemic depression and anxiety (with the most recent matched measures available). We included pre-pandemic measures of depression and anxiety as covariates into our regression models, so the shared variance between pre-pandemic and COVD-19 pandemic depression and anxiety were accounted for. The adjusted coefficients represent the extent to which the factors are associated with depression and anxiety during the COVID-19 pandemic, independent of prior mental health. Analysis was conducted separately for all cohorts, adjusted for sex, age and the date they completed the COVID-19 questionnaire (to account for response times). We chose to run minimised regressions to avoid potential biases from collider bias and to identify risk populations who could be followed up in greater detail, with more specific confounding structures. Pre-pandemic mental well-being was not assessed in ALSPAC-parents or Generation Scotland cohorts; therefore, we restricted this analysis to depression and anxiety only. Continuous COVID-19 pandemic and pre-pandemic depression and anxiety were standardised to create Z-scores, allowing comparison of effect sizes across outcomes and cohorts.
Missing data
Our eligible samples were those who completed at least one mental health measure during the COVID-19 surveys: ALSPAC-parents cohort, n = 3579; ALSPAC-young cohort, n = 2872 and Generation Scotland cohort, n = 4208 (Supplement Figs 1–3, Supplement Table 1). To address potential bias from attrition in the cohorts, we imputed pre-pandemic depression, anxiety and factors, with related information and auxiliary variables up to the eligible samples, using multiple imputation by chained equations to generate 50 imputed data-sets.Reference Royston and White48 Details regarding imputation and a list of auxiliary variables are available in the Supplementary Material.
Sensitivity analyses
We ran several sensitivity analyses, including complete-case analysis, adjusting for educational background with the imputed data, using the validated cut-offs rather than continuous scores as outcomes and using varying timings for pre-pandemic depression, anxiety and financial problems, to ensure there were no substantial changes as a result of proximal timings between assessments and the COVID-19 pandemic. We also estimated ‘counterfactual’ trajectories for the mental health measures in the ALSPAC-young cohort to highlight differences in what would we expected had COVID-19 not happened, given previous trajectories, compared with what was observed during the pandemic. Finally, we analysed item-level responses for the SMFQ, GAD-7 and SWEMWBS to examine how specific components of each measurement differed from the most recent pre-pandemic assessment and the COVID-19 pandemic assessment. Further information regarding these analyses are given in the Supplementary Material.
Results
Data on mental health outcomes during the COVID-19 pandemic were available for 3579 people (mean age 58.67 years, s.d. 4.82) for the ALSPAC-parents cohort, 2872 people (mean age 27.61 years, s.d. 0.54) for the ALSPAC-young cohort and 4208 people (mean age 59.24 years, s.d. 12.03) for the Generation Scotland cohort. Individuals included in these analyses were more likely to be female and have higher educational backgrounds, but did not differ by pre-existing depression or anxiety symptoms (Supplementary Table 1).
Prevalence of mental health outcomes during the COVID-19 pandemic
The prevalence of probable depression during the COVID-19 pandemic was highest for younger individuals (ages 18–40 years), and decreased with older age in ALSPAC and Generation Scotland. Similar results were observed for probable anxiety and lower well-being (Supplementary Figs 4 and 5).
Differences in mental health before and during the COVID-19 pandemic in the ALSPAC-young cohort
The percentage of ALSPAC-young participants with probable depression was lower during the pandemic, at 18.14% (95% CI 16.76–19.61%) compared with 24.35% (95% CI 23.04–26.70%) at the most recent pre-pandemic assessment. However, the percentage of participants with probable anxiety disorder almost doubled during the pandemic, at 24.35% (95% CI 22.81–25.96%) compared with pre-pandemic levels (12.97%, 95% CI 11.87–14.15%); as did the percentage for lower well-being, at 13.27% (95% CI 12.07–14.15%) compared with 7.59% (95% CI 6.82–8.43%) (Fig. 1, Supplementary Tables 5 and 6). When examining continuous measures for comparisons between the most recent pre-pandemic and pandemic assessments, there was a mean difference of −0.60 (95% CI −0.84 to −0.37) in SMFQ score, 1.36 (95% CI 1.10–1.61) in GAD-7 score and 2.45 (95% CI 2.25–2.65) in SWEMWBS score. For magnitude, these estimates represent a 0.11, 0.26 and 0.51 standardised effect difference for depression, anxiety and lower well-being, respectively (Supplementary Table 7). Item-level analysis showed that for the SMFQ (depression), the only items that scored higher during the COVID-19 pandemic were ‘no enjoyment’, ‘felt restless’ and ‘found it hard to think’. For the GAD-7 (anxiety) and the SWEMWBS (mental well-being), all items scored higher during the COVID-19 pandemic compared with the most recent pre-pandemic assessment, with similar variances (Supplementary Fig. 6).
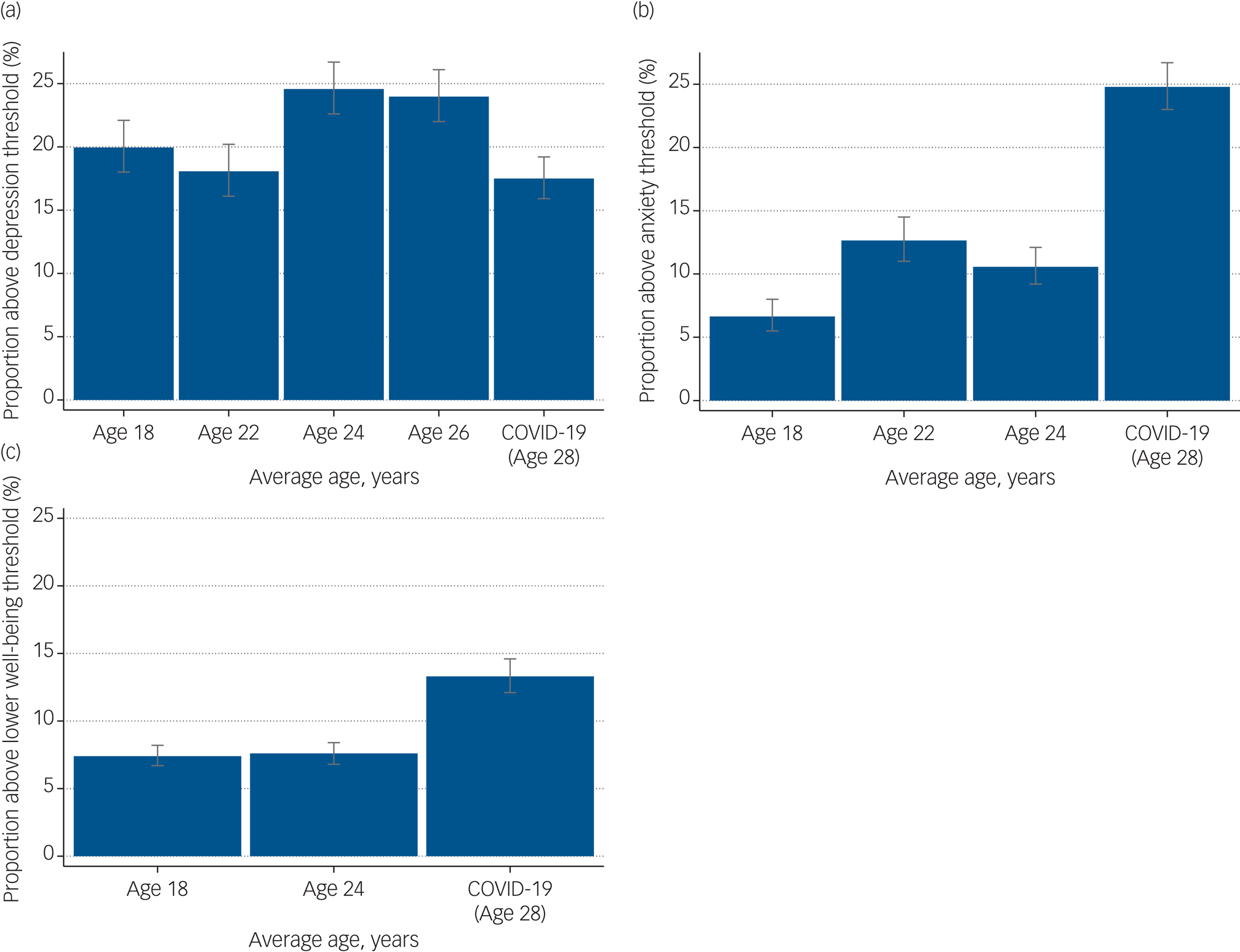
Fig. 1 Changes in mental health from pre-pandemic to during the COVID-19 pandemic in the ALSPAC-young cohort. (a) Changes in probable depression, as assessed by the SMFQ. (b) Changes in probable generalised anxiety disorder, as assessed by the GAD-7 at age 22 years and the CISR GAD at ages 18 and 24 years. (c) Changes in lower well-being, as assessed by the SWEMWBS. ALSPAC-young, original children in the Avon Longitduinal Study of Parents and Children; CISR GAD, Clinical Interview Schedule – Revised, Generalised Anxiety Disorder; GAD-7, Generalised Anixety Disorder Assessment; SMFQ, Short Mood and Feelings Questionnaire; SWEMWBS, Short Warwick Edinburgh Mental Wellbeing Scale.
Factors related to depression and anxiety during the COVID-19 pandemic
Supplementary Table 8 and Figs 2 and 3 show all the associations between pre-pandemic and COVID-19-specific factors and depression and anxiety during the early stages of COVID-19, accounting for pre-pandemic assessments of depression and anxiety (measured on a continuous scale in s.d. units for ease of comparison between cohorts and outcomes, i.e. standardised regression coefficients). As stated above, these results can be interpreted as factors associated with depression and anxiety during the pandemic, after accounting for previous depression and anxiety, thus resulting in associations that are independent of prior mental health.

Fig. 2 Associations between pre-pandemic and COVID-19-specific factors and depression during the COVID-19 pandemic, adjusted for the most recent pre-pandemic assessment of depression, sex, age and when the COVID-19 questionnaire was completed, using imputed data (estimates match Supplementary Table 8). Estimates refer to an s.d. increase in depression, over and above pre-pandemic depression. (a) Associations between pre-pandemic sociodemographic factors and depression during the COVID-19 pandemic. (b) Associations between pre-pandemic physical health and COVID-19-specific factors and depression during the COVID-19 pandemic. (c and d) Associations between pre-pandemic mental health factors and depression during the COVID-19 pandemic. ALSPAC-parents, original parents in the Avon Longitudinal Study of Parents and Children; ALSPAC-young, original children in the Avon Longitudinal Study of Parents and Children; OCD, obsessive compulsive disorder; PRS, polygenic risk score.

Fig. 3 Associations between pre-pandemic and COVID-19-specific factors and anxiety during the COVID-19 pandemic, adjusted for the most recent pre-pandemic assessments of anxiety, sex, age and when the COVID-19 questionnaire was completed, using imputed data (estimates match Supplementary Table 8). Estimates refer to an s.d. increase in anxiety, over and above pre-pandemic anxiety. (a) Associations between pre-pandemic sociodemographic factors and anxiety during the COVID-19 pandemic. (b) Associations between pre-pandemic physical health and COVID-19-specific factors and anxiety during the COVID-19 pandemic. (c and d) Associations between pre-pandemic mental health factors and anxiety during the COVID-19 pandemic. ALSPAC-parents, original parents in the Avon Longitudinal Study of Parents and Children; ALSPAC-young, orignal children in the Avon Longitudinal Study of Parents and Children; OCD, obsessive compulsive disorder; PRS, polygenic risk score.
Pre-pandemic sociodemographic factors
Being female and pre-pandemic financial problems were associated with higher depression and anxiety during the COVID-19 pandemic in ALSPAC-parents, ALSPAC-young and Generation Scotland cohorts. Lower educational background was associated with greater depression in ALSPAC-parents and Generation Scotland cohorts, but not in the ALSPAC-young cohort; and with greater anxiety in ALSPAC-parents and ALSPAC-young cohorts, but not in the Generation Scotland cohort. Higher income before the pandemic was associated with lower depression in ALSPAC-parents and Generation Scotland cohorts, but not in the ALSPAC-young cohort; and with lower anxiety in ALSPAC-young and Generation Scotland cohorts, but not in the ALSPAC-parents cohorts. Higher neighbourhood deprivation was associated with higher depression in ALSPAC-parents and Generation Scotland cohorts, but not in the ALSPAC-young cohort; and with higher anxiety in ALSPAC-parents, ALSPAC-young and Generation Scotland cohorts. Being a parent of a young child was associated with higher anxiety in the ALSPAC-young cohort, but not in the Generation Scotland cohort (not assessed in the ALSPAC-parents cohort), and was not associated with depression in either cohort. Reporting an emotionally abusive partner was only available in the ALSPAC-parents cohort, and was positively associated with both greater depression and anxiety. Estimates are given in Supplementary Table 8 and shown in Figs 2A and 3A.
Physical health factors
Pre-pandemic obesity was associated with higher depression and anxiety in all cohorts. Pre-pandemic asthma status had positive associations with higher anxiety in ALSPAC-young and Generation Scotland cohorts, but not in the ALSPAC-parents cohort; and with higher depression in the Generation Scotland cohort, but not in either ALSPAC cohorts (see Supplementary Table 8 and Figs 2B and 3B).
COVID-19-specific factors
A self-reported suspected or confirmed COVID-19 diagnosis was associated with higher depression and anxiety in the ALSPAC-parents cohort, but only higher depression in Generation Scotland and ALSPAC-young cohorts. Living alone during the pandemic was also associated with higher depression in all cohorts, but was not associated with anxiety. No access to a garden was associated with higher depression in ALSPAC-parents, ALSPAC-young and Generation Scotland cohorts, along with higher anxiety in the Generation Scotland cohort. Self-isolation was associated with higher depression and anxiety in both ALSPAC-parents and ALSPAC-young cohorts, but was not measured in the Generation Scotland cohort. Key workers (of any kind) and healthcare workers were not associated with higher depression or anxiety in any cohort. However, there was an association between being a key worker and lower depression in the ALSPAC-young cohort, but this was not replicated in the ALSPAC-parents or Generation Scotland cohorts. Estimates are given in Supplementary Table 8 and shown in Figs 2B and 3B.
Pre-pandemic mental health and psychological factors
There were consistent associations for factors such as a history of major depression, a history of generalised anxiety disorder (not assessed in Generation Scotland), negative cognitive styles, psychosis-like symptoms, higher neuroticism and a history of self-harm (latter three not assessed in the ALSPAC-parents cohort). Eating disorder traits were associated with higher depression and anxiety in the ALSPAC-young cohort, but not in the ALSPAC-parents cohort, and was not assessed in Generation Scotland. Personality disorder traits were associated with greater depression in the ALSPAC-parents cohort, but not in the ALSPAC-young cohort; and with higher anxiety in both ALSPAC cohorts, but was not assessed in Generation Scotland. The depression polygenic risk score was positively associated with depression and anxiety in ALSPAC-parents and Generation Scotland cohorts, but was not associated with either depression or anxiety in the ALSPAC-young cohort. A history of alcohol misuse was associated with increased depression in the ALSPAC-young cohort, but not in ALSPAC-parents or Generation Scotland cohorts; and with increased anxiety in ALSPAC-parents and ALSPAC-young cohorts, but not in the Generation Scotland cohort. By contrast, daily smoking was associated with increased depression and anxiety in ALSPAC-parents and Generation Scotland cohorts, but not in the ALSPAC-young cohort. Several factors only measured in the ALSPAC-young cohort showed strong associations with higher depression and anxiety during the COVID-19 pandemic, including high obsessive–compulsive traits, high autistic traits and pre-pandemic reporting of difficulties accessing mental health services (see Supplementary Table 8 and Figs 2C, 2D, 3C and 3D).
Sensitivity analyses
The main results were similar to the complete-case analysis (Supplementary Table 9), adjusting for educational background with the imputed sample (Supplementary Table 10); examining different pre-pandemic timings of depression, anxiety and factors (Supplementary Tables 11–13); and examining the binary outcomes of depression and anxiety (Supplementary Table 14). Trajectory analyses (Supplementary Fig. 7) suggested higher anxiety and lower well-being during the COVID-19 pandemic were not expected, given the previous trajectory of pre-pandemic assessments. However, depression was in line with expectations.
Discussion
We report a population-based longitudinal study examining mental health during the COVID-19 pandemic. Although we found no clear evidence that depression differed during the COVID-19 pandemic from pre-pandemic assessments, there was strong observational evidence that anxiety was higher and well-being was lower during the pandemic, compared with pre-pandemic levels. Irrespective of the overall population differences in depression and anxiety, several sociodemographic, psychological, physical and COVID-19-specific factors were associated with greater depression and anxiety during the COVID-19 pandemic.
Mental health during the COVID-19 pandemic compared with pre-pandemic assessments
Approximately twice as many young adults experienced probable anxiety disorder and lower well-being during the pandemic, compared with previous longitudinal assessments. The mean rises of 0.26 s.d. in GAD-7 scores and 0.51 s.d. in SWEMWBS scores represent effect sizes that are clinically important and of a magnitude similar to those seen following treatment.Reference Lewis, Duffy, Ades, Amos, Araya and Brabyn49,Reference Carpenter, Andrews, Witcraft, Powers, Smits and Hofmann50 The rise in magnitude of anxiety and reduction in well-being in the ALSPAC-young cohort goes against expectations in the absence of COVID-19, highlighted in our sensitivity analysis with counterfactual trajectories, and shown by the wealth of descriptive mental health data in ALSPAC. The uncertainty and sudden change to everyday life, as well as concerns over health, may explain why anxiety has initially risen, rather than depression. The apparent rise in younger ages may reflect the effects of mitigation measures (i.e. lockdown and social distancing) rather than a risk of COVID-19 infection (potentially higher in older populations). Furthermore, depression usually relates to feelings of loss,Reference Malhi and Mann51 whereas anxiety relates to threat,Reference Craske and Stein52 which in this case could be rapid change in society and potential for adverse social and psychological outcomes. There is also evidence that anxiety changes more rapidly than depression after treatment.Reference Lewis, Duffy, Ades, Amos, Araya and Brabyn49 What separates this pandemic from historical outbreaks is the global impact. This, alongside the community spirit, may have been initially protective against the self-blame and guilt intrinsic to depression.Reference Malhi and Mann51 Indeed, the depression items that scored lower in the pandemic, compared with pre-pandemic assessments, related to feelings of self-blame. However, this may change as the pandemic evolves and restrictions are eased, thus continued monitoring of mental health is vital for understanding both the short- and long-term impact of the pandemic.
Population factors associated with depression and anxiety during the COVID-19 pandemic
When accounting for pre-pandemic depression and anxiety, a reported or suspected COVID-19 infection was a factor for higher depression and anxiety during the pandemic in ALSPAC-parents and Generation Scotland cohorts, possibly reflecting the high perceived risk to physical health in older ages and supporting previous research,Reference Rogers, Chesney, Oliver, Pollak, McGuire and Fusar-Poli2 but must be interpreted with some caution because COVID-19 status in this study largely includes participants’ perception that they have COVID-19 (because of a lack of testing at this stage of the pandemic). It may be that those with pre-existing depression and anxiety are also more likely to perceive that their symptoms are COVID-19-related, and are therefore subject to reverse causation. There was consistent evidence from participants in ALSPAC and Generation Scotland that health risk groups previously associated with COVID-19, such as those with pre-pandemic obesity and, to some extent, pre-pandemic asthma, had higher depression and anxiety during the pandemic, potentially reflecting concerns regarding perceived risk of infection or the effects of more stringent social distancing. There was no evidence that key workers or health workers were at greater risk of depression or anxiety, suggesting that these groups are not yet experiencing difficulties.
Those who were self-isolating were at higher risk of both anxiety and depression, but living alone was consistently associated with greater depression only. The manifestation of depression rather than anxiety for those living alone may relate to loneliness, which is amplified with physical contact restricted to within households, again reflecting depression being related to absence and loss rather than threat, whereas self-isolation (which in this context is related to COVID-19 exposure) may be linked to anxiety through associated threat of the virus. Parents of young children were more anxious in ALSPAC, which may reflect stress related to the sudden change in child care provision. Financial problems, lower income and deprivation were associated with greater risk of depression and anxiety in ALSPAC-parents and Generation Scotland cohorts. Financial problems were also associated with higher depression and anxiety in the ALSPAC-young cohort. Although these cohorts may have different populations, the replication of financial concerns highlights the importance of global policies to mitigate the sudden socioeconomic impact of the pandemic. and ensure financial measures are accessible to those in need.Reference Wright, Steptoe and Fancourt53
As expected, individuals with a history of worse mental health across multiple domains were at greater risk of higher depression and anxiety during the pandemic, supporting concerns raised at the beginning of this pandemicReference Holmes, O'Connor, Perry, Tracey, Wessely and Arseneault1,Reference Gunnell, Appleby, Arensman, Hawton, John and Kapur15,Reference Druss54,Reference Yao, Chen and Xu55 and highlighting groups who could benefit from immediate support. Personality traits such as neuroticism and negative thinking patterns were strong factors for higher depression and anxiety during the pandemic, and are modifiable with interventions that could benefit those at risk currently or in future outbreaks, even if delivered remotely.Reference Shore, Schneck and Mishkind56
However, there are several limitations. First, as the pandemic is a universal exposure, it is difficult to attribute COVID-19 or its management directly to mental health outcomes. Many factors are likely to show an association with later depression and anxiety at any time.Reference Malhi and Mann51 However, we were able to use rich longitudinal data and methods before and during the COVID-19 pandemic, to demonstrate that anxiety and lower well-being were worse during the pandemic compared with several recent occasions. Sensitivity analysis suggested that this may go against expectations, but detailed follow-up of these measures is essential to fully understand the trajectory of mental health as a result of the COVID-19 pandemic. Nevertheless, it is likely these effects are, to some extent, related to COVID-19, and these results are some of the first to highlight observational associations that could be tested in more causal settings in future. Second, there were some differences in the measures used to assess mental health, both in the pre-pandemic and COVID-19 surveys and across cohorts. The ALSPAC-young cohort was the only cohort that had the same measures of mental health before and during the pandemic, meaning we were only able to accurately describe the change in mental health in this cohort. Thus, the substantial increase in anxiety and decrease in well-being may only be relevant to young populations. Caution must be taken when comparing change over time in the ALSPAC-parents cohort analysis because the measures differed before and during the pandemic. However, our analysis exploring the relationship between factors and mental health during the COVID-19 pandemic remains valid, as despite different pre-pandemic and COVID-19 pandemic measures, the underlying constructs of the measures are the same. These measures were validated against the same standard interview measures, meaning that it is possible to compare longitudinal associations across cohorts, a major strength of our study compared with some previous cross-sectional research. A third limitation is the difference in follow-up length across cohorts. These can be subject to recency effects, where results are stronger if they were measured more proximal to the outcome. However, sensitivity analyses exploring different pre-pandemic timings for depression and anxiety as mental health covariates, and for financial problems as a factor, gave similar conclusions, as shown in Supplementary Tables 11–13. Furthermore, under usual circumstances, depression and anxiety in adulthood are relatively stable, with measures several years apart showing high correlations.Reference Netsi, Pearson, Murray, Cooper, Craske and Stein57,Reference Kwong58 Thus, even measures assessed a number of years ago are valid methods to account for previous mental health. Finally, although we were able to use existing data such as educational background to identify pre-pandemic missingness and use such variables in imputation models, we did not impute any data beyond the sample with complete COVID-19 survey data, given that the data were unique. Thus, there may be issues with generalisability, as respondents were more likely to be female and from higher educational backgrounds than previous surveys.
In conclusion, these results are some of the first to provide an initial indication that the COVID-19 pandemic and related mitigation measures are associated with a clinically relevant increase in anxiety in younger populations. Several groups within the population were at heightened risk of higher levels of depression and anxiety during the pandemic. Future work is needed to understand the mechanisms and interplay between pre-pandemic and COVID-19-specific factors and mental health during the COVID-19 pandemic. Future research should consider how changes in anxiety might influence public behaviour through contact patterns and adherence to policies. Depression and anxiety, along with associated impairment, should continue to be carefully monitored to forecast the long-term impact of this crisis. This can help to ensure that future policies consider optimal preservation of both physical and mental health.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1192/bjp.2020.242
Funding
This research was supported by the University of Bristol and Wellcome Trust.
Acknowledgements
The UK Medical Research Council (MRC) and Wellcome Trust (grant number 217065/Z/19/Z), and the University of Bristol, provide core support for ALSPAC. A comprehensive list of grant funding is available on the ALSPAC website (http://www.bristol.ac.uk/alspac/external/documents/grant-acknowledgements.pdf). We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. Part of this data was collected with REDCap, see the REDCap website for details (https://projectredcap.org/resources/citations/). A.S.F.K., R.M.P., K.T., D.S., S.H., D.A.L. and N.J.T. work in, or are affiliated with, the MRC Integrative Epidemiology Unit, which is funded by the University of Bristol and UK MRC (grants MC_UU_00011/3 and MC_UU_00011/6). A.S.F.K., R.M.P and K.T. are supported by the European Research Council under the European Union's Seventh Framework Programme, and grants 758813 (Mental Health Intergenerational Transmission [MHINT]) and 669545 from the European Research Council Grant Agreements. This work was supported by the Wellcome Trust through the Wellcome Longitudinal Population Studies COVID-19 Secretariat and Steering Group (UK Longitudinal Population Studies [LPS] COVID-19 coordination, grant 221574/Z/20/Z) and the UK MRC COVID-19 Longitudinal Health and Wealth – National Core Study (LHW-NCS, grant MC_PC_20030). This work was also supported by the NIHR Biomedical Research Centre at University Hospitals Bristol NHS Foundation Trust and the University of Bristol, which provides support for D.J.G., P.A.M., S.Z., D.R. and D.A.L. Generation Scotland received core support from the Chief Scientist Office of the Scottish Government Health Directorates (grant CZD/16/6) and the Scottish Funding Council (grant HR03006), and is currently supported by the Wellcome Trust (grant 216767/Z/19/Z). Genotyping of the Generation Scotland samples was carried out by the Genetics Core Laboratory at the Wellcome Trust Clinical Research Facility, University of Edinburgh, Scotland, funded by the MRC and Wellcome Trust (grant 104036/Z/14/Z). This work has made use of the resources provided by the Edinburgh Compute and Data Facility (http://www.ecdf.ed.ac.uk/). N.J.T. is a Wellcome Trust Investigator (grant 202802/Z/16/Z), is the Principal Investigator of ALSPAC (MRC and Wellcome Trust grant 217065/Z/19/Z) and works within the Cancer Research UK (CRUK) Integrative Cancer Epidemiology Programme (grant C18281/A19169). D.A.L. is an NIHR Senior Investigator (grant NF-0616-10102). None of the named funders influenced the study design, data collection, analyses or interpretation of results. The views expressed in this paper are those of the authors and not necessarily of any of the funders, the National Health Service or the Department of Health.
Data availability
ALSPAC data is available to researchers through an online proposal system. Information regarding access can be found on the ALSPAC website (http://www.bristol.ac.uk/media-library/sites/alspac/documents/researchers/data-access/ALSPAC_Access_Policy.pdf). Generation Scotland: Scottish Family Health Study data is available to researchers on application to the Generation Scotland Access Committee ([email protected]). The managed access process ensures that approval is granted only to research that comes under the terms of participant consent.
Author contributions
A.S.F.K., R.M.P., M.J.A., K.N., K.T., A.M.M., D.A.L., D.P. and N.J.T. contributed to the conception and design of the study. A.S.F.K., R.M.P., M.J.A., K.N., A.C., S.H., C.F.-R., D.A., R.F., D.S., D.A.L., D.P. and N.J.T. contributed to the organisation of the conduct of the study. A.S.F.K. carried out the study (including acquisition of data). A.S.F.K. and M.J.A. analysed the data. A.S.F.K. and R.M.P. drafted the initial output. All authors contributed to the interpretation of data. All authors have read and approved the final version of the manuscript. A.S.F.K. will serve as guarantor for the contents of the paper. H.B., N.W., S.Z., D.J.G., P.A.M., N.M., A.R., M.H. and D.R. contributed to the interpretation of data and approved the final version of the manuscript.
Declaration of interests
D.A.L. declares receiving research support from several national and international government and charity funders and Roche Diagnostics and Medtronic Ltd for research unrelated to that presented here. All other authors declare no competing interests.








eLetters
No eLetters have been published for this article.